Abstract
Background.
A comparative analysis between centenarians’ children and neighborhood controls is an efficient approach to learn how familial longevity influence and its interaction with environmental factors affect healthy aging. Yet, there are few extant studies that inform this topic; this study expands this literature.
Methods.
We analyze data from 417 children of centenarians and 560 neighborhood controls without family history of longevity in China (all participants aged 60–80) using ordered logit regression models.
Results.
We found that, compared to the neighborhood controls and adjusted for various potentially confounding factors, centenarians’ children had significantly better instrumental activities of daily living function(p < .001), smaller number of chronic conditions or health problems(p < .01), less anxiety and loneliness(p < .01), better cognitive function (p < .01), more resilience (p < .01), better self-rated health (p < .001), and better self-rated life satisfaction (p < .001). The results also reveal that interactions between familial longevity influence and one of three environmental factors (whether, as children, they received adequate medical care when ill, number of living children, and household economic conditions) may possibly affect health outcomes at old ages (p < .05). We discovered that effects of the environmental factors on health outcome are substantially stronger among elders who have no family history of longevity compared to centenarians’ children who probably carry positive genes and/or lifestyle behaviors from their long-lived parent(s), which may promote longevity.
Conclusion.
Familial longevity influence, through genetics and family lifestyle, is significantly associated with various aspects of health at older ages. Interactions between familial longevity influence and some environmental factors may affect health in old age.
Key Words: Centenarians’ children, Familial longevity influence, Genetics and family environment, Healthy aging, China.
GENETIC heredity is an important determinant of health and longevity, and research indicates that the effect of genetic inheritance on health and longevity becomes increasingly larger with advancing age, especially at ages greater than 100 (1). Family lifestyle is another important determinant of health and longevity (2). The term “familial longevity influence” used in this article includes both genetic inheritance and family lifestyle. We investigate health consequences of familial longevity influence and its interactions with environmental factors.
Because a focus on extreme cases is often a good way to gain research leverage at reasonable expense, investigation of centenarians’ offspring and controls is an efficient way to learn how genetic inheritance and family environment influence healthy aging. Prior research has suggested that centenarian offspring have better profiles of blood pressure and diabetes mellitus (3); similarly, Adams and colleagues (4) found that centenarian offspring have a 78% lower risk of myocardial infarction, 83% lower risk of stroke, and 86% lower risk of developing diabetes mellitus compared with the referent group.
Recent research has shown that interactions between genetic inheritance and environmental exposures also play a crucial role in health outcomes. Environmental exposures may regulate gene expression via DNA methylation and histone modification, which then influences health and longevity of the elderly (5,6). For example, a recent study shows that, adjusted for various confounders, the interactions between carrying the genotype FOXO1A-209, which significantly reduces survival probability from middle age to age 100 and above, and regular exercise significantly enhance survival by 31%–32% (p < .05) at ages ≥92 in Han Chinese people (7). Many previous studies have provided evidence of linkages between childhood conditions, socioeconomic status, family resources, and health outcomes in later life (8,9). These literatures led us to believe that it may be theoretically reasonable to assume that the interactions between familial longevity influence and childhood conditions, current economic status, and familial support resources (such as number of surviving children) would affect health outcomes at old ages. Although a considerable number of investigators have explored the effects of interactions between genetic and environmental factors on health outcomes and behaviors in children and adolescents (10,11), there are very few publications concerning the effects of interactions between familial longevity influence and environmental factors (abbreviated as F × E hereafter) on health outcomes at older ages.
All previously published studies comparing centenarians’ offspring and their peers were from industrialized countries. Western centenarians are generally less robust than centenarians in developing countries, who are highly selected by severe life conditions and high mortality in the past. For example, there were about five centenarians per million in China in the 1990s, compared with 50 per million in Western Europe, because proportionally many more Chinese died before reaching age 100. Only exceptionally robust Chinese elders became a centenarian due to greater exposure to environmental insults in China than that in Western Europe (12). Clearly, research comparing centenarians’ children and their peers in China is particularly useful for identifying the effects of familial longevity influence and its interactions with environmental exposures on healthy aging.
After a careful literature search, we found that previous studies in this field investigated a limited number of specific diseases and disorders, but none of them dealt with multiple dimensions of physical health, mental health, and subjective well-being simultaneously in a single study. However, in addition to physical health, mental health (eg, cognitive function and negative emotion) and subjective well-being (eg, self-rated health and self-rated life satisfaction) are also important dimensions of health in elderly populations (13). For example, anxiety and loneliness, which are components of mental health, are relatively more prevalent in the elderly than in younger adults and have adverse consequences on health outcomes such as poor physical health, reduced quality of life, and excess mortality (14). Subjective well-being has been found to be a predictor of mortality and health outcomes. For example, high level of life dissatisfaction at baseline significantly increased the odds of experiencing the onset of disability (15) and mortality (16) in the following years. We also found that none of the previously published studies on centenarians’ children and their peers explored the effects of F × E interactions on health outcomes. The present study intends to fill in these research gaps by exploring the effects of familial longevity influence and its interactions with several environmental factors on physical health, mental health, and subjective well-being at old ages.
Based on a careful literature search and our unique data set from children of centenarians and neighborhood controls in China, we intend to test the following two hypotheses:
H1: As compared to the neighborhood controls without family history of longevity, adjusted for various potentially confounding factors, children of centenarians have significantly better physical and mental health and subjective well-being.
H2: The interactions between familial longevity influence and three types of environmental factors, including childhood conditions, current economic status, and family support resources (measured by number of living children), may affect health outcomes at old ages.
Data, Measurements, and Methods
Data Sources
The current study is based on data from in-home interviews of 977 respondents aged 60–80 in eight areas spanning the northern, middle and southern parts of China; these respondents are part of the 2008–2009 wave of Chinese Longitudinal Healthy Longevity Survey (CLHLS). The 977 respondents include 417 individuals who are biological children of centenarians (each centenarian has one child included in this study) and 560 unrelated controls living in the same or neighboring village or street. All of the neighborhood controls do not have family history of longevity; namely, both of their biological parents died before age 85, and none of their siblings survived to age 85 (see online supplementary materials, section SM-I for details on how the eight areas and the participants were selected).
Measurements
Dependent variables.— Instrumental activities of daily living.—For each of the eight daily tasks of shopping, cooking a meal, washing clothing, visiting neighbors, walking continuously for 1 km, lifting a weight of 5kg, continuously crouching and standing up three times, and taking public transportation, the score is 1 or 0 if the participant needed or did not need help, respectively, to perform the task. The range of the scores of instrumental activities of daily living (IADL) disability is from 0 to 8. These IADL categories are in fact a mixture of the standard IADL (17) with a new construct (visiting neighbors, which is a daily task for many elderly in the Chinese cultural context) and the standard functional limitations (eg, lifting a weight of 5kg) (18). Because activity of daily living (ADL) disability (bathing, dressing, indoor transferring, going to the toilet and cleaning oneself afterward, eating, and continence) is rare among the participants aged 60–80 in our sample (only 2.4% of centenarians’ children and 3.2% of the neighborhood controls were ADL disabled), we do not include ADL as a dependent health variable in this study.
Self-reported chronic conditions or health problems.—The CLHLS collected self-reported information on the following chronic conditions or health problems: hypertension, diabetes, heart disease, stroke and/or other cerebrovascular disease, bronchitis and/or emphysema and/or asthma and/or pneumonia, pulmonary tuberculosis, cataracts, glaucoma, cancer, prostate tumor, gastric or duodenal ulcer, Parkinson’s disease, bedsore, arthritis, dementia, epilepsy, cholecystitis or cholelithiasis, blood disease, chronic nephritis, galactophore disease, uterine tumor, and hepatitis. We dichotomized the responses as having none or at least one of the chronic conditions or health problems. The number of self-reported chronic conditions or health problems (which is within the possible range of 0–22) is categorized as 0, 1, 2, 3, and 4+ and employed as an additional health outcome.
Mini-mental state examination.—The international standard mini-mental state examination (MMSE) questionnaire (19,20) was adapted to Chinese cultural context and was carefully tested in our pilot survey interviews (20). The questionnaire included items regarding orientation, registration, attention, calculation, recall, and language, with a total score ranging from 0 to 30. Higher score of MMSE means better cognitive functioning.
Anxiety and loneliness.—Anxiety and loneliness, which are components of mental disorder and depression in the elderly, have adverse consequences such as reduced quality of life and excess mortality (21,22), higher age-related increases in systolic blood pressure (SBP) (14), higher vascular resistance (23), and poorer antibody response to vaccine (24). In this study, data on anxiety and loneliness collected in the CLHLS consist of answers to two questions about (i) “feel fearful or anxious” and (ii) “feel lonely and isolated.” The respondents were coded as 0 if they reported neither of the two symptoms; coded as 1 if they reported either one of the two symptoms; and coded as 2 if they reported both symptoms.
Simplified resilience score.—We use a simplified resilience score (SRS) emphasizing coping and adjustment among the elderly, which is theoretically guided by the general framework of the Connor-Davidson Resilience Scale (CD-RISC) (21) and based on the available data collected through seven questions related to resilience in the CLHLS (22). In general, the seven items reflect personal tenacity, optimism, coping with negative mood, secure relationship, and self-control, which are deemed as important factors of resilience (21). The total SRS score ranges from 0 to 22, with higher scores reflecting greater resilience (22). (The internal consistency of SRS measured by Cronbach’s alpha coefficient is 0.69, indicating its reliability is reasonably adequate (14). Principal component analysis generates three factors with eigenvalues >1, explaining 78.5% of the total variance. These basic indicators of the psychometric properties show that the SRS based on the CLHLS data are reasonably acceptable).
Self-rated life satisfaction.—According to the previous literature, high levels of life dissatisfaction at baseline significantly increased the odds of experiencing the onset of disability (25) and mortality (26) in the following years. We use the international standard self-rated life satisfaction (27) to measure subjective well-being. Self-rated poor life satisfaction is coded as 0, 1, 2, 3, or 4 if the interviewees’ response to the question “How do you rate your life at present?” is very good, good, so so, bad, and very bad, respectively.
Self-rated health.—Self-rated poor health is coded as 0, 1, 2, 3, or 4 if the interviewees’ response to the question “How do you rate your health?” is very good, good, so so, bad, and very bad, respectively. Although self-rated health normally does not serve as an indicator of subjective well-being, several studies have demonstrated a robust and significant relationship between self-rated health and subjective well-being (28).
The independent variable.— The key independent variable in this study is whether the respondent is a centenarian’s biological child or a neighborhood control who had no first-degree relatives who survived to age 85. We include the following covariates in our statistical models, based on reviews of previous studies in this field and our understanding of the Chinese social context.
Demographic variables.—Include age and gender.
Childhood conditions.—Include availability of medical care in childhood, based on the question, “Could you get adequate medical service when you were sick in childhood?” Those who answer “yes” or “did not get sick in childhood” are coded as 1, representing adequate medical service and good health status in childhood. Those who answer “no” are coded as 0. The interviewers’ manual defined “adequate medical care” to mean that the parents were able to have the child to see a medical doctor and get either Chinese or Western medicine when the child was ill.
Adulthood socioeconomic variables.—Include education (no schooling vs ≥1 year of schooling; about half of the Chinese elderly women aged 60–80 had no schooling) and self-reported household economic condition (good vs poor as compared with the average in the community).
Family/social connection and support variables.—Include marital status (currently married vs not married, ie, divorced, widowed, or never married); number of living children; social and leisure activity index (the summation of seven variables of gardening, personal outdoor activities excluding exercise, raising poultry or pets, reading, playing cards or mah-jong, listening to the radio or watching TV, and participating in some organized social activities excluding religious participation).
To simplify the presentations, childhood conditions, socioeconomic status, and family/social connections and support are hereafter referred to as “environmental factors.”
Statistical Methods
We conducted seven ordered logit regressions to estimate the effect of familial longevity influence (ie., centenarian’s child vs neighborhood control without family history of longevity) and other covariates on seven categorical health outcomes: IADL disabled, categorized number of chronic conditions or health problems, poor self-rated health, poor self-rated life satisfaction, anxiety and loneliness, MMSE score, and simplified resilience score. Wald statistical tests confirmed that the proportional odds ratio/parallel lines hypothesis is met in all of the seven ordered logit models. To test our theoretical hypothesis H2, we estimated the effects of possible interaction terms between familial longevity influence and each of the three environmental factors including childhood conditions, current economic status, and family support resources (measured by number of living children) in the ordered logit regression models (29). Similar to some previous studies (29) and due to space limitation, we only present and discuss statistically significant interaction effects in this article. The technical details concerning the estimates of the interactions between familial longevity influence and the environmental factors are presented in Supplementary material SM-II. All analyses were performed using STATA/SE 10.0
Results
Descriptive Statistics and Main Effects of the Six Environmental Factors
Table 1 presents the sample distributions for gender, mean age, and the six potentially confounding environmental variables, as well as the statistical tests of difference between centenarians’ children and their neighborhood controls. Table 2 presents comparisons of the health outcome indicators between the centenarians’ children and the neighborhood controls who have no family history of longevity. The summary descriptive statistics, without controlling for covariates, clearly show that centenarians’ children are significantly better off in all of the seven health outcome indicators considered than the neighborhood controls who have no family history of longevity.
Table 1.
Descriptive Statistics of Sample Distributions for Centenarians’ Children and Neighborhood Controls
| Centenarians’ Children | Neighborhood Controls | |||||
|---|---|---|---|---|---|---|
| Women | Men | Both Sexes | Women | Men | Both Sexes | |
| Number of participants | 98 | 319 | 417 | 269 | 291 | 560 |
| Mean age of the participants | 68.9 | 69.0 | 69.0 | 71.2 | 70.7 | 71.0 |
| % Men among total number of participants | — | 76.5 | — | — | 52.0 | — |
| % Got adequate medical care when ill in childhood | 36.7 | 28.2 | 30.2 | 23.8 | 32.0 | 28.0 |
| % Household economic condition is good | 21.4 | 13.8 | 15.6 | 10.4 | 12.4 | 11.4 |
| % Had >1 year of schooling | 63.3 | 82.8 | 78.2 | 37.9 | 74.6 | 57.0 |
| % Currently married | 74.5 | 88.4 | 85.1 | 67.3 | 73.5 | 70.5 |
| Average number of living children | 3.6 | 3.4 | 3.5 | 4.0 | 3.5 | 3.7 |
| Mean of the social and leisure activity index | 2.3 | 2.7 | 2.6 | 2.3 | 2.6 | 2.4 |
Table 2.
Descriptive Health Outcome Comparisons between Centenarians’ Children and Neighborhood Controls
| Centenarians’ Children | Neighborhood Controls | |||||
|---|---|---|---|---|---|---|
| Women | Men | Both Sexes | Women | Men | Both Sexes | |
| Number of participants | 98 | 319 | 417 | 269 | 291 | 560 |
| Average score of IADL disability | 0.67 | 0.42 | 0.48*** | 1.04 | 0.80 | 0.92*** |
| % Having anxiety and loneliness | 5.1 | 5.6 | 5.5*** | 12.6 | 7.9 | 10.2*** |
| Average MMSE score | 27.2 | 28.3 | 28.0*** | 26.1 | 27.7 | 27.0*** |
| Average number of chronic conditions/health problems | 0.85 | 0.66 | 0.70*** | 0.98 | 0.95 | 0.96*** |
| % With at least one chronic disease | 53.1 | 46.1 | 47.7*** | 61.0 | 59.8 | 60.4*** |
| Average score of self-rated poor health | 1.19 | 1.30 | 1.28*** | 1.62 | 1.60 | 1.61*** |
| Average score of self-reported poor quality of life | 1.06 | 1.30 | 1.24** | 1.44 | 1.41 | 1.43** |
| Average simplified resilience score | 5.8 | 6.0 | 5.9*** | 5.4 | 5.5 | 5.5*** |
Note: The statistical significant level of the differences between both sexes of centenarians’ children and both sexes of neighborhood controls are indicated by **p < .01, ***p < .001.
The sample distributions of the covariates in Table 1 show that centenarians’ children have better socioeconomic status (SES) than the neighborhood controls. For example, 78.2% of centenarians’ children had at least 1 y of schooling, in contrast to 57.0% among the neighborhood controls; 15.6% of the centenarians’ children reported that their economic condition was good, which was 4.2 percentage points higher than that of the neighborhood controls; 76.5% percent of centenarians’ children were men, in contrast to 52% among the neighborhood controls (The higher number of male participants among children of centenarians compared to the neighborhood controls is due to the fact that most Chinese old parents live with an adult son; the CLHLS survey selected centenarians’ children mostly within the household, whereas the controls were selected randomly); more centenarians’ children are currently married (85.1%) compared with the neighborhood controls (70.5%). Clearly, the centenarians’ children in our sample have favorable demographic and SES characteristics, as compared to the neighborhood controls, which may positively affect their health outcomes. As a result, we cannot draw any conclusion on whether the substantially large differences in the average values of the health outcome indicators between centenarians’ children and the neighborhood controls presented in Table 2 are caused by familial longevity influence or demographic/SES characteristics. Therefore, we employ multivariate statistical models to investigate the effects of familial longevity influence and its interactions with environmental factors on health outcomes, while controlling for various potentially confounding covariates of age, gender, childhood and adulthood SES, and family/social connection and support. Results are presented in Tables 3 and 4.
Table 3.
Estimates of the Odds Ratios from Ordered Logit Models of the Effects of Study Covariates and the Significant Interactions on the Health Outcomes
| IADL Disabled | Number of Chronic Conditions | Self-rated Poor Health | Self-rated Poor Life Satisfaction | |||
|---|---|---|---|---|---|---|
| Independent Variables Code of the model | I-1 | I-2 | II-1 | III-1 | IV-1 | IV-2 |
| Neighborhood controls (centenarians’ children) | 1.65** | 1.98*** | 1.49** | 1.93*** | 1.45** | 2.72*** |
| Age | 1.15*** | 1.15*** | 1.04** | 1.00 | 0.99 | 0.99 |
| Male (female) | 0.75+ | 0.77 | 0.85 | 1.16 | 1.30+ | 1.28+ |
| Got adequate medication when ill in childhood (no) | 0.41*** | 0.77 | 0.97 | 0.69** | 0.87 | 0.87 |
| Family economic condition is good (no) | 0.59+ | 0.57* | 1.02 | 0.42*** | 0.29*** | 0.29*** |
| Has >1 year of schooling (no) | 0.72+ | 0.70* | 1.13 | 1.06 | 0.83 | 0.83 |
| Currently married (no) | 1.05 | 1.03 | 0.85 | 0.89 | 0.89 | 0.88 |
| Number of living children | 1.01 | 1.01 | 0.99 | 1.06 | 0.97 | 1.07 |
| Social and leisure activity index | 0.72*** | 0.72*** | 1.04 | 0.80*** | 0.87** | 0.88* |
| F × E interaction terms (RERI) | ||||||
| “Controls” × “Got adequate medical care when ill in childhood” | — | 0.40* | — | — | — | — |
| “Controls” × “Number of living children” | — | — | — | — | — | 0.84* |
| LR chi2 | 234.8 | 239.6 | 31.7 | 96.1 | 80.5 | 85.3 |
| Prob > chi2 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Log likelihood: –2log(L) | 1766.1 | 1761.3 | 2383.2 | 2509.0 | 2391.3 | 2386.4 |
| Log likelihood change: = –2[log(L0) – log(L1)] | 4.8* | — | — | 4.9* | ||
Notes: *p < .05, **p < .01, ***p < .001.
The category in the parentheses after the independent variables is the reference group.
Table 4.
Estimates of the Odds Ratios from Ordered Logit Models of the Effects of Study Covariates and the Significant Interactions on the Health Outcomes
| Dependent Variable | Anxiety and Loneliness | Better MMSE Score | Better Resilience Score | |
|---|---|---|---|---|
| Code of the model | V-1 | V-2 | VI-1 | VII-1 |
| Neighborhood controls (centenarians’ children) | 1.46* | 1.63** | 0.72** | 0.67** |
| Age | 1.02 | 1.02 | 0.94*** | 0.96*** |
| Male (female) | 0.74* | 0.75+ | 1.46** | 1.02 |
| Got adequate medication when ill in childhood (no) | 0.67* | 0.66** | 1.32* | 1.32* |
| Family economic condition is good (no) | 0.81 | 1.27 | 1.07 | 1.21 |
| Has >1 year of schooling (no) | 0.91 | 0.92 | 3.06*** | 1.23 |
| Currently married (no) | 0.35*** | 0.35*** | 0.89 | 4.46*** |
| Number of living children | 0.96 | 0.96 | 0.99 | 1.07+ |
| Social and leisure activity index | 0.90+ | 0.90+ | 1.22*** | 1.18** |
| F × E interaction terms (RERI) | ||||
| “Controls” × “Household economic condition is good” | — | 0.43* | — | — |
| LR chi2 | 101.4 | 105.2 | 257.9 | 205.0 |
| Prob > chi2 | 0.000 | 0.000 | 0.000 | 0.000 |
| Log likelihood: –2log(L) | 1551.6 | 1547.8 | 3596.9 | 2656.0 |
| Log likelihood change: = –2[log(L0) – log(L1)] | 3.8* | — | — | |
Notes: The same as in Table 3.
As shown in Tables 3 and 4, adjusted for the various covariates, older respondents had significantly higher risks of IADL disability and having chronic conditions and health problems but significantly lower scores on cognitive function and resilience. We did not find any significant association between age and self-rated health, self-rated life satisfaction, and anxiety and loneliness. As compared to their female counterparts, old men are significantly less likely to be IADL disabled, significantly less likely to report anxiety and loneliness, report significantly better cognitive capacity, and have a marginally significant higher risk of self-rated poor life satisfaction. There are no significant gender differentials in the number of chronic conditions and health problems, self-rated health, and resilience scores. Adequate medication when ill in childhood is positively associated with health outcome at old ages and most of the estimates are statistically significant. Family economic condition and education are, in general, positively associated with health outcome, but most of the estimates are not statistically significant. Being currently married is significantly associated with mental health (measured by negative emotion and MMSE) but not significantly associated with physical health (measured by IADL and number of chronic conditions or health problems) and subjective well-being (measured by self-rated health and life satisfaction). The estimates show that number of living children was not significantly associated with health outcome, but social and leisure activity mostly had significant effects on health outcomes at old ages.
The Main Effects of the Familial Longevity Influence on Health Outcome
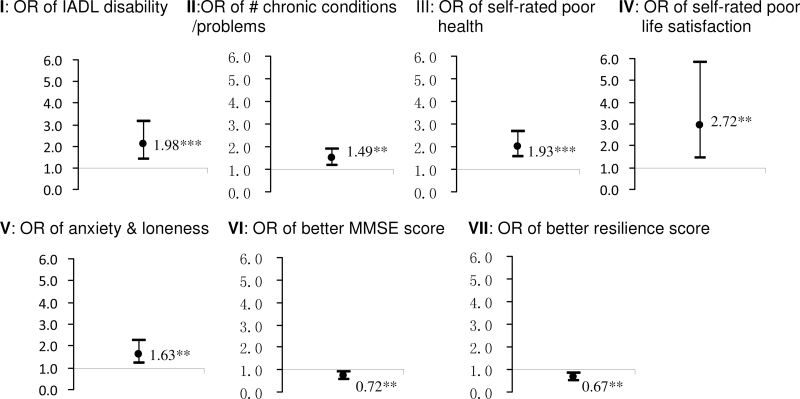
Estimates of the main effects of the familial longevity influence on health outcome from the regressions are presented in Figure 1 and in Tables 3 and 4. The results indicate that, compared to the centenarians’ children, the neighborhood controls without family history of longevity were 98% more likely to be IADL disabled (p < .001), 49% more likely to have a larger number of chronic conditions or health problems (p < .01), 93% more likely to report poor health (p < .001), 172% more likely to report poor life satisfaction (p < .001), 63% more likely to suffer anxiety and loneliness (p < .01), 28% less likely to have better MMSE score (p < .01), and 33% less likely to have better simplified resilience score (p < .01). All of these estimates are adjusted for potentially confounding covariates, including demographic characteristics, childhood and adulthood SES, and family/social connection and support.
Figure 1.
Estimates of the odds ratios (ORs) from ordered logit models of the main effects of familial longevity influence on health outcome at old ages: neighborhood controls versus centenarians’ children, adjusted for various confounding factors.
Effects of Interactions Between the Familial Longevity Influence and Environmental Factors (F × E Interactions)
Adopted from the standard definition of an interaction between environmental exposure and a genetic variant (10), we define that an interaction between an environmental exposure and familial longevity influence is present if the effect of an environmental exposure on a health outcome indicator differs significantly among individuals with different familial longevity influence statuses. In Tables 3 and 4, we present the statistically significant (p < .05) estimates of the relative excess risk index (RERI) of health outcomes (30,31), due to the F × E interactions in models I-(2), IV-(2), and V-(2), together with the effects of familial longevity influence and environmental exposures(see SM-II for technical details). Following the standard Aiken and West procedure (32), we conducted blocked multivariate regressions with the interaction term in the last block, and we presented the χ2 tests to show whether the difference of likelihood ratios between the full model including the interaction block and the model without the interaction block are statistically significant. Such tests also inform whether the last block of interactions included in the regression is statistically significant. The results of these additional tests (see the last a few lines of Tables 3 and 4) confirm that the interactions between familial longevity influence and one of the three environmental factors (whether as children they received adequate medical care when ill, number of living children, and household economic conditions) are statistically significant (p < .05) in models I-(2), IV-(2), and V-(2) The significant results of these additional tests also imply that the likelihood of the Type 1 error in our estimates of the interaction effects may be small (33).
The possibilities of correlations between familial longevity influence and any one of the three environmental factors with statistically significant F × E interaction terms (RERI, listed in Tables 3 and 4) are ruled out by the statistical tests and regression analysis (see SM-III, Tables S2 and S3 in SM). Thus, the estimates of RERI in Tables 3 and 4 represent the F × E interaction effects. The estimates show that the F × E interactions between no family history of longevity and receiving adequate medical care when ill in childhood significantly reduce the risk of IADL disability at old ages by 60% (p < .05) (see Model I-(2) in Table 3). F × E interactions between no family history of longevity and larger number of living children significantly reduce the risk of self-rated poor life satisfaction by 16% (p < .05; see Model IV-(2) in Table 3). F × E interactions between no family history of longevity and good household economic condition significantly reduce the risk of anxiety and loneliness by 57% (p < .05; see Model V-(2) in Table 4).
In addition to analyzing the RERI of health outcomes due to the F × E interactions defined and discussed earlier, an intuitive way to present and interpret the F × E interaction effects is to compare the relative risks of health outcomes of those who are exposed or not exposed to the environmental factor within the group of centenarians’ children and within the neighborhood controls without family history of longevity (see Section SM-III of supplementary material for technical details). As shown in Table 5, receiving adequate medical care when ill in childhood may reduce the risk of IADL disability by 23.0% in the centenarians’ children compared to 57.1% in the neighborhood controls (model I-[2] in Table 5). Among centenarians’ children, increasing the number of living children by 1 may increase the risk of self-reported poor life satisfaction by 7.0% (not statistically significant), but it may reduce the risk of self-reported poor life satisfaction by 9.9% in neighborhood controls (model IV-[2] in Table 5). The estimates for model V-(2) shown in Table 5 show that good household economic condition may increase the risk of anxiety and loneliness by 27% (not statistically significant) among centenarians’ children; however, in the neighborhood controls, good household economic condition helped to reduce the risk of anxiety and loneliness by 45.4%.
Table 5.
Estimates of the Odds Ratios (ORFE) of Health Outcome for Individuals with Familial Longevity Influence Status (F) and Environmental Exposure Status (E) and the Relative Excess Risk due to the F × E Interaction
| Dependent Variable and Model Code | I-(2): IADL Disabled(ordered logit model) | IV-(2): Poor Self-ratedLife Satisfaction (ordered logit model) | V-(2): Anxiety and Loneliness (ordered logit model) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Environmental exposure(E = 0 or 1) | Got adequate medicalcare when ill in childhood | Number of living children | Good economic condition | ||||||
| No(E = 0) | Yes(E = 1) | DifferenceE = 1 vs 0 | Median(E = 0) | Median+1(E = 1) | DifferenceE = 1 vs 0 | No(E = 0) | Yes(E = 1) | DifferenceE = 1 vs 0 | |
| Centenarians’ children (F = 0) | 1.00 (ref.) | 0.77 | –23.0% | 1.00 (ref.) | 1.07 | 7.0% | 1.00 (ref.) | 1.27 | 27.0% |
| Neighborhood control (F = 1) | 1.98*** | 0.85 | –57.1% | 2.72*** | 2.45 | –9.9% | 1.63** | 0.89 | –45.4% |
| Relative excess risk index due to F × E interaction | 0.40* (0.176, 0.892) p = .025 | 0.84* (0.722, 0.981) p = .027 | 0.43* (0.185, 0.998) p = .049 | ||||||
Notes: *p < .05, **p < .01, ***p < .001; see section SM-IV of Supplementary Material for some technical details concerning the estimates presented in this table.
Discussion
We conducted multivariate logit regression analysis, employing the unique data from 417 children of centenarians and 560 neighborhood controls who have no family history of longevity. We found that, compared to the neighborhood controls who have no family history of longevity and adjusted for age, gender, and six major environmental factors, the elderly who have a centenarian parent have significantly better instrumental activities of daily living function (p < .001), smaller number of chronic conditions or health problems (p < .01), less anxiety and loneliness (p < .01), better cognitive function (p < .01), more resilience (p < .01), better self-rated health (p < .001), and better self-rated life satisfaction (p < .001). Based on these findings, we conclude that familial longevity influence (including influences of genetics and the family environment) is strongly and positively associated with physical health, mental health, and subjective well-being at old ages.
The results also reveal that the interactions between familial longevity influence and the three environmental factors (whether as children they received adequate medical care when ill, number of living children, and household economic conditions) play some significant (p < .05) roles in determining the three health outcome indicators (IADL, self-rated life satisfaction, and anxiety-loneness) at old ages. We discovered that the effects of these environmental factors on the health outcome indicators are substantially stronger among elders who have no family history of longevity compared to centenarians’ children who likely carry genes and/or inherited healthy behavior and better family lifestyle from long-lived parents. This interesting finding may be understood from a more general mechanism: in the absence of a given protective factor (eg, familial longevity influence), the other protective factors have stronger effects on health. This finding, although mixing genetic inheritance and family lifestyle, is generally consistent with other studies focusing on effects of interactions between genetic variants and behavioral/ environmental factors. For example, Zeng and colleagues found that the negative effects of the four life stress factors on self-rated health among the carriers of APOE4, a genotype that is associated with poor health and higher mortality (34,35), are much stronger than those among the APOE4 noncarriers (36). Talmud and colleagues found that middle-aged individuals with the D9N allele for lipoprotein lipase had a markedly increased risk for ischemic heart disease when they smoked, whereas the risk associated with smoking was much less in those who did not carry the D9N allele (37).
The findings of the present study could imply that, although familial longevity influence is one of the important factors that determine health outcome, positive social/behavioral/environmental factors may be significantly more important for those who do not have the advantage of family history of longevity, as compared to those who are with long-lived parents. Thus, in consideration of the cost–benefit effectiveness of health promotion programs and the stronger health assistance needs for the disadvantaged groups, future interventions may need to give more attention to and target those who do not have the advantage of familial longevity influence (38).
Although we believe that our findings summarized and discussed herein are useful, we must be aware of their limitations and cautious in interpreting them. First, we consider our estimates concerning the effects of F × E interactions as exploratory rather than conclusive. In our statistical analysis, we constructed seven regression models and each of them has a health outcome indicator as dependent variables, representing different aspects of physical health, mental health, and subjective well-being. In each of the seven regression models, we tried to test our theoretical hypothesis concerning the interactions between familial longevity influence and each of the three environmental factors of childhood conditions, current economic status, and family support resources measured by number of living children. In total, we conducted 21 (= 3 × 7) statistical comparisons on F × E interactions. We believe that we do not need to follow the Bonferroni method (or other similar method) to correct the estimated p values through multiplying the p by number of comparisons, although we must be cautious in interpreting the results. This consideration is consistent with recommendations in the literature. For example, in the book Intuitive Biostatistics, Harvey Motulsky described both the importance of correcting multiple comparisons to prevent high risk of false-positive errors if the comparisons are independent of each other and how to do it; he also discussed that in many studies, investigators measure the health outcome using a variety of complementary measures; these data can lead to multiple p values but should not be corrected for multiple comparisons in order to avoid the too high costs of false-negative errors, because the null hypotheses are not independent and, to a large degree, the various outcomes measure the same thing (39). Similar points were emphasized and numerically demonstrated in the section entitled “When not to correct for multiple comparisons” in the Handbook of Biological Statistics by McDonald (40). Note that the multiple comparisons in our present study are not independent of each other, because we use highly correlated health outcome indicators as dependent variables in each of the seven regressions. Thus, we believe that there is no need to follow the Bonferroni method (or other similar method) to correct the estimated p values, because the costs of increasing the chance of false-negative errors may be too high. Of course, we must be cautious in interpreting our present findings concerning the interaction effects as exploratory, rather than conclusive, because our estimates may still potentially involve false-positive errors. Future studies need more stringent tests of the significance with larger samples and replication studies to validate our exploratory findings on the effects of interactions between familial longevity influence and the environment factors on health outcomes at old ages.
We are also aware that it is difficult to separate different causes of the association based on our present case–control analysis. Although familial longevity influence may positively affect the health of centenarians’ children, it might also be possible that having healthier children might help the parents’ exceptional longevity to some extent. Furthermore, we do not yet know the biological mechanisms by which the degree of impacts of environmental factors on health outcome are substantially different between centenarians’ children and the neighborhood controls who have no family history of longevity. Clearly, more in-depth studies including more stringent tests of the significance and replication studies are warranted for deeper understanding of the effects of interactions between familial longevity influence and environmental exposures on health outcome at old ages.
Funding
This study is part of the project funded by National Institute on Aging at the National Institutes of Health (R01 AG023627 to Y.Z.), National Natural Science Foundation of China (71110107025 to Y.Z.), and National Key Basic Research Program of China: 2013CB530700 to Y.Z. and G.J.).
Supplementary Material
Supplementary material can be found at: http://biomedgerontology.oxfordjournals.org/
Acknowledgments
We are very grateful for the thoughtful comments provided by the anonymous reviewers, the editors, and Dr. Jessica Sautter. Y.Z. designed the research, supervised data collection and data analysis, and wrote the article. H.S.C analyzed data; X.M.S. and Z.X.Y performed data collection; Z.Y. suggested revisions of the article; and D.G.B., J.G., and Z.Y. suggested study design and revisions of the article.
References
- 1. Perls TT, Wilmoth J, Levenson R, et al. Life-long sustained mortality advantage of siblings of centenarians. Proc Natl Acad Sci USA. 2002; 99: 8442–8447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychol Bull. 2002; 128: 330–366 [PubMed] [Google Scholar]
- 3. Barzilai N, Gabriely I, Gabriely M, Iankowitz N, Sorkin JD. Offspring of centenarians have a favorable lipid profile. J Am Geriatr Soc. 2001; 49: 76–79 [DOI] [PubMed] [Google Scholar]
- 4. Adams ER, Nolan VG, Andersen SL, Perls TT, Terry DF. Centenarian offspring: start healthier and stay healthier. J Am Geriatr Soc. 2008; 56: 2089–2092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. IOM (Institute of Medicine, Academy of Sciences) Committee Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. In: Hernandez LM, Blazer DG.eds. Washington, DC: National Academia of Sciences; 2006. [PubMed] [Google Scholar]
- 6. Tsankova N, Renthal W, Kumar A, Nestler EJ. Epigenetic regulation in psychiatric disorders. Nat Rev Neurosci. 2007; 8: 355–367 [DOI] [PubMed] [Google Scholar]
- 7. Zeng Y, Cheng L, Chen H, et al. Effects of FOXO genotypes on longevity: a biodemographic analysis. J Gerontol A Biol Sci Med Sci. 2010; 65: 1285–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hayward MD, Gorman BK. The long arm of childhood: the influence of early-life social conditions on men’s mortality. Demography. 2004; 41: 87–107 [DOI] [PubMed] [Google Scholar]
- 9. Yi Z, Gu D, Land KC. The association of childhood socioeconomic conditions with healthy longevity at the oldest-old ages in China. Demography. 2007; 44: 497–518 [DOI] [PubMed] [Google Scholar]
- 10. Rutter M, Silberg J. Gene-environment interplay in relation to emotional and behavioral disturbance. Annu Rev Psychol. 2002; 53: 463–490 [DOI] [PubMed] [Google Scholar]
- 11. Guo G, Roettger ME, Cai T. The integration of genetic propensities into social-control models of delinquency and violence among male youths. Am Soc Rev. 2008; 73: 543–568 [Google Scholar]
- 12. Jeune B, Vaupel JW, eds. Exceptional Longevity: From Prehistory to the Present. Odense, Denmark: Odense University Press; 1995. [Google Scholar]
- 13. World Health Organization, 2010. WHO Healthy Workplace Framework and Model: Background and Supporting Literature and Practices http://www.who.int/occupational_health/publications/healthy_workplaces_background_documentdfinal.pdf (accessed Oct. 20, 2011).
- 14. Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006; 21: 152–164 [DOI] [PubMed] [Google Scholar]
- 15. Collins AL, Goldman N, Rodríguez G. Is positive well-being protective of mobility limitations among older adults? J Gerontol B Psychol Sci Soc Sci. 2008; 63: P321–P327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lyyra TM, Törmäkangas TM, Read S, Rantanen T, Berg S. Satisfaction with present life predicts survival in octogenarians. J Gerontol B Psychol Sci Soc Sci. 2006; 61: P319–P326 [DOI] [PubMed] [Google Scholar]
- 17. Wiener JM, Hanley RJ, Clark R, Van Nostrand JF. Measuring the activities of daily living: comparisons across national surveys. J Gerontol. 1990; 45: S229–S237 [DOI] [PubMed] [Google Scholar]
- 18. Nagi SZ. Disability concepts revisited: implications for prevention. In: Pope A, Taylor A, eds. Disability in America: Toward a National Agenda for Prevention. Washington, DC: National Academy Press; 1991. [Google Scholar]
- 19. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12: 189–198 [DOI] [PubMed] [Google Scholar]
- 20. Zeng Y, Vaupel JW. Functional capacity and self–evaluation of health and life of oldest old in China. J Soc Issues. 2002; 58: 733–748 [Google Scholar]
- 21. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003; 18: 76–82 [DOI] [PubMed] [Google Scholar]
- 22. Zeng Y, Shen K. Resilience significantly contributes to exceptional longevity. Curr Gerontol Geriatr Res. 2010; 2010: 525693.10.1155/2010/525693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hawkley LC, Cacioppo JT. Loneliness and pathways to disease. Brain Behav Immun. 2003; 17 Suppl 1: S98–105 [DOI] [PubMed] [Google Scholar]
- 24. Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychol. 2005; 24: 297–306 [DOI] [PubMed] [Google Scholar]
- 25. Koivumaa-Honkanen H, Kaprio J, Honkanen R, Viinamäki H, Koskenvuo M. Life satisfaction and depression in a 15-year follow-up of healthy adults. Soc Psychiatry Psychiatr Epidemiol. 2004; 39: 994–999 [DOI] [PubMed] [Google Scholar]
- 26. Koivumaa-Honkanen H, Honkanen R, Viinamäki H, Heikkilä K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy Finnish adults. Am J Epidemiol. 2000; 152: 983–991 [DOI] [PubMed] [Google Scholar]
- 27. Kahneman D, Krueger AB. Developments in the measurement of subjective well-being. J Econ Pers. 2008; 20: 3–24 [Google Scholar]
- 28. Siahpush M, Spittal M, Singh GK. Happiness and life satisfaction prospectively predict self-rated health, physical health, and the presence of limiting, long-term health conditions. Am J Health Promot. 2008; 23: 18–26 [DOI] [PubMed] [Google Scholar]
- 29. Audrain-McGovern J, Lerman C, Wileyto EP, Rodriguez D, Shields PG. Interacting effects of genetic predisposition and depression on adolescent smoking progression. Am J Psychiatry. 2004; 161: 1224–1230 [DOI] [PubMed] [Google Scholar]
- 30. Andersson T, Alfredsson L, Källberg H, Zdravkovic S, Ahlbom A. Calculating measures of biological interaction. Eur J Epidemiol. 2005; 20: 575–579 [DOI] [PubMed] [Google Scholar]
- 31. de Mutsert R, Jager KJ, Zoccali C, Dekker FW. The effect of joint exposures: examining the presence of interaction. Kidney Int. 2009; 75: 677–681 [DOI] [PubMed] [Google Scholar]
- 32. Aiken LS, West S G. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 33. Helm R, Mark A. Analysis and evaluation of moderator effects in regression models: state of art, alternatives and empirical example. Rev Manage Sci. 2012;6(4):307–332. 10.1007/s11846-010-0057-y [Google Scholar]
- 34. Blazer DG, Fillenbaum G, Burchett B. The APOE-E4 allele and the risk of functional decline in a community sample of African American and white older adults. J Gerontol A Biol Sci Med Sci. 2001; 56: M785–M789 [DOI] [PubMed] [Google Scholar]
- 35. Albert SM, Gurland B, Maestre G, Jacobs DM, Stern Y, Mayeux R. APOE genotype influences functional status among elderly without dementia. Am J Med Genet. 1995; 60: 583–587 [DOI] [PubMed] [Google Scholar]
- 36. Zeng Y, Hughes CL, Lewis MA, Li J, Zhang F. Interactions between life stress factors and carrying the APOE4 allele adversely impact self-reported health in old adult. J Gerontol A Biol Sci Med Sci. 2011; 66A: 1054–1061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Talmud PJ, Bujac SR, Hall S, Miller GJ, Humphries SE. Substitution of asparagine for aspartic acid at residue 9 (D9N) of lipoprotein lipase markedly augments risk of ischaemic heart disease in male smokers. Atherosclerosis. 2000; 149: 75–81 [DOI] [PubMed] [Google Scholar]
- 38. Ryff CD, Singer BH. Social environments and the genetics of aging: advancing knowledge of protective health mechanisms. J Gerontol B Psychol Sci Soc Sci. 2005; 60 Spec No 1: 12–23 [DOI] [PubMed] [Google Scholar]
- 39. Harvey M. Intuitive Biostatistics, 2nd ed. Oxford, United Kingdom: Oxford University Press; 1995. [Google Scholar]
- 40. McDonald JH. Handbook of Biological Statistics, 2nd ed Baltimore, MD: Sparky House Publishing; 2009: 319 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.