Abstract
Background:
Recent WHO guidelines recommended a universal “test and treat” strategy for malaria mainly by use of the rapid diagnostic test (RDT) in all areas. There are concerns about RDT that use the antigen histidine-rich protein2 (HRP2) to detect Plasmodium falciparum, because infection can persist after effective treatment.
Aim:
The aim of this paper is to describe the accuracy of the first response (HRP2)-RDT compared with malaria microscopy used for guiding the field treatment of patients in an outbreak situation in the Al-Rahabah area in Al-Rydah district in Hadramout/Yemen.
Materials and Methods:
An ad hoc cross sectional survey of all febrile patients in the affected area was conducted in May 2011. The field team was developed including the case management group and the entomology group. The group of case management prepared their plan based on “test and treat” strategy by using First Response Malaria Antigen HRP2 rapid diagnostic test for falciparum malaria, artemsinin-based combination therapy (ACT) according to the national policy of anti-malaria drugs in Yemen were supplied to treat those who were found to be RDT positive in the field; also blood smear films were taken from every patient with fever in order to validate the use of the RDT in the field. Blood film slides prepared and read by skilled lab technicians, the fourth reading was done by one lab expert in the malaria referral lab.
Results:
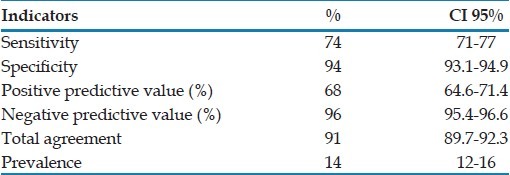
The accuracy parameters of HRP2 compared with microscopy are: Sensitivity (74%), specificity (94%). The positive predictive value is 68% and the negative predictive value is 96%. Total agreement is 148/162 (93%) and the overall prevalence is 14%. All the positive malaria cases were of P. falciparum either coming from RDT or microscopy.
Conclusions:
HRP2–rapid test is an acceptable test as a guide for field treatment in an outbreak situation where prompt response is indicated. Good prepared blood film slides should be used as it is feasible to evaluate the accuracy of RDTs as a quality control tool.
KEY WORDS: Malaria, rapid diagnostic test, Yemen
INTRODUCTION
Malaria management policies currently recommended that the treatment should only be administered after laboratory confirmation. Where microscopy is not available, rapid diagnostic tests (RDTs) are the usual alternative.[1] Recent WHO guidelines recommended application of the universal “test and treat” strategy for malaria mainly by use of the RDT in all areas.[2] A RDT needs less expertise and short time that give it superiority for using in an outbreak investigation so it can be used to treat patients as quick as possible in remote areas. There are also concerns about RDTs that use the antigen histidine-rich protein2 (HRP2) to detect Plasmodium falciparum, because infection can persist after effective treatment.[3]
A local outbreak of malaria was reported from Al-Rahabah area in Al-Rydah district of Hadramout governorate of Yemen in April-May 2011. The population (about 5000) in this area is tribal and nomadic, they are mobilizing dispersed groups, and no health services are available. The first notification for the malaria occurrence in the area was reported in April 2011 where private clinics and laboratories in the neighboring sub-district reported to malaria control program that all the new malaria cases where diagnosed and treated last month (April 2011) were coming from the Al-Rahabah area. The malaria control program in Hadramout region prepared a team to investigate the outbreak from epidemiological and entomological perspectives, taking into consideration community expectations and concerns about treatment of the sick persons and preventive measures required.
The aim of this paper is to describe the accuracy of the first response (HRP2)-RDT compared with malaria microscopy used for guiding the field treatment of patients in an outbreak situation.
MATERIALS AND METHODS
An ad hoc cross-sectional survey of all febrile patients in the affected area (Al-Rahabah village) in Al-Rydah district was conducted in May 2011. Al-Rydah district is located at 150 km east to Mukalla city (capital of Hadramout) where the regional office of malaria control program. The field team was developed including the case management group and the entomology group, constituting of one epidemiologist, one general practitioner and one medical assistant and three skilled medical laboratory technicians. The case management group prepared their plan based on “test and treat” strategy by using First Response Malaria Antigen HRP2 RDT for falciparum malaria, artemsinin-based combination therapy (ACT) according to the national policy of anti-malaria drugs in Yemen. In the field, blood samples collected from febrile patients were tested for malaria parasites using First Response® Malaria Ag. P. falciparum (HRP2) produced by Premier Medical Corporation Ltd (India); the provided information in the instruction guideline indicated sensitivity of 95% and specificity of 99.5% compared with malaria microscopy.[4] The test uses approximately 5 μl of blood and is readable after 15 min following the manufacturer's instructions. Participants with positive RDT results were offered immediate treatment according to national guidelines and a standardized questionnaire was filled by the health personnel. In order to validate the use of RDT in the field, duplicate thick blood slides for each participant were prepared and stained with Giemsa according to standard protocol, blood for thick smear and RDT were collected from the same finger-prick. Each film was examined by the medical laboratory technicians and graded as positive (asexual malaria parasites seen) or negative (no malaria parasites seen) based on the inspection of 200 fields of the thick smear. We took a fourth reading by expert in the malaria referral laboratory as a final result who was blinded to the diagnosis of the first slide-reader.
Statistical analysis
Frequencies and percentages and 95% confidence interval (CI 95%) were used to calculate sensitivity, specificity, and positive predictive value and negative predictive value.
Ethical consideration
Verbal informed consents were obtained from patients; the study is part of an outbreak investigation and control which is agreed by the local health authority. Malaria control program (Hadramout region) funded and approved this work.
RESULTS
A total of 162 patients were investigated, out of them, 25 being RDT positive and 23 being positive by microscopy. The accuracy parameters of HRP2 compared with microscopy are: Sensitivity (74%), specificity (94%). The positive predictive value is 68% and the negative predictive value is 96%. Total agreement is 148/162 (91%) and the overall prevalence is 14% [Table 1]. All the positive malaria cases were of P. falciparum either coming from RDT or microscopy.
Table 1.
Sensitivity, specificity and predictive values of rapid diagnostic test (HRP2-RDT) compared with slide microscopy, Al-Rahabah outbreak, 2011
DISCUSSION
HRP2-based malaria RDTs have shown high sensitivity and specificity for detecting P. falciparum malaria in a variety of study settings but they are susceptible to heat and humidity and variation in individual performance,[5] this is the case in the study area where investigation done on May 2011, the month of high temperature (about 40°C) and humidity (more than 70%).
It was reported elsewhere that sensitivity of RDT increased with increasing parasite density[5,6] and it was varied from low sensitivity (64.8%)[7] to high sensitivity (97.5%);[5] in this study, the sensitivity of HRP2-RDT was 74%, it is acceptable for field diagnosis and based on a good blood film preparation; the explanation behind low sensitivity are that patients with low parasitemia could not be detected taking into consideration the environmental factors of high temperature and humidity.
High specificity was reported in some studies[6,8,9] but one study reported low specificity of HRP2-RDT for diagnosis of falciparum malaria in children[5] and another study about all age groups;[7] in this study, high specificity was reported (94%). Although Singh et al. reported low specificity of HRP2 (69.9%) but it has clear advantages over other types of RDTs.[9]
Low-predictive value are positive due to high false positive tests (32%); false positive results are of HRP2-RDT because this antigen can persist after effective treatment.[3,10] In general, total agreement (91%) was acceptable for using this test in conditions like the study area.
Low prevalence of malaria characterized the Al-Rydah district and Hadramout region where only 500 cases reported during 2010 in the governorate with a population of 1,200,000 persons (annual incidence of <1 per 1000) and prevalence of less than 1%.[11] In this study; although there was a low prevalence of 14%, it was considered as an outbreak. A diagnostic test will be relevant if the prevalence in the population is low.[2]
CONCLUSIONS
HRP2-rapid diagnostic test is an acceptable test as a guide for field treatment in an outbreak situation where prompt response is indicated. Good prepared blood film's slides should be used as it is feasible to evaluate the accuracy of RDTs as a quality control tool.
ACKNOWLEDGEMENT
The authors express great thanks to Dr. Anisa Saggaf Albiti (Hematologist in Al-Gomhoryah teaching hospital in Aden/Yemen) for her efforts in revising the text and gave valuable comments.
Footnotes
Source of Support: This investigation was supported by the National Malaria Control Program (Hadramout Region) in Yemen.
Conflict of Interest: There is no conflict of interest
REFERENCES
- 1.Bisoffi Z, Sirima SB, Menten J, Pattaro C, Angheben A, Gobbi F, et al. Accuracy of a rapid diagnostic test on the diagnosis of malaria infection and of malaria-attributable fever during low and high transmission season in Burkina Faso. Malar J. 2010;9:192. doi: 10.1186/1475-2875-9-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Graz B, Willcox M, Szeless T, Rougemont A. “Test and Treat” or presumptive treatment for malaria in high transmission situations? A reflection on the latest WHO guidelines. Malar J. 2011;10:136. doi: 10.1186/1475-2875-10-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kyabayinze DJ, Tibenderana JK, Odong GW, Rwakimari JB, Counihan H. Operational accuracy and comparative persistent antigenicity of HRP2 rapid diagnostic tests for Plasmodium falciparum malaria in a hyperendemic region of Uganda. Malar J. 2008;7:221. doi: 10.1186/1475-2875-7-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Premier Medical Corporation Ltd. First Response Malaria Antigen, P. falciparum (HRP2) card test: Instruction for use. India. [Last accessed on 2011 Jul 10]. Available from: http://www.premiermedcorp.com/rapidtests.html .
- 5.Mtove G, Nadjm B, Amos B, Hendriksen IC, Muro F, Reyburn H. Use of an HRP2-based rapid diagnostic test to guide treatment of children admitted to hospital in a malaria-endemic area of north-east Tanzania. Trop Med Int Health. 2011;16:545–50. doi: 10.1111/j.1365-3156.2011.02737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMorrow Ml, Masanja MI, Abdulla SM, Kahigwa E, Kachur SP. Challenges in routine implementation and quality control of rapid diagnostic tests for malaria–Rufiji District, Tanzania. Am J Trop Med Hyg. 2008;79:385–90. [PMC free article] [PubMed] [Google Scholar]
- 7.McMorrow Ml, Masanja MI, Kahigwa E, Abdulla SM, Kachur SP. Quality assurance of rapid diagnostic tests for in routine patient care in rural Tanzania. Am J Trop Med Hyg. 2010;82:151–5. doi: 10.4269/ajtmh.2010.09-0440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Batwala V, Magnussen P, Nuwaha F. Are rapid diagnostic tests more accurate in diagnosis of Plasmodium falciparum malaria compared to microscopy at rural health centers? Malar J. 2010;9:349. doi: 10.1186/1475-2875-9-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh N, Shukla MM, Shukla MK, Mehra RK, Sharma S, Bharti PK, et al. Field and laboratory comparative evaluation of rapid malaria diagnostic tests versus traditional and molecular techniques in India. Malar J. 2010;9:191. doi: 10.1186/1475-2875-9-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osman MM, Nour BY, Sedig MF, De Bes L, Babikir AM, Mohamedani AA, et al. Informed decision-making before changing to RDT: A comparison of microscopy, rapid diagnostic test and molecular techniques for the diagnosis and identification of malaria parasites in Kassala, eastern Sudan. Trop Med Int Health. 2010;15:1442–8. doi: 10.1111/j.1365-3156.2010.02659.x. [DOI] [PubMed] [Google Scholar]
- 11.Malaria control program-Hadramout Region/Yemen. The annual report. 2010 [Google Scholar]


