Abstract
Background:
Complicated falciparum malaria remains a major cause of morbidity and mortality worldwide. Plasmodium falciparum malaria is a syndrome and a disease of protean clinical manifestations. All cases of falciparum malaria are potentially severe and life threatening, especially when managed inappropriately.
Aim:
The aim of the present study is to study clinical presentation and complications of patients with complicated P. falciparum malaria and its outcome.
Settings and Design:
This was retrospective observational study, conducted at tertiary care center in western Maharashtra from January 2011 to December 2011.
Materials and Methods:
Total 47 patients fulfilling criterion of complicated malaria due to P. falciparum who presented with fever having positive trophozoites of P. falciparum in blood smear were included in this study. Statistical analysis was done by EPI Info 6 statistical software.
Results and Conclusion:
A total 47 patients had smear positive complicated P. falciparum malaria with 39 were male and 8 were female patients. Total three (6.38%) patients had hypoglycemia at the time of admission. Total 29 (61.70%) patients had jaundice of which 20 were with anemia. Total 22 (46.80%) had anemia of which 20 were with jaundice. Total 6 (12.76%) had cerebral malaria, 6 (12.76%) had acute renal failure (ARF), 5 (10.63%) had acute respiratory distress syndrome (ARDS) and 1 (2.12%) had thrombocytopenia. Total 26 patients had single complication in the form of cerebral malaria 6 (12.76%), jaundice 9 (19.14%), ARF 5 (10.63%), ARDS 4 (8.51%) and anemia 2 (4.25%). Total 20 patients had two complications in the form of jaundice with anemia 20 (42.55%). One (2.12%) patient had four complications in the form of cerebral malaria with ARF with ARDS with thrombocytopenia with 100% mortality. Overall case fatality rate was 10.63% (5/47). The case fatality rate for isolated ARDS was 50% (2/4), with ARF was 20% (1/5) and with cerebral malaria it was 16.66% (1/6). Case fatality rate was highest in patients with ARDS compared to ARF and cerebral malaria with ‘P’ = 0.0221.
Conclusions:
In present study most common presentation was jaundice and anemia. Cerebral malaria, ARF and ARDS were uncommon presentation. Overall case fatality rate of complicated P. falciparum malaria was 10.63%. The case fatality rate was highest with multi-organ dysfunction (100%). This study highlights the significant burden of P. falciparum complicated malaria with isolated complication like ARDS with high mortality rate of 50% in present population.
KEY WORDS: Complicated falciparum malaria, acute respiratory distress syndrome, acute renal failure, multi-organ dysfunction, cerebral malaria
INTRODUCTION
Of the four species of malarial parasites that commonly cause infection in man, Plasmodium falciparum is responsible for virtually all the severe cases and deaths. The considerable mortality and morbidity in falciparum malaria is due to its protean manifestation, multi-organ involvement and delay in diagnosis and failure of administration of treatment promptly.[1,2] All cases of falciparum malaria are potentially severe and life threatening medical emergency. Malaria must be distinguished from other febrile illnesses including viral illnesses (such as dengue fever and influenza), typhoid, brucellosis, respiratory and urinary tract infections. The acute coma of cerebral malaria must be distinguished from viral encephalitis (herpes simplex, human immunodeficiency virus and enteroviral), bacterial meningoencephalitis (pyogenic and rarely tuberculous) and fungal meningoencephalitis, brain abscess, heat stroke, cerebrovascular events, hypertensive encephalopathy, intoxications with drugs and poisons as well as other causes of coma.[1,2] The renal failure of malaria must be distinguished from renal impairment due to other febrile illnesses such as leptospirosis. The jaundice and hepatomegaly of malaria should not be confused with that of viral hepatitis (hepatitis A virus, hepatitis B virus, hepatitis C virus), leptospirosis, drug-induced diseases and alcohol. Severe and complicated malaria is characterized by multiorgan involvement including ARF, acute lung injury (ALI) and ARDS. This study was conducted to review the complications of P. falciparum malaria at a tertiary care centre.
MATERIALS AND METHODS
This study was a retrospective observational study on complicated falciparum malaria conducted at Krishna institute of medical sciences Karad. This study is approved by ethical committee of Krishna institute of medical sciences, Karad. Adult patients with age >18 years with smear positive falciparum malaria with various complications admitted to medical wards and intensive care unit (ICU) from January 2011 to December 2011 were included in this study. A total 47 patients with positive blood smear for P. falciparum malaria were included in present study with complicated P. falciparum malaria. The coexistence of other diseases like pneumonia, urinary tract infection, leptospirosis, H1N1 and viral hepatitis and mixed malarial infections were excluded from the present study by appropriate investigations.
Peripheral blood smears were collected on admission for Giemsa staining and subsequently every 12 and 48 hours to assess parasitemia. Blood was collected for estimation of glucose, urea, creatinine, serum electrolytes, liver function tests, haemoglobin, platelet count, total leukocyte count and prothrombin time (PT). Arterial blood gas analysis in patients with respiratory distress was done in 11 patients. Chest radiograph and electrocardiogram was done as and when needed for diagnosis of respiratory distress and pulmonary edema [Figure 1]. The diagnosis of malaria was made with detection of asexual form of P. falciparum from Giemsa stained peripheral blood smear.[2] In a patient with P. falciparum asexual parasitaemia and no other obvious cause of symptoms, the presence of one or more of the following clinical or laboratory features classifies the patient as suffering from severe malaria.
Figure 1.
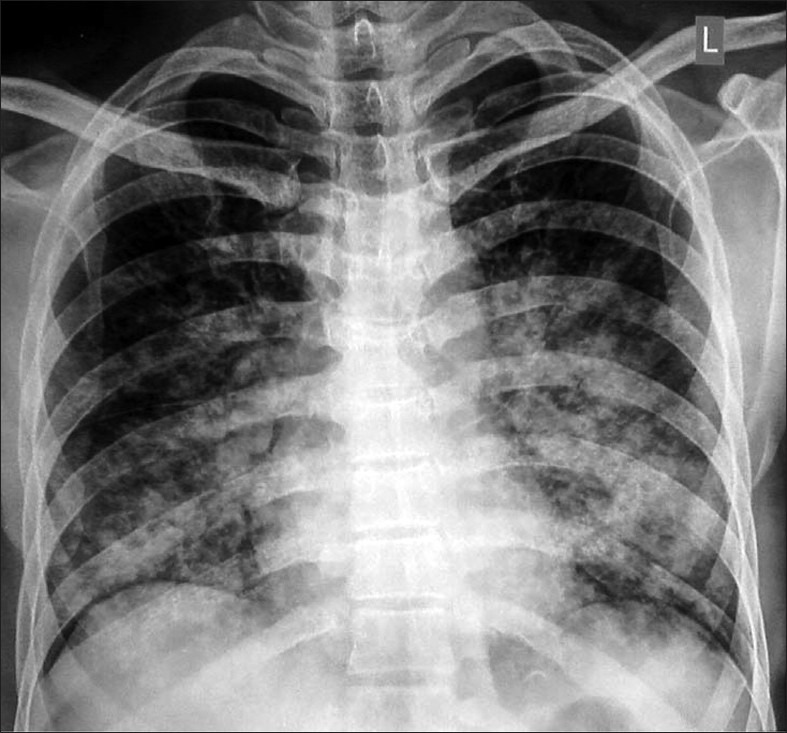
Chest radiograph showing suggestive of ARDS in a patient with complicated falciparum malaria
Severe complicated malaria was diagnosed according to the guidelines of World Health Organization. Cerebral malaria was diagnosed when a patient had unarousable coma using Glasgow Coma Scale with exclusion of other etiologies with multiple convulsions – more than two episodes in 24 hours, renal failure, jaundice, hypoglycaemia and severe anemia were diagnosed when serum creatinine was more than 2.0 mg/dl, s. bilirubin was more than 2.0 mg/dl, random blood glucose was less than 60 mg/ dl and hemoglobin was less than 7.0 gm/dl, respectively. The metabolic acidosis was labeled if plasma bicarbonate <15 mmol/l. Circulatory collapse (hypotension) had been defined as systolic blood pressure (BP) <90 or a fall in BP of more than 40 mm of Hg unresponsive to fluid administration. Respiratory distress was defined when patient had tachypnoea with or without pulmonary edema (radiological).[3,4]
Patients with complication were grouped under single complication, two complications, three complications and multiple complications. Onset time, resolution time, duration, and progression of complications as well as duration of hospital stay were determined. The outcome was binary, i.e., either recovery or death. Airway was secured in unconscious patient, intravenous (IV) infusion of dextrose normal saline was started with central venous pressure (CVP) monitoring. In unconscious patients, lumbar puncture and cerebrospinal fluid (CSF) study was done to exclude bacterial/viral meningitis. Patients were examined and assessed frequently until full recovery or death. All patients were treated with intravenous quinine dihydrochloride at a loading dose of 20 mg/ kg administered over 3 h. Subsequent dose of 10 mg/ kg administered over 2 h every 8 h in a 10% dextrose solution until the patient could take medication orally. Treatment was continued for 7–10 days. Complications such as anemia, hypoglycaemia, convulsion, renal failure, jaundice, respiratory failure and circulatory collapse were treated according to the standard protocol. The data were pooled, computerized, and analyzed by evaluation version of EPI Info. 6 [(Epi Info is public domain statistical software for epidemiology developed by Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia (USA)]. Patient characteristics and the outcome of interest and relative risk and their corresponding 95% confidence interval were calculated. Prevalence rates were given in percentage. Various numbers are given as mean and standard deviation±1 SD. For continuous variable, mean values were compared using two sample ‘t’ tests for independent samples. Categorical variables have been compared by using χ2 (Chi-square) test. The probability <0.05 was considered as significant.
RESULTS
A total 47 smear positive patients were included in present study with criterion fulfilling complicated P. falciparum malaria of both gender. Data was collected for this retrospective study from medical records of the institute. Total 39 (82.97%) were males and 8 (17.02%) were female patients with mean age of 29±11 years and 31±12 years for females. Out of total 47 patients, 27 (57.44%) patients were critically ill and treated in ICU and remaining 20 (42.55%) were managed in medical wards. All 47 (100%) patient had fever as a presenting complaint at the time of admission. Vomiting was present in 9 (19.14%) patients. Total 4 (8.5%) patients were unconscious and 4 (5.47%) patients had generalized tonic clonic convulsions. Three (6.38%) patients had hypoglycemia at the time of admission. Total 29 (61.70%) patients had jaundice. Total 4 (8.5%) patients had hypotension. Oliguria was present in 6 (12.76%) patients as a presenting feature. Breathlessness and cough was present in 5 (10.63%) patients with low SpO2. One (2.12%) patient had bleeding tendency in the form of malena and hematemesis. Splenomegaly was present in 27 (57.44%) patients and hepatomegaly was present in 25 (53.19%) patients. Total 20 (42.55%) patients had pallor [Table 1 and Figure 2]. The mean and standard deviation (±1) of laboratory parameters is shown in Table 2.
Table 1.
Clinical profile of complicated malaria
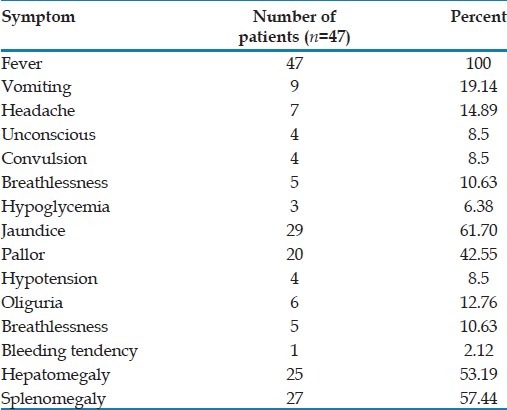
Figure 2.
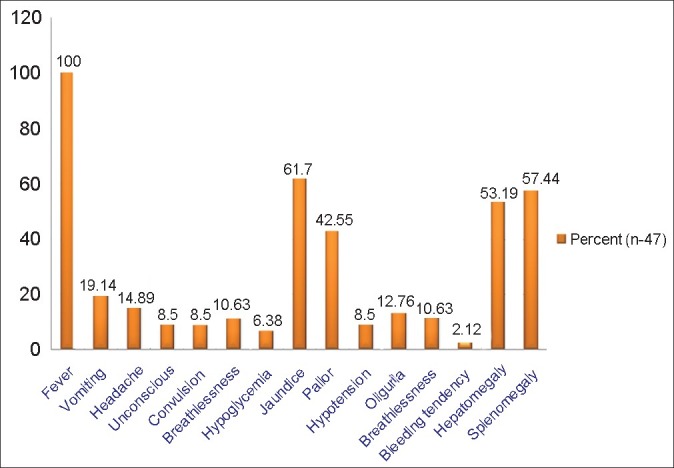
Clinical profile of complicated P. falciparum malaria
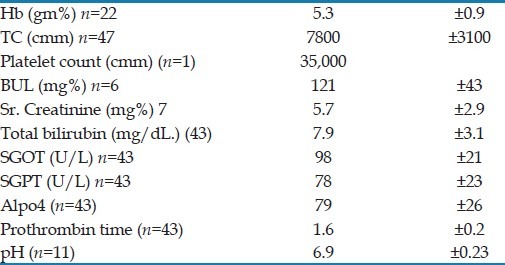
Table 2.
Mean and standard deviation of laboratory parameters
Total 20 patients had jaundice with anemia. Total 9 (58.90%) patients had isolated jaundice, 2 (4.25%) had anemia, 6 (12.76%) had cerebral malaria. Total 6 (12.76%) had ARF, 5 (10.63%) had ALI/ARDS and one (2.12%) had thrombocytopenia. In present study most common presentation was with jaundice and anemia while ARF and ARDS were uncommon presentation with poor outcome and high mortality. Total 28 patients had single complication in the form of cerebral malaria 6(19.17%), jaundice 9 (20.54%), 4 (8.51%) had ARDS, 5 (10.63%) had ARF and anemia 2 (21.91%). Total 20 (42.55%) patients had two complications in the form of jaundice with anemia. One (2.12%) patient had four complications in the form of cerebral malaria with ARF, ARDS and thrombocytopenia. Patient with four complications succumbed. Total 5 (10.63%) had isolated cerebral malaria without other organ involvement. A total of 9 patients required blood transfusions for severe anemia. At the time of admission total 4 (8.51%) patients had shock which was treated by fluid resuscitation and inotropic agent support under CVP monitoring. A total of six patients developed ARF required renal replacement therapy in the form of hemodialysis (7±3 cycles). A total of 11 patients had acidic pH of which 6 (12.76%) had metabolic acidosis and 5 (10.63%) had respiratory acidosis which was corrected by hemodialysis, artificial ventilator and/or sodium bicarbonate supplementation. Out of 47 patients admitted and treated for complicated P. falciparum malaria, 42 (89.36%) patients were discharged in ambulatory state after recovery from complications and parasitic clearance [Table 3 and Figure 3]. Six patient had oliguric renal failure and all of them required hemodialysis of which 5 (83.33%) recovered while one (16.66%) died. Five patients had pulmonary involvement in the form of ARDS of which all required artificial ventilator of which 3 (60%) succumbed [Table 4].
Table 3.
Clinical presentation and complications of falciparum malaria
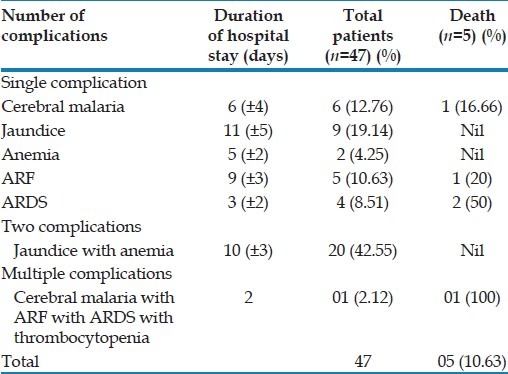
Figure 3.
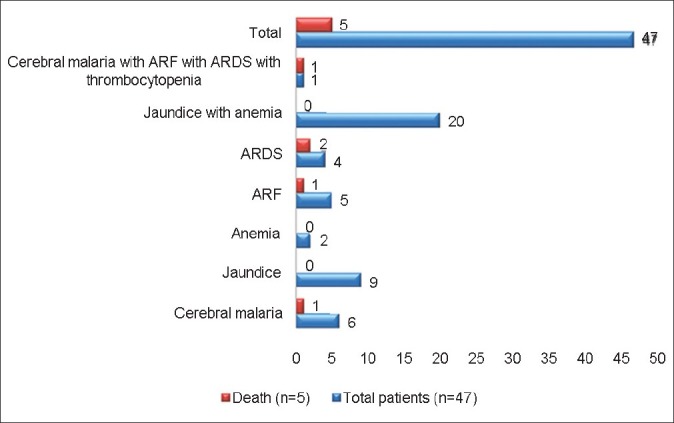
Clinical syndrome of complicated P. falciparum malaria
Table 4.
Comparison of case fatality rate amongst the complications of falciparum malaria
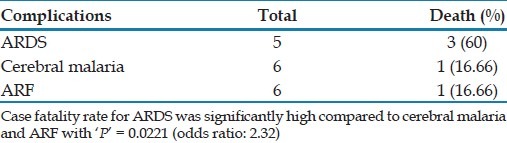
Out of total 6 patients with cerebral malaria, 1 (16.66%) succumbed. Four patients developed isolated ARDS of which two (50%) succumbed. Five patients developed isolated ARF of which one (20%) succumbed. One (2.12%) patient had four complications in the form of cerebral malaria with ARF with ARDS with thrombocytopenia with 100% mortality. Case fatality rate was significantly high with ARDS compared to cerebral malaria and ARF with ‘P’ = 0.0221 (odds ratio: 2.32). [Table 4].
A total of five patients succumbed with complicated P. falciparum malaria with case fatality rate of 10.63%. In univariate analysis overall case fatality rate was highest with pulmonary involvement (ARDS) compared with other complications which was statistically significant (‘P’=0.0221). The case fatality rate with ARDS was 50% (2/4), with ARF was 20% (1/5) and with cerebral malaria it was 16.66% (1/6). Patients presented with hypotension had more incidence of ARF (4/6) compared to with normotension. Multi-organ failure associated with 100% mortality.
DISCUSSION
In present study most common presentation was jaundice with anemia. ARF and ARDS were less common presentation with poor prognosis and significantly high mortality. A total of 26 (55.31%) patients had single complication. 20 (42.55%) patients had two complications in the form of jaundice with anemia. One (2.12%) patient had four complications in the form of cerebral malaria with ARF with ARDS with thrombocytopenia with 100% mortality. Five patients died with complicated P. falciparum malaria with case fatality rate of 10.63%. Cerebral malaria, ARF, ARDS, and thrombocytopenia are the less common presenting features in present study. Overall case fatality rate was highest with multi-organ dysfunction compared to single complication. Case fatality rate was highest in patients with ARDS compared to ARF, cerebral malaria with ‘P’=0.0221. We compared our results with various studies. Prakash et al.[5] in their study quoted the mortality rate of 30.8% in complicated malaria with ARF which is comparable with present study in which mortality rate with ARF was 16. 66%. Mishra et al.,[6] in their study stated that the case-fatality rate due to severe malaria is 10%–15% in spite of therapy but it increases in the presence of renal failure or respiratory distress (pulmonary edema or ARDS). In present study overall case fatality rate was (10.63%) and in patients with multi-organ dysfunction it was 100%. Kochar et al.,[7] in their study reported the overall mortality of 11.09%; similarly in our study mortality rate was 10.63%. Morality was highest in ARDS (81.25%) which is comparable with our study where case fatality rate with multi-organ dysfunction was 60% with ARDS. Mishra et al.,[8] in their study in eastern India found that 175 (23%) of the cases were fatal, mortality being particularly high (59%) among those with multiorgan failure. These findings are comparable with present study in which 1 (2.12%) patient had multiple complications in the form of ARF with ARDS with thrombocytopenia with 1 (100%) death. Total 5 patients died with complicated P. falciparum malaria with case fatality rate of 10.63%. The case fatality rate with ARDS was 60% (3/5), with ARF was 16.66% (1/6) and with cerebral malaria it was 16.66% (1/6). Case fatality rate was highest in patients with ARDS compared to ARF, cerebral malaria, jaundice and anemia with ‘P’<0.0221. Jain et al.,[9] in their study found that, ARF was present in 22% and respiratory distress was seen in 22% patients, Mortality was high among adults with multiple organ failures. Overall case fatality rate was 21%. These findings are similar to our study where 5 (10.63%) patients had ARDS and 6 (12.76%) had ARF. Chishti et al.,[10] found that 90.63% of patients with falciparum malaria developed one or more complications. The most common complication is anemia accounting for 76.56% and total 12.5% died due to development of multiple complications. Similarly in our study 22 (46.80%) patients had anemia of which 20 (42.55%) had anemia with jaundice with mortality of 10.63%. Similarly Mohanty et al.,[11] in their study of P. falciparum malaria patients quoted mortality of 13.65%. Prakash J et al.,[12] reported P. falciparum with ARF in 79.61% of cases with mortality of 15.7%. Kanodia KV et al.,[13] reported P. falciparum associated ARF in which 64% of the patients recovered completely. Similarly in our study all 6 (12.76%) patients required hemodialysis of which 4 (66.66%) recovered near total and 2 (33.33%) succumbed. Maheshwari A et al.,[14] reported overall mortality rate of 18.5% and with multi-organ failure it was 33.3%. Kochar et al.,[15] in their prospective study in Bikaner, Rajasthan (northwest India) 2001 found that jaundice (58.85%) followed by severe anemia (26.04%), shock (10.94%), cerebral malaria (10.94%), renal failure (6.25%) and ARDS (2.08%) were the complications seen in falciparum malaria. Similarly, the important cause of mortality in 2001 was multiple organ dysfunctions (71.10%) with predominant presentation of jaundice and renal failure. These findings are comparable with present study. Eryüksel et al.,[16] Mohan et al.,[17] and Manyindo et al,[18] reported P. falciparum associated pulmonary complications in the form of ARDS with high mortality rate similar to present study. Eiam-Ong S et al.,[19] stated renal involvement in P. falciparum similar to our study. This study highlights the ARDS and ARF are the main factors predicting mortality in complicated falciparum malaria.
CONCLUSION
To conclude, unusual early isolated renal and pulmonary manifestations were the presenting feature of complicated P. falciparum malaria with high mortality as was seen in present study. The mortality rate was significantly high with multi-organ dysfunction. All the patients with ARF and ARDS had shock as a presenting feature. Multi-organ dysfunction had high case fatality rate (100%). Mainstay of treatment consists of appropriate antimalarial drug therapy, fluid replacement, early institution of artificial ventilation and renal replacement therapy. Invariably all the patients with ARF required daily dialysis. Severe ARF, and ALI/ARDS were poor prognostic factors in patients with P. falciparum infection in present study. The patients with ARDS should be managed in an ICU. Careful attention must be paid to hemodynamic stabilization and optimizing fluid balance. ARDS in malaria is a disease with a high mortality, and early diagnosis, institution of specific antimalarial treatment and assisted ventilation can be life-saving. This study confirms presence of complicated falciparum malaria with multi-organ dysfunction in western Maharashtra. P. falciparum malaria is an important treatable cause of ALI or ARDS and ARF in study population. P. falciparum malaria should be considered as an etiological agent for ARDS and ARF with multiple organ dysfunction syndrome in a clinical scenario of febrile illness.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Pasvol G. The treatment of complicated and severe malaria. Br Med Bull. 2005;75-76:29–47. doi: 10.1093/bmb/ldh059. [DOI] [PubMed] [Google Scholar]
- 2.Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 2005;434:214–7. doi: 10.1038/nature03342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster. Trans R Soc Trop Med Hyg. 2000;94(Suppl 1):S1–90. [PubMed] [Google Scholar]
- 4.World Health Organization. World malaria situation in 1992 Part I. Wkly Epidemiol Rec. 1994;69:309–14. [PubMed] [Google Scholar]
- 5.Prakash J, Singh AK, Kumar NS, Saxena RK. ARF in Plasmodium vivax malaria. J Assoc Physicians India. 2003;51:265–7. [PubMed] [Google Scholar]
- 6.Mishra SK, Mohanty S, Satpathy SK, Mohapatra DN. Cerebral malaria in adults- a description of 526 cases admitted to Ispat General Hospital in Rourkela, India. Ann Trop Med Parasitol. 2007;101:187–93. doi: 10.1179/136485907X157004. [DOI] [PubMed] [Google Scholar]
- 7.Kochar D, Kumawat BL, Karan S, Kochar SK, Agarwal RP. Severe and complicated malaria in Bikaner (Rajasthan), western India. Southeast Asian J Trop Med Public Health. 1997;28:259–67. [PubMed] [Google Scholar]
- 8.Mishra SK, Mahanta KC, Mohanty S. Malaria associated ARF–experience from Rourkela, eastern India. (654).J Indian Med Assoc. 2008;106:640–2. [PubMed] [Google Scholar]
- 9.Jain V, Nagpal AC, Joel PK, Shukla M, Singh MP, Gupta RB, et al. Burden of cerebral malaria in central India (2004-2007) Am J Trop Med Hyg. 2008;79:636–42. [PMC free article] [PubMed] [Google Scholar]
- 10.Chishti SA, Duidang L, Kasar A, Raman M, Luikham A. Severe falciparum malarial complications in Ukhrul, Manipur. J Indian Med Assoc. 2000;98:619–22. [PubMed] [Google Scholar]
- 11.Mohanty S, Mishra SK, Pati SS, Pattnaik J, Das BS. Complications and mortality patterns due to Plasmodium falciparum malaria in hospitalized adults and children, Rourkela, Orissa, India. Trans R Soc Trop Med Hyg. 2003;97:69–70. doi: 10.1016/s0035-9203(03)90027-7. [DOI] [PubMed] [Google Scholar]
- 12.Prakash J, Gupta A, Kumar O, Rout SB, Malhotra V, Srivastava PK. ARF in falciparum malaria—increasing prevalence in some areas of India—a need for awareness. Nephrol Dial Transplant. 1996;11:2414–6. doi: 10.1093/oxfordjournals.ndt.a027206. [DOI] [PubMed] [Google Scholar]
- 13.Kanodia KV, Shah PR, Vanikar AV, Kasat P, Gumber M, Trivedi HL. Malaria induced ARF: A single center experience. Saudi J Kidney Dis Transpl. 2010;21:1088–91. [PubMed] [Google Scholar]
- 14.Maheshwari A, Singh AK, Sinha DK, Tripathi K, Prakash J. Spectrum of renal disease in malaria. (146, 148).J Indian Med Assoc. 2004;102:143. passim. [PubMed] [Google Scholar]
- 15.Kochar DK, Kochar SK, Agrawal RP, Sabir M, Nayak KC, Agrawal TD, et al. The changing spectrum of severe falciparum malaria: A clinical study from Bikaner (northwest India) J Vector Borne Dis. 2006;43:104–8. [PubMed] [Google Scholar]
- 16.Eryüksel E, Gün D, Odabaşi Z, Karakurt S, Celikel T. Acute respiratory distress syndrome in Plasmodium falciparum malaria. Southeast Asian J Trop Med Public Health. 2009;40:1179–82. [PubMed] [Google Scholar]
- 17.Mohan A, Sharma SK, Bollineni S. Acute lung injury and acute respiratory distress syndrome in malaria. J Vector Borne Dis. 2008;45:179–93. [PubMed] [Google Scholar]
- 18.Manyindo N, Simo D, Arora S, Unegbu U, Oyiriaru D, Wills R. A case of successfully treated acute respiratory distress syndrome complicating Plasmodium falciparum malaria. J Natl Med Assoc. 2011;103:64–7. doi: 10.1016/s0027-9684(15)30247-9. [DOI] [PubMed] [Google Scholar]
- 19.Eiam-Ong S. Current knowledge in falciparum malaria-induced ARF. J Med Assoc Thai. 2002;85(Suppl 1):S16–24. [PubMed] [Google Scholar]


