Abstract
We have previously described critical and non-redundant roles for the PI3K p110δ during the activation and differentiation of naïve T cells and p110δ inhibitors are currently being developed for clinical use. However, to effectively treat established inflammatory or autoimmune diseases it is important to be able to inhibit previously activated or memory T cells. In this study, using the isoform-selective inhibitor IC87114, we show that sustained p110δ activity is required for IFNγ production. Moreover, acute inhibition of p110δ inhibits cytokine production and reduces hypersensitivity responses in mice. Whether p110δ played a similar role in human T cells was unknown. Here we show that IC87114 potently blocked TCR-induced PI3K signaling by both naïve and effector/memory human T cells. Importantly, IC87114 reduced cytokine production by memory T cells from healthy and allergic donors and from inflammatory arthritis patients. These studies establish that previously activated memory T cells are at least as sensitive to p110δ inhibition as naïve T cells and show that mouse models accurately predict p110δ function in human T cells. There is therefore a strong rationale for p110δ inhibitors to be considered for therapeutic use in T cell-mediated autoimmune and inflammatory diseases.
Introduction
In many immune-mediated diseases, T cells with an activated or memory phenotype accumulate at the site of tissue destruction. Genetic susceptibility to autoimmunity is often linked to the MHC locus and other loci that affect T cell biology, thus implying pathological roles for T cells in autoimmunity 1,2. Indeed there is mounting evidence that perturbation of antigen receptor signaling in T cells often contributes to autoimmune diseases 3. Therapeutics affecting T cells such as glucocorticoids, methotrexate, cyclosporine (CS), CTLA4-Ig, and rapamycin are used effectively to treat or ameliorate immune-related disorders. However, these therapies can be associated with undesirable side-effects and/or unresponsiveness in some patients 4-7. Hence, there is a real need for additional drugs that target T cells but do not compromise organ function or leave the patient unduly susceptible to infections.
The Class I PI3Ks phosphorylate phosphatidylinositol-(4,5)-phosphate to produce phosphatidylinositol-(3,4,5)-phosphate (PIP3). PIP3 acts as a second messenger by recruiting pleckstrin homology (PH) domain-containing proteins to the plasma membrane where they activate signaling pathways that promote proliferation, survival, differentiation, and chemotaxis 8. Class I PI3Ks are sub-divided into two groups based on their structure: Class IA PI3Ks are heterodimers consisting of one regulatory subunit (p85α,p85β, p50α, p55α, or p55γ) and one catalytic subunit (p110α, p110β, or p110δ) while Class IB PI3Ks are heterodimers consisting of one regulatory subunit (p101 or p84) and a single catalytic subunit (p110γ) 9.
p110δ is expressed at high levels in leukocytes, and is a major PI3K isoform controlling antigen (Ag)-evoked immune responses 10,11. Genetic inactivation of p110δ in mice results in impaired B cell development and function 12-16, diminished primary and secondary T cell-dependent immune responses 12,17,18, failure of naïve cells to differentiate to TH1 or TH2 subsets 19, decreased regulatory T cell numbers and function 20, and altered Ag-induced trafficking of T cells 21. Nonetheless, T cell development occurs normally in p110δ-deficient mice, suggesting that p110δ is not essential for all aspects of TCR signaling 12-14. Additional roles for p110δ have been described in mast cells 22,23, neutrophils 24-26 and NK cells 27-31. Genetic or pharmacological inhibition of p110δ using the small molecule inhibitor IC87114 (IC) reduced disease severity in preclinical rodent models of rheumatoid arthritis 25, asthma 18,32, and allergy 22,23, while glucocorticoid resistance was reversed in a smoking-induced airway inflammation model 33. p110δ selective inhibitors also reduced proliferation of acute myeloid leukemia cells and rendered them more sensitive to chemotherapeutics 34,35. Together, these results suggest that small-molecule inhibitors against p110δ may be used to alleviate immune system-mediated diseases. Indeed, p110δ-selective inhibitors are currently being evaluated in Phase I clinical trials 36.
Much of our knowledge of p110δ comes from mouse studies. Although broadly similar, human and mouse immune systems harbor some notable differences 37. This also extends to the PI3K signaling pathway since human neutrophils are more reliant on p110δ than mouse neutrophils for fMLP responses 24. This result stresses the requirement to validate results obtained from mouse studies in human experimental model systems. It is also worth noting that as a consequence of multiple exposures to infectious organisms, humans tend to have greater proportions of memory cells than do mice bred in a pathogen-free environment. Inhibiting previously activated T cells will likely be critical if p110δ inhibitors are to be used effectively to treat T-cell mediated pathologies.
In the p110δD910A mouse which was genetically engineered to express catalytically inactive p110δ, naïve CD4+ T cells proliferated poorly and produced significantly less cytokine, suggesting that p110δ activity is required for optimal responses to antigen, especially under sub-optimal stimulation conditions (e.g. in the absence of costimulation) 12,17,19. Previously activated T cells (referred to here as effector or memory T cells) have a lower threshold of activation linked to re-wiring of signal transduction pathways and are less dependent on costimulation 38. Hence it was not obvious whether p110δ would boost activation of memory T cells as it does in naïve T cells. In this study, we have used IC to acutely inhibit p110δ in effector and memory T cells from mice and humans and monitored intracellular signaling events, proliferation, cytokine production and inflammatory responses.
We found that sustained p110δ activation is required for IFNγ production and that IC potently blocked effector responses from effector/memory T cells in both species. p110δ inhibition also reduced contact-hypersensitivity (CHS) reactions in mice, and cytokine production by T cells from patients with allergy or reactive arthritis (ReA). We conclude that p110δ plays an important role in the activation of effector and memory T cells in humans and mice.
Materials and Methods
Mice
p110δD910A , OT1 and OT2 mice have been described previously 12,39,40, and were backcrossed to C57BL/6 background for at least 10 generations. Mice were maintained under specific pathogen free conditions. All protocols involving live animals were approved by the United Kingdom Home Office and institutional ethics review.
Reagents
IC87114 26 was synthesized as described (D030 from patent WO 01/81346). IC inhibits p110δ kinase activity with an IC50 between 0.1-0.5 μM, and only shows cross-reactivity with other PI3K isoforms at concentrations over 10 μM 26,41. CS was synthesized at UCB. OVA257-264 and OVA323-339 were synthesized by Southampton Polypeptides. Other chemicals were purchased from Sigma-Aldrich unless otherwise specified.
Culture media
Mouse T cells were cultured in RPMI-1640 (Invitrogen) with 5% FCS (TCS Cellworks), 1% Penicillin-Streptomycin and β-mercaptoethanol. Human cells were cultured in RPMI-1640 and 1% penicillin-streptomycin and either 5% human AB serum or 10% FCS. Cells were incubated at 37°C with 5% CO2.
Mouse cell purification and activation
CD4+ or CD8+ T cells were negatively selected from lymph nodes and/or spleens by magnetic sorting. Cells were incubated with FITC-labeled anti-B220, −CD25, −CD69, −CD49b, and –MHC Class II Abs. CD8+ T cell purifications also included anti-CD4 while CD4+ T cell purifications included anti-CD8 (all eBioscience). Ab-coated cells were then depleted with anti-FITC MACS beads (Miltenyi). The resulting population was ≥95% CD4+ or CD8+. For naïve and effector/memory T cell studies, negatively selected CD4+ T cells were stained with anti-CD62L-PE (eBioscience) before being FACS-sorted into CD62L+ and CD62L− populations. The resulting populations were greater than 97% pure.
To activate CD8+ OT1 T cells or CD4+ OT2 T cells, purified cells were stimulated in triplicate in a 1:1 ratio with irradiated T cell-depleted spleen cells pulsed with 1 μM chicken ovalbumin peptide (OT1:OVA257-264 peptide; OT2: OVA323-339 peptide) in the presence of DMSO alone, LY294002 (LY) or IC. Polyclonal CD62L+ and CD62L− CD4+ T cells were activated in triplicate with 1 μg/mL plate-bound anti-CD3 (Clone 2C11) in the presence of DMSO alone, LY or IC. Supernatants were collected at 48 h and assayed by ELISA (eBioscience), and cells were pulsed with 3H-Thymidine overnight before harvesting.
Anti-CD3 and Concanavalin A (ConA) injections
Mice were dosed once orally with 30 mg/kg IC in 1% methylcellulose (MCL) or with 1% MCL vehicle control alone 30 minutes before they were injected intravenously with anti-CD3 (0.01 mg/kg) or ConA (15 mg/kg). 1.5 hours after injection, the mice were terminally anaesthetized and bled by heart puncture. Cytokine levels in the serum were measured using a FlowCytomix kit from Bender Medsystems.
CHS studies
100μl of 7% TNCB in a 4:1 acetone/olive oil mix or acetone/olive oil alone (for unsensitized controls) was applied to the shaved abdomens of p110δD910A or C57BL/6J controls. Six days later, ear thickness was measured with a micrometer (Kroeplin). Mice were subsequently dosed orally with 30 mg/kg IC in 1% MCL or with 1% MCL vehicle control alone 1 h before and 5 h after elicitation of CHS. To elicit CHS, 1% TNCB in a 9:1 olive oil/acetone mix was applied to an ear. Ear thickness was measured again 24 h later. The change in ear thickness was measured as the size difference before and after re-challenge.
To measure a secondary CHS response, mice were sensitized and elicited as above but without drug treatment during the primary elicitation. Four weeks after the initial sensitization, mice were drug treated and re-elicited as above, and the change in ear thickness calculated after 24 h.
Human cell purification
PBMCs from healthy humans were isolated using a Ficoll gradient. In some experiments, cells were negatively selected according to manufacturer’s instructions using RosetteSep Human T cell Enrichment Cocktail (for total T cells), or EasySep Human Naïve CD4+ T cell or Memory CD4+ T cell Enrichment kits (for naïve or effector/memory T cells respectively) (Stem Cell Technologies). Total CD4+ T cells were negatively selected from atopic donors using Human CD4+ T Cell Isolation Kit II (Miltenyi), and autologous APCs isolated from the positively selected fraction. Purified cells were >95% pure. Mononuclear cells were also isolated from the synovial fluid of patients fulfilling ESSG criteria for spondyloarthritis, and had clinical reactive arthritis (ReA)42.
Human T cell biochemistry
For Western blot analysis, total (CD3+) T cells were pre-treated with DMSO alone, LY or IC and subsequently stimulated by first adding 0.3 μg/mL anti-CD3 (Clone OKT3) and 1 μg/mL anti-CD28 (Clone CD28.2; Immunotech). After 2 min, these Abs were cross-linked for 5 min with 10 μg/mL goat anti-mouse IgG, F(ab’)2 (Jackson ImmunoResearch). Lysates were probed with polyclonal rabbit anti-phospho-Ser473-Akt, -Thr308-Akt, -Thr202/Tyr204-Erk1/2, total Akt and total Erk1/2 (all Cell Signaling Technologies).
For fluorescent cell bar-coding experiments, total T cells were pre-treated with DMSO alone, LY or IC and subsequently stimulated by first adding 0.3 μg/mL biotinylated anti-CD3 and 5 μg/mL biotinylated anti-CD28. After two min, cells were cross-linked with 20μg/mL avidin (Zymed) at 37C, and aliquots were withdrawn at the indicated time points. Cells were fixed for 10min at 37 °C with Fix Buffer I (BD Biosciences), washed, and then fluorescently bar-coded as described previously43. Briefly, aliquots were stained for 20 min at room temp in different dilutions of Alexa Fluor 488 and Pacific Blue™ succinimidyl ester (Invitrogen), providing each sample with a unique fluorescent signature. Cells were washed and then pooled for further staining. Cells were permeabilized in Perm Buffer III (BD Biosciences), washed and stained with phosphospecific Abs (Cell Signal Technology: Alexa 647-conjugated pSer473-Akt clone D9E, pThr202/Tyr204-Erk1/2 clone E10, or pSer235/236-S6 clone D57.2.2E; or unconjugated pSer9-GSK3β followed by Alexa-647 goat anti-rabbit IgG (Invitrogen)) and lineage markers (CD3 clone SK7, CD4 clone SK3, CD45RO clone UCHL1; all BD Biosciences) for 30 min at room temp. T cell subsets were defined as follows: Naïve CD4+ (CD3+CD4+CD45RO−), effector/memory CD4+ (CD3+CD4+CD45RO+), naïve CD8+ (CD3+CD4−CD45RO−), and effector/memory CD8+ (CD3+CD4−CD45RO+). Cells were processed on a FACS Canto II flow cytometer (BD Biosciences). Data were analyzed using the Stanford University Cytobank program (http://cytobank.stanford.edu/). Arcsinh medians with a co-factor of 150 were used for the statistical calculation of fold change in Alexa-647 between individual samples using the following equation:
Results were visualized either as heatmaps or as overlaid histograms.
Human T cell activation
CD3+ human primary T cells were activated with T Cell Expander Dynabeads (Invitrogen) in a 1:1 bead to cell ratio. Supernatants for IL2 and IFNγ measurements were collected after 16 h. CD45RA+ or CD45RO+ CD4+ T cells were stimulated with 3.75 μg/mL plate-bound anti-CD3 (Clone UCHT1; BD Bioscience) for 48 h before measuring proliferation and cytokine production. Total PBMCs were stimulated with 1 μg/mL tetanus toxin (Calbiochem) for seven days before measuring proliferation and cytokine production. CD4+ T cells from PBMCs of atopic donors were mixed 1:1 with autologous APCs and stimulated with 25 μg/mL house dust mite antigen (Greer Laboratories) for six days before measuring cytokine production. Mononuclear cells from the synovial fluid of ReA patients presenting in clinic were stimulated with plate-bound anti-CD3 for 72 h before measuring proliferation and cytokine production. Cytokine concentrations from culture supernatants were assayed by ELISAs from R&D Systems or MesoScale Discovery.
Statistics
In mouse experiments, the effects of genetic or pharmacological inactivation of p110δ were compared to uninhibited wild type (WT) controls in mice using Student’s t tests, except for the CHS studies where the one way ANOVA with a Bonferroni post-test was used. Responses of human cells treated with IC were compared to DMSO controls using one-sided repeated measures ANOVA on log-transformed data. Responses of cells treated with LY or CS were compared to DMSO controls using Student’s t test on log-transformed data. Probabilities were calculated using GraphPad Prism or SPSS, and p values are annotated on figures with the following symbols: *0.01≤p≤0.05 **0.001≤p≤0.01 ***p≤0.001. % inhibition of human cells was calculated as: 100* (1-((inhibited sample –unstimulated sample)/ (uninhibited sample –unstimulated sample)), and median values are shown below the graphs with negative numbers indicating an enhanced response.
Results
Naïve and effector/memory mouse CD4+ T cells are sensitive to p110δ inhibition
We have previously shown that p110δ is required for PIP3 accumulation for at least 30 min after TCR stimulation in CD4+ T cells 17. However, the kinetics of PI3K activation after this time point is unknown. CD8+ T cells only required PI3K activation for the first nine hours after activation to induce a full proliferative program 44. This suggested that prolonged activation of PI3Ks (including p110δ) may not be required in T cells.
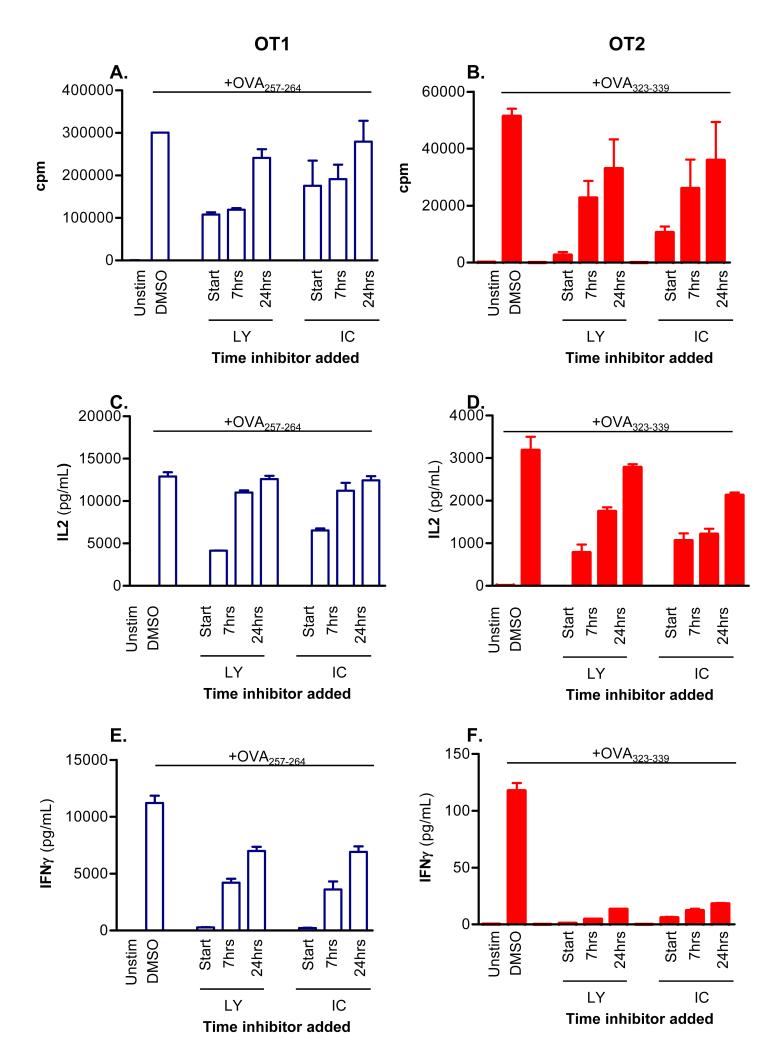
To examine this hypothesis further, OT1 (CD8+) and OT2 (CD4+) TCR transgenic cells were activated with APCs and peptide, and either 10 μM of the pan-PI3K inhibitor LY or 5 μM of the p110δ-selective inhibitor IC were added at the start of the culture or up to 24 h later. Proliferation, IL2 and IFNγ production after 48 h were subsequently compared to DMSO-treated controls. In both CD8+ and CD4+ T cells, proliferation and IL2 production were only minimally affected when either LY or IC was added 24 h after activation (Figure 1A-D). By contrast, delayed addition of IC profoundly blocked IFNγ production (Figure 1E, F). We conclude that both in CD4+ and CD8+ T cells, p110δ activity needs to be sustained for longer to optimize IFNγ production than is required for proliferation or IL2 production.
Figure 1. p110δ regulates cytokine production late after TCR stimulation.
CD8+ OT1 (left column) or CD4+ OT2 (right column) T cells were stimulated with irradiated APCs+1 mM OVA peptide or left unstimulated. 10 mM LY or 5 mM IC was added either at the start of co-culture, seven or 24 h later. Vehicle control (DMSO) was added at the experiment start for uninhibited controls. After 48 h, proliferation (A, B), IL2, (C,D) and IFNγ production (E, F) were measured. Data shown are mean ± SEM of triplicate readings and are representative of two independent experiments.
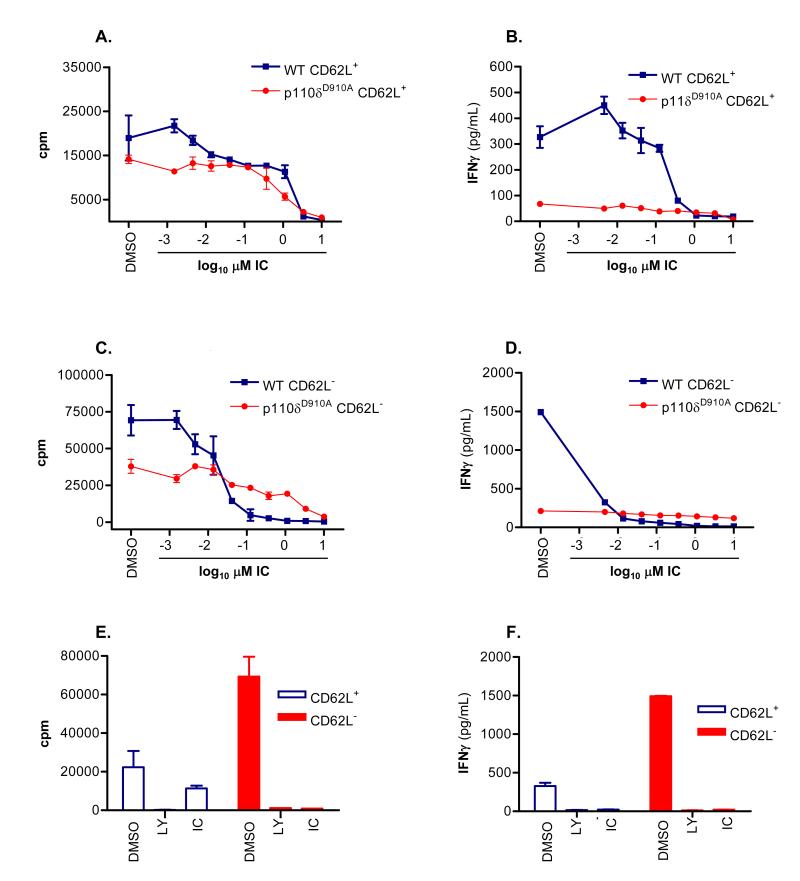
We next asked whether previously activated CD4+ T cells also retained sensitivity to p110δ inhibition. CD4+ T cells from (wild-type) WT and p110δD910A mice were sorted into naïve CD62L+ and effector/memory CD62L− populations, and stimulated with plate-bound anti-CD3 in the presence of DMSO, LY or IC added for the duration of the experiment. Proliferation was blocked in WT CD62L+ and CD62L− cells with an IC50 of 1.233±0.16 μM and of 0.04±0.03 μM, respectively (Figure 2A, C). IFNγ production was ten-fold more sensitive with IC50’s of 0.12± 0.09 μM and 0.001± 0.0007 μM in WT CD62L+ and CD62L− cells, respectively (Figure 2B, D). Inactivation of p110δ by 1 μM IC blocked cytokine responses to similar levels as did 10 μM LY (Figure 2E, F). Naïve CD62L+ CD4+ T cells from p110δD910A mice proliferated poorly and produced only 20% of the IFNγ seen in WT cells (Figure 2A, B) as seen previously 19. Here we extend these findings by showing that the same pattern persists in previously activated CD62L− p110δD910A T cells. Although IC showed some suppression of p110δD910A T cell proliferation at the higher concentrations, the low amount of IFNγ produced by p110δD910A T cells was not further reduced by IC (compare Figures 2A and 2C with 2B and 2D). The minimal impact of IC on IFNγ production by p110δD910A cells suggests that the inhibition of WT cells at low concentrations was not due to off-target effects (Figure 2B, D).
Figure 2. p110δ regulates naïve and effector/memory CD4+ T cell activation.
CD62L+ (naïve) and CD62L− (effector/memory) CD4+ T cells from WT and p110δD910A mice were stimulated by anti-CD3 in the presence of DMSO alone, LY or IC. After 48 h, proliferation (A, C, E) and IFNγ production (B, D, F) were measured. The effects of IC on naïve (A, B) or effector/memory (C, D) T cells were determined. Proliferation (E) and IFNγ production (F) were measured in WT cells when cells were treated with DMSO alone, 10 mM LY or 1 mM IC. Data shown are the mean ± SEM of replicate readings and are representative of at least two independent experiments.
To determine if acute the effect of acute p110δ inhibition on cytokine responses in vivo, mice were injected with anti-CD3 or ConA and cytokine levels in the serum was measured 1.5 hours later. Oral administration of IC reduced IL2, IL4, IL17, IFNγ and TNFα levels in the serum (Figure 3 A-E).These results demonstrate that IC can block T cell-dependent cytokine production in vivo.
Figure 3. IC reduces T cell cytokine production and contact hypersensitivity responses in vivo.
WT B6 mice were given one oral dose of IC (30 mg/kg) 30 minute before being administered anti-CD3 or ConA intravenously. Cytokines concentrations in the serum 1.5 h post injection were measured. A: IL2, B: IL4, C: IL17, D: IFNγ, E: TNFα. F-G: WT and p110δD910A mice were sensitized on the abdomen with TNCB and then re-challenged with TNCB on one ear 6 days (F; primary response) or 6 and 30 days (G; secondary response) later. Mice were dosed twice orally with 30 mg/kg IC or methylcellulose (MCL) alone on the day of the final re-challenge, and the change in ear thickness was measured 24 h later. The effect of p110δ genetic or pharmacological inactivation was compared to WT mice receiving MCL only, and p values were calculated using one way ANOVA with Bonferroni post-test. p values are represented with the following symbols: *0.01≤p≤0.05 **0.001≤p≤0.01 ***p≤0.001. Data is representative of 3 experiments for primary responses and 1 experiment for secondary responses.
To test if p110δ inhibition could impair functional recall responses in vivo, the ability of IC to block elicitation of a T cell-dependent CHS reaction was tested. WT or p110δD910A mice were sensitized topically on their abdomens with the hapten trinitrochlorobenzene (TNCB), and then re-challenged after six days on one ear. Mice were dosed twice with either 30 mg/kg IC or 1% methylcellulose (MCL) vehicle control on the day of re-challenge, and ear swelling was measured 24 h later (Figure 3F)). Ear swelling was reduced by ~60% in both WT mice treated with IC and in p110δD910A mice, showing that acute blockade of p110δ in primed cells reduced hypersensitivity as effectively as blocking p110δ chronically in naïve cells. IC treatment in p110δD910A mice did not suppress swelling further, showing that inhibition by drug was not due to off-target effects (Figure 3F). No response was observed from either genotype when mice were challenged on their ear in the absence of prior sensitization (data not shown), confirming that the swelling responses were mediated by primed effector cells.
To determine whether a secondary response to TNCB retained the same sensitivity to p110δ inhibition, WT and p110δD910A mice were sensitized and elicited as before except without drug treatment. Four weeks after initial sensitization, ears were TNCB-challenged for a second time and mice were dosed twice with either 30 mg/kg IC or 1% MCL vehicle control on the day of the second re-challenge. The ears of both WT and p110δD910A mice were more swollen after the second elicitation than the first (Figure 3G and data not shown), indicating that a memory-type response was being measured. Similar to the primary response (Figure 3F), a ~50% reduction in swelling was observed in IC-treated WT mice as well as in p110δD910A mice with or without IC treatment (Figure 3G). We conclude that p110δ participates in primary and secondary responses in vivo.
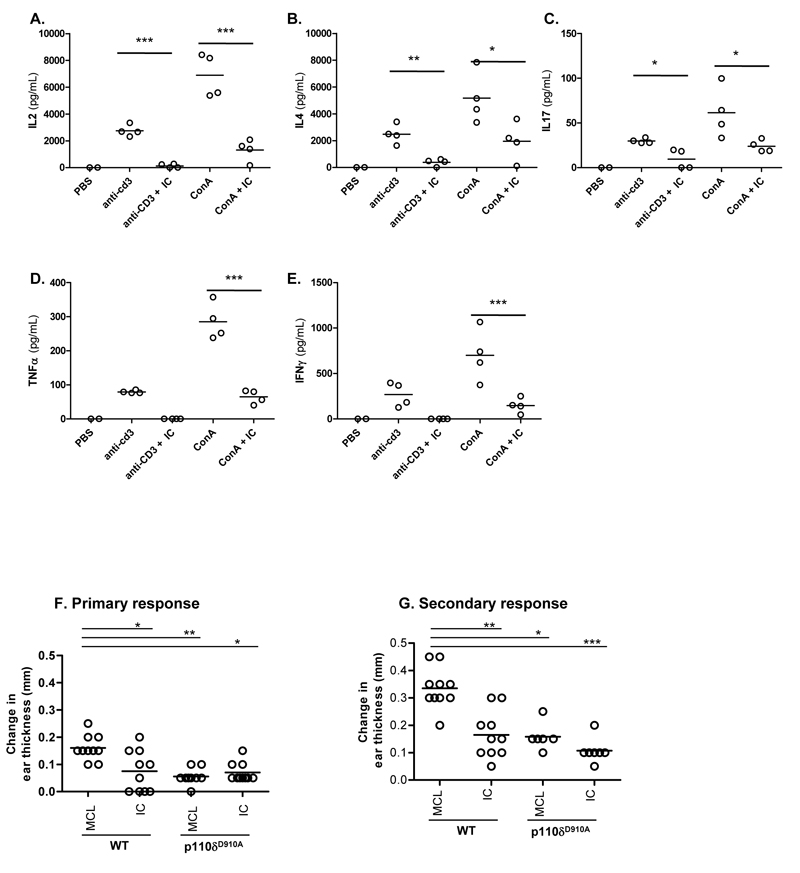
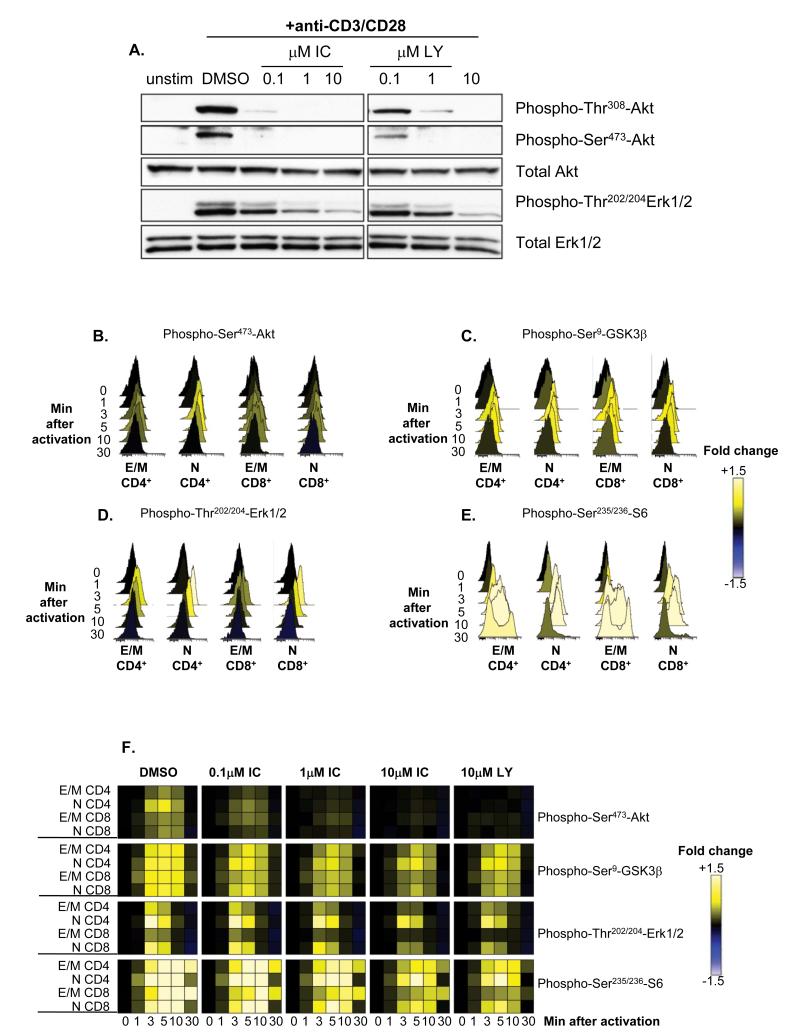
p110δ is the main transducer of PI3K signals in TCR-stimulated human T cells
We have shown that TCR-induced phosphorylation of Akt in mouse T cells is highly sensitive to p110δ inhibition 12,17,19. Because Akt phosphorylation only occurs if PIP3 is produced, these results demonstrated that p110δ is the main PI3K isoform activated by the TCR. To determine if human T cells were also dependent on p110δ to activate the PI3K pathway, primary T cells from healthy donors were stimulated for five minutes with anti-CD3 and anti-CD28 in the presence of DMSO alone, IC or LY, and phosphorylation of Akt and Erk were subsequently analyzed by immunoblotting (Figure 4A). Both LY and IC blocked Akt phosphorylation in a dose-dependent manner. IC inhibited Akt phosphorylation as potently as LY, suggesting that p110δ transmits PI3K signals from the TCR and CD28 in human T cells and that other isoforms cannot substantially compensate. Erk phosphorylation was only partially blocked by 10 μM of either inhibitor, consistent with a non-essential but accessory role for PI3K in regulating Erk in T cells under some stimulatory conditions 12,19.
Figure 4. p110δ regulates TCR signaling by human T cells.
(A) T cells from healthy human donors were pre-treated with DMSO alone, IC or LY and stimulated with anti-CD3 and anti-CD28 for 5 min. Lysates were immunoblotted to examine the levels of total and phosphorylated Akt and Erk. Data represents one of three donors. (B-F) T cells from healthy human donors were pre-treated with DMSO alone, IC or LY and stimulated with anti-CD3 and anti-CD28 for different time points. The pooled bar-coded aliquots were stained for surface markers and phospho-proteins and analyzed by flow cytometry. Populations were gated into naïve (N) and effector/memory (E/M) CD4+ and CD8 + T cells and changes in phosphorylation were assessed for each population. Histograms showing dynamics of phosphorylation of Akt (B), GSK3β (C), Erk (D) and S6 (E) in DMSO treated samples are shown. (F) The data for DMSO and inhibitor-treated samples were converted into a heat map showing fold change compared to unstimulated control. The data presented is representative or three independent experiments with different donors
Some signaling differences have been observed in naïve, activated and memory T cells, and between CD4+ and CD8+ T cells 38,45,46. Hence, it was plausible that IC may affect T cell subsets differently. To compare the potency of IC on different T cell subsets, purified primary T cells were treated with DMSO alone, IC, or LY before stimulation with anti-CD3 and anti-CD28, and PI3K targets were analyzed by phospho-flow cytometry at various time points (Figure 4 B-F). By analyzing populations separately on the basis of surface phenotype, the effects of inhibitors could be assessed in naïve CD4+ (CD3+CD4+CD45RO−), effector/memory CD4+ (CD3+CD4+CD45RO+), naïve CD8+ (CD3+CD4−CD45RO−), and effector/memory CD8+ T cells (CD3+CD4−CD45RO+). Raw data were then converted into a heat map comparing the change in fluorescence to an unstimulated control. Histograms for samples treated with DMSO alone (Figure 4 B-E) are shown to demonstrate the levels of phosphorylation represented by each color in the heat map (Figure 4F). Each subset reacted similarly to IC, with phosphorylation of Akt, S6 and GSK3β reduced at even the lowest concentration of IC while Erk phosphorylation was only diminished at 10 μM IC (Figure 4F). These data demonstrate that in each T cell subset, CD3 and CD28 activate p110δ and that prior activation status does not influence sensitivity to IC. Moreover, these data reveal redundancy in signals leading to GSK3 and S6 phosphorylation as these phosphorylation events were less sensitive to PI3K inhibition than was Akt phosphorylation. Indeed, Erk and Rsk are known to contribute to these signaling events independently of PI3K 47,48.
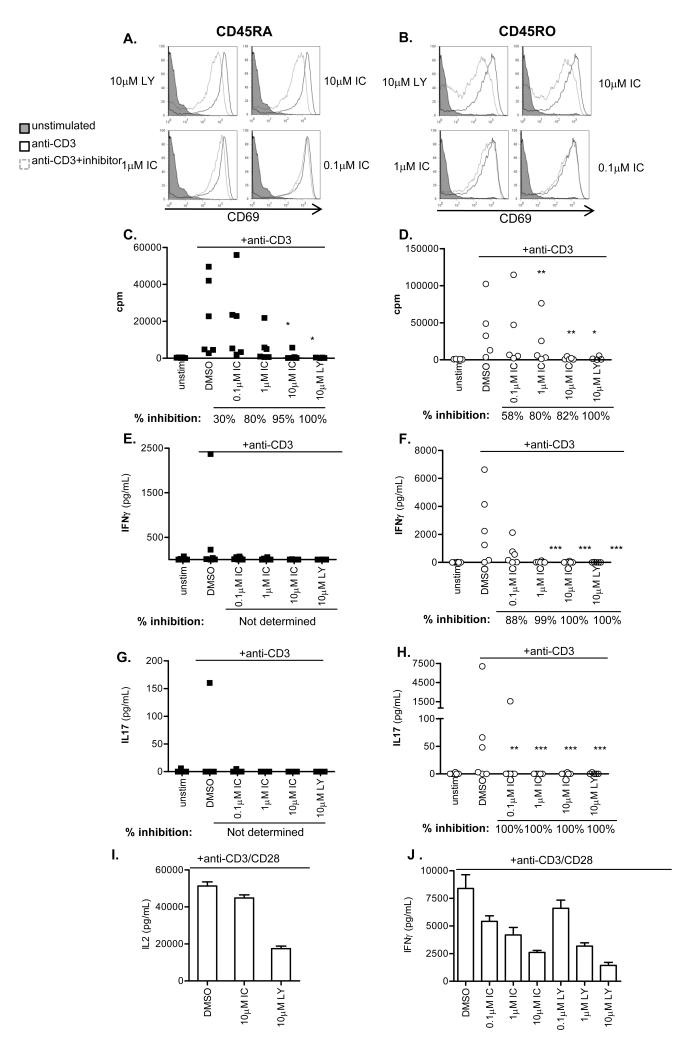
Because IFNγ is primarily secreted by previously activated T cells, we next sub-fractionated CD4+ T cells isolated from healthy donors into naïve CD45RA+ and effector/memory CD45RO+ populations, and stimulated for 48 h with anti-CD3 in the presence DMSO alone, LY or IC. Up-regulation of the activation marker CD69 was undiminished in all but the highest concentration of PI3K inhibitors which correlated with the level of Erk inhibition (Figure 5A, B). However, IC concentrations between 1-10 μM diminished proliferation of both CD45RA+ and CD45RO+ CD4+ T cells to a similar extent as LY (Figure 5C, D). IFNγ and IL17 production was undetectable in CD45RA+ cells from most donors, but LY and IC profoundly blocked production of IFNγ and IL17 by CD45RO+ cells (Figure 5F, H). Individual donors varied in sensitivity to IC at the lowest concentration used (0.1 μM). To indicate the most common level of inhibition observed, % inhibition was calculated for each donor as described in Materials and Methods and the median value shown beneath the graph. These data suggest that human effector/memory T cells are at least as sensitive to p110δ inhibition as naïve T cells.
Figure 5. p110δ inhibitors block proliferation and cytokine production by naïve and effector/memory CD4+ T cells.
CD4+CD45RA+ (left column) and CD4+CD45RO+ (right column) T cells were stimulated with anti-CD3 in the presence of DMSO alone, IC or LY. At 48 h, CD69 expression.(A,B), proliferation (C,D), IFNγ (E,F), and IL17 (G,H) production were measured. (A,B) Data is representative of one of three donors. (C-H) Each dot represents an individual donor. To calculate p values, Student’s t test was used to compare DMSO alone to LY, and one-way repeated measures ANOVA was used to compare DMSO alone to IC. p values are represented with the following symbols: *0.01≤p≤0.05 **0.001≤p≤0.01 ***p≤0.001. % inhibition was calculated for each donor to determine the range of sensitivity in the population, and median values shown below the graph. I-F: T cells were stimulated for 16 h with anti-CD3 and anti-CD28 in the presence of DMSO alone, IC or LY, and IL2 (I) or IFNγ (J) production was measured. Data shows mean ± SEM of triplicate readings and is representative of one of three donors.
Because CD28 costimulation has been shown, under some circumstances, to be insensitive to p110δ inhibition 12, we also stimulated human T cells with anti-CD3 and anti-CD28. Consistent with previous results in mouse 12, we found that anti-CD28 stimulated robust IL2 production in absence of p110δ activity. However, IFNγ production was inhibited by IC in a dose dependent manner. The ability of LY, but not IC to inhibit IL2 production may reflect a role for mTOR in blocking IL2 production as LY, but not IC, targets the catalytic activity of this kinase 41.
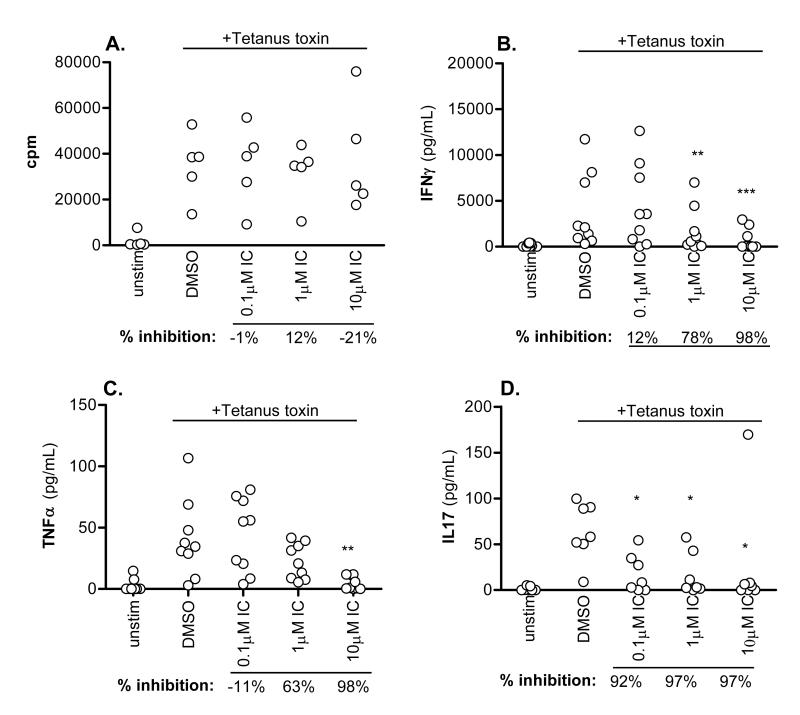
CD45R0+ cells include both recently activated effector and resting memory cells. As a second, more definitive approach to monitor the sensitivity of human memory T cells to p110δ inhibition, unfractionated PBMCs were pulsed with tetanus toxin in the presence of DMSO alone or IC. Tetanus toxin will only elicit a response from individuals who have previously been vaccinated against tetanus and the response is mediated by memory cells. Proliferation was unaffected by p110δ in this context (Figure 6A) (although we observed some inhibition of proliferation in other experiments). However, T cell-derived cytokine production was still blocked by IC, with >50% of IFNγ and TNFα production blocked at ≥1μM and IL17 blocked at ≤0.1μM (Figures 6B-D). We conclude that cytokine production by human memory T cells is highly sensitive to p110δ inhibition.
Figure 6. p110δ inhibition blocks recall responses.
PBMCs from healthy donors were stimulated with tetanus toxin in the presence of DMSO alone or IC. After 7 days, proliferation (A), IFNγ (B), TNFα (C), and IL17 (D) production were measured. Each dot represents an individual donor. To calculate p values, one-way repeated measures ANOVA was used to compare DMSO alone to IC. p values are represented with the following symbols:*0.01≤p≤0.05 **0.001≤p≤0.01 ***p≤0.001. % inhibition was calculated for each donor to determine the range of sensitivity in the population, and median values are shown below the graph.
p110δ inhibitors block cytokine production from disease-associated T cells
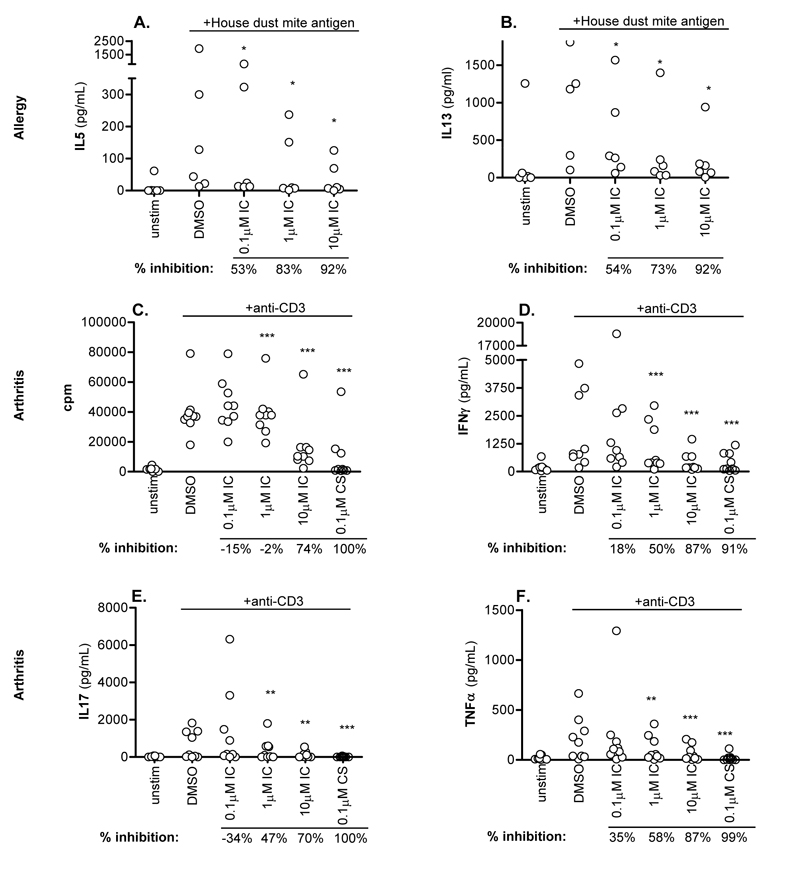
Because p110δ inhibitors are being developed to treat immune disorders, we asked how effective IC was in dampening T cell responses from individuals presenting with atopy or inflammatory arthritis. Unfractionated PBMCs from allergic individuals were stimulated with house dust mite antigen in the presence of DMSO alone or IC, and assayed after 6 days for TH2 cytokine production (Figure 7A, B). In five donors, IC blocked cytokine production potently, though a sixth donor was unresponsive. IC blocked IL5 production with an IC50 range between 0.06 and 0.35 μM and IL13 with an IC50 range between 0.1 and 0.3 μM (data not shown). Our data show that allergen-driven TH2 T cells are sensitive to p110δ inhibition.
Figure 7. p110δ inhibition blocks recall responses from disease samples.
(A,B) PBMCs from atopic individuals were pulsed with house dust mite antigen in the presence of DMSO alone or IC. After 6 days, IL5 (A) and IL13 (B) were measured. (C-F) Mononuclear cells from synovial fluid of ReA patients were stimulated with anti-CD3 in the presence of DMSO alone, IC or CS. Proliferation (C), IFNγ (D), IL17 (E) and TNFα (F) production were measured at 72 h. Each dot represents an individual donor. To calculate p values, Student’s t test was used to compare DMSO alone to CS, and one-way repeated measures ANOVA was used to compare DMSO alone to IC. p values are represented with the following symbols: *0.01≤p≤0.05 **0.001≤p≤0.01 ***p≤0.001. % inhibition was calculated for each donor to determine the range of sensitivity in the population, and median values are shown below the graph.
As in rheumatoid arthritis, T cells from the synovial fluid (SF) of ReA patients have an effector/memory phenotype and secrete large quantities of IL17 and TNFα 49. We stimulated ReA SF mononuclear cells with anti-CD3 in the presence of DMSO alone, IC or CS, and proliferation and arthritis-associated cytokine production were assayed after 72 h. Proliferation was unaffected, but IFNγ, IL17 and TNFα production were all blocked in a dose-dependent manner with the highest concentrations of IC achieving a similar abrogation as CS (Figure 7 C-F). This suggests that p110δ inhibition has the potential to be an effective blocker of TH1 and TH17 inflammatory T cell responses in the context of inflammatory arthritis.
Discussion
In this study, we have demonstrated that both mouse and human effector/memory T cells are highly sensitive to p110δ inhibition. Moreover, cytokine production by disease-enhancing T cells can be blocked by a p110δ-specific inhibitor.
In mice, genetic models showed that p110δ is a crucial PI3K isoform involved in TCR-induced signaling 12,17,19. Here we show that both CD62L+ naïve T cells and CD62L− effector/memory T cells are sensitive to inhibition with the p110δ-selective inhibitor IC. Indeed, effector/memory T cells appeared more sensitive to IC, suggesting that it might be possible to tune the level of p110δ inhibition in the clinic to preferentially affect pathogenic T cells. We also demonstrated that signals transduced by p110δ 24 h or more after initial TCR stimulation can potently promote IFNγ production, suggesting that p110δ inhibitors may be effective during an on-going immune response. Chronic inactivation of p110δ in p110δD910A mice or acute p110δ inactivation with IC partially blocked CHS in mice during primary and secondary responses. These and previous studies 18,32,33 suggest that p110δ inhibitors have promising therapeutic potential for the treatment of T cell-mediated pathologies. However, no studies had directly addressed the role of p110δ in TCR activation of human T cells and the possibility remained that additional PI3K isoforms might render p110δ redundant. This appears not to be the case, as IC inhibited anti-CD3 and anti-CD28 stimulated phosphorylation of Akt and reduced phosphorylation of Akt targets S6 and GSK3β at a concentration where it does not inhibit other PI3K isoforms. Blockade of TCR-induced p110δ signaling did not lead to generalized T cell suppression, as CD69 up-regulation was unaffected except at the highest doses of inhibitor. Instead, p110δ inhibition had a selective effect on cytokine production, which could be reduced or completely blocked in effector/memory T cells. We had previously demonstrated in mice that naive T cells require p110δ activity for differentiation to T helper subsets 19; here we extend this work by demonstrating that sustained p110δ activity controls cytokine production in differentiated T cells.
Re-activation of memory T cells is involved in disease maintenance in many inflammatory conditions, and blockade of their cytokine production may limit activation of accessory cells and tissue destruction. This is evidenced by elevated levels of TH2 cytokines in atopy and asthma and TH1 and TH17 cytokines in arthritis and chronic obstructive pulmonary disease 5,6. Modulation of cytokine responses can be efficacious in the clinic. The therapeutic benefit observed with corticosteroid treatment for asthma and TNFα antagonists for arthritis and other autoimmune disorders such as psoriasis is thought to reflect suppression of the expression of inflammatory cytokines 6,7. However, severe asthmatics and patients with COPD often resist corticosteroids and many arthritis patients are refractory to TNFα antagonists 5,6. Thus additional strategies are needed to complement or supplement existing drugs. Here we show that p110δ inhibitors potently suppress TH2-associated cytokines produced by T cells from allergic patients. In addition, we show that when mononuclear cells from sites of active inflammation in ReA patients were treated with IC, cytokine responses that directly drive disease were dampened. In rheumatoid arthritis, synovial fluid cells show elevated phosphorylation of Akt and other downstream molecules 50-52. It is therefore plausible that dysregulation of PI3K-dependent pathways may directly contribute to or drive inflammatory disease.
In conclusion, we demonstrate here that both mouse and human effector/memory cells utilize p110δ to promote cytokine production in T cells and that p110δ should therefore be considered as a target for therapeutic intervention of T cell-mediated pathology.
Acknowledgements
We thank Anne Segonds-Pichon for help with statistical analysis; and Bart Vanhaesebroeck and Fabien Garcon for critical review of manuscript. Funding for this research was supported by grants from the Biotechnology and Biological Sciences Research Council (BSRC) (KO) and the Norwegian Functional Genomics Program, the Research Council of Norway, the Norwegian Cancer Society and, Novo Nordic Foundation (KT). DR was supported by a joint Collaborative Award in Science and Engineering from the BBSRC and UCB.
Footnotes
Authorship Contributions DRS, EB, KM, VQD, DTP, FG and PB did experiments and analyzed data, KMT, BT, KT, PB and KO supervised the project and analyzed data, JC and HG provided essential materials and advice, DRS wrote the paper with help from EB and KO. All authors read and commented on a draft of the manuscript and contributed intellectually to the project.
Disclosure of conflicts of interest Some of the authors are or have been employees of a company that develop PI3K inhibitors.
Ethical approval All experiments involving mice were conducted in according protocols approved by the UK Home Office and institutional ethical review committees. All human tissues had been donated under informed consent and experiments were done in accordance with institutional ethical review guidelines.
References
- 1.Pearce SH, Merriman TR. Genetic progress towards the molecular basis of autoimmunity. Trends Mol Med. 2006;12:90–98. doi: 10.1016/j.molmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Taneja V, David CS. Lessons from animal models for human autoimmune diseases. Nat Immunol. 2001;2:781–784. doi: 10.1038/ni0901-781. [DOI] [PubMed] [Google Scholar]
- 3.Zikherman J, Weiss A. Antigen receptor signaling in the rheumatic diseases. Arthritis Res Ther. 2009;11:202. doi: 10.1186/ar2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Neill LA. Targeting signal transduction as a strategy to treat inflammatory diseases. Nat Rev Drug Discov. 2006;5:549–563. doi: 10.1038/nrd2070. [DOI] [PubMed] [Google Scholar]
- 5.McInnes IB, Schett G. Cytokines in the pathogenesis of rheumatoid arthritis. Nat Rev Immunol. 2007;7:429–442. doi: 10.1038/nri2094. [DOI] [PubMed] [Google Scholar]
- 6.Barnes PJ. Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol. 2008;8:183–192. doi: 10.1038/nri2254. [DOI] [PubMed] [Google Scholar]
- 7.Feldmann M, Maini SR. Role of cytokines in rheumatoid arthritis: an education in pathophysiology and therapeutics. Immunol Rev. 2008;223:7–19. doi: 10.1111/j.1600-065X.2008.00626.x. [DOI] [PubMed] [Google Scholar]
- 8.Hawkins PT, Anderson KE, Davidson K, Stephens LR. Signalling through Class I PI3Ks in mammalian cells. Biochem Soc Trans. 2006;34:647–662. doi: 10.1042/BST0340647. [DOI] [PubMed] [Google Scholar]
- 9.Vanhaesebroeck B, Leevers SJ, Panayotou G, Waterfield MD. Phosphoinositide 3-kinases: a conserved family of signal transducers. Trends Biochem Sci. 1997;22:267–272. doi: 10.1016/s0968-0004(97)01061-x. [DOI] [PubMed] [Google Scholar]
- 10.Okkenhaug K, Ali K, Vanhaesebroeck B. Antigen receptor signalling: a distinctive role for the p110δ isoform of PI3K. Trends Immunol. 2007;28:80–87. doi: 10.1016/j.it.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fruman DA, Bismuth G. Fine tuning the immune response with PI3K. Immunol Rev. 2009;228:253–272. doi: 10.1111/j.1600-065X.2008.00750.x. [DOI] [PubMed] [Google Scholar]
- 12.Okkenhaug K, Bilancio A, Farjot G, et al. Impaired B and T cell antigen receptor signaling in p110delta PI 3-kinase mutant mice. Science. 2002;297:1031–1034. doi: 10.1126/science.1073560. [DOI] [PubMed] [Google Scholar]
- 13.Jou ST, Carpino N, Takahashi Y, et al. Essential, nonredundant role for the phosphoinositide 3-kinase p110delta in signaling by the B-cell receptor complex. Mol Cell Biol. 2002;22:8580–8591. doi: 10.1128/MCB.22.24.8580-8591.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clayton E, Bardi G, Bell SE, et al. A crucial role for the p110delta subunit of phosphatidylinositol 3-kinase in B cell development and activation. J Exp Med. 2002;196:753–763. doi: 10.1084/jem.20020805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Alwan MM, Okkenhaug K, Vanhaesebroeck B, Hayflick JS, Marshall AJ. Requirement for phosphoinositide 3-kinase p110delta signaling in B cell antigen receptor-mediated antigen presentation. J Immunol. 2007;178:2328–2335. doi: 10.4049/jimmunol.178.4.2328. [DOI] [PubMed] [Google Scholar]
- 16.Llorian M, Stamataki Z, Hill S, Turner M, Martensson IL. The PI3K p110delta is required for down-regulation of RAG expression in immature B cells. J Immunol. 2007;178:1981–1985. doi: 10.4049/jimmunol.178.4.1981. [DOI] [PubMed] [Google Scholar]
- 17.Garcon F, Patton DT, Emery JL, et al. CD28 provides T-cell costimulation and enhances PI3K activity at the immune synapse independently of its capacity to interact with the p85/p110 heterodimer. Blood. 2008;111:1464–1471. doi: 10.1182/blood-2007-08-108050. [DOI] [PubMed] [Google Scholar]
- 18.Nashed BF, Zhang T, Al-Alwan M, et al. Role of the phosphoinositide 3-kinase p110delta in generation of type 2 cytokine responses and allergic airway inflammation. Eur J Immunol. 2007;37:416–424. doi: 10.1002/eji.200636401. [DOI] [PubMed] [Google Scholar]
- 19.Okkenhaug K, Patton DT, Bilancio A, Garcon F, Rowan WC, Vanhaesebroeck B. The p110delta isoform of phosphoinositide 3-kinase controls clonal expansion and differentiation of Th cells. J Immunol. 2006;177:5122–5128. doi: 10.4049/jimmunol.177.8.5122. [DOI] [PubMed] [Google Scholar]
- 20.Patton DT, Garden OA, Pearce WP, et al. Cutting edge: the phosphoinositide 3-kinase p110 delta is critical for the function of CD4+CD25+Foxp3+ regulatory T cells. J Immunol. 2006;177:6598–6602. doi: 10.4049/jimmunol.177.10.6598. [DOI] [PubMed] [Google Scholar]
- 21.Jarmin SJ, David R, Ma L, et al. T cell receptor-induced phosphoinositide-3-kinase p110delta activity is required for T cell localization to antigenic tissue in mice. J Clin Invest. 2008;118:1154–1164. doi: 10.1172/JCI33267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ali K, Bilancio A, Thomas M, et al. Essential role for the p110delta phosphoinositide 3-kinase in the allergic response. Nature. 2004;431:1007–1011. doi: 10.1038/nature02991. [DOI] [PubMed] [Google Scholar]
- 23.Ali K, Camps M, Pearce WP, et al. Isoform-specific functions of phosphoinositide 3-kinases: p110 delta but not p110 gamma promotes optimal allergic responses in vivo. J Immunol. 2008;180:2538–2544. doi: 10.4049/jimmunol.180.4.2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Condliffe AM, Davidson K, Anderson KE, et al. Sequential activation of class IB and class IA PI3K is important for the primed respiratory burst of human but not murine neutrophils. Blood. 2005;106:1432–1440. doi: 10.1182/blood-2005-03-0944. [DOI] [PubMed] [Google Scholar]
- 25.Randis TM, Puri KD, Zhou H, Diacovo TG. Role of PI3Kdelta and PI3Kgamma in inflammatory arthritis and tissue localization of neutrophils. Eur J Immunol. 2008;38:1215–1224. doi: 10.1002/eji.200838266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sadhu C, Masinovsky B, Dick K, Sowell CG, Staunton DE. Essential role of phosphoinositide 3-kinase delta in neutrophil directional movement. J Immunol. 2003;170:2647–2654. doi: 10.4049/jimmunol.170.5.2647. [DOI] [PubMed] [Google Scholar]
- 27.Guo H, Samarakoon A, Vanhaesebroeck B, Malarkannan S. The p110 delta of PI3K plays a critical role in NK cell terminal maturation and cytokine/chemokine generation. J Exp Med. 2008;205:2419–2435. doi: 10.1084/jem.20072327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim N, Saudemont A, Webb L, et al. The p110delta catalytic isoform of PI3K is a key player in NK-cell development and cytokine secretion. Blood. 2007;110:3202–3208. doi: 10.1182/blood-2007-02-075366. [DOI] [PubMed] [Google Scholar]
- 29.Saudemont A, Garcon F, Yadi H, et al. p110gamma and p110delta isoforms of phosphoinositide 3-kinase differentially regulate natural killer cell migration in health and disease. Proc Natl Acad Sci U S A. 2009;106:5795–5800. doi: 10.1073/pnas.0808594106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tassi I, Cella M, Gilfillan S, et al. p110gamma and p110delta phosphoinositide 3-kinase signaling pathways synergize to control development and functions of murine NK cells. Immunity. 2007;27:214–227. doi: 10.1016/j.immuni.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 31.Zebedin E, Simma O, Schuster C, et al. Leukemic challenge unmasks a requirement for PI3Kdelta in NK cell-mediated tumor surveillance. Blood. 2008;112:4655–4664. doi: 10.1182/blood-2008-02-139105. [DOI] [PubMed] [Google Scholar]
- 32.Lee KS, Lee HK, Hayflick JS, Lee YC, Puri KD. Inhibition of phosphoinositide 3-kinase delta attenuates allergic airway inflammation and hyperresponsiveness in murine asthma model. Faseb J. 2006;20:455–465. doi: 10.1096/fj.05-5045com. [DOI] [PubMed] [Google Scholar]
- 33.Marwick JA, Caramori G, Stevenson CC, et al. Inhibition of PI3K{delta} Restores Glucocorticoid Function in Smoking-induced Airway Inflammation in Mice. Am J Respir Crit Care Med. 2009 doi: 10.1164/rccm.200810-1570OC. [DOI] [PubMed] [Google Scholar]
- 34.Sujobert P, Bardet V, Cornillet-Lefebvre P, et al. Essential role for the p110delta isoform in phosphoinositide 3-kinase activation and cell proliferation in acute myeloid leukemia. Blood. 2005;106:1063–1066. doi: 10.1182/blood-2004-08-3225. [DOI] [PubMed] [Google Scholar]
- 35.Billottet C, Grandage VL, Gale RE, et al. A selective inhibitor of the p110delta isoform of PI 3-kinase inhibits AML cell proliferation and survival and increases the cytotoxic effects of VP16. Oncogene. 2006;25:6648–6659. doi: 10.1038/sj.onc.1209670. [DOI] [PubMed] [Google Scholar]
- 36.Flinn JCB IW, Furman RR, Brown JR, Lin TS, Bello C, Giese NA, Yu AS. Preliminary evidence of clinical activity in a phase I study of CAL-101, a selective inhibitor of the p1108 isoform of phosphatidylinositol 3-kinase (P13K), in patients with select hematologic malignancies. ASCO annual meeting; Orlando FL. 2009. [Google Scholar]
- 37.Mestas J, Hughes CC. Of mice and not men: differences between mouse and human immunology. J Immunol. 2004;172:2731–2738. doi: 10.4049/jimmunol.172.5.2731. [DOI] [PubMed] [Google Scholar]
- 38.Chandok MR, Farber DL. Signaling control of memory T cell generation and function. Semin Immunol. 2004;16:285–293. doi: 10.1016/j.smim.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 39.Hogquist KA, Jameson SC, Heath WR, Howard JL, Bevan MJ, Carbone FR. T cell receptor antagonist peptides induce positive selection. Cell. 1994;76:17–27. doi: 10.1016/0092-8674(94)90169-4. [DOI] [PubMed] [Google Scholar]
- 40.Barnden MJ, Allison J, Heath WR, Carbone FR. Defective TCR expression in transgenic mice constructed using cDNA-based alpha- and beta-chain genes under the control of heterologous regulatory elements. Immunol Cell Biol. 1998;76:34–40. doi: 10.1046/j.1440-1711.1998.00709.x. [DOI] [PubMed] [Google Scholar]
- 41.Knight ZA, Gonzalez B, Feldman ME, et al. A pharmacological map of the PI3-K family defines a role for p110alpha in insulin signaling. Cell. 2006;125:733–747. doi: 10.1016/j.cell.2006.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dougados M, van der Linden S, Juhlin R, et al. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991;34:1218–1227. doi: 10.1002/art.1780341003. [DOI] [PubMed] [Google Scholar]
- 43.Krutzik PO, Nolan GP. Fluorescent cell barcoding in flow cytometry allows high-throughput drug screening and signaling profiling. Nat Methods. 2006;3:361–368. doi: 10.1038/nmeth872. [DOI] [PubMed] [Google Scholar]
- 44.Costello PS, Gallagher M, Cantrell DA. Sustained and dynamic inositol lipid metabolism inside and outside the immunological synapse. Nat Immunol. 2002;3:1082–1089. doi: 10.1038/ni848. [DOI] [PubMed] [Google Scholar]
- 45.Kaech SM, Wherry EJ, Ahmed R. Effector and memory T-cell differentiation: implications for vaccine development. Nat Rev Immunol. 2002;2:251–262. doi: 10.1038/nri778. [DOI] [PubMed] [Google Scholar]
- 46.Seder RA, Ahmed R. Similarities and differences in CD4+ and CD8+ effector and memory T cell generation. Nat Immunol. 2003;4:835–842. doi: 10.1038/ni969. [DOI] [PubMed] [Google Scholar]
- 47.Salmond RJ, Emery J, Okkenhaug K, Zamoyska R. MAPK, Phosphatidylinositol 3-Kinase, and Mammalian Target of Rapamycin Pathways Converge at the Level of Ribosomal Protein S6 Phosphorylation to Control Metabolic Signaling in CD8 T Cells. J Immunol. 2009;183:7388–7397. doi: 10.4049/jimmunol.0902294. [DOI] [PubMed] [Google Scholar]
- 48.Shaw RJ, Cantley LC. Ras, PI(3)K and mTOR signalling controls tumour cell growth. Nature. 2006;441:424–430. doi: 10.1038/nature04869. [DOI] [PubMed] [Google Scholar]
- 49.Beacock-Sharp H, Young JL, Gaston JS. Analysis of T cell subsets present in the peripheral blood and synovial fluid of reactive arthritis patients. Ann Rheum Dis. 1998;57:100–106. doi: 10.1136/ard.57.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim KW, Cho ML, Park MK, et al. Increased interleukin-17 production via a phosphoinositide 3-kinase/Akt and nuclear factor kappaB-dependent pathway in patients with rheumatoid arthritis. Arthritis Res Ther. 2005;7:R139–148. doi: 10.1186/ar1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ludikhuize J, de Launay D, Groot D, et al. Inhibition of forkhead box class O family member transcription factors in rheumatoid synovial tissue. Arthritis Rheum. 2007;56:2180–2191. doi: 10.1002/art.22653. [DOI] [PubMed] [Google Scholar]
- 52.Reedquist KA, Ludikhuize J, Tak PP. Phosphoinositide 3-kinase signalling and FoxO transcription factors in rheumatoid arthritis. Biochem Soc Trans. 2006;34:727–730. doi: 10.1042/BST0340727. [DOI] [PubMed] [Google Scholar]