Abstract
Background
More than half of US adults use dietary supplements. Some reports suggest that supplement users have higher vitamin intakes from foods than nonusers, but this observation has not been examined using nationally representative survey data.
Objective
The purpose of this analysis was to examine vitamin intakes from foods by supplement use and how dietary supplements contribute to meeting or exceeding the Dietary Reference Intakes for selected vitamins using data from the National Health and Nutrition Examination Survey among adults (aged ≥19 years) in 2003–2006 (n=8,860).
Results
Among male users, mean intakes of folate and vitamins A, E, and K from food sources were significantly higher than among nonusers. Among women, mean intakes of folate and vitamins A, C, D, and E from foods were higher among users than nonusers. Total intakes (food and supplements) were higher for every vitamin we examined among users than the dietary vitamin intakes of nonusers. Supplement use helped lower the prevalence of intakes below the Estimated Average Requirement for every vitamin we examined, but for folic acid and vitamins A, B-6, and C, supplement use increased the likelihood of intakes above the Tolerable Upper Intake Level.
Conclusions
Supplement use was associated with higher mean intakes of some vitamins from foods among users than nonusers, but it was not associated with the prevalence of intakes less than the Estimated Average Requirement from foods. Those who do not use vitamin supplements had significantly higher prevalence of inadequate vitamin intakes; however, the use of supplements can contribute to excess intake for some vitamins.
Keywords: Dietary supplements, NHANES, Vitamins, Users and non-users of supplements
More than half of adults use dietary supplements in the United States (1), primarily in the form of multivitamins with or without minerals (2). Paradoxically, dietary supplement users tend to have higher intakes of some vitamins from food sources than people who do not use supplements (3,4), perhaps in part because they consume more fruits and vegetables (4,5).
Dietary supplements can provide large amounts of micro-nutrients to the diet. For example, in the Multiethnic Cohort Study (6), multivitamin dietary supplement users consumed the Recommended Dietary Allowance for thiamin; riboflavin; niacin; vitamins A, B-6, B-12, and E; and folate from the supplements alone. Thus, the use of dietary supplements has the potential to lower the prevalence of inadequate dietary intakes among adults for many micronutrients (3,7,8). However, dietary supplement use also has to potential to increase the risk of intakes above the tolerable upper intake level (UL) (9,10).
Previous nationally representative survey data (1994–1996) have only been examined for differences in vitamin intakes from foods between users and nonusers of dietary supplements among older adults (4). Since the authors published these data, the use of dietary supplements has increased dramatically in the United States (11). In addition, research is needed to examine adults’ vitamin intakes by supplement use across all age groups. Furthermore, it is important to understand whether those who use supplements use them to avoid nutrient deficiencies or whether they contribute to risk of excess intakes. Therefore, we examined vitamin intakes from food sources by dietary supplement use and assessed how dietary supplements contributed to meeting or exceeding the Dietary Reference Intakes for selected vitamins in the National Health and Nutrition Examination Survey (NHANES) 2003–2006.
METHODS
Study Population
The National Center for Health Statistics of the Centers for Disease Control and Prevention collects NHANES data. Written informed consent was obtained for all participants and the survey protocol was approved by the Research Ethics Review Board at the National Center for Health Statistics. We combined data from NHANES 2003–2004 and 2005–2006 for these analyses (12). The combined sample included 18,063 participants who had provided 24-hour dietary intake data. We excluded those aged <19 years (n=7,962) and pregnant and/or lactating women (n=1,241). The final analytic sample size was 8,860 people aged ≥19 years.
Dietary Intake
NHANES participants completed an in-person household interview and underwent a health examination in a mobile examination center that included providing an in-person 24-hour dietary recall. Survey personnel collected a second 24-hour dietary recall by telephone approximately 3 to 10 days after the health examination. The collection of both 24-hour recalls used the US Department of Agriculture’s automated multiple-pass method (13,14).
Survey personnel collected dietary supplement use information during the household interview as part of the dietary supplement questionnaire (12). This questionnaire assesses participants’ use of vitamins, minerals, herbs, and other dietary supplements during the past 30 days. Survey personnel also collected detailed information about the type, consumption frequency, duration, and amount of each reported dietary supplement that respondents took. The average daily intake of vitamins from dietary supplements was calculated for individuals using the number of days that supplement use was reported, the reported amount taken per day, and the serving size unit from the product label; the details on these procedures are available elsewhere (7,8).
Operational Definitions
We defined nonusers of dietary supplements as those who did not report taking a dietary supplement within the past 30 days. We describe dietary intakes for nonusers based on intakes from foods alone. We defined users of dietary supplements as those who reported taking a dietary supplement that contained a given vitamin within the past 30 days. For example, a vitamin C user was someone who took a multivitamin containing vitamin C or a dietary supplement containing vitamin C only. We examined the dietary intakes (ie, from foods only) of users and compared these intakes to those of nonusers. We also calculated total vitamin intakes, which we defined for dietary supplement users as vitamin intakes from food sources plus vitamin intakes from dietary supplements.
The prevalence of inadequate dietary intakes of a group was determined using the Estimated Average Requirement (EAR) cut-point method for all vitamins (15). The cut-point method requires more than one 24-hour dietary recall to adjust for individual variation. The EAR cut-point method assumes that there is no correlation between intakes and requirements; the variance in intakes is greater than the variance of requirements; and the distribution of requirements is symmetrical around the EAR. If these assumptions are met, the number of individuals with usual intakes below the EAR is proportionate to the prevalence of the group with inadequate intakes.
Vitamin Bioequivalence for Folate, Retinol, and Tocopherol
Folic acid does not occur naturally in the food supply but is the form of the vitamin that manufacturers use to fortify foods and in dietary supplements. The bioavailability of food folate is much lower than that of folic acid in fortified foods and dietary supplements. For this reason, the Food and Nutrition Board of the National Academies developed the dietary folate equivalent to reflect this differential bioavailability (16). The EAR for folate is expressed in dietary folate equivalents. The Food and Nutrition Board established an UL for folic acid only.
The Food and Nutrition Board established the EAR for vitamin A in micrograms of retinol activity equivalents to account for the different biological activities of retinol and the provitamin-A carotenoids (17). The UL for vitamin A applies only to micrograms retinol and does not include the carotenoids. The Dietary Reference Intake for vitamin E is described in milligrams of α-tocopherol (18). The UL for vitamin E is only for supplemental sources and does not include vitamin E that occurs naturally in foods.
Statistical Analysis
We adjusted the 24-hour dietary recall data for within-person variability and other covariates using the National Cancer Institute (NCI) method (19); the amount-only part of the NCI method (ie, not the frequency of intake that applies to usual intake of foods) is applicable to estimates of usual nutrient intakes. The first step in the NCI method includes a preliminary data adjustment to shift the observed vitamin intakes from the 24-hour dietary recalls away from zero (if necessary) and the incorporation of the NHANES survey weights, which make the estimates nationally representative. The method removes the effect of the sequence of the 24-hour dietary from the estimated nutrient intake distribution (day 1 or day 2). We also adjusted for the day of the week that the survey personnel collected the 24-hour recall data, which we dichotomized as weekend (Friday through Sunday) or weekday (Monday through Thursday). The final covariate was the use of dietary supplements. Additional details on the NCI method are available elsewhere (19), and the software macros necessary to fit this model and to estimate usual intake distributions are available on the NCI Web site (20).
We performed all statistical analyses using SAS (version 9.3, 2008, SAS Institute Inc, Cary, NC) software. We used sample weights to account for differential nonresponse and noncoverage and to adjust for planned oversampling of some groups. We estimated mean usual dietary and total vitamin intakes. We compared mean usual dietary intakes of vitamins between dietary supplement users and nonusers and the proportion meeting the EAR and exceeding the UL by computing a Z statistic. We set significance at a Bonferroni-corrected P value of <0.003. A Bonferroni adjusted P value is calculated by dividing the traditional P value of 0.05 by the number of statistical test performed, we compared eight vitamins by sex (n=16 tests).
RESULTS
Mean Dietary Intakes by Dietary Supplement Use Category
Among men when age groups were combined, the mean intakes of folate, vitamin A, vitamin E, and vitamin K from food sources were significantly higher among those who used dietary supplements than those who did not (Table 1). We found no differences between male users and nonusers of dietary supplements for vitamins B-6, B-12, C, and D. Mean intakes by age groups can be found in Table 2 (available online at www.andjrnl.org). In women, dietary intakes of folate and vitamins A, C, D, and E from foods were significantly higher among those who used dietary supplements than among non-users. Although we examined thiamin, riboflavin, and niacin, we found no significant differences in dietary intakes from foods between male or female users and nonusers (data not shown). As expected, mean total vitamin intakes were higher for every vitamin we examined (including thiamin, riboflavin, and niacin) among both male and female supplement users than among nonusers (Table 1).
Table 1.
Vitamin intakes (mean ± standard error [SE]) by adults who do not use dietary supplements (nonusers), dietary intakes of consumers of dietary supplements (users–foods), and total intakes from diet and supplemental intakes (users–total) of consumers of dietary supplements among adults (aged 19 y and older) in the United States, 2003–2006a
| Vitamin | Men
|
Women
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-users
|
Users–Foods
|
Users–Total
|
Non-users
|
Users–Foods
|
Users–Total
|
|||||
| Mean ± SE | n | Mean ± SE | n | Mean ± SE | Mean ± SE | n | Mean ± SE | n | Mean ± SE | |
| Folate (dietary folate equivalent) | 603 ± 11x | 3,152 | 663 ± 11y | 1,407 | 1,289 ± 14z | 437 ± 9x | 2,677 | 492 ± 11y | 1,624 | 1,200 ± 29z |
| Vitamin B-6 (mg) | 2.3 ± 0.03x | 3,138 | 2.4 ± 0.05x | 1,421 | 14.0 ± 1.4y | 1.6 ± 0.03a | 2,665 | 1.7 ± 0.03a | 1,636 | 15.4 ± 0.9y |
| Vitamin B-12 (μg) | 6.6 ± 0.2x | 3,131 | 6.4 ± 0.2x | 1,428 | 66 ± 6b | 4.1 ± 0.1a | 2,662 | 4.4 ± 0.1a | 1,639 | 72 ± 8y |
| Vitamin A (retinal activity equivalent) | 615 ± 15x | 3,187 | 722 ± 20y | 1,372 | 1,957 ± 52c | 501 ± 13a | 2,743 | 617 ± 15b | 1,558 | 1,852 ± 66z |
| Vitamin C (mg) | 89 ± 2x | 2,978 | 99 ± 4x | 1,581 | 392 ± 38b | 71 ± 2a | 2,492 | 85 ± 2b | 1,809 | 375 ± 15z |
| Vitamin D (μg) | 5.1 ± 0.2x | 3,175 | 5.3 ± 0.2z | 1,384 | 13.7 ± 0.3b | 3.5 ± 0.1a | 2,604 | 4.3 ± 0.2b | 1,697 | 14.3 ± 0.5z |
| Vitamin E (α-tocopherol equivalent) | 7.7 ± 0.1x | 3,044 | 8.8 ± 0.2y | 1,515 | 96 ± 5.9z | 5.9 ± 0.1x | 2,553 | 6.7 ± 0.2y | 1,748 | 110 ± 6.1z |
| Vitamin K (μg) | 85 ± 3x | 3,447 | 104 ± 5y | 1,112 | 125 ± 5z | 81.7 ± 2.6a | 3,250 | 95.2 ± 4.2a | 1,051 | 12 ± 4.4y |
Sample sizes differ for each vitamin because the supplements that respondents used contained different combinations of the vitamins studied.
Different subscript letters (x, y, z) denote significant differences between categories of use from the diet and differences between dietary and total intakes, Bonferroni-corrected P value ≤0.003.
Table 2.
Mean ± standard error (SE) dietary intakes for selected vitamins from food sources among users and nonusers of dietary supplements by the Dietary Reference Intake age groups and sex among US adults, 2003–2006
| Group | Age (y) | Usual Intake—Folate (Dietary Folate Equivalent)
|
Usual Intake—Vitamin C (mg)
|
Usual Intake—Vitamin B-6 (mg)
|
Usual Intake—Vitamin B-12 (mg)
|
Usual Intake—Vitamin A
|
Usual Intake—Vitamin D (μg)
|
Usual Intake—Vitamin K (μg)
|
Usual Intake—Vitamin E (α-tocopherol Equivalents)
|
||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
||||||||||||||||||
| n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | ||
| Men | 19–30 | 885 | 665 ± 26 | 212 | 694 ± 28 | 844 | 88 ± 4 | 253 | 98 ± 7 | 886 | 2.4 ± 0.1 | 211 | 2.6 ± 0.12 | 884 | 6.3 ± 0.3 | 213 | 7.1 ± 0.4 | 887 | 566 ± 23 | 210 | 691 ± 35* | 887 | 4.8 ± 0.2 | 210 | 5.3 ± 0.4 | 929 | 77 ± 3.4 | 168 | 109 ± 8.1* | 881 | 7.6 ± 0.2 | 216 | 9.2 ± 0.3* |
| 31–50 | 1,023 | 616 ± 15 | 416 | 674 ± 24 | 980 | 89 ± 4 | 459 | 96 ± 4 | 1,015 | 2.3 ± 0.0 | 424 | 2.5 ± 0.06* | 1,015 | 6.4 ± 0.5 | 424 | 6.6 ± 0.2 | 1,033 | 615 ± 24 | 406 | 711 ± 26 | 1,030 | 5.2 ± 0.3 | 409 | 5.2 ± 0.3 | 1,106 | 90 ± 3.5 | 333 | 103 ± 4.9 | 1,006 | 8.1 ± 0.2 | 433 | 9.4 ± 0.3* | |
| 51–70 | 771 | 539 ± 13 | 444 | 629 ± 22 | 729 | 90 ± 4 | 486 | 100 ± 6 | 771 | 2.1 ± 0.1 | 444 | 2.3 ± 0.09 | 766 | 6.0 ± 0.4 | 449 | 6.1 ± 0.3 | 794 | 620 ± 17 | 421 | 720 ± 34 | 783 | 5.0 ± 0.2 | 432 | 5.3 ± 0.3 | 857 | 89 ± 3.2 | 358 | 105 ± 8.9 | 738 | 7.3 ± 0.2 | 477 | 8.7 ± 0.4* | |
| 71+ | 473 | 522 ± 14 | 335 | 583 ± 16* | 425 | 97 ± 5 | 383 | 108 ± 6 | 466 | 2.1 ± 0.1 | 342 | 2.1 ± 0.06 | 466 | 6.5 ± 1.0 | 342 | 5.7 ± 0.2 | 473 | 776 ± 34 | 335 | 771 ± 32 | 475 | 5.8 ± 0.3 | 333 | 5.6 ± 0.3 | 555 | 78 ± 3.5 | 253 | 97 ± 5.6 | 419 | 6.7 ± 0.3 | 389 | 7.4 ± 0.3 | |
| Women | 19–30 | 687 | 446 ± 15 | 226 | 503 ± 30 | 662 | 69 ± 4 | 251 | 70 ± 4 | 682 | 1.5 ± 0.1 | 231 | 1.6 ± 0.07 | 688 | 3.7 ± 0.2 | 225 | 4.5 ± 0.3 | 694 | 411 ± 16 | 219 | 548 ± 34* | 691 | 3.0 ± 0.2 | 222 | 4.0 ± 0.3 | 798 | 68 ± 3.1 | 115 | 73 ± 8.4 | 683 | 5.8 ± 0.2 | 230 | 6.4 ± 0.3 |
| 31–50 | 913 | 450 ± 17 | 437 | 503 ± 22 | 855 | 70 ± 4 | 495 | 81 ± 5 | 898 | 1.6 ± 0.03 | 452 | 1.7 ± 0.04 | 906 | 4.1 ± 0.1 | 444 | 4.4 ± 0.2 | 937 | 504 ± 17 | 413 | 628 ± 30* | 906 | 3.6 ± 0.2 | 444 | 4.2 ± 0.2 | 1,098 | 86 ± 3.7 | 252 | 106 ± 7.1 | 889 | 6.2 ± 0.2 | 461 | 7.0 ± 0.2 | |
| 51–70 | 668 | 416 ± 15 | 583 | 489 ± 18 | 628 | 69 ± 3 | 623 | 90 ± 3* | 675 | 1.5 ± 0.1 | 576 | 1.7 ± 0.05 | 666 | 4.0 ± 0.2 | 585 | 4.3 ± 0.1 | 709 | 543 ± 23 | 542 | 620 ± 23 | 644 | 3.5 ± 0.2 | 607 | 4.2 ± 0.2 | 849 | 89 ± 3.9 | 402 | 96 ± 5.3 | 639 | 5.7 ± 0.2 | 612 | 6.9 ± 0.2* | |
| 71+ | 409 | 416 ± 15 | 378 | 462 ± 17 | 347 | 82 ± 4 | 440 | 95 ± 3 | 410 | 1.6 ± 0.0 | 377 | 1.6 ± 0.05 | 402 | 4.3 ± 0.2 | 385 | 4.5 ± 0.2 | 403 | 577 ± 23 | 384 | 665 ± 22 | 363 | 4.3 ± 0.2 | 424 | 4.8 ± 0.1 | 505 | 79 ± 4.2 | 282 | 84 ± 5.8 | 342 | 5.3 ± 0.2 | 445 | 6.0 ± 0.2 | |
Significantly different at a Bonferroni-adjusted P value ≤0.003.
Prevalence of Inadequate Intakes from Food Sources Only
The prevalence of inadequate dietary intakes (ie, intakes below the EAR) was significantly lower among male supplement users than nonusers for vitamins A and E (Table 3). We found no differences in the prevalence of inadequate vitamin intakes from food sources alone among men for folate or vitamins B-6, B-12, C, or D. Among women, we observed a lower prevalence of inadequate dietary intakes of vitamins A and C for users of dietary supplements than for nonusers. We observed no differences in the prevalence of inadequate vitamin intakes from food sources among women for folate and vitamins B-6, B-12, D, and E.
Table 3.
The prevalence (mean ± standard error [SE]) of inadequate vitamin intakes as assessed using the Estimated Average Requirement (EAR) among adults (aged ≥19 y) in the United States, 2003–2006a
| Vitamin | Men
|
Women
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-users
|
Users–Foods
|
Users–Total | Non-users
|
Users–Foods
|
Users–Total | |||||
| Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | |||
| Folate (dietary folate equivalent) | 6 ± 1x | 3,152 | 2.7 ± 0.7x | 1,407 | 0.1 ± 0.02y | 23 ± 2x | 2,677 | 18 ± 2x | 1,624 | 0.7 ± 0.1y |
| Vitamin B-6 (mg) | 6 ± 1x | 3,138 | 6 ± 1x | 1,421 | 0.08 ± 0.04y | 27 ± 3x | 2,665 | 21 ± 2.4x | 1,636 | 0.5 ± 0.1y |
| Vitamin B-12 (μg) | 0.6 ± 0.3x | 3,131 | 0.5 ± 0.2x | 1,428 | 0 ± 0a | 8 ± 1.4x | 2,662 | 5.7 ± 1.5x | 1,639 | 0.1 (0)y |
| Vitamin A (retinol activity equivalent) | 59 ± 2x | 3,187 | 43 ± 3y | 1,372 | 2.7 ± 0.4z | 56 ± 2x | 2,743 | 38 ± 2.3y | 1,558 | 2.0 ± 0.3z |
| Vitamin C (mg) | 48 ± 2x | 2,978 | 41 ± 3x | 1,581 | 2.5 ± 0.4y | 47 ± 2x | 2,492 | 34 ± 2y | 1,809 | 2.5 ± 0.4z |
| Vitamin D (μg) | 93 ± 1x | 3,175 | 93 ± 1x | 1,384 | 25 ± 2y | 98 ± 0.4x | 2,604 | 97 ± 1x | 1,697 | 25 ± 1.1y |
| Vitamin E (α-tocopherol equivalent) | 93 ± 1x | 3,044 | 85 ± 2y | 1,515 | 4 ± 0.4z | 99 ± 0.5x | 2,553 | 96 ± 1x | 1,748 | 7 ± 0.6y |
Sample sizes differ for each vitamin because the supplements that respondents used contained different combinations of the vitamins studied.
Different subscript letters (x, y, z) denote significant differences between categories of use from the diet and differences between dietary and total intakes, Bonferroni-corrected P value ≤0.003.
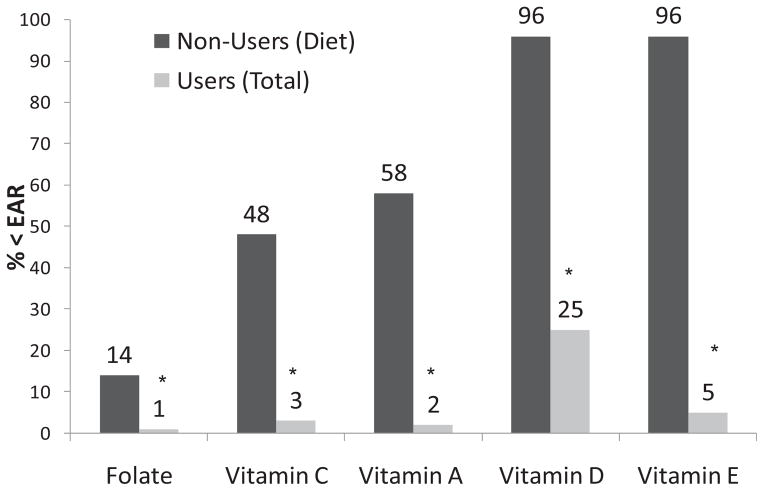
Comparisons of Intakes from Food Sources of Nonusers to Total Intakes of Users
For adults (combined sexes), when we compared the prevalence of at-risk intakes between the dietary intakes of nonusers (from foods only) and the total intakes of users (from foods and supplements), significantly more nonusers were at risk for inadequacy for every vitamin that we examined (Figure). The difference in prevalence between users and nonusers was most notable for the fat-soluble vitamins A, E, and D. When we combined data from both sexes, the prevalence of not meeting the EAR was 16%±1% for vitamin B-6 and 4%±0.8% for vitamin B-12 among nonusers and <0.5% for both vitamins in users (data not shown).
Figure.
Prevalence of vitamin intakes below the Estimated Average Requirement (EAR) by dietary supplement use among adults (sexes combined) in the United States, 2003–2006. *Denotes statistically significant difference between users and non-users of dietary supplements, P<0.003.
Among men, the prevalence of inadequate vitamin intakes from food sources among nonusers of dietary supplements was significantly higher than the prevalence of inadequate total vitamin intakes among dietary supplement users for every vitamin that we examined, with the exception of vitamin B-12. Data from men showed that <1% had diet or total vitamin B-12 intakes below the EAR. Among women, the prevalence of inadequate vitamin intakes from food sources alone among nonusers of dietary supplements was significantly higher than the prevalence of inadequate total vitamin intakes among dietary supplement users for every vitamin we examined. Regardless of sex, the most notable differences were among the fat-soluble vitamins D and E, whose inadequate status prevalence estimates dropped from more than 95% in nonusers to 25% for vitamin D and 5% for vitamin E among users (Table 3).
Among adults aged 19 to 30 years the prevalence of at-risk dietary intakes was almost 70% for vitamin A, but among supplement users this prevalence was only 4% (Table 4, available online at www.andjrnl.org). Approximately 35% to 40% of older women who did not use dietary supplements containing vitamin B-6 had inadequate intakes, compared with <1% of dietary supplement users. About 12% of women aged 19 to 30 years had inadequate dietary intakes of vitamin B-12, compared with <0.5% of women in this age group who used supplements. Overall, about 40% to 50% of nonusers had dietary vitamin C intakes associated with a risk of not meeting the EAR, compared with <5% of supplement users. More than 90% of adults who did not use supplements had inadequate dietary intakes of vitamins D and E from foods. Although the prevalence of inadequate vitamin D and E intakes was substantially lower in supplement users, about 40% of adults aged 19 to 30 years had inadequate vitamin D total intakes and about 13% had inadequate total vitamin E intakes.
Table 4.
Prevalence (% ± standard error [SE]) of inadequate intakes from food sources for nonusers, and from total intakes for dietary supplement users as assessed using the Estimated Average Requirement (EAR) among adults (≥19 y) by the Dietary Reference Intake age groups and sex in the United States, 2003–2006
| Age (y) | Usual Intake—Folate (Dietary Folate Equivalents)
|
Usual Intake—Vitamin C (mg)
|
Usual Intake—Vitamin B-6 (mg)
|
Usual Intake—Vitamin B-12 (mg)
|
Usual Intake—Vitamin A
|
Usual Intake—Vitamin D (μg)
|
Usual Intake—Vitamin E (α-tocopherol Equivalents)
|
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
Non-users
|
Users
|
||||||||||||||||
| n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | n | % ± SE | ||
| Men | 19–30 | 885 | 4 ± 1.1 | 212 | 0.1 ± 0.1* | 844 | 49 ± 3 | 253 | 5.0 ± 0.8* | 886 | 2 ± 0.6 | 211 | 0.02 ± 0.02* | 884 | 0.6 ± 0.3 | 213 | 0.0 ± 0 | 887 | 65 ± 3 | 210 | 4.4 ± 1.3* | 887 | 94 ± 1 | 210 | 36 ± 4* | 881 | 94 ± 1 | 168 | 5.4 ± 1* |
| 31–50 | 1,023 | 4 ± 0.7 | 416 | 0.0 ± 0* | 980 | 49 ± 3 | 459 | 5.0 ± 1.0* | 1,015 | 2 ± 0.6 | 424 | 0.02 ± 0.02* | 1,015 | 0.6 ± 0.2 | 424 | 0.0 ± 0 | 1,033 | 59 ± 3 | 406 | 3.2 ± 0.7* | 1,030 | 92 ± 2 | 409 | 30 ± 3* | 1,006 | 91 ± 2 | 333 | 4.3 ± 1* | |
| 51–70 | 771 | 8 ± 1.3 | 444 | 0.0 ± 0* | 729 | 48 ± 3 | 486 | 2.8 ± 0.7* | 771 | 14 ± 2 | 444 | 0.19 ± 0.13* | 766 | 0.9 ± 0.4 | 449 | 0.0 ± 0 | 794 | 58 ± 2 | 421 | 1.7 ± 0.5* | 783 | 93 ± 1 | 432 | 19 ± 2* | 738 | 95 ± 1 | 358 | 2.4 ± 1* | |
| 71+ | 473 | 8 ± 1.1 | 335 | 0.1 ± 0.1* | 425 | 43 ± 4 | 383 | 1.3 ± 0.3* | 466 | 15 ± 2 | 342 | 0.13 ± 0.07* | 466 | 0.4 ± 0.2 | 342 | 0.0 ± 0 | 473 | 39 ± 3 | 335 | 0.8 ± 0.3* | 475 | 89 ± 2 | 333 | 10 ± 1* | 419 | 97 ± 1 | 253 | 3.4 ± 1* | |
| Women | 19–30 | 687 | 26 ± 2.5 | 226 | 0.7 ± 0.3* | 662 | 49 ± 4 | 251 | 5.0 ± 1.2* | 682 | 23 ± 3 | 231 | 0.34 ± 0.19* | 688 | 11.8 ± 2.5 | 225 | 0.1 ± 0.1* | 694 | 73 ± 3 | 219 | 3.9 ± 1.1* | 691 | 99 ± 0.5 | 222 | 39 ± 4* | 683 | 99 ± 1 | 115 | 12.6 ± 2* |
| 31–50 | 913 | 21 ± 2.3 | 437 | 1.1 ± 0.4* | 855 | 48 ± 4 | 495 | 3.7 ± 0.8* | 898 | 19 ± 2 | 452 | 0.33 ± 0.16* | 906 | 6.8 ± 1.3 | 444 | 0.1 ± 0.1* | 937 | 55 ± 3 | 413 | 2.3 ± 0.6* | 906 | 98 ± 1 | 444 | 31 ± 2* | 889 | 98 ± 1 | 252 | 8.6 ± 2* | |
| 51–70 | 668 | 24 ± 3.3 | 583 | 0.5 ± 0.1* | 628 | 49 ± 3 | 623 | 1.3 ± 0.2* | 675 | 40 ± 5 | 576 | 0.58 ± 0.16* | 666 | 8.4 ± 1.9 | 585 | 0.1 ± 0* | 709 | 48 ± 3 | 542 | 1.6 ± 0.5* | 644 | 99 ± 0.5 | 607 | 20 ± 2* | 639 | 99 ± 1 | 402 | 4.3 ± 1* | |
| 71+ | 409 | 24 ± 2.7 | 378 | 0.4 ± 0.2* | 347 | 37 ± 4 | 440 | 0.7 ± 0.2* | 410 | 34 ± 4 | 377 | 0.59 ± 0.20* | 402 | 5.8 ± 2.0 | 385 | 0.0 ± 0* | 403 | 42 ± 3 | 384 | 0.8 ± 0.3* | 363 | 96 ± 1 | 424 | 15 ± 1* | 342 | 99 ± 1 | 282 | 4.4 ± 1* | |
Significantly different at a Bonferroni-adjusted P value ≤0.003.
Prevalence of Intakes Above the UL
This population did not have usual dietary intakes of vitamins from foods alone that were above the UL. However, when we examined total vitamin intakes among users, we found that several total vitamin intakes exceeded the UL (Table 5). Specifically, about 7% of adult supplement users exceeded the UL for folic acid and 5% of adults older than age 50 years exceed the vitamin A UL. With the exception of women aged 71 years or older, <5% of adult B-6 supplement users had total intakes above the UL. About 2% of adult dietary supplement users exceeded the UL for vitamin C. Less than 0.7% of supplement users had total intakes that exceeded the UL for vitamins D and E (data not shown).
Table 5.
The prevalence of total dietary intakes above the Tolerable Upper Intake Level (UL) among users of dietary supplements in the United States (aged ≥19 y), 2003–2006
| User group | Age (y) | Folic acid (n=3,031) | Vitamin A (n=2,930) | Vitamin B-6 (n=3,057) | Vitamin C (n=3,390) |
|---|---|---|---|---|---|
| ←---% ± standard error---→ | |||||
| All | ≥19 | 7.0 ± 0.5 | 3.0 ± 0.5 | 3.5 ± 0.4 | 1.6 ± 0.3 |
| 19–30 | 8.1 ± 1.4 | 1.2 ± 0.6 | 1.3 ± 0.6 | 0.9 ± 0.7 | |
| 31–50 | 5.7 ± 0.7 | 2.0 ± 0.7 | 3.3 ± 0.7 | 1.9 ± 0.6 | |
| 51–70 | 7.8 ± 0.9 | 3.9 ± 0.9 | 3.9 ± 0.9 | 1.8 ± 0.6 | |
| ≥71 | 6.6 ± 1.0 | 5.2 ± 1.1 | 5.5 ± 1.1 | 1.3 ± 0.4 | |
| Men | ≥19 | 6.3 ± 0.6 | 2.8 ± 0.5 | 3.0 ± 0.6 | 1.6 ± 0.5 |
| 19–30 | 5.1 ± 1.9 | 1.5 ± 0.8 | 1.1 ± 0.8 | 1.6 ± 1.4 | |
| 31–50 | 5.4 ± 1.0 | 1.3 ± 0.5 | 2.7 ± 0.8 | 1.8 ± 0.8 | |
| 51–70 | 7.2 ± 1.0 | 4.3 ± 1.3 | 3.8 ± 1.6 | 1.5 ± 0.6 | |
| ≥71 | 8.4 ± 1.4 | 4.9 ± 1.2 | 4.6 ± 1.3 | 1.6 ± 0.6 | |
| Women | ≥19 | 7.5 ± 0.9 | 3.2 ± 0.7 | 3.9 ± 0.6 | 1.6 ± 0.4 |
| 19–30 | 10.7 ± 2.4 | 0.8 ± 0.8 | 1.5 ± 0.8 | 0.3 ± 0.3 | |
| 31–50 | 6.2 ± 1.2 | 2.7 ± 1.2 | 3.9 ± 1.2 | 2.0 ± 0.9 | |
| 51–70 | 8.2 ± 1.3 | 3.7 ± 1.1 | 4.0 ± 1.1 | 2.0 ± 0.8 | |
| ≥71 | 5.6 ± 1.4 | 5.4 ± 1.7 | 6.1 ± 1.4 | 1.0 ± 0.5 | |
DISCUSSION
More than half of adults (53%) reported use of a dietary supplement in NHANES 2003–2006 (1), and the most frequently reported supplement was a multivitamin (11). The usual mean vitamin intakes from food sources were higher for supplement users when compared with those of nonusers for some vitamins in US adults: folate and vitamins A and E. In addition, among men, vitamin K intake from foods was higher among users than nonusers and among women the same was true for vitamins C and D.
Although mean intakes of vitamins from food sources differed by the use of supplements, very little difference was observed in the prevalence of inadequate vitamin intakes from foods alone between users and nonusers of supplements with the exception of vitamin A (and vitamin C in women and vitamin E in men). We recently examined mineral intakes from food sources between users and nonusers of dietary supplements in NHANES 2003–2006 (21). We observed both higher mineral intakes from food sources and a lower prevalence of inadequate mineral intakes from foods for most minerals (especially in women) among US adults who used dietary supplements. From the public health perspective, the prevalence of inadequate intakes from foods is more meaningful than an examination of the differences in mean intakes. For minerals, there are true differences (ie, lower prevalence of inadequate mineral intakes) between the users and non-users of mineral containing supplements in their intakes of minerals from foods. In contrast, among users of vitamin supplements and nonusers such differences were not apparent, with the exception of vitamin A from food sources. That is, those who chose mineral supplements did have a significantly lower prevalence of inadequate mineral intakes from foods alone, but those who chose vitamin supplements did not necessarily have different prevalence of inadequate vitamin intakes from food sources alone. A dramatically lowered prevalence of inadequate total intakes (diet plus supplements) was observed across every vitamin that we examined among dietary supplement users when compared to the vitamin intakes from foods of nonusers. Thus, those who do not use vitamin dietary supplements have a significantly higher prevalence of inadequate vitamin intakes among US adults—especially for vitamins A, C, D, and E.
A large proportion of nonusers did not meet the EAR for vitamin A, and dietary intakes of vitamin A from foods were consistently higher among users than nonusers as well. Vitamin A exists in two forms, retinol found primarily in animal products, and carotenoids found primarily in vegetables. Both forms of the vitamin have biological activity and both were considered in our estimates. More than 90% of adults who did not use dietary supplements in our study failed to meet the recommended intake levels for vitamins E and D. When we examined supplement users, we observed a much lower prevalence of inadequate intakes for vitamin E. However, even with supplement use, vitamin D intakes were still low, placing some at risk, particularly older adults. Because vitamin D can be made in vivo from exogenous ultraviolet light exposure, the vitamin D nutritional status of US adults cannot be determined simply by dietary intake estimates alone. The EAR for vitamin D intakes does not reflect the influence of ultraviolet light exposure (22). Future work should address the serum 25-hydroxyvitamin D status of dietary supplement users and nonusers separately.
Our results show that about 12% of young adult women (aged 19 to 30 years) do not meet the EAR for vitamin B-12. Previous studies have shown that women in this age group also have lower serum vitamin B-12 concentrations (23). Oral contraceptive use seems to be associated with lower serum vitamin B-12 in younger women in NHANES (23); but our data suggest that lower dietary exposure may also be involved. Given the role of vitamin B-12 in red blood cell formation, neurological function, and DNA synthesis further investigation of these trends among young women may be warranted.
Because dietary supplements have the potential to greatly influence nutrient intake distributions, it is not surprising that although supplement users in our study had a lower prevalence of inadequate intakes, they also had a higher prevalence of excessive intakes (higher than the UL) for folic acid and vitamin A and, to a lesser extent, for vitamins B-6 and C. Also, 5% of older adults (aged 71 years and older) using supplements exceed the UL for vitamin A. Excess vitamin A is associated with headaches, liver damage, and reduced bone strength, all of which would be of concern. High retinol exposure is known to be teratogenic (17); about 2% of reproductive aged women using supplements exceeded the UL in this study. About 11% of women aged 19 to 30 years who used dietary supplements exceed the UL for folic acid, which is 1,000 μg. Public health experts believe that women of reproductive age need to increase their folic acid intakes because of the strong evidence that folic acid can prevent neural tube defects in children (24). Excessive folic acid intakes may mask the hematological signs of a vitamin B-12 deficiency (16) and although this deficiency is more prevalent in older adults, it deserves attention because of the low vitamin B-12 intake in young women.
Sebastian and colleagues (3) examined vitamin intakes by dietary supplement use in older adults in the Continuing Survey of Food Intakes by Individuals (1994–1996). The only difference in vitamin intake from foods that these authors found was that male supplement users (aged 51 to 70 years) had higher vitamin C intakes than nonusers and female supplement users (aged 51 years or older) had higher vitamin C, vitamin B-6, folate, and vitamin E intakes than nonusers. We found many more differences in the vitamin intakes from foods between dietary supplement users and nonusers than the authors of this earlier report, who also used nationally representative data (3). However, we examined all adult age groups, whereas the earlier report focused exclusively on older adults. Also, dietary supplement use increased dramatically after the passage of the Dietary Supplement Health and Education Act of 1994, so Sebastian and colleagues collected their data at a time when supplement use was lower than its current level.
Tetens and colleagues (25) have recently published estimates of micronutrient intakes by supplement use from the Danish National Birth Cohort. Like our study, Tetens and colleagues also found that the differences in nutrient intakes were much more evident among women than men (25). This is an interesting finding, and may indicate that female supplement users exhibit different eating patterns (ie, more nutrient dense) than male supplement users.
A strength of our investigation is that we examined usual vitamin intakes that we had adjusted for the effects of within-person variability. We also used the recommended method of analysis for total nutrient intakes, which is to adjust the dietary data first and then add the average supplement dose (26). However, the adjustment procedures rely on assumptions, chief of which are that nutrient intake from food sources on the 24-hour dietary recalls are unbiased and that the self-reported dietary supplement intake reflects true long-term supplement intake. Another assumption is that labeled levels of vitamins in dietary supplements reflect the actual amounts contained in the supplements, even though some analytical data on dietary supplements suggest that actual levels exceed the labeled values for some vitamins (27,28).
CONCLUSIONS
Dietary supplements constitute an important source of vitamins for large segments of the adult population in the United States. In general, we observed that adults who use dietary supplements tend to already have higher mean vitamin intakes from foods than those who do not use supplements, but do not differ in the prevalence if inadequate vitamin intakes from food sources. Users of supplements had a significantly lower prevalence of inadequate total vitamin intakes than those who do not use supplements. Dietary supplement use remains a controversial public health strategy to improve nutrient intakes because, although this use is associated with lower prevalence of intakes below the EAR, supplement use is also associated with an increased risk of intakes above the UL. For this reason, Murphy and colleagues (9) suggested that supplement manufacturers try to better tailor the levels of nutrients in dietary supplements to help meet, but not exceed, nutrient needs.
Acknowledgments
FUNDING/SUPPORT
The original statistical analysis to separate fortified and enriched foods from other foods and dietary supplements used in this article was funded by the Fortification Committee of the International Life Sciences Institute, North American Branch. The International Life Sciences Institute was not involved in the interpretation or presentation of data for this work. This work was supported in part by resources from the US Department of Agriculture Research Service under agreement no. 58-1950-7-707 and the Office of Dietary Supplements at the National Institutes of Health.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
References
- 1.Bailey RL, Gahche JJ, Lentino CV, et al. Dietary supplement use in the United States, 2003–2006. J Nutr. 2011;141(2):261–266. doi: 10.3945/jn.110.133025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Radimer K, Bindewald B, Hughes J, Ervin B, Swanson C, Picciano MF. Dietary supplement use by US adults: Data from the National Health and Nutrition Examination Survey, 1999–2000. Am J Epidemiol. 2004;160(4):339–349. doi: 10.1093/aje/kwh207. [DOI] [PubMed] [Google Scholar]
- 3.Sebastian RS, Cleveland LE, Goldman JD, Moshfegh AJ. Older adults who use vitamin/mineral supplements differ from nonusers in nutrient intake adequacy and dietary attitudes. J Am Diet Assoc. 2007;107(8):1322–1332. doi: 10.1016/j.jada.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Foote JA, Murphy SP, Wilkens LR, Hankin JH, Henderson BE, Kolonel LN. Factors associated with dietary supplement use among healthy adults of five ethnicities: The Multiethnic Cohort Study. Am J Epidemiol. 2003;157(10):888–897. doi: 10.1093/aje/kwg072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Touvier M, Niravong M, Volatier JL, et al. Dietary patterns associated with vitamin/mineral supplement use and smoking among women of the E3N-EPIC cohort. Eur J Clin Nutr. 2009;63(1):39–47. doi: 10.1038/sj.ejcn.1602907. [DOI] [PubMed] [Google Scholar]
- 6.Park SY, Murphy SP, Martin CL, Kolonel LN. Nutrient intake from multivitamin/mineral supplements is similar among users from five ethnic groups: The Multiethnic Cohort Study. J Am Diet Assoc. 2008;108(3):529–533. doi: 10.1016/j.jada.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Bailey RL, Dodd KW, Gahche JJ, et al. Total folate and folic acid intake from foods and dietary supplements in the United States: 2003–2006. Am J Clin Nutr. 2010;91(1):231–237. doi: 10.3945/ajcn.2009.28427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey RL, Dodd KW, Goldman JA, et al. Estimation of total usual calcium and vitamin D intakes in the United States. J Nutr. 2010;140(4):817–822. doi: 10.3945/jn.109.118539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murphy SP, White KK, Park SY, Sharma S. Multivitamin-multimineral supplements’ effect on total nutrient intake. Am J Clin Nutr. 2007;85(suppl 1):280S–284S. doi: 10.1093/ajcn/85.1.280S. [DOI] [PubMed] [Google Scholar]
- 10.Bailey RL, McDowell MA, Dodd KW, Gahche JJ, Dwyer JT, Picciano MF. Total folate and folic acid intakes from foods and dietary supplements of US children aged 1–13 y. Am J Clin Nutr. 2010;92(2):353–358. doi: 10.3945/ajcn.2010.29652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gahche J, Bailey R, Burt V, et al. Dietary supplement use among U.S. adults has increased since NHANES III (1988–1994) NCHS Data Brief. 2011:61. [PubMed] [Google Scholar]
- 12.National Health and Nutrition Examination Survey SP. Questionnaire Component: Dietary Supplements Questionnaire Data, 2003–2004. National Center for Health Statistics; [Accessed April 1, 2010]. Web site. http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/dsq_c.pdf. [Google Scholar]
- 13.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136(10):2594–2599. doi: 10.1093/jn/136.10.2594. [DOI] [PubMed] [Google Scholar]
- 14.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 15.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes Applications in Dietary Assessment. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 16.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes For Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academies Press; 1998. [PubMed] [Google Scholar]
- 17.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Molybdenum, Nickel, Silicon, Vanadium and Zinc. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 18.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 19.Tooze JA, Midthune D, Dodd KW, et al. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106(10):1575–1587. doi: 10.1016/j.jada.2006.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Usual dietary intakes: The NCI method. National Cancer Institute; [Accessed August 1, 2009]. Web site. http://riskfactor.cancer.gov/diet/usualintakes/method.html. [Google Scholar]
- 21.Bailey RL, Fulgoni VL, Keast DR, Dwyer JT. Dietary supplement use is associated with higher intakes of minerals from food sources. Am J Clin Nutr. 2011;94:1376–1381. doi: 10.3945/ajcn.111.020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 23.Bailey RL, Carmel R, Green R, et al. Monitoring of vitamin B12 nutritional status in the United States using plasma methylmalonic acid and serum vitamin B12. Am J Clin Nutr. 2011;94:552–561. doi: 10.3945/ajcn.111.015222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992;327(26):1832–1835. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- 25.Tetens I, Biltoft-Jensen A, Spagner C, et al. Intake of micronutrients among Danish adult users and non-users of dietary supplements. Food Nutr Res. 2011:55. doi: 10.3402/fnr.v55i0.7153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garriguet D. Combining nutrient intake from food/beverages and vitamin/mineral supplements. Health Rep. 2010;21(4):71–84. [PubMed] [Google Scholar]
- 27.Dwyer JT, Holden J, Andrews K, et al. Measuring vitamins and minerals in dietary supplements for nutrition studies in the USA. Anal Bioanal Chem. 2007;389(1):37–46. doi: 10.1007/s00216-007-1456-z. [DOI] [PubMed] [Google Scholar]
- 28.Roseland JM, Holden JM, Andrews KW, et al. Dietary supplement ingredient database (DSID): Preliminary USDA studies on the composition of adult multivitamin/mineral supplements. J Food Comp Anal. 2008;21(suppl 1):S69–S77. doi: 10.1016/j.jfca.2007.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]