Abstract
Background.
Physical activity (PA) appears to have a positive effect on physical function, however, studies have not examined multiple indices of physical function jointly nor have they conceptualized physical functioning as a state rather than a trait.
Methods.
About 424 men and women aged 70–89 were randomly assigned to complete a PA or a successful aging (SA) education program. Balance, gait speed, chair stand performance, grip strength, and time to complete the 400-m walk were assessed at baseline and at 6 and 12 months. Using hidden Markov model, empiric states of physical functioning were derived based on these performance measures of balance, strength, and mobility. Rates of gain and loss in physical function were compared between PA and SA.
Results.
Eight states of disability were identified and condensed into four clinically relevant states. State 1 represented mild disability with physical functioning, states 2 and 3 were considered intermediate states of disability, and state 4 severe disability. About 30.1% of all participants changed states at 6 months, 24.1% at 12 months, and 11.0% at both time points. The PA group was more likely to regain or sustain functioning and less likely to lose functioning when compared with SA. For example, PA participants were 20% more likely than the SA participants to remain in state 1.
Conclusion.
PA appears to have a favorable effect on the dynamics of physical functioning in older adults.
Key Words: Older adults, Physical activity, Randomized controlled trial, Physical functioning, Transitional states.
WITH more than 40 million people in the United States aged 65 and older (1), researchers have witnessed an unprecedented population shift. Clearly a priority for public health must be to ensure that older adults are able to maintain their independence as long as possible. Indeed, there is reason for alarm in that estimates from the Medicare Current Beneficiary Survey indicate that up to 47% of persons aged 65 and older have either mild limitation with mobility or more severe physical disability (1). Because physical function is central to the loss of mobility and activities of daily living that serve as core dimensions of physical disability (2,3), the goal of the current research is to examine how patterns in several common performance measures of physical function fluctuate across a period of 1 year as a function of older prefrail adults’ involvement in a physical activity (PA) intervention—the Lifestyle Intervention and Independence for Elders Pilot (LIFE-P) study (4).
Results from several large epidemiological studies and data from recent randomized clinical trials have provided convincing evidence that PA has a favorable effect on performance-based measures of physical function including those that assess balance (5), strength (6), and mobility (7). However, none of these studies have considered the possibility that physical functioning should be treated as a dynamic state, a conceptual position which posits that older adults’ transition in and out of different states of function across time. In addition, different components of function such as balance, strength, and mobility may have discrete patterns of change as functional decline progresses from mild to severe. This implies that physical disablement is inherently multivariate and that studying single outcomes in isolation ignores this inherent complexity.
The proposition that functional status is a dynamic state rather than static is not new. Almost 20 years ago, Verbrugge and colleagues (8) followed older persons after in-hospital treatment for chronic health conditions. They found that most people regained physical functioning in the first month after discharge, stabilized for several months, and then began to fluctuate and generally decline in the second year. They stated that disability outcomes “…are very dynamic over a year’s time for persons with serious chronic illness (p. 104).” In recent years, Gill and colleagues have provided much additional evidence to support this perspective. Using a prospective community cohort of persons more than 71 years old (n = 754), they recorded changes in disability status on a monthly basis. In 2004, Hardy and Gill (9) reported that over a median follow-up of 51 months, 56% of participants who initially could bathe, dress, walk inside the house, and transfer from a chair lost one or more of these abilities. Also, 81% of the newly impaired group eventually regained independence in these activities of daily livings with 57% maintaining these abilities for at least 6 months. On the other hand, whereas 60% of those participants who experienced disability for more than 3 months also recovered to an independent state, only a third of this group remained disability free for at least 6 months. Studying the same cohort, Gill and Kurland (10) showed that in the year before the study, prior to being classified as nondisabled, 55 participants had been disabled for a single month, 8 had been disabled for a single episode of 2 months, 18 had experienced chronic disability of more than 3 months, and 11 had some other pattern of short-term disability. A similar trend for dynamic changes in physical disability among older adults with knee pain was recently published by Rejeski and colleagues (11) using data from the Observational Arthritis Study in Seniors.
Given the dynamic nature of the disablement process in aging, the researchers’ objective is to describe the heterogeneity and patterns of change that occur among six objective indices of physical function across a period of 1 year among older adults in LIFE-P. The researchers will describe the relative probability of transitioning between states over time and examine whether an exercise intervention influences the probability of transitioning between states. Unlike other studies that used subjective criteria to classify individuals, in this study the states are directly determined from the data and represent clusters of participants with a similar functional profile within each cluster. The researchers hypothesize that the LIFE-P PA intervention will lower the incidence of declining profiles in physical function—balance, strength, and mobility—and increase the incidence of recovery from lost function as compared with the successful aging (SA) education treatment. It is important to note that this hypothesis was not prespecified as a part of LIFE-P.
There are several novel features of this study that build on previous LIFE-P publications and make a significant contribution to the literature on physical disability. First and most important, the researchers treat physical disablement as a multivariate construct, proposing that over time it is important to study “phenotypes” or patterns of change in multiple outcomes simultaneously. The researchers focus on objective indices of physical function, a core determinant of physical disablement, and consider both healthy and limited states of different functional domains concurrently. The reason for and value inherent to this approach can be gleaned by a simple example; two people can have the exact same score on the short physical performance battery (SPPB) yet have different phenotypes in strength, balance, and mobility. Second, the researchers provide specific information regarding transitions in physical function for both arms of the study for a period of 1 year, statistically testing the effects of these interventions on transitions in states or phenotypes, both positive and negative.
Methods
The LIFE Pilot Study
The study design for LIFE-P has been described previously (12). Participants were aged 70–89 years and able to complete a 400-m walk in less than 15 minutes. The study was conducted at four field centers (Cooper Institute, Stanford University, University of Pittsburgh, and Wake Forest University). Major exclusion criteria included presence of severe heart failure, uncontrolled angina, and other severe illnesses that might interfere with PA. All participants completed a 1-week behavioral run-in prior to random assignment to either a PA intervention or a SA education comparison intervention (“successful aging”). The PA intervention consisted of aerobic (walking), strength, balance, and flexibility exercises. The control group attended workshops on a variety of health topics relevant to older adults. See Pahor and colleagues (4) for a comprehensive description of the interventions. Written informed consent was obtained; the NIH and IRBs for all participating institutions approved the protocol and consent forms. Between May 2004 and February 2005, 424 participants were enrolled. At baseline and at 6 and 12 months, comprehensive standardized assessments were conducted by trained research staff masked to intervention assignment.
Data Collection
The researchers’ outcome measures in this study include the three components of the SPPB, time to complete the 400-m walk, and grip strength. The SPPB is a performance-based test that includes a usual pace 4-m walk, five repeated chair stands, and a test of balance.40 All three components of the SPPB are measured on a scale from 0 to 4. For balance, points are awarded based on ability to hold different positions. For the 4-m walk and chair stands, participants were timed and assigned points corresponding to the quartiles of participants tested in the Established Populations for the Epidemiologic Study of the Elderly project (13). For the 400-m walk, participants were asked to walk 10 laps of a 40-m course (20 m out, 20 m back) at their usual pace. Participants were allowed to stop and rest in a standing position for a maximum of 60 seconds per stop, but they were not allowed to sit. The time to walk 400-m was recorded with a stopwatch in seconds. Grip strength was measured using a Jamar handheld dynamometer (J.A. Preston Corp., Clifton, NJ) with the participant seated, elbow slightly flexed, wrist in a neutral position, and the interphalangeal joint of the index finger at 90°. The participant was instructed to squeeze the handle of the dynamometer with maximal effort for 3–5 seconds. Two trials on the left and right hands were assessed and the average of the stronger hand was used in these analyses. Besides the primary predictor of intervention status, other predictor variables include health conditions (eg, body mass index and disease status, see Table 1) and demographics variables (age, gender, race, education, marital status, and living arrangements).
Table 1.
Baseline Characteristics of LIFE-P Participants
| Characteristic | Physical Activity Group (n = 213) | Successful Aging Group (n = 211) | p Value* |
|---|---|---|---|
| Age, M ± SD | 76.5±4.2 | 77.0±4.3 | .24 |
| Race/ethnicity, n (%) | .87 | ||
| African American/black | 37 (17.4) | 40 (19.0) | |
| Caucasian/white | 160 (75.1) | 155 (73.5) | |
| Latino, Hispanic/Spanish | 10 (4.7) | 10 (4.7) | |
| Other/mixed | 6 (2.8) | 5 (2.4) | |
| Refused/missing | 0 (0.0) | 1 (0.5) | |
| Sex, n (%) | .89 | ||
| Female | 146 (68.5) | 146 (69.2) | |
| Male | 67 (31.5) | 65 (30.8) | |
| Smoking status, n (%) | .87 | ||
| Never | 174 (81.7) | 176 (83.4) | |
| Former | 32 (15.0) | 28 (13.3) | |
| Current | 7 (3.3) | 7 (3.3) | |
| Education, n (%) | .86 | ||
| <High school | 5 (2.3) | 6 (2.8) | |
| High school | 58 (27.2) | 58 (27.5) | |
| >High School | 142 (66.7) | 142 (67.3) | |
| Other/refused | 8 (3.8) | 5 (2.4) | |
| Marital status, n (%) | .65 | ||
| Married | 78 (36.6) | 89 (42.2) | |
| Divorced/separated | 37 (17.4) | 28 (13.3) | |
| Widowed | 86 (40.4) | 87 (41.2) | |
| Other | 12 (5.6) | 7 (3.3) | |
| Self-reported health, n (%) | .48 | ||
| Excellent | 10 (4.7) | 7 (3.3) | |
| Very good | 48 (22.5) | 63 (29.9) | |
| Good | 115 (54.0) | 105 (49.8) | |
| Fair | 35 (16.4) | 30 (14.2) | |
| Poor | 4 (1.9) | 3 (1.4) | |
| Do not know/refused | 1 (0.5) | 3 (1.4) | |
| Body mass index, m/kg2, M ± SD | 30.8±6.9 | 29.9±6.1 | .15 |
| Abdominal circumference, cm, M ± SD | 100.8±21.4 | 98.8±20.5 | .33 |
| Functional measures | |||
| Any activity of daily living difficulty, n (%) | 172 (80.8) | 175 (82.9) | .56 |
| Difficulty walking one quarter of a mile, n (%) | 13 (6.1) | 15 (7.1) | .68 |
| Difficulty walking 1 mile, n (%) | 82 (38.5) | 100 (47.4) | .06 |
| SPPB score, M ± SD | 7.6±1.5 | 7.5±1.4 | .43 |
| Balance, M ± SD | |||
| Gait speed, M ± SD | |||
| Chair stand, M ± SD | |||
| Grip strength in dominant hand, kg, M ± SD | 26.7±9.5 | 24.0±8.1 | .46 |
| 400-m Walk time (s) M ± SD | 492±114 | 492±114 | .75 |
Notes: LIFE-P = lifestyle interventions and independence for elders pilot study; M = mean; SD = standard deviation; SPPB = short physical performance battery.
*Continuous variables were analyzed using independent t tests; categorical variables were analyzed using chi-square.
Adapted from Katula JA, Kritchevsky SB, Guralnik JM, et al. (20).
Statistical Analysis
The basic tool for the statistical analysis was the hidden Markov model (HMM). Like the latent class model, HMM provides a structural analysis of participant profiles in terms of their responses to study outcomes. The HMM model also goes beyond the capacity of latent class models in allowing a longitudinal analysis of the patterns of change in disability. Applying HMM to the LIFE-P data set resulted in an empirically derived set of states for physical functioning, the number of which is determined by a goodness-of-fit criterion, the Bayesian information criterion. Each participant can be classified as a member of any one of the several states at any given time point and it is assumed that the number and structure of the states is constant across time. The Markov assumption in HMM states that transition probabilities from a state at time t to a state at time t + 1 only depend on the state at t and not on the history prior to time t. The probability of transitioning from one state to another can also be estimated from the data. The researchers’ strategy in assessing the effect of intervention on the dynamic between states is to first describe the transition probabilities by intervention status and then examine whether the intervention promotes gain or protects against loss in physical function. Furthermore, the researchers ordered the states and then analyzed the patterns of transition using the mixed effects generalized linear model (14,15). The analytic model is essentially an ordinal logistic regression equipped with a submodel of random effects that takes into account the fact that the transitions over time for the same individual are correlated events. Missing values were treated as missing at random. There was no observation that missed all measures of interest defined by the HMM. Under the missing at random assumption observations with partially missing values (<1%) were retained. The HMM was implemented in a specialized program written in MATLAB (Mathworks, Natick, MA) (16,17). The mixed effects generalized linear model was implemented using the program PROC GLIMMIX (SAS, Cary, NC).
Results
Baseline characteristics were similar for the two randomized groups (see Table 1). There were 424 observations available for the SPPB and the 400-m walk time at baseline and 408 for grip strength. At 6/12 months, the number of observations was 401/398 for the SPPB, 395/384 for the 400-m walk, and 365/376 for grip strength. The use of HMM resulted in eight empirically derived states; these eight states were condensed into four clinically relevant states: good physical functioning (state 1), mild deficits (states 2), moderate deficits (state 3), or severe deficits (state 4). Figure 1 provides a visual representation of these four states. The conditional distributions of the measures are normalized and then depicted in the form of a dot chart with a bar of length 2 SD centered at the mean (the dot). In interpreting these data, the reader should keep in mind that participants in LIFE-P could not have an SPPB score above 9 to be included in the trial although participants did score above 9 at follow-up assessments. For ease of interpretation, the time to complete the 400-m walk is multiplied by −1 so a higher number implies better mobility.
Figure 1.
Conditional probability profile of the four-state model. Legend: State 1 = good mobility; State 2 = mild deficits in physical function; State 3 = moderate deficits in physical function; State 4 = severe deficits in physical function; Dots represent means of the variables and bars indicate 95% confidence limits.
Persons in state 1, characterized as having good physical function, performed in the upper quartile on balance and mobility, but exhibited some relative loss in strength, albeit minimal. State 2 describes participants exhibiting mild deficits in physical functioning. They had a noticeable loss of balance with trends for decline in grip strength and 400-m walk time. State 3, characterized by moderate deficits in physical functioning, represents a profile in which people experience compromised performance on all five indicators of physical function with a substantial decline in gait speed. Finally, in state 4 or severely compromised physical function, there is a further eroding of performance on all indicators of physical function with a dramatic reduction in gait speed and performance in the 400-m walk. Indeed, the clinical relevance of the four-state model is supported by the mean decline in SPPB scores (8.90, 8.15, 7.32, and 5.49), 400-m walk time (400.48, 430.92, 506.78, and 641.28 seconds), and grip strength (30.38, 27.09, 23.86, and 21.11 kg) from states 1 to 4, respectively. Of note, the percentages of diabetic (cardiovascular disease) participants across states 1 to 4 are 16 (11), 28 (22), 25 (19), and 32 (26), respectively.
Profiles for physical functioning changed from baseline to 6 and 12 months. For example, the incidence of any change, whether positive or negative, was 30.1% at 6 months and 24.1% at 12 months, whereas 11% changed at both intervals. More people improved in physical functioning (20% at 6 months and 12% at 12 months) then declined (11% at 6 months and 12% at 12 months). Fifty-six percent of people did not experience any detectable change in physical functioning over the course of the study.
The probabilities of transitioning to a better or worse state are shown for each arm in Table 2. When compared with the SA group, those in the PA arm experienced a higher incidence of change to a more favorable state and a lower incidence of change to a less favorable state. For PA, 76% of persons in state 1 at baseline remained in state 1, whereas 56% of persons in SA who were in state 1 at baseline remained in state 1 for the follow-up visits, a difference of 20% (p < .001). For the most impaired persons in state 4 at baseline, 14% of those in PA regained some functioning, whereas it was 6% for SA, a difference of 8% (p = .007). The probability of transitioning to the other states, and percentage of participants improving, declining, or staying the same, is shown in Table 2 for states 2 and 3. Differences were not significant for these two states.
Table 2.
Probability of Transitioning to Better or Worse State
| Physical Activity Group (n = 213) | Successful Aging Group (n = 211) | |
|---|---|---|
| % Getting better (n) | ||
| State 1 | NA | NA |
| State 2 | 34 (30) | 33 (32) |
| State 3 | 39 (69) | 35 (53) |
| State 4** | 14 (6) | 6 (4) |
| % With no change (n) | ||
| State 1** | 76 (65) | 56 (48) |
| State 2 | 48 (39) | 45 (48) |
| State 3 | 55 (120) | 58 (109) |
| State 4** | 86 (34) | 94 (64) |
| % Getting worse (n) | ||
| State 1** | 24 (31) | 44 (36) |
| State 2 | 19 (23) | 21 (14) |
| State 3 | 6 (9) | 7 (14) |
| State 4 | NA | NA |
Notes: For a specific state, % getting better, no change, and getting worse add to 100% (within rounding error). NA = not applicable.
**p < .01.
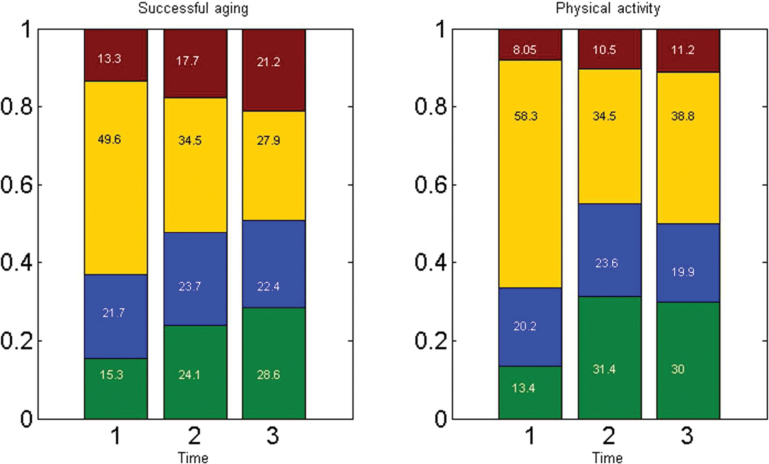
Figure 2 shows the prevalence of the four disability states over time for both PA and SA. The graph confirms the finding from examining the transition probabilities; that is, the intervention group benefitted from a slower trend in the growing rate of the worst state (state 4), as well as better retention of the best state (state 1) over time.
Figure 2.
State prevalence across time stratified by randomization arm. Legend: Green = state 1 = good physical functioning; Blue = state 2 = mild deficits in physical functioning; Yellow = state 3 = moderate deficits in physical functioning; Red = state 4 = severe deficits in physical functioning; Time 1 = baseline; Time 2 = 6 mo; Time 3 = 12 mo; Numbers within bars indicate percentage of total population in that states at that time.
Results from the mixed effects generalized linear model are summarized in Table 3. For ease of interpretation, states 2 and 3 were combined into one state, and ordinal logistic regression with mixed effects were applied to the consolidate data set. Table 3 shows that after controlling for baseline disability state, the PA intervention reduced the odds of transitioning into a worse state by almost 60% (odds ratio [OR] = 0.41, p < .001). Other significant factors included age (OR = 1.34, p < .0001), body mass index (OR = 1.16, p < .0001), and diabetes (OR = 2.71, p = .007). These results suggest that PA had a strong protective effect in preventing the loss of physical functioning, whereas conditions such as overweight and diabetes render strong negative effects on transitions in physical function.
Table 3.
Mixed Effects Generalized Linear Model Analysis of Mobility State Outcome*
| Effect | Odds Ratio | Lower 95% Limit | Upper 95% Limit | p |
|---|---|---|---|---|
| Baseline state 1† | 0.000† | 0.000 | 0.000 | <.0001 |
| Baseline state 2/3 | 0.000† | 0.000 | 0.003 | <.0001 |
| Intervention‡ | 0.405 | 0.211 | 0.778 | .0069 |
| Gender§ | 1.048 | 0.510 | 2.115 | .8982 |
| Black|| | 1.415 | 0.601 | 3.328 | .4271 |
| Latino¶ | 0.970 | 0.206 | 4.576 | .9691 |
| Other# | 0.190 | 0.028 | 1.307 | .0922 |
| Age | 1.345 | 1.228 | 1.473 | <.0001 |
| Body mass index | 1.157 | 1.089 | 1.229 | <.0001 |
| Cardiovascular disease** | 1.754 | 0.758 | 4.061 | .1902 |
| Hypertension†† | 0.545 | 0.026 | 11.393 | .6956 |
| Diabetes‡‡ | 2.706 | 1.316 | 5.565 | .0071 |
| Cancer§§ | 0.949 | 0.437 | 2.061 | .8949 |
*States for physical functioning was coded as 1, 2, 3 according to state 1, state 2/3 (combined), and state 4.
†–§§Respective reference category = state 4, control, female, white, no cardiovascular disease, no hypertension, no diabetes, and no cancer.
Discussion
The four states or phenotypes characterized in Figure 1 illustrate that there is not a uniform shift among all indicators of physical functioning when moving from one state to the next, supporting the researchers’ position that disablement is a multivariate construct. Of interest, is that even participants in state 1, the most favorable state, exhibited some deficit in measures of strength. Whereas loss of balance was the defining characteristic of state 2, state 3 was marked by a substantial reduction in gait speed. Finally, state 4 was characterized by an even greater reduction in gait speed and further negative shifts in the other four indicators of function. Clearly, this is a severe state for the status of older adults’ physical function as is evident by the clinical correlates of state 4.
The heterogeneity observed among indicators of physical function between the four states has important implications for research and clinical practice. First, there is little doubt that PA interventions for older adults need to consider the functional needs of participants. Walking programs in sterile laboratory environments do not address the complex nature of physical decline with aging. Indeed, this is one reason that LIFE-P included strength and balance as elements of training and promoted walking at home in environments that are more ecologically relevant to the maintenance of independent living. The researchers recently conducted a pilot study of older adults who scored either low or high on the SPPB and were randomized to either a traditional walking program in an exercise facility or one that combined walking with perceptual motor and cognitive challenges incorporated into the training regimen (18). What was striking about the findings is that participants who scored low on the SPPB did much better in the complex training regimen than in a traditional walking program. The reverse was true for those who scored high on the SPPB. This work supports the concept that tailoring PA interventions to specific deficits, that is, the current state of physical functioning, is an important consideration.
Several important differences were found between SA and PA for LIFE-P in terms of incidence of transition for profiles of physical functioning. PA reduced the likelihood of declining physical function for the older adults enrolled in the trial as compared with those in SA. For example, the probability of staying in the highest functioning state was 76% for PA, but only 56% for SA. The general trend that PA offered a protective effect for declining physical functioning is further confirmed by the mixed effects generalized linear model in which the risk of transitioning into a poorer state was reduced by 60% compared with SA (OR = 0.41, = 0.21, 0.78). The researchers remark here that the mixed effects model requires a so-called subject-specific interpretation, namely, that the intervention effect should be interpreted as if the same person received one intervention versus the other. It is interesting to note that this effect is almost of the same magnitude as either not having diabetes (OR = 1/(2.71) = 0.37, = 0.18, 0.76) or of a 7.0 point decrease in body mass index (OR = 0.36, = 0.24, 0.55) for obese older adults.
Importantly, there also appear to be some benefits for PA in terms of moving people to a state of higher functioning for those in the most severe state of physical function. Among those participants randomized to PA, the probability of moving out of state 4 was 14% compared with only 6% for SA. The researchers’ analyses provide further support for the hypothesis that physical function is a highly dynamic process in which people lose and regain function over short-time intervals (8–10). To the researchers’ knowledge, it is the first study to document this effect using performance-based measures of physical function. Overall, 44% of the total sample experienced a change in mobility from baseline during the 12-month course of the study. In fact, this study is likely to have underestimated the true incidence of change in physical function by assessing persons at only 6-month intervals and by combining eight states into four states. Had assessments been done monthly, or eight states been used, more changes probably would have been detected. The decision to use the four-state model was made because of practical and technical concerns; that is, the eight-state model was both difficult to interpret and required a larger sample size to support meaningful inference. Also of note is the fact that both groups experienced some spontaneous improvement in mobility status from baseline. One can only speculate as to why SA experienced some improvement, but several reasons come to mind. First, consistent with the conceptual model of this study, older adults move into and out of functional deficits even in the absence of active treatment. Thus, some drift in a positive direction is not unexpected. Second, it is not uncommon for some members of “untreated” comparison groups in lifestyle behavioral interventions to alter their behavior in line with “treated” groups. And third, it is possible that the physical functioning of the SA group benefitted from education, albeit not nearly as great as was observed in PA. It is also important to note that most of the benefit from the PA intervention was seen at 6 months. Although benefits were generally maintained at 12 months, they did not increase further.
This study has several limitations. First, given that the number of follow-ups was limited, it is not clear whether the positive effects of PA on physical function are sustainable over the long term. The current study also limits the number of disability states by combining “smaller” states. The simplified analysis could miss nuanced information about transitions related to physical functioning. However, using a large number of states with the current sample size is likely to result in less robust findings. The researchers recognize this trade-off and expect that the dilemma could be solved more satisfactorily through a larger study. Indeed, the LIFE-P main study is ongoing and the sample size is substantially larger (n = 1,600). Another limitation of the finding in this study is that the exercise undertaken by LIFE-P participants was relatively intensive and required assistance from trained intervention staff in order to ensure that exercise protocols were followed. This potentially limits the generalizability of the study. Finally, a limitation of the study is that the Markov assumption in the HMM may be too restrictive. It remains an empirical question whether relaxation of the (first order) Markov assumption to allow memory for prior states could improve the fit to the data. Some recent studies suggest that current disability status depends on a longer disability history of the individual (19). The researchers plan to investigate this issue in the future by using higher order Markov assumptions or a summarized measure of disability history.
In summary, the prescription of PA should give due consideration to the complexity inherent in physical functioning. The current data suggest that the protective effect of PA against the loss of physical function represents a pronounced effect, whereas its ability to move older adults out of compromised states of function is moderate. Given the researchers’ finding that PA can slow the loss of physical functioning with aging, and, in some cases, expedite recovery from poor states of functioning, good medical practice for physicians who care for older adults is to both assess their patients’ level of function and encourage either informal or formal prescriptions for PA training.
Funding
The Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) Study was funded by a National Institutes of Health/National Institute on Aging Cooperative Agreement (UO1 AG22376) and sponsored in part by the Intramural Research Program, National Institute on Aging, National Institutes of Health. Preparation of this study was also supported by National Institute on Aging (R01AG031827A) (PI: Ip). Drs. Ip, Rejeski, and Marsh are supported by the WFU Claude D. Pepper Center (NIA P30 AG021332).
References
- 1. Shumway-Cook A, Ciol MA, Yorkston KM, Hoffman JM, Chan L. Mobility limitations in the medicare population: prevalence and sociodemographic and clinical correlates. J Am Geriatr Soc. 2005; 53(7):1217–1221 [DOI] [PubMed] [Google Scholar]
- 2. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983; 31(12):721–727 [DOI] [PubMed] [Google Scholar]
- 3. Rejeski W, Ip E, Marsh A, Miller M, Farmer D. Measuring disability in older adults: the ICF framework. Geriatr Gerontol Intl. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for elders pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006; 61(11):1157–1165 [DOI] [PubMed] [Google Scholar]
- 5. Sturnieks DL, St George R, Lord SR. Balance disorders in the elderly. Clin Neurophysiol. 2008; 38: 467–478 [DOI] [PubMed] [Google Scholar]
- 6. Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004; 59(1):48–61 [DOI] [PubMed] [Google Scholar]
- 7. Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise? J Gerontol A Biol Sci Med Sci. 2001; 56(7):M412–M423 [DOI] [PubMed] [Google Scholar]
- 8. Verbrugge LM, Reoma JM, Gruber-Baldini AL. Short-term dynamics of disability and well-being. J Health Soc Behav. 1994; 35(2):97–117 [PubMed] [Google Scholar]
- 9. Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004; 291(13):1596–1602 [DOI] [PubMed] [Google Scholar]
- 10. Gill TM, Kurland BF. Prognostic effect of prior disability episodes among nondisabled community-living older persons. Am J Epidemiol. 2003; 158(11):1090–1096 [DOI] [PubMed] [Google Scholar]
- 11. Rejeski WJ, Ip EH, Marsh AP, Zhang Q, Miller ME. Obesity influences transitional states of disability in older adults with knee pain. Arch Phys Med Rehabil. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rejeski WJ, Fielding RA, Blair SN, et al. The lifestyle interventions and independence for elders (LIFE) pilot study: design and methods. Contemp Clin Trials. 2005; 26(2):141–154 [DOI] [PubMed] [Google Scholar]
- 13. Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000; 55(4):M221–M231 [DOI] [PubMed] [Google Scholar]
- 14. Breslow NE. Approximate inference in generalized linear mixed models. Am Stat Assoc. 1993; 88: 9–25 [Google Scholar]
- 15. Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. Heidelberg-New York: Springer-Verlag; 2000. [Google Scholar]
- 16. Zhang Q, Snow JA, Rijmen F, Ip E. Multivariate discrete hdden Markoc models for domain-based measurements and assessments. J Comput Graph Stat. 2010; 19: 746–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ip E, Snow JA, Heckert D, Zang Q, Gondolf E. Latent Markov models for analyzing temporal configuration for violence profiles and trajectories in a sample of batterers. Sociol Meth Res. 2010; 39: 222–255 [Google Scholar]
- 18. Marsh AP, Chmelo EA, Katula JA, Mihalko SL, Rejeski WJ. Should physical activity programs be tailored when older adults have compromised function? J Aging Phys Act. 2009; 17(3):294–306 [DOI] [PubMed] [Google Scholar]
- 19. Hardy SE, Allore HG, Guo Z, Dubin JA, Gill TM. The effect of prior disability history on subsequent functional transitions. J Gerontol A Biol Sci Med Sci. 2006; 61(3):272–277 [DOI] [PubMed] [Google Scholar]
- 20. Katula JA, Kritchevsky SB, Guralnik JM, et al. Lifestyle interventions and independence for elders pilot study: Recruitment and baseline characteristics. J. Am. Geriatr. Soc. 2007;55(5):674–683 [DOI] [PubMed] [Google Scholar]