Abstract
Background:
Under the National Vector Borne Disease Control Program, the Enhanced Malaria Control Project (EMCP) with World Bank assistance was implemented in India, in the eastern state of Orissa.
Aims:
This article tries to analyze the possible reasons for the poor performance of EMCP in a few states of India.
Settings and Design:
The eastern state of India is taken as a case study for looking into systemic, human resource, and logistics related issues that could explain the poor performance of EMCP in a few states of India.
Materials and Methods:
Field visits were made to some selected EMCP areas in the state of Orissa. Operational issues-related implementation of various components of the project were scrutinized.
Statistical analysis:
Not Applicable.
Results:
While the project was highly successful in a few states of India, it had limited success in some states. It was learnt that the honorarium meant for Fever Treatment depot [FTD] work was divided among all the malaria workers. In high-risk areas, presumptive radical treatment was being carried on by malaria workers for every case of fever. Using Rapid Diagnostic Tests (RDTs) in such areas seemed to have no relevance. The laboratory technician ignored malaria work, due to a high work load and no additional incentive. In the Primary Health Centers (PHCs) the Medical officers had either not visited the village under indoor residual spray or symbolically visited only five to six houses. Cement tanks had to be built for larvivorus fish breeding. However, they had not been mad.
Conclusions:
The success of a public health program is dependent more on project implementation, management, monitoring, and evaluation of project activities than the volume of financial resource allocation.
KEYWORDS: Malaria, World bank, EMCP
INTRODUCTION
In India, the problem of malaria has been controlled in most parts of the country. The high endemic areas contribute to 80% of the burden of disease in the country. Although approximately 95% of the country's population lives in malaria-endemic areas, 80% of malaria occurs among 20% of the population who are classified as ‘high-risk populations’. The geographical areas where ‘high-risk populations’ reside are, Andhra Pradesh, Chhatisgarh, Gujarat, Jharkhand, Madhya Pradesh, Maharashtra, Orissa, and Rajasthan – the seven north-eastern states – and Sikkim.[1].
The Enhanced Malaria Control Project was launched in April 1997, with the assistance of the World Bank. This directly benefited the six crore Tribal Population of the eight peninsular states covering 100 districts and 19 urban areas. However, the population living in other malaria endemic areas was also benefited, as the strengthening of the components of Information, Education, and Communication (IEC) and Training and Management Information System had covered the entire country.[2]
The medium-term objective of the project was to help India create an enhanced and more effective malaria control program by: (i) using a better mix of effective malaria control interventions, responsive to local needs; and (ii) strengthening of the National Program. The long-term objective was to reduce death, morbidity, and social, and economic losses from malaria.
The Enhanced Malaria Control Project had five components: (i) Early Diagnosis and Prompt Treatment (EDPT); (ii) Selective Vector Control; (iii) Insecticide-treated Bed Nets (ITNs); (iv) Epidemic Response and Inter-sectoral Collaboration; and (v) Institutional Strengthening.[3]
The Project was initiated in 1997 to be taken up for five years. The project initially covered 1045 tribal blocks (PHCs) in 100 districts, in the eight states mentioned earlier. In 2003, it expanded to cover 200 PHCs, and added two states, Karnataka and West Bengal. It was extended up to March 2005.
The Orissa scenario
Malaria is a major public health problem in the state of Orissa, which contributes the highest number of malaria cases (22%); 43% of total P. falciparum cases and about 50% of all reported deaths due to malaria in the country, although it constitutes only 4% of the total population of India. P. falciparum is the major cause of malaria and accounts for 80 – 90% of the malarial cases in the tribal areas of the state, which have distinct ecological features such as hilly terrain, forest fringe, and forested area or foothill ecosystems where all the malariogenic factors operate at their maximum efficiency. Malaria is clearly one of the major health problems in this region and is responsible for the significant morbidity and mortality.[4]
Some of the key inputs that were given to Orissa under EMCP were:
Strengthening early diagnosis and prompt treatment activities by establishing at villages, Drug Distribution Centers (DDCs), which were depots for chloroquine tablets, and Fever Treatment Depots, which in addition to being depots, took blood smears from fever cases. In addition Malaria Link Volunteers (MLVs) were identified at the community level, who would function like FTDs and also undertake health education activities. Rapid Diagnostic Test (RDT) kits were introduced only in EMCP blocks for early detection of malaria cases. Microscopes were bought and provided to all the PHCs to strengthen their laboratory activities. Pre-packaged formulations of chloroquine and primaquine (blister packs) were being distributed in selected areas.
Wages were given for DDT spraying. Use of insecticide treated nets (ITNs) was being promoted. Use of larvivorous fish was being promoted.
Training of health staff for upgradation of skills. Pharmacists were being trained to overcome shortage of laboratory technicians.
Extensive health education activities were being taken up.
MATERIALS AND METHODS
A field visit was undertaken at Dhenkanal, Angul, and Nayagarh districts of Orissa state during the year 2004. Many primary health centres were visited. There was interaction with the health staff.
RESULTS
Malaria link volunteer
Under EMCP, Malaria link volunteer (MLVs) are chosen from the community, who would administer presumptive treatment for every case of fever, collect a blood smear, and carry the blood smear to the primary health center twice week. They are paid a honorarium of INR 450 (about US $ 10) per month under EMCP. Any one from the community such as a teacher, shopkeeper, and the like, could be trained as an MLV. However, as the number of volunteers is limited, Anganwadi workers (AWW) are usually made MLVs. As the AWWs already undertake many activities, the honorarium earned as MLV would compensate them to some extent.
It was observed during the field visit that, in any given district, there were EMCP blocks and non-EMCP blocks. It was found that there was unrest among the AWWs, as for the same work of FTD, some (under EMCP block) got paid and the rest were not paid. Even in the EMCP blocks, only few AWWs could be paid as the number of MLVs to be identified was far lesser than the actual number of AWWs. It was learnt that the honorarium was divided among all the AWWs equally in the EMCP block. So in effect, the AWW who also doubled up as MLV ended up getting only about Rs 100.
Blister packs
These packs contain only four tablets (three chloroquin tablets of 600 mg and one 45 mg tablet). It is designed to increase drug compliance. The patient takes one 600 mg chloroquine tablet + one 45 mg Primaquin tablet on the first day. The second 600 mg chloroquine tablet is taken on the second day, and the third 600 mg chloroquine tablet is taken on the third day. Routinely in the program, the patient needs to swallow almost a ‘handful’ of regular low strength tablets (150 mg chloroquine and 7.5 mg Primaquin tablets). The number of tablets to be swallowed by the patient may go up to 22 according to the regimen followed. The cost of these blister formulations is higher. There is need to generate evidence of increase in the compliance.
Rapid diagnostic test kits
Malaria rapid diagnostic test (RDTs) are being given to the PHCs in the EMCP blocks. These are to be used by the malaria workers who are working in remote and difficult areas. The cost of diagnosis by RDTs is said to be about seven to eight times that of diagnosis by usual microscopy. The issue, as observed in the field, is that in high-risk areas, presumptive radical treatment is being carried on by malaria workers for every case of fever, without waiting for the result of microscopy. Using RDTs in such areas appears of no relevance, as in any case the presumptive radical treatment is being given for all fever cases.
Strengthening of laboratories
Binocular microscopes have been supplied to the PHCs. Upgrading of the laboratories has also been done under the Revised National Tuberculosis Control Program (RNTCP). To overcome shortage of laboratory technicians, the pharmacists in PHCs are trained in malaria microscopy. It was observed during the visit that the same technician had to do both the malaria and tuberculosis diagnosis work. The workload was high. As the technician got some honorarium under RNTCP, the attention to malaria work was limited.
DDT spray
Most of the PHCs had started their first round of the spray operation around May 15, 2004 and had completed by mid July 2004. The PHC Medical Officer (MO) should compulsorily inspect at least 10% of the houses during the spray activity, and Block Extension Educator (BEE) of the PHC should visit at least 20 - 25% of the houses, to monitor and ensure the quality of spray. This was hardly happening. In the PHCs where we went randomly, the MO had either not visited or visited symbolically, five to six houses. Worse yet, in one PHC, the Block Extension Educator had visited only two houses (less than the MO).
Larvivorous fish hatchery
Funds had sanctioned to build a hatchery tank at each PHC at the block level, to breed and supply larvivorous fish for vector control. It was observed that the cement tanks had been built. However, they had not been made functional in many cases, as the staff had not been adequately trained, or no funds were available for maintenance. It should be emphasized that having built the tanks they should be put to use for the intended purpose, lest the tanks themselves turn into breeding grounds for mosquitoes.
DISCUSSION
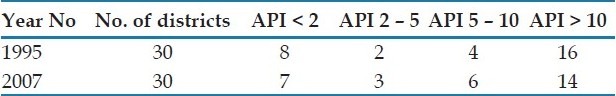
Although health is the state subject as per the constitution of India, the Government of India contributes 50% of the expenditure of the selective activities being carried out by the States for control of malaria. The N.E. states, along with parts of Orissa, Jharkhand, and West Bengal, a population of 100 million, are also receiving special inputs under the Global Fund. The Enhanced Malaria Control Project with the assistance of the World Bank was carried out from September 1997 to December 2002, in the tribal predominant hard-core districts of the state. In these states, some 200 districts contributed most to the burden of the disease. Due to the limited capacity of the health infrastructure, detailed information on the patients from the primary health care centers (PHCs) was not included in the reporting system. [Table 1]
Table 1.
Comparative Malaria situation in 1995 and 2007[5]
Experience from EMCP demonstrated a wide variability in the implementation capacity and resources between the states. States such as Maharashtra, Gujarat, and Andhra Pradesh, had a more established health infrastructure and significant financing from their state governments. Implementation in these states took off rapidly and the impact was dramatic. The burden of malaria dropped drastically during the project period. In contrast, the infrastructure and financing in states like Orissa, Jharkand, and Chhattisgarh were less well-established, implementation was slow or nonexistent until aggressive TA was provided by the National Program.
Targeting areas with the highest disease burden and vulnerable populations (i.e., tribal populations) was critical to the success of EMCP. The selection of the blocks to be included in the project was based on: (i) API of more than 2 for the past three years; (ii) P. falciparum more than 30% of the total malaria cases; (iii) 25% of the PHC population had to be tribal; and (iv) reported deaths due to malaria. In addition, states with low performance with high burden, such as Orissa and Jharkhand, were given greater attention and supervision.
India had spent up to 25% of its health budget on malaria control from 1977-1997, and starting in 1997, India planned to spend $40 million on malaria control, a 60% increase from the previous year. This expenditure was part of a five-year program aimed to target 100 districts where 80% of all P. falciparum cases occurred, 70 - 80% of the malaria control money in India is spent on insecticides.[5]
Decentralizing implementation support also permitted the National Program to focus on their technical support to those states and districts where implementation progress was slow (e.g., Orissa). In spite of all these inputs, the outcome in terms of malaria morbidity and mortality was not as drastic as expected.
CONCLUSION
The success of the Public Health Program is dependent more on project Implementation, management, monitoring, and evaluation of project activities, than the volume of financial resource allocation. Although enormous resources were given under the EMCP project, the need of the hour was optimum utilization of the resources. Operational issues in the field need to be addressed and concurrently strategies that are in compliance with the local challenges need to be adopted. Studies toward costing, evaluation, and impact assessment of the components are required.
Footnotes
Source of Support: WHO-India Regional office, India
Conflict of Interest: None declared
REFERENCES
- 1.WHO-SEARO Estimation of Malaria Disease burden in India. Report of an Informal Consultative Meeting New Delhi, India SEA-MAL-256 Distribution: Limited. 2007. Nov 21-23, http://203.90.70.117/PDS_DOCS/B3210.pdf .
- 2.Enhanced Malaria Control Project (EMCP) http://nihfw.org/NDC/DocumentationServices/NationalHealthProgramme/nationalanti-malariaprogramme.html .
- 3. http://www.worldbank.org.in/wbsite/external/countries/southasiaext/indiaextn/0,contentMDK:20469057~menuPK:295605~pagePK:141137~piPK:141127~theSitePK:295584,00.html .
- 4. http://www.mrcindia.org/rourkela.htm .
- 5. http://www.brown.edu/Research/EnvStudies_Theses/full9900/creid/malaria_in_india.htm .


