Abstract
Since its introduction in the People’s Republic of China in 1992, minimally invasive esophagectomy (MIE) has shown the classical advantages of minimally invasive surgery over its open counterpart. Like all pioneers of the technique, cardiothoracic surgeons in the People’s Republic of China claim that MIE has a lower risk of pulmonary infection, faster recovery, a shorter hospital stay, and a more rapid return to daily activities than open esophagectomy, while offering the same functional and oncologic results. There has been burgeoning interest in MIE in the People’s Republic of China since 1995. The last decade has witnessed nationwide growth in the application of MIE and yielded a significant amount of scientific data in support of its clinical merits and advantages. However, no prospective randomized controlled trials have actually investigated the benefits of MIE in the People’s Republic of China. Here we review the current data and state of the art MIE treatment for esophageal cancer in the People’s Republic of China.
Keywords: esophagectomy, minimally invasive esophagectomy, esophageal cancer, review
Introduction
The global incidence of esophageal cancer has increased by 50% in the past two decades.1,2 Advances in neoadjuvant and adjuvant chemotherapy and chemoradiotherapy have led to increasingly multimodal treatment for patients with esophageal cancer, which has decreased the rate of local recurrence and improved long-term survival for some patients. However, surgical resection with radical lymphadenectomy is regarded as one of the curative options for resectable esophageal cancer.3–6 Frequently, due consideration of surgical resection may not be given because of concerns with regard to the morbidity of open esophagectomy.
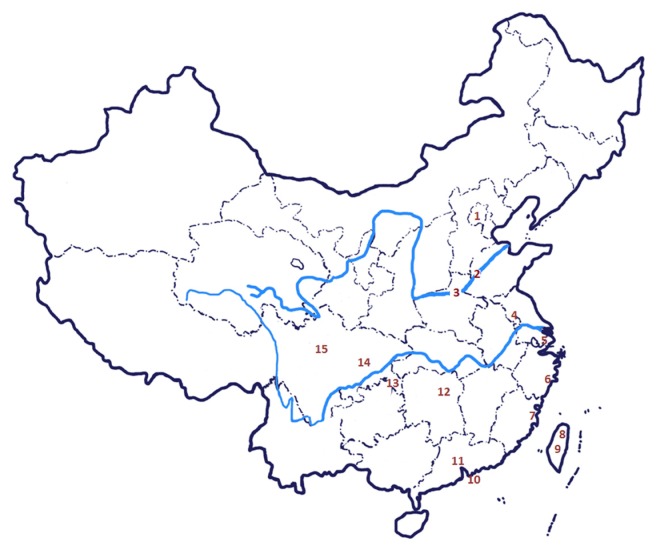
In an effort to decrease the morbidity associated with open esophagectomy, Chinese surgeons have adopted a minimally invasive approach to esophageal resection. Because of the potential advantages, including avoiding thoracotomy and laparotomy and reducing the rate of pulmonary infections (thus reducing the inpatient stay),7,8 minimally invasive esophagectomy (MIE) was introduced into clinical practice in Taiwan9 in 1992 at the same time as in Western countries,10–12 was gradually implemented, and is now a commonplace procedure in the People’s Republic of China (Figure 1), including in Beijing,13–15 Jinan in Shandong Province,16 Zhengzhou in Henan Province,17 Nanjing in Jiangsu Province,18 Shanghai,19–30 Taizhou in Zhejiang Province,31–33 Fuzhou in Fujian Province,34–36 Taipei9 and Taichung37 in Taiwan, Hongkong,38–40 Guangzhou in Guangdong Province,41,42 Changsha in Hunan Province,43 Chongqing,44,45 and Chengdu46–48 and Nanchong49 in Sichuan Province. There has been burgeoning interest in MIE since it was first described in Taiwan in 19959 and in the People’s Republic of China in 1999.13 The last decade has witnessed nationwide growth in use of MIE, yielding a significant amount of scientific data to support its clinical merits and advantages. Here we review the current data and state of the art for MIE in the treatment of esophageal cancer in the People’s Republic of China.
Figure 1.
Fifteen national areas implementing minimally invasive esophagectomy in the People’s Republic of China.
Notes: High-volume centers: First Affiliated Hospital, School of Medicine, Peking University and Chaoyang Hospital, Capital Medical University in Beijing; Shandong Provincial Hospital, Shandong University in Jinan; The Affiliated Tumor Hospital, Zhengzhou University in Zhengzhou; Jiangsu Provincial Cancer Hospital in Nanjing; Zhongshan Hospital, Fudan University, The Cancer Hospital of Fudan University, Changzheng Hospital, Second Military Medical University and Shanghai Chest Hospital, Shanghai Jiaotong University in Shanghai; Taizhou Hospital, Wenzhou Medical College in Taizhou; Affiliated Union Hospital of Fujian Medical University and Fujian Provincial Tumor Hospital of Fujian Medical University in Fuzhou; Chang Gung Memorial Hospital, Chang Gung Medical College in Taipei; Tungs’ Taichung MetroHarbor Hospital in Taichung; University of Hong Kong Medical Centre, Queen Mary Hospital and The Chinese University of Hong Kong, Prince of Wales Hospital in Hongkong; Nanfang Hospital, Southern Medical University and Cancer Center, Sun Yatsen University in Guangzhou; Second Xiangya Hospital of Central South University in Changsha; Daping Hospital, Third Military Medical University in Chongqing; West China Hospital, Sichuan University in Chengdu; The Second Clinical Institute, North Sichuan Medical College in Nanchong.
Literature on MIE in the People’s Republic of China
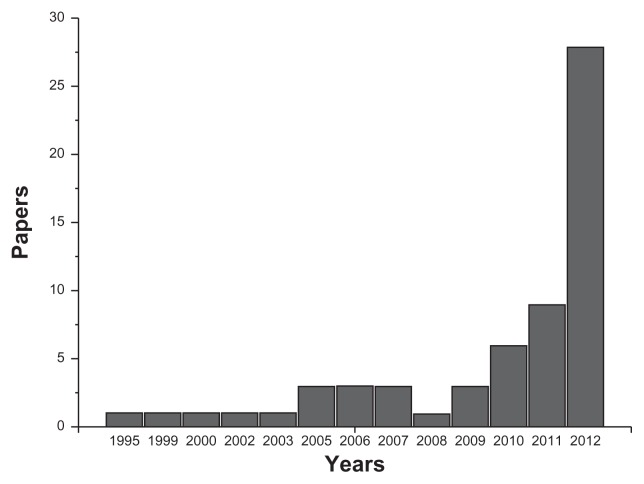
The current literature was reviewed by searching the PubMed/Medline database from January 1992 to December 2012 using keywords such as “minimally invasive oesophagectomy”, “MIE”, and “China”. Sixty-one full articles were found to be relevant to MIE (Figure 2). A total of 33 publications (54.1%) were in English. However, nearly half of all relevant clinical reports (28, 45.9%) were published in Chinese, despite the fact that it has been necessary to report the current status of MIE as performed in the People’s Republic of China to cardiothoracic surgeons worldwide. A marked increase in the number of papers dedicated to MIE was observed from 2010 to 2012 (Figure 2), which probably reflects increased research interest among the surgical community and wider clinical application of this patient-friendly approach.
Figure 2.
Numbers of papers related to minimally invasive esophagectomy performed in the People’s Republic of China identified in the PubMed/Medline database, using keywords such as “minimally invasive oesophagectomy”, “MIE”, and “China”.
Operative data on MIE
Key outcomes of the major studies are summarized in the Tables 1 and 2. Thirty-two relevant papers, consisting of prospective and retrospective studies, were identified. Eight papers directly compared open oesophagectomy and MIE, and16,17,21,30,31,39,41,48 five of these involved studies performed prospectively.16,31,39,41,48 Common outcome measures included operative data (operative time, blood loss, conversion rate), morbidity (duration of intensive care and total hospital stay), complications (pulmonary complications, anastomotic leaks, chylothorax), mortality data, and follow-up periods. Neoadjuvant treatment numbers were included for each study.
Table 1.
Survey over major reports of minimally invasive esophagectomy in the People’s Republic of China: operative data
| Reference | PS/RS | Patient (n) | AC | TC | AS | Position | OT (min) | BL (mL) | C, n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Liu et al9 | RS | 20 | Open | MI | Thoracic | Left Lateral | 280 | 250 | NA |
| Li et al14 | PS | 6 | MI | MI | Thoracic | Left Lateral | 260 ± 42 | 520 ± 160 | 0 |
| Li et al15 | RS | 6 | MI | MI | Thoracic | Left Lateral | 380 | 300 | 0 |
| Du et al16 | PS | 45 | Open | HA | Cervical/ thoracic | Left Lateral | 29 ± 5 (TC) | 93 ± 19 (TC) | NA |
| 27 | Open | MI | Cervical | Left Lateral | 425 (240–538) | 400 (100–1200) | 1 (4) | ||
| Liu et al17 | RS | 98 | MI | MI | Cervical | Left Lateral | 134.5 ± 42.3 | 85.1 ± 32.8 | NA |
| Hou et al18 | RS | 41 | MI | MI | Cervical | Prone | 230 (170–310) | 275 (100–320) | NA |
| 41 | MI | MI | Cervical | Left Lateral | 280 (190–380) | 360 (120–670) | NA | ||
| Wu et al20 | PS | 32 | Open | MI | Cervical | Supine | 180 | 218 | 0 |
| 8 | MI | MI | Cervical | Supine | 220 | 100 | 0 | ||
| Zhou et al22 | PS | 30 | Open | MI | Cervical | Left Lateral | 225 (195–290) | 250 ± 52.2 | 1 (3) |
| Tan et al23 | RS | 36 | Open | MI | Cervical | Left Lateral | 250 (190–330) | 165 (100–350) | 0 |
| Wang et al24 | PS | 27 | MI | MI | Cervical | Left Lateral | 267 ± 51 | 327 ± 83 | NA |
| Feng et al25 | PS | 27 | MI | MI | Cervical | Supine | 194.4 ± 26 | 215 ± 111.6 | 0 |
| 27 | MI | MI | Cervical | Left Lateral | 228.1 ± 35.8 | 142.6 ± 51.3 | 0 | ||
| Wang et al26 | RS | 48a | MI | MI | Cervical | Left Lateral | 279 ± 64 | 359 ± 156 | NA |
| 49b | MI | MI | Cervical | Left Lateral | 266 ± 56 | 336 ± 130 | NA | ||
| Feng et al27 | RS | 52 | MI | MI | Cervical | Left Lateral | 82 ± 17 (TC) | 139 ± 54 (TC) | 0 |
| RS | 36 | MI | MI | Cervical | Prone | 70 ± 20 (TC) | 100 ± 52 (TC) | 0 | |
| Shen et al28 | RS | 76 | MI | MI | Cervical | Prone | 89 ± 32 (TC) | 152 ± 108 | 0 |
| Feng et al29 | PS | 41 | MI | MI | Cervical | Decubitus | 217 ± 32 | 142 ± 49 | 1 (2.4) |
| PS | 52 | MI | MI | Cervical | Prone | 202 ± 21 | 123 ± 56 | 0 | |
| Wang et al30 | RS | 260 | MI/O | MI | Cervical | Left Lateral | 105 ± 30 (TC) | 95 ± 48 (TC) | NA |
| Zhu et al31 | PS | 25 | Open | MI | Thoracic | Left Lateral | 88 ± 15 (TC) | 280 ± 132 (TC) | NA |
| Chen et al32 | PS | 67 | MI | MI | Cervical | Left Lateral | 274 ± 15 | 225 ± 31 | NA |
| Zhu et al33 | PS | 11 | MI | MI | Cervical | Left Lateral | 242.3 ± 27.0 | 168.2 ± 95.6 | NA |
| Lin et al34 | RS | 80 | MI | MI | Cervical | Left Lateral | NA | 100–250 | 6 (8) |
| Liu et al35 | RS | 297 | MI | MI | Cervical | Left Lateral | 242.3 ± 58.7 | NA | 1 (3) |
| Lin et al36 | RS | 150 | MI | MI | Cervical | Left Lateral | 258 ± 45 | 207 ± 130 | 6 (4) |
| Cense et al38 | PS | 30 | Open | MI | Cervical | Left Lateral | 400 (180–570) | 700 (164–3000) | 2 (7) |
| Law et al39 | PS | 30 | Open | MI | Thoracic | Left Lateral (29)/ prone (1) | 392 (180–570) | 700 (164–3000) | 2 (6.7) |
| Wong et al40 | PS | 12 | MI | MI | Thoracic | Supine | 510 (300–660) | 500 (250–2500) | 1 (8) |
| Wang et al41 | PS | 33 | MI | MI | Cervical | Na | NA | NA | NA |
| Xie et al42 | RS | 100 | MI | MI | Cervical | Left Lateral | 310 | 200 | 4 (4) |
| Yuan et al43 | PS | 32 | MI | MI | Cervical | Left Lateral | 290.8 ± 36.9 | NA | NA |
| 36 | Open | MI | Cervical | Supine | 249.0 ± 31.0 | NA | NA | ||
| Guo et al44 | RS | 89 | Open | MI | Cervical | Left Lateral | 323.7 ± 50.3 | 307.8 ± 162.7 | 8 (9.0) |
| Guo et al45 | RS | 135 | Open | MI | Cervical | Left Lateral | 334 ± 51.1 | 349.3 ± 164.8 | 10 (7.4) |
| Zhang et al46 | RS | 160 | MI | MI | Cervical | Prone | 230–780 | 20–4000 | 9 (5.6) |
| Gao et al48 | PS | 96 | MI | MI | Cervical | Left Lateral | 330.2 ± 36.7 | 346.7 ± 41.1 | 0 |
Notes:
Retrosternal route of gastric tube reconstruction;
prevertebral route of gastric tube reconstruction.
Abbreviations: PS, prospective study; RS, retrospective study; AC, abdominal component; TC, thoracic component; AS, anastomosis site; OT, operation time; BL, blood loss; C, conversion rate; MI, minimally invasive; O, open; NA, not available; HA, hand-assisted.
Table 2.
Survey of major reports of minimally invasive esophagectomy in the People’s Republic of China: mortality, morbidity, and postoperative complications
| Reference | Patient (n) | AL, n (%) | PC, n (%) | Ch, n (%) | ICUS (d) | HS (d) | 30-DM | Mortality, n (%) | FP (m) |
|---|---|---|---|---|---|---|---|---|---|
| Liu et al9 | 20 | 0 | 0 | 0 | NA | 19 | NA | NA | 11.5 |
| Li et al14 | 6 | 0 | NA | NA | 0 | 17 | NA | NA | 2.5 |
| Li et al15 | 6 | 0 | 0 | 0 | NA | NA | NA | NA | NA |
| Du et al16 | 45 | NA | NA | NA | NA | 10.0 ± 1.0 | NA | NA | NA |
| Liu et al17 | 98 | 2 (2.0) | 10 (10.2) | 3 (3.1) | NA | 12.7 ± 3.5 | 1 | NA | NA |
| Hou et al18 | 41 | 1 (2.4) | 2 (4.9) | 0 | NA | NA | NA | NA | 15.7 |
| 41 | 1 (2.4) | 1 (2.4) | 2 (4.9) | NA | NA | NA | NA | 16.3 | |
| Wu et al20 | 32 | 3 (9.4) | 1 (3.1) | 1 (3.1) | 2.2 | 11.6 | NA | NA | NA |
| 8 | 1 (12.5) | 0 | 0 | 1.2 | 10.6 | NA | NA | NA | |
| Zhou et al22 | 30 | 2 (6.7) | 2 (6.7) | 1 (3.3) | NA | 11.7 ± 6.3 | 0 | 0 | NA |
| Tan et al23 | 36 | 5 (13.9) | 1 (2.8) | 1 (2.8) | NA | 8.7 | 0 | 0 | NA |
| Wang et al24 | 27 | 5 (18.5) | 1 (3.7) | 2 (7.4) | 2.3 ± 1.7 | NA | NA | NA | NA |
| Feng et al25 | 27 | 5 (18.5) | 7 (25.9) | 0 | 3.1 ± 4.4 | 11.1 ± 6.6 | 1 | NA | 36 |
| 27 | 4 (14.8) | 4 (14.8) | 1 (3.7) | 1.9 ± 4.2 | 13.3 ± 10.6 | 0 | NA | 36 | |
| Wang et al26 | 48 | 10 (20.8) | 2 (4.2) | 1 (2.1) | 2.5 ± 1.7 | NA | 0 | NA | NA |
| 49 | 3 (6.1) | 6 (12.2) | 1 (2.0) | 2.8 ± 1.9 | NA | 0 | NA | NA | |
| Feng et al27 | 52 | 8 (15.4) | 5 (9.6) | 2 (3.8) | 1.3 ± 3.5 | 13.6 ± 9.3 | NA | NA | NA |
| 36 | 2 (5.6) | 1 (2.8) | 0 | 1.1 ± 1.5 | 10.9 ± 6.0 | NA | NA | NA | |
| Shen et al28 | 76 | 16 (21.1) | 5 (6.6) | 1 (1.3) | NA | 19.2 ± 16.3 | NA | 0 | NA |
| Feng et al29 | 41 | 9 (22.0) | 4 (9.8) | NA | 3.5 ± 1.3 | 17.4 ± 12.5 | NA | NA | NA |
| 52 | 4 (7.7) | 5 (9.6) | NA | 1.5 ± 1.1 | 11.4 ± 6.8 | NA | NA | NA | |
| Wang et al30 | 260 | 26 (10) | 22 (8.5) | 3 (1.2) | NA | 14.3 ± 7.5 | NA | 2 (7.7) | NA |
| Zhu et al31 | 25 | 1 (4) | NA | NA | NA | 10.9 ± 2.5 | NA | NA | NA |
| Chen et al32 | 67 | NA | 7 (10.4) | NA | NA | 11.5 ± 1.6 | NA | NA | 14.0 ± 2.2 |
| Zhu et al33 | 11 | 2 (18.2) | 3 (27.3) | NA | NA | 18.9 ± 10.3 | NA | NA | 4.5 |
| Lin et al34 | 80 | 1 (1.3) | NA | 2 (2.5) | NA | NA | NA | NA | NA |
| Liu et al35 | 297 | 9 (3.0) | 41 (18.8) | NA | NA | 17.4 ± 9.8 | NA | NA | NA |
| Lin et al36 | 150 | 9 (6.0) | 17 (11.3) | 5 (3.3) | NA | NA | 2 (1.3) | 9 (6) | 3–22 |
| Cense et al38 | 30 | 1 (3.3) | 12 (40) | NA | NA | NA | NA | NA | NA |
| 27 | 1 (3.7) | 13 (48.1) | NA | NA | NA | NA | 2 (7) | NA | |
| Law et al39 | 30 | 1 (3.3) | 12 (40) | 0 | NA | NA | 1 | NA | NA |
| Wong et al40 | 12 | 1 (8.3) | 2 (17) | NA | 2 | 41 | 0 | 0 | NA |
| Wang et al41 | 33 | 1 (3.0) | 0 | 0 | NA | NA | NA | NA | NA |
| Xie et al42 | 100 | 11 (11) | 13 (13) | 3 (3) | 1 (1) | 12 (12) | NA | NA | NA |
| Yuan et al43 | 32 | 2 (6.3) | NA | NA | 1 | 11.1 ± 1.3 | 0 | NA | NA |
| 36 | 5 (13.9) | NA | NA | 1 | 11.6 ± 1.7 | 0 | NA | NA | |
| Guo et al44 | 89 | 6 (6.7) | 4 (4.5) | 4 (4.5) | NA | 15.2 ± 9.8 | NA | NA | NA |
| Guo et al45 | 135 | 9 (6.7) | 7 (5.2) | 8 (5.9) | NA | NA | NA | NA | NA |
| Zhang et al46 | 160 | 21 (13.1) | 25 (15.6) | 4 (2.5) | 1 | 13.1 | 2 (1.3) | 4 (2.5) | NA |
| Gao et al48 | 96 | 7 (7.3) | 13 (13.5) | 1 (1.1) | 19.2 ± 3.5 | 12.6 ± 8.8 | NA | 2 (2.1) | NA |
Abbreviations: AL, anastomotic leaks; PC, pulmonary complication; Ch, chylothorax; ICUS (d), intensive care unit stay (days); HS (d), hospital stay (days); 30-DM, 30-day mortality; FP (m), follow-up period (months); NA, not available.
Surgical approaches
Surgical approaches for MIE performed by Chinese cardiothoracic surgeons are multiple and complicated. As listed in Table 1, the majority of centers use mainly total MIE (laparoscopic and thoracoscopic esophagectomy), whereas hybrid MIE (thoracoscopy and laparotomy/laparoscopy and thoracotomy) is used in routine practice in some centers. At our center, we originally used hybrid MIE31 but more recently transitioned to a minimally invasive modified McKeown 3-incision total MIE (laparoscopic and thoracoscopic esophagectomy) in 2010.32,33
Operative time and blood loss
Operative time varied significantly between the studies, reflecting the type of MIE performed as well as accumulated experience and technical skills (Table 1). Blood loss also varied significantly from center to center, comprising around 100–700 mL (Table 1). Major blood loss and need for blood transfusion in particular increased the risk of postoperative morbidity and mortality.
Conversion to open esophagectomy
The conversion rate reported in the literature is in a range of 0%–9.7% (Table 1). However, with surgical experience, the conversion rate reduces and currently does not exceed 5% in expert centers in the People’s Republic of China. The main reason for conversion was bleeding. It is not appropriate to consider conversion from MIE to open esophagectomy as a failure because patient safety and the oncologic integrity of the procedure should be of supreme importance.
Mortality, morbidity, and postoperative complications
Mortality rates following total MIE vary between 0% and 7.7% (Table 2), which compares favorably with an open transthoracic procedure mortality rate of 9.2% and an open transhiatal procedure mortality rate of 7.2%.50 However, at least half of the patients who undergo open oesophagectomy, performed through a right thoracotomy and laparotomy, are at risk of developing pulmonary complications requiring a protracted stay in intensive care, with consequences for quality of life during convalescence.50 Anastomotic leak is one of the most feared complications of MIE. From the operative data, the MIE leakage rate was in the range of 0%–20.8% (Table 2), which is comparable with the leakage rates reported for open oesophagectomy.51 Median duration of postoperative stay in intensive care following MIE was one day in the majority of studies (Table 2). MIE is associated with a significant reduction in hospital stay, with a mean postoperative stay of 12 days (Table 2).
Outcomes
There is little survival data for MIE available in the People’s Republic of China. Only one study reported overall survival after MIE.25 Feng et al reported median survival for patients in a thoracoscope-assisted transthoracic esophagectomy group and in a mediastinoscope-assisted transhiatal esophagectomy group of 34.4 months and 36.8 months, respectively.25 There do not appear to be any prospective, randomized, controlled trials comparing the oncologic outcome of MIE with that of open esophagectomy. The present knowledge is based mainly on short-term, nonrandomized comparative studies or historical comparisons with outcomes of open surgery.31,39,41,48
Conclusion
In conclusion, MIE is becoming more popular in the People’s Republic of China now that Chinese cardiothoracic surgeons are receiving adequate training in major centers. Use of the technique is growing in the People’s Republic of China, as confirmed by the increasing number of recently published papers on MIE. However, no prospective, randomized, controlled trials have investigated the benefits of MIE in this country. Such trials, directly comparing MIE and open approaches, are urgently needed.
Acknowledgments
This work was supported by grants from Zhejiang Provincial Science and Technology Major Projects (2011C13039-2) and Zhejiang Provincial Science and Technology Innovation Team Projects (2011R09040-03).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin. 1999;49(1):33–64. doi: 10.3322/canjclin.49.1.33. [DOI] [PubMed] [Google Scholar]
- 3.Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349(23):2241–2252. doi: 10.1056/NEJMra035010. [DOI] [PubMed] [Google Scholar]
- 4.Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12(7):681–692. doi: 10.1016/S1470-2045(11)70142-5. [DOI] [PubMed] [Google Scholar]
- 5.Cerfolio RJ, Bryant AS, Hawn MT. Technical aspects and early results of robotic esophagectomy with chest anastomosis. J Thorac Cardiovasc Surg. 2013;145(1):90–96. doi: 10.1016/j.jtcvs.2012.04.022. [DOI] [PubMed] [Google Scholar]
- 6.Kastenmeier A, Gonzales H, Gould JC. Robotic applications in the treatment of diseases of the esophagus. Surg Laparosc Endosc Percutan Tech. 2012;22(4):304–309. doi: 10.1097/SLE.0b013e318258340a. [DOI] [PubMed] [Google Scholar]
- 7.Palanivelu C, Prakash A, Senthilkumar R, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position – experience of 130 patients. J Am Coll Surg. 2006;203(1):7–16. doi: 10.1016/j.jamcollsurg.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 8.Luketich JD, Alvelo-Rivera M, Buenaventura PO, et al. Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg. 2003;238(4):486–494. doi: 10.1097/01.sla.0000089858.40725.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu HP, Chang CH, Lin PJ, Chang JP. Video-assisted endoscopic esophagectomy with stapled intrathoracic esophagogastric anastomosis. World J Surg. 1995;19(5):745–747. doi: 10.1007/BF00295920. [DOI] [PubMed] [Google Scholar]
- 10.Sabanathan S, Mearns AJ, Richardson J. Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb. 1992;37(4):284–285. [PubMed] [Google Scholar]
- 11.DePaula AL, Hashiba K, Ferreira EA, de Paula RA, Grecco E. Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc. 1995;5(1):1–5. [PubMed] [Google Scholar]
- 12.Zingg U, McQuinn A, DiValentino D, et al. Minimally invasive versus open esophagectomy for patients with esophageal cancer. Ann Thorac Surg. 2009;87(3):911–919. doi: 10.1016/j.athoracsur.2008.11.060. [DOI] [PubMed] [Google Scholar]
- 13.Wang J, Liu T, Xing M. Video-assisted thoracic surgery in the management of chest diseases. Zhonghua Yi Xue Za Zhi. 1999;79(8):589–591. Chinese. [PubMed] [Google Scholar]
- 14.Li H, Hu B, You B, Miao JB, Fu YL, Chen QR. Combined laparoscopic and thoracoscopic Ivor Lewis esophagectomy for esophageal cancer: initial experience from the People’s Republic of China. Chin Med J (Engl) 2012;125(8):1376–1380. [PubMed] [Google Scholar]
- 15.Li H, Hu B, You B, et al. Completely minimally invasive Ivor Lewis esophagectomy: the preliminary experience of circular-stapled anastomosis with the trans-oral anvil. Zhonghua Wai Ke Za Zhi. 2010;48(22):1747–1750. Chinese. [PubMed] [Google Scholar]
- 16.Du JJ, Meng L, Chen JH, et al. Hand-assisted video-thoracoscopy for resection of esophageal cancer. Zhonghua Wai Ke Za Zhi. 2005;43(6):351–353. Chinese. [PubMed] [Google Scholar]
- 17.Liu BX, Li Y, Qin JJ, et al. Comparison of thoracolaparoscopic and open three-field subtotal esophagectomy for esophageal cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):938–942. Chinese. [PubMed] [Google Scholar]
- 18.Hou YL, Zhao JQ, Guo W, Zang B, Tang DR. Comparison of the short- term outcomes of patients with esophageal cancer after subtotal esophagectomy via thoracoscopy in left lateral position and in prone position. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):950–953. Chinese. [PubMed] [Google Scholar]
- 19.Xue L, Pan T, Xu Z, et al. Multi-factor investigation of early postoperative cardiac arrhythmia for elderly patients with esophageal or cardiac carcinoma. World J Surg. 2009;33(12):2615–2619. doi: 10.1007/s00268-009-0222-0. [DOI] [PubMed] [Google Scholar]
- 20.Wu B, Xue L, Qiu M, et al. Video-assisted mediastinoscopic transhiatal esophagectomy combined with laparoscopy for esophageal cancer. J Cardiothorac Surg. 2010;5:132. doi: 10.1186/1749-8090-5-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mao T, Fang WT, Gu ZT, Yao F, Guo XF, Chen WH. Comparative study of perioperative complications and lymphadenectomy between minimally invasive esophagectomy and open procedure. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):922–925. Chinese. [PubMed] [Google Scholar]
- 22.Zhou J, Chen H, Lu JJ, et al. Application of a modified McKeown procedure (thoracoscopic esophageal mobilization three-incision esophagectomy) in esophageal cancer surgery: initial experience with 30 cases. Dis Esophagus. 2009;22(8):687–693. doi: 10.1111/j.1442-2050.2009.00963.x. [DOI] [PubMed] [Google Scholar]
- 23.Tan LJ, Wang Q, Feng MX, et al. Video-assisted thoracoscopic esophagectomy in esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2008;11(1):24–27. Chinese. [PubMed] [Google Scholar]
- 24.Wang H, Feng M, Tan L, Wang Q. Comparison of the short-term quality of life in patients with esophageal cancer after subtotal esophagectomy via video-assisted thoracoscopic or open surgery. Dis Esophagus. 2010;23(5):408–414. doi: 10.1111/j.1442-2050.2009.01025.x. [DOI] [PubMed] [Google Scholar]
- 25.Feng MX, Wang H, Zhang Y, Tan LJ, Xu ZL, Qun W. Minimally invasive esophagectomy for esophageal squamous cell carcinoma: a case-control study of thoracoscope versus mediastinoscope assistance. Surg Endosc. 2012;26(6):1573–1578. doi: 10.1007/s00464-011-2073-7. [DOI] [PubMed] [Google Scholar]
- 26.Wang H, Tan L, Feng M, Zhang Y, Wang Q. Comparison of the short-term health-related quality of life in patients with esophageal cancer with different routes of gastric tube reconstruction after minimally invasive esophagectomy. Qual Life Res. 2011;20(2):179–189. doi: 10.1007/s11136-010-9742-1. [DOI] [PubMed] [Google Scholar]
- 27.Feng MX, Tan LJ, Wang H, et al. Comparison of thoracoscopic esophagectomy in decubitus position with prone position. Zhonghua Wei Chang Wai Ke Za Zhi. 2011;14(9):686–688. Chinese. [PubMed] [Google Scholar]
- 28.Shen Y, Zhang Y, Tan L, et al. Extensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single center. J Gastrointest Surg. 2012;16(4):715–721. doi: 10.1007/s11605-012-1824-7. [DOI] [PubMed] [Google Scholar]
- 29.Feng M, Shen Y, Wang H, et al. Thoracolaparoscopic esophagectomy: is the prone position a safe alternative to the decubitus position? J Am Coll Surg. 2012;214(5):838–844. doi: 10.1016/j.jamcollsurg.2011.12.047. [DOI] [PubMed] [Google Scholar]
- 30.Wang H, Tan LJ, Li JP, et al. Evaluation of safety of video-assisted thoracoscopic esophagectomy for esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):926–929. Chinese. [PubMed] [Google Scholar]
- 31.Zhu CC, Chen SL, Ye MH. Esophagectomy combined with radical lymphadenectomy by video-thoracoscopy. Zhonghua Wai Ke Za Zhi. 2005;43(10):628–630. Chinese. [PubMed] [Google Scholar]
- 32.Chen BF, Zhu CC, Wang CG, et al. Clinical comparative study of minimally invasive esophagectomy versus open esophagectomy for esophageal carcinoma. Zhonghua Wai Ke Za Zhi. 2010;48(16):1206–1209. Chinese. [PubMed] [Google Scholar]
- 33.Zhu CC, Chen BF, Kong M, et al. Neoadjuvant chemoradiotherapy followed by combined thoracoscopic and laparoscopic esophagectomy in the treatment of locally advanced esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):943–946. Chinese. [PubMed] [Google Scholar]
- 34.Lin J, Kang M, Chen C, et al. Thoracolaparoscopy oesophagectomy and extensive two-field lymphadenectomy for oesophageal cancer: Introduction and teaching of a new technique in a high-volume centre. Eur J Cardiothorac Surg. 2013;43(1):115–121. doi: 10.1093/ejcts/ezs151. [DOI] [PubMed] [Google Scholar]
- 35.Liu SY, Wang F, Zheng QF, Chen XF. Clinical application of minimally invasive esophagectomy for esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):947–949. Chinese. [PubMed] [Google Scholar]
- 36.Lin JB, Kang MQ, Lin RB, Zhen W, Chen C. Thoracolaparoscopic esophagectomy with two-field lymph node dissection for esophageal carcinoma: report of 150 cases. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):930–933. Chinese. [PubMed] [Google Scholar]
- 37.Lin FC, Russell H, Ferguson MK. Strangulation of the reconstructive gastric tube by the azygos arch. Ann Thorac Surg. 2006;82(2):e8–e10. doi: 10.1016/j.athoracsur.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 38.Cense HA, Law S, Wei W, et al. Pharyngo-laryngo-esophagectomy using the thoracoscopic approach. Surg Endosc. 2007;21(6):879–684. doi: 10.1007/s00464-006-9049-z. [DOI] [PubMed] [Google Scholar]
- 39.Law SY, Fok M, Wei WI, et al. Thoracoscopic esophageal mobilization for pharyngo-laryngo-esophagectomy. Ann Thorac Surg. 2000;70(2):418–422. doi: 10.1016/s0003-4975(00)01402-8. [DOI] [PubMed] [Google Scholar]
- 40.Wong SK, Chan AC, Lee DW, To EW, Ng EK, Chung SC. Minimal invasive approach of gastric and esophageal mobilization in total pharyngo-laryngo-esophagectomy: total laparoscopic and hand-assisted laparoscopic technique. Surg Endosc. 2003;17(5):798–802. doi: 10.1007/s00464-002-9117-y. [DOI] [PubMed] [Google Scholar]
- 41.Wang YB, Cai RJ, Han YJ, Wang WJ, Yang XY, Liu SE. Quality of life in patients with esophageal carcinoma undergoing thoracoscopic and laparoscopic esophagectomy and circular stapled cervical esophagogastric anastomosis via retrosternal route. Zhonghua Wei Chang Wai Ke Za Zhi. 2011;14(6):428–431. Chinese. [PubMed] [Google Scholar]
- 42.Xie X, Fu JH, Wang JY, et al. Analysis of learning process of video-assisted minimally invasive esophagectomy for thoracic esophageal carcinoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):918–921. Chinese. [PubMed] [Google Scholar]
- 43.Yuan YC, Xia ZK, Yin N, Yin BL, Hu JG. Modified thoracoscopic versus minimally invasive oesophagectomy in curative resection of oesophageal cancer. J Int Med Res. 2011;39(3):904–911. doi: 10.1177/147323001103900324. [DOI] [PubMed] [Google Scholar]
- 44.Guo W, Zou YB, Ma Z, et al. One surgeon’s learning curve for video-assisted thoracoscopic esophagectomy for esophageal cancer with the patient in lateral position: how many cases are needed to reach competence? Surg Endosc. 2012 Oct 24; doi: 10.1007/s00464-012-2614-8. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 45.Guo W, Zhao YP, Jiang YG, et al. Prevention of postoperative chylothorax with thoracic duct ligation during video-assisted thoracoscopic esophagectomy for cancer. Surg Endosc. 2012;26(5):1332–1326. doi: 10.1007/s00464-011-2032-3. [DOI] [PubMed] [Google Scholar]
- 46.Zhang ZM, Wang Y, Gao YS, Song Y, Ma L. Minimally invasive esophagectomy for esophageal carcinoma: clinical analysis of 160 cases. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):934–937. Chinese. [PubMed] [Google Scholar]
- 47.Wang ZQ, Zhang YC, Zhang Q, Zhu XJ, Shu Y, Zhou ZG. Laparoscopic transhiatal extended gastrectomy for type II, III esophagogastric junction cancer: a preliminary report of 55 cases. Zhonghua Wei Chang Wai Ke Za Zhi. 2010;13(9):652–655. Chinese. [PubMed] [Google Scholar]
- 48.Gao Y, Wang Y, Chen L, Zhao Y. Comparison of open three-field and minimally-invasive esophagectomy for esophageal cancer. Interact Cardiovasc Thorac Surg. 2011;12(3):366–369. doi: 10.1510/icvts.2010.258632. [DOI] [PubMed] [Google Scholar]
- 49.Ren MY, Huang B, Zhang J, Pu M, Deng SH. Laparoscopic transhiatal proximal gastrectomy for adenocarcinoma of the esophagogastric junction: report of 98 cases. Zhonghua Wei Chang Wai Ke Za Zhi. 2012;15(9):906–909. Chinese. [PubMed] [Google Scholar]
- 50.Hulscher JB, van Sandick JW, de Boer AG, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med. 2002;347(21):1662–1669. doi: 10.1056/NEJMoa022343. [DOI] [PubMed] [Google Scholar]
- 51.Hulscher JB, Tijssen JG, Obertop H, van Lanschot JJ. Transthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysis. Ann Thorac Surg. 2001;72(1):306–313. doi: 10.1016/s0003-4975(00)02570-4. [DOI] [PubMed] [Google Scholar]