Abstract
Objective
In 2005 the American College of Surgeons passed a mandate requiring that Level I trauma centers have a mechanism to identify patients who are problem drinkers and have the capacity to provide an intervention for patients who screen positive. The aim of the Disseminating Organizational Screening and Brief Intervention Services (DO-SBIS) cluster randomized trial is to test a multilevel intervention targeting the implementation of high quality alcohol screening and brief intervention (SBI) services at trauma centers.
Method
Twenty sites selected from all US Level I trauma centers were randomized to participate in the trial. Intervention site providers receive a combination of workshop training in evidence-based motivational interviewing (MI) interventions and organizational development activities prior to conducting trauma center-based alcohol SBI with blood alcohol positive injured patients. Control sites implement care as usual. Provider MI skills, patient alcohol consumption, and organizational acceptance of SBI implementation outcomes are assessed.
Results
The investigation has successfully recruited provider, patient, and trauma center staff samples into the study and outcomes are being followed longitudinally.
Conclusion
When completed, the DO-SBIS trial will inform future American College of Surgeons’ policy targeting the sustained integration of high quality alcohol SBI at trauma centers nationwide.
Keywords: Acute care medical trauma centers, Injury, Alcohol, Screening and brief intervention, American College of Surgeons
1. Introduction
Physical injury with and without traumatic brain injury constitutes a major public health problem for both civilian and veteran trauma-exposed patient populations. Each year in the United States (US), approximately 1.5-2.5 million Americans are so severely injured that they require inpatient surgical hospitalization.
Epidemiological investigations have documented that alcohol use problems are endemic among US trauma center inpatients. A body of evidence derived from efficacy and effectiveness spectrum randomized clinical trials now suggests that alcohol screening and brief intervention (SBI) programs derived from motivational interviewing (MI) principles may reduce alcohol consumption among patients presenting to acute care medical, trauma center settings. Thus, the widespread integration of high quality alcohol SBI into acute injury care has the potential to markedly increase the population impact of injury prevention efforts and has been a longstanding public health objective.
In 2005, the American College of Surgeons, the primary agency responsible for developing United States’ trauma center regulatory requirements, passed a resolution mandating that Level I trauma centers must have a mechanism to identify patients who are problem drinkers and have the capacity to provide an intervention for patients who screen positive. Trauma centers that are found not to be performing alcohol SBI during American College of Surgeons’ verification site visits risk losing College accreditation and associated federal funding. This represents the first ever nationwide United States policy mandate for the integrated treatment of alcohol use problems in a general medical setting (i.e., hospital inpatient, emergency department, or primary care outpatient setting). Although an enormous first step, specific alcohol screening and brief intervention methodology is being left to the discretion of each trauma center. There is a substantial risk that the mandate will be implemented with marked variability and that lower quality alcohol SBI procedures could become the default standard of trauma center care nationwide. The overarching goal of this research program is to harness the opportunity afforded by the American College of Surgeons’ mandate by taking investigative steps to test the delivery of high quality, evidence-based alcohol SBI procedures.
2. Conceptual frameworks informing the DO-SBIS study protocol
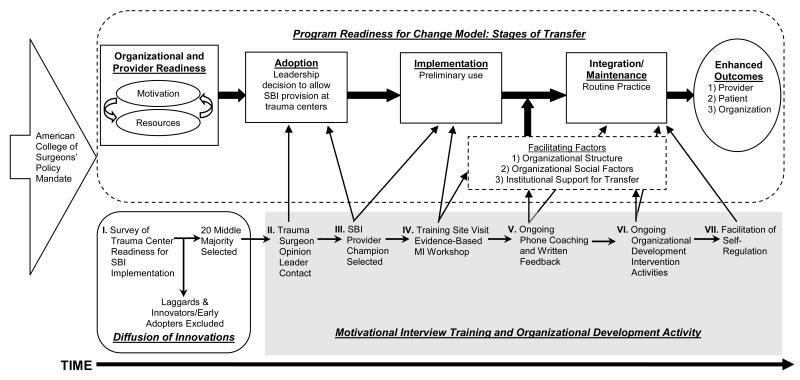
A number of conceptual frameworks inform the development and implementation of the Disseminating Organizational Screening and Brief Intervention Services (DO-SBIS) study protocol (Figure 1). Just as readiness has given a model for individual level change , organizational behavior and implementation science frameworks can be incorporated into a program readiness for change model that can guide integration of high quality alcohol SBI services into routine trauma center practice (Figure 1). The model outlines three key stages in the transfer of new alcohol SBI : 1) Adoption, an initial leadership decision to allow new screening and brief intervention procedure provision at a trauma center, 2) Implementation, the preliminary use of a new method, and 3) Integration, the maintenance into routine practice. The program readiness for change model identifies multiple potential trauma center provider and patient level targets for organizational development activities. The model suggests that organizational and provider readiness for change are key attributes for initial assessment. Multiple trauma center provider, patient, and organizational level targets for institutional development activities are also identified by the model.
Fig. 1.
DO-SBIS study conceptual frameworks and procedures.
Diffusion of innovation research suggests that trauma centers may be classified into adopter categories with regard to institutional readiness to implement evidence-based alcohol SBI procedures (Figure 1). Adopter categories range from innovators or early adopters (i.e., groups likely to rapidly take up an innovative technology), through middle majority adopters (i.e., medium uptake), and laggards (i.e., slow to adopt or no uptake). Diffusion of innovation research also suggests that trauma centers in the middle majority adopter category that are neither innovators nor laggards may be best suited for intervention. These centers are anticipated to be receptive to implementing high quality screening and brief intervention procedures in the wake of the American College of Surgeons’ mandate, yet are unlikely to do so without evidence-based intervention training and organizational development activities. Literature suggests that innovators and early adopters may already be implementing high quality SBI services and may not require intervention, and that laggards may be unresponsive to intervention.
3. Methods
3.1. Design overview
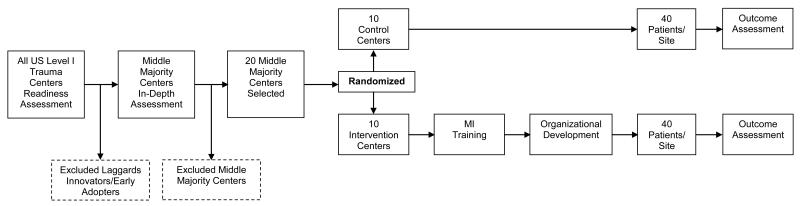
The specific aim of the DO-SBIS investigation is to test, in a cluster randomized clinical trial design, the effects of a multilevel intervention on the delivery of high quality alcohol SBI services at 20 United States Level I trauma centers (Figure 2). The 10 Level I trauma center sites randomized to the intervention receive a combination of workshop training, as well as feedback and coaching in evidence-based MI interventions. Intervention sites also receive organizational development intervention activity delivered by the interdisciplinary study team members. Control sites implement usual care alcohol SBI. Trauma center provider, patient, and organizational level outcomes are collected and followed longitudinally.
Fig. 2.
DO-SBIS study protocol.
3.2. Selection of trauma center sites and providers
A nationwide readiness assessment was conducted prior to the implementation of the clinical trial in order to classify US Level I trauma centers into adopter categories (Figure 2). The nationwide readiness survey included interviews with trauma program coordinators at each US Level I trauma center site. Survey items assessed current alcohol SBI practices, previous trauma center training in alcohol SBI, and willingness to receive additional provider, patient, and organizational level trainings. Hospital and national websites were used to characterize centers with regard to hospital beds, training programs, and National Institute of Health (NIH) alcohol protocol grant funding. Sites classified as innovators and early adopters demonstrated well developed alcohol SBI services and had established trauma surgical and SBI provider champions; innovator sites often demonstrated prior NIH or other extramural funding for alcohol SBI protocols. Laggard sites endorsed little training or service development, had no champions, and displayed little or no future interest in SBI organizational development. Middle majority sites fell between these two extremes, demonstrating interest in SBI related organizational development, but with fewer established champions and prior training/service development.
Middle majority adopter sites were retained in the study as they were anticipated to be receptive to implementing a screening and brief intervention procedure, yet unlikely to do so without externally prompted evidence-based intervention training and organizational development activities (Figure 2). The middle majority adopter sites received further in-depth evaluations performed by the study’s principal investigator and trauma surgical co-investigators that included rated discussions with potential trauma surgery opinion leaders and alcohol SBI provider champions. Site motivation and readiness to participate in the study were reassessed during these evaluations. This readiness assessment was used to select 20 American College of Surgeons verified middle majority centers for randomization in the clinical trial. Prior to randomization, a single trauma surgeon opinion leader and alcohol SBI provider champion(s) were identified at each site. Also prior to randomization, organizational process mapping was applied to each of the 20 sites in order to identify 10 staff affiliated with trauma center alcohol screening and brief intervention work units.
3.3. Randomization
The unit of randomization was the individual trauma center. Randomization occurred in a 1:1 ratio according to a computer-generated random assignment sequence.
3.4. Blinding
Research assistants conducting all assessments and follow-up interviews are blinded to trauma center intervention and control group assignments. Similarly, patients recruited from intervention and control group sites are not aware of trauma center group assignments.
3.5. Multilevel intervention procedures
The 10 intervention trauma center alcohol SBI providers were randomized to receive evidence-based MI workshop training, telephone coaching, and written feedback via email in conjunction with organizational development activities targeting the delivery of high quality alcohol SBI services. The MI intervention component has been successfully developed and implemented by the study team over the past decade in clinical trials and subsequently in routine clinical practice.
To initiate the intervention training, a one-day MI workshop is conducted at each intervention trauma center. During the site visit, the alcohol SBI champion provider(s) at each intervention trauma center receives training in the delivery of MI interventions targeting changes in post-injury alcohol consumption and related behaviors. Motivational interviewing approaches encourage movement in the direction of reductions in at-risk drinking behaviors by empathically exploring ambivalent feelings about alcohol use after an injury. The core intervention is a 20-30 minute motivational interview that can be delivered at bedside to injured inpatients by the full spectrum of trauma center providers (e.g., masters in social work and nursing providers). The acute care MI protocol developed for the intervention consisted of a graded sequence of the following clinical tasks: 1) Eliciting from patients their views on the importance of changing, as well as their confidence in being able to change, 2) giving patients personalized feedback on alcohol use, and 3) clarifying the patient’s goals (e.g., to quit or cut down) and action plans. Each patient’s motivation for counseling and readiness for change determined when and how many of these tasks will be discussed. The earlier tasks were emphasized with patients in the pre-contemplation or contemplation stages of change, and the later tasks were emphasized with those in the preparation or action stages. Previous investigation suggests that training workshops, plus feedback and coaching are the optimal procedures for teaching evidence-based alcohol intervention. For six months after the site visit, alcohol SBI provider champions at intervention sites receive expert telephone coaching and written feedback in motivational interviewing.
At intervention sites, training in MI is embedded within ongoing organizational development intervention activities (Figure 1). The organizational development intervention components are distilled from evidence-based organizational interventions including the Availability, Responsiveness, and Continuity (ARC) intervention. Organizational development interventions such as ARC aim to improve human service organizations’ delivery of health services by facilitating personal relationships with members of an organization, enhancing network development among providers, team building, enabling collaborative participatory decision making, providing information and feedback, facilitating conflict resolution when necessary, enhancing continuous quality improvement efforts, and aiding with job redesign. For the purposes of the current investigation, the organizational development intervention procedure has been adapted to fit the stages of the program change model (Figure 1). Study team intervention logs are used to document the timing and delivery of organizational development intervention activities.
3.6. Control trauma centers
Control trauma centers implement SBI care as usual. Preliminary studies suggest that there may be marked variation in SBI implementation at usual care control sites. As an incentive for study participation, both control and intervention sites receive a waiver on the American College of Surgeons alcohol SBI requirement during study participation. As a further incentive for participation, control sites receive a MI site visit training at the termination of the study protocol after recruitment and outcome assessments are complete.
3.7. Patient eligibility and enrollment
Patients included in the trial are male and female survivors of motor vehicle crashes, assaults, and other intentional and unintentional injuries, ages ≥ 18, who are so severely injured that they require inpatient hospital admission. Injured participants recruited into the trial are consecutively admitted patients who test positive for blood alcohol. Patients with self-inflicted injuries, monolingual non-English speaking injury survivors, and prisoners are excluded from the trial. Patients with Alcohol Use Disorders Identification Test (AUDIT) scores ≥ 20 are also excluded from the trial as these patients are less likely to benefit from brief interventions. After patients consent to the protocol and have received their baseline assessment from trauma center providers, SBI provider champions at intervention and control sites are instructed to deliver brief interventions targeting alcohol use reductions.
3.8. Outcome assessments: Overview
Provider, patient, and organizational level outcomes are collected in order to assess the impact of the multilevel intervention (Table 1). To assess sustained intervention effects over time, all outcome assessments extend longitudinally beyond the six months of active intervention site training.
Table 1.
DO-SBIS study protocol measures and outcome assessments
| Timing | Assessment | N | Mode | Measures | Outcome |
|---|---|---|---|---|---|
| Pre-randomization | All United States Level I trauma center program coordinators |
204 | Phone | Alcohol SBI Readiness Survey |
Classification/selection of RCT middle majority adopter sites |
| Pre-randomization | Middle majority adopter trauma centers |
40 | Phone | Early adopter status interview assessment |
Selection of site trauma surgeon and SBI provider interventionist(s) |
| Pre-randomization baseline, 1-week, 1-, 4-, 7-, 17-, and 27-month follow- up |
Alcohol SBI champion(s) | 20+ | Phone | MITI-coded standardized patient actor interviews [34] |
Motivational interviewing intervention fidelity and skill level |
| Pre-randomization baseline, 7-, 17-, and 27-month follow-up |
Trauma center staff comprising alcohol SBI work unit |
10*20 | Web | Organizational Social Context and Readiness [44, 45] |
Organizational climate, culture, and readiness for change |
| Pre-intervention, 6-, and 12-month post-hospital admission |
Patient self-report of primary alcohol outcomes |
800 | In-person/ Phone |
AUDIT, Form 90, and SIP [33, 34] |
Alcohol consumption and alcohol use problems |
| Pre-intervention, 6-, and 12-month post-hospital admission |
Patient self-report of secondary outcomes including PTSD, depression, drug use & function |
800 | In-person/ Phone |
Multiple (PCL-C, PHQ- 9, Form 90 drug, MOS SF-12) [41-43] |
Trauma center secondary outcomes |
| RCT recruitment period | Patient trauma registry data | 800 | CONSORT | Diagram of patient flow through protocol at 20 sites |
Estimation of target population and intervention reach |
| RCT development and implementation |
Study intervention team members’ records |
5 | Computer entry | Logs and field notes | Intervention activity documentation |
| Study end-point | Trauma center SBI champion(s) | 20 | In-person/ Phone |
Semi-structured qualitative interviews |
Facilitators and barriers to SBI implementation and maintenance |
3.9. Provider assessments of MI fidelity
The DO-SBIS investigators sought to advance the field of randomized MI training trials by deploying multiple measures of MI skill over a greatly extended time period. Therefore, the study design compares the natural development of MI skill over time (control group) with the development of formally-trained clinicians (intervention group) during both the training period and for nearly two years after the end of formal training. An accurate time series of real-world trauma clinicians’ skill development enhances current and future training and supervision efforts at trauma centers.
Intervention and control alcohol SBI providers participate in a total of seven 20-minute standardized patient actor telephone interviews. Baseline standardized patient interviews with providers took place at all 20 sites prior to randomization (Table 1). Intervention sites were scheduled for standardized patient interviews one week after workshop training and then again at 1-, 4-, 7-, 17-, and 27-months after the intervention workshop training; control site practitioners undergo a comparable sequencing of baseline, as well as 7-, 17-, and 27-month follow-up assessments. Frequent early longitudinal assessments are required in order to measure the impact of initial intensive workshop training, written feedback, and telephone coaching. Multiple longitudinal assessments may also allow for discrimination between transient training effects of the standardized patient interviews anticipated to occur in both intervention and control site providers, versus sustained gains in MI proficiency anticipated to occur only in intervention group providers as a result of workshop training, feedback and coaching.
For each assessment point, telephone appointments are made by the study standardized patients, who are blinded to SBI provider intervention and control group status. Each standardized patient interview lasted approximately 20 minutes and is audio-recorded. Standardized patient interviews incorporate a graded sequence of clinical difficulty ranging from early interviews, in which actors role-play patients ready and willing to change, to final interviews, in which actors role-play more challenging patients who are in the pre-contemplation stage of change.
Each interview is coded with the Motivational Interviewing Treatment Integrity coding system. Trained coders apply MITI coding rules to derive scores while listening to audiotaped standardized MI interviews. Global scores evaluating the entire session rate each counselor’s MI Spirit, Evocation, and Collaboration. Also, the frequencies of individual provider behaviors are counted by coders during the interview. These behavioral scores include open and closed questions, simple and complex reflections, giving information, and MI-adherent and -nonadherent behaviors. The MITI has established reliability and validity, and MITI coding procedures have been manualized and applied in over 20 published studies.
3.10. Patient outcomes
All patient level outcomes, including the primary outcome of interest post-injury alcohol consumption, are assessed via patient self-reports (Table 1). Investigation of standardized assessments of patient self-reported alcohol consumption across clinical populations including injured trauma survivors suggests that while some variation in the accuracy of self-reports exists, self-reports have established reliability and validity and can be used with confidence.
The AUDIT is being used to assess alcohol use at baseline in the inpatient ward and again 6- and 12-months after each patient’s hospital admission. The AUDIT is a 10-item screening instrument for the early identification of problem drinkers. In addition to the AUDIT, Form 90 will be used to augment the assessment of alcohol consumption at the 6- and 12-month time points. Form 90 is an optimal assessment for the investigation as it can be flexibly employed in telephone evaluations and the brief interviews required in general medical setting follow-ups. Form 90 has established reliability and convergent validity. The 6- and 12-month follow-up telephone interviews will also include selected Form 90 items assessing the use of drugs, the use of substance-related health services, recurrent injury events, episodes of driving under the influence of alcohol, and substance-related legal encounters (Table 1). These Form 90 items will be augmented with the Short Inventory of Problems in order to enhance the assessment of alcohol and drug-related problem behaviors. Additional trauma center patient level assessments derived from previous acute care study protocols by the investigative team included posttraumatic stress disorder symptoms, depression, and functional outcomes (Table 1).
3.11. Trauma center staff organizational outcomes
The investigation uses the Organizational Social Context (OSC) and Organizational Readiness for Change (ORC) measures to assess and compare acceptance of SBI services for intervention and control site staff (Table 1). The OSC assesses domains of organizational climate and culture, including emphasis on emotional support, job satisfaction, hierarchy of authority, motivation, and service quality. The ORC assesses four domains of organizational readiness for the implementation of trauma center alcohol programs, including motivational readiness, institutional resources, staff attributes, and institutional climate. These organizational assessments have established reliability and validity when used across diverse institutional contexts. Ten staff members, identified by the institutional process mapping procedure, constituted the trauma center organizational alcohol SBI work unit for each assessment. Intervention sites receive assessments at baseline pre-randomization, and 7-, 17-, and 27-month follow-up. Control sites undergo a comparable sequencing of baseline pre-randomization, and 7-, 17-, and 27-month follow-up assessments (Table 1).
3.12. Other DO-SBIS study protocol assessments
Each patient enrolled consents to the release of trauma center medical record data; de-identified trauma registry data for all trauma patients admitted during the time period of each site’s patient recruitment is also obtained. The characteristics of patients recruited into the investigation will be compared to the population of patients admitted at the individual site during the time period of recruitment (Table 1). The nature and duration of all intervention contacts is documented and used to assess elements of the organizational development intervention activities. Study logs will also document when providers either discontinue delivering SBI (attrition), or are terminated from trauma center employment (turnover). After the completion of the clinical trial, study investigators will conduct semi-structured qualitative interviews with each site’s SBI provider champion(s).
3.13. Analysis plan
The purpose of the DO-SBIS statistical analyses is to compare trends in the primary outcomes for the 20 trauma centers assigned to intervention and control conditions. All primary statistical analyses will be conducted with the intent-to-treat sample. The investigation will use mixed effects, hierarchical regression models to test the primary provider, patient, and organizational level hypotheses for both continuous and discrete outcome variables.
A particular strength of mixed effects, hierarchical regression models is the ability to model patients, providers, and treatment nested within trauma center sites. A key consideration for the trial is this nesting and the ascertainment of associated intraclass correlations (ICC). All sample size estimates are therefore adjusted for the clustering of patients and providers within trauma center sites, using appropriate ICCs derived from the investigative group’s previous multisite trauma center studies.
3.14. Sample size and power
The primary outcome variables are intervention and control group: 1) Ratings of provider proficiency in the delivery of evidence-based MI intervention derived from the MITI, 2) Patient self-reported alcohol consumption 6- and 12-months post-injury, and 3) Staff ratings of organizational climate, culture, and readiness derived from the OSC and ORC. Power analyses were conducted to determine the appropriate number of patients for the study using the Power Analysis and Sample Size Software. Sample size estimates were inflated to account for any anticipated ICC using previously described methods.
Hypothesis 1
SBI providers at intervention sites will demonstrate greater proficiency in MI interventions over time as evidenced by improved MITI scores. Estimates of evidence-based MI workshop training on MI proficiency were derived from published reports on evaluations of MI workshop participants. For power analyses we used pre-training and follow-up assessment of a specific MI behavior, the percentage of open-ended questions asked. Previous investigation with community substance abuse counselors suggests that at baseline, untrained providers will ask between 25-30% (SD = 16%) open-ended questions. Follow-up assessments suggest that MI proficient providers will ask 41% (SD = 23%) open-ended questions, while untrained providers should remain in the 25-30% range. With α = 0.05 and 0.75 correlation of scores across assessment points, the investigation will require 20 providers (i.e., at least 1 provider at each site) to attain >80% power. The investigation anticipates having at least one SBI provider at each site. Of note, the anticipated ICC for providers nested within sites is negligible.
Hypothesis 2
Patients who receive SBI services at intervention trauma centers will demonstrate significant reductions in alcohol consumption over time compared to patients at control trauma centers. Estimates for the effect size in the current investigation are derived from previous studies across Level I trauma center sites. Previous MI interventions conducted by highly trained Ph.D. and M.S.W. level providers were associated with 12-month effect sizes of ≥ 0.30. We conservatively estimate that in this nationwide trial, routine trauma center SBI providers will be 60% as effective in delivery of MI, yielding a 12-month effect size of 0.18. Comparisons of blood alcohol concentrations from our previous studies that have randomly sampled injured patients suggest an ICC = 0.00028 across trauma center sites. Assuming a linearly increasing effect size culminating at 0.18, a constant correlation of 0.70 across assessments, an ICC = 0.00028, α = 0.05, and 30% 12-month attrition, to attain 80% power the investigation will require recruitment of 800 patients (40 patients * 20 sites) in order to retain 520 patients at the 12-month post-injury follow-up.
Hypothesis 3
Providers at intervention sites will demonstrate significantly improved scores on organizational climate, culture, and readiness inventories over time. Estimates of the impact of the MI training and organizational development activities on organizational climate, culture, and readiness are derived from previous acute care medical organizational assessments. Intervention sites are hypothesized to demonstrate scores on organizational culture-emphasis emotional support subscales reflective of high quality acute care environments, while control sites will be hypothesized to demonstrate scores reflective of lower quality acute care environments. Of particular note, organizational climate, culture, and readiness inventories are anticipated to demonstrate a high ICC. With an ICC = 0.53, α = 0.05, the investigation will require 200 providers (i.e., 10 providers at each site) to attain 80% power.
3.15 Study Design Considerations and Limitations
The trauma surgical study context influenced a number of important investigative design considerations and study limitations. The investigation used an AUDIT ≥ 20 cutoff to exclude heavy drinkers, because World Health Organization guidelines strongly recommend that patients with AUDIT scores ≥ 20 receive referral to a specialist for a diagnostic evaluation. The American College of Surgeons’ Alcohol mandate only requires that patients receive screening and intervention. Thus in order to comply with both the College mandate and the WHO guidelines, patients included in the study had AUDIT scores < 20 and received alcohol screening and brief interventions. Patients with AUDIT scores ≥ 20 were excluded from the study, yet continued to receive trauma center alcohol care that could include screening, intervention, and referral to treatment. A limitation of this approach may have been to exclude the most highly symptomatic drinkers and thus diminish the likelihood of finding an intervention treatment effect.
Also, in this implementation spectrum cluster randomized trial, we did not have the flexibility to require an extensive training period for providers, or train alternate providers beyond those selected by the trauma center as SBI champions. Therefore, we were not able to train providers to proficiency in motivational interviewing as might occur in efficacy or even effectiveness spectrum trials.
Another design consideration was that any of the five MITI global indices including: Global Spirit, Percentage Complex Reflections, Reflection to Question Ratio, Percent MI Adherence, and Percent Open Questions could have been selected for use inthe power and sample size estimations. Percent Open Questions was a MITI indice that had been used as a primary training outcome in previous investigations by members of the investigative group , thus providing preliminary data for power analyses; This indice also had the greatest “face validity” for pragmatically oriented trauma surgical co-investigators. Finally, human subjects’ considerations including the complexity of orchestrating IRB approvals across the 20 trauma center sites pragmatically influenced the decision to assess MI fidelity through audio recorded standardized patients interviews rather than audio recorded sessions with actual injured trauma center patients.
4. Results
A total of 40 SBI providers (16 intervention and 24 control) are undergoing serial assessments of MI skills with standardized patient assessments. Providers are predominantly female (95%) and from White backgrounds (88%). On average, providers have been employed at their respective trauma centers for 7 years and graduated from college or other educational programs 16 years prior to study participation. There were no significant differences between intervention and control group providers with regard to demographic, trauma center, or educational characteristics.
A total of 878 blood alcohol positive injured patients have been recruited from the 20 trauma center sites; 409 or 47% of patients were recruited from intervention sites and 469 or 53% were recruited from control sites. The average age of patients is 36.9 years old, 24% of patients are female, and 38% are from non-White backgrounds. The mean AUDIT score for patients is 10.1 (SD = 5.0). There were no significant differences between intervention and control group patients with regard to demographic or clinical characteristics.
A total of 219 (109 intervention and 110 control) trauma center staff are participating in the longitudinal organizational climate, culture, and readiness assessments. Providers are predominantly female (71%) and from White backgrounds (87%). On average, providers have been employed at their respective trauma centers for 9 years and graduated from college or other educational programs 16 years prior to study participation. There were no significant differences between intervention and control group staff with regard to demographic, trauma center, or educational characteristics.
5. Conclusion
The aims, design, and time trajectory of the DO-SBIS investigation derive from the opportunity presented by the American College of Surgeons’ policy mandate for SBI services as a requisite for Level I trauma center accreditation. A novel aim of the investigation is to conduct a definitive multisite randomized clinical trial that will inform future American College of Surgeons’ policy mandates for high quality evidence-based alcohol SBI services at Level I trauma centers. The American College of Surgeons’ commitment to review the empiric literature and mandate procedures derived from this evidence provides a unique “make it happen” regulatory context in which to conduct this general medical setting cluster randomized trial. Thus, findings from the study will be used to directly inform the development of performance standards and quality indicators that will be incorporated into future mandates and clinical practice guidelines targeting the sustainable delivery of high quality alcohol SBI procedures for trauma centers throughout the US.
ACKNOWLEDGEMENTS
Melanie-Kukana Maglaya, B.S., Roselyn Peterson, B.A., and Leiszle Ziemba, B.A., assisted in developing and formatting the manuscript, figures, tables, and references. Sources of support were United States National Institute of Health Grants R01 AA016102 and K24 MH086814.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Douglas F. Zatzick, Department of Psychiatry and Behavioral Sciences, Harborview Injury Prevention and Research Center, University of Washington School of Medicine, Seattle, WA 98104, USA.
Dennis M. Donovan, Alcohol and Drug Abuse Institute, Department of Psychiatry and Behavioral Sciences, University of Washington, Seattle, WA 98105, USA
Chris Dunn, Department of Psychiatry and Behavioral Sciences, Harborview Injury Prevention and Research Center, University of Washington School of Medicine, Seattle, WA 98104, USA
Gregory J. Jurkovich, Department of Surgery, Denver Health Care System, Denver, CO 80204, USA
Jin Wang, Harborview Injury Prevention and Research Center, University of Washington School of Medicine, Seattle, WA 98104, USA
Joan Russo, Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle, WA 98195, USA
Frederick P. Rivara, Department of Pediatrics, Harborview Injury Prevention and Research Center, University of Washington School of Medicine, Seattle, WA 98104, USA
Christopher D. Zatzick, Beedie School of Business, Simon Fraser University, Burnaby, BC V5A 1S6, Canada
Jeff R. Love, Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle, WA 98104, USA
Collin R. McFadden, Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle, WA 98104, USA
Larry M. Gentilello, Harborview Injury Prevention and Research Center, University of Washington School of Medicine, Seattle, WA 98104, USA
REFERENCES
- [1].United States. President’s Commission on Care for America’s Returning Wounded Warriors . Serve, support, simplify: Report of the president’s commission on care for america’s returning wounded warriors. President’s Commission on Care for America’s Returning Wounded Warriors; Washington, DC: 2007. [Google Scholar]
- [2].Bonnie RJ, Fulco CE, Liverman CT, editors. Reducing the burden of injury: Advancing prevention and treatment. National Academy Press; Washington, DC: 1999. [PubMed] [Google Scholar]
- [3].National Center for Injury Prevention . In: Cdc 2012. Office of Statistics and Programming, editor. Center for Disease Control and Prevention; Atlanta: 2012. [Google Scholar]
- [4].Bergen GS, National Center for Health Statistics (U.S.) Injury in the united states: 2007 chartbook. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; Hyattsville: 2008. [Google Scholar]
- [5].Soderstrom CA, Smith GS, Dischinger PC, et al. Psychoactive substance use disorders among seriously injured trauma center patients. JAMA. 1997;277:1769–74. [PubMed] [Google Scholar]
- [6].Dunn C, Zatzick D, Russo J, et al. Hazardous drinking by trauma patients during the year after injury. Journal of Trauma. 2003;54:707–12. doi: 10.1097/01.TA.0000030625.63338.B2. [DOI] [PubMed] [Google Scholar]
- [7].Ramchand R, Marshall GN, Schell TL, et al. Alcohol abuse and illegal drug use among los angeles county trauma patients: Prevalence and evaluation of single item screener. J Trauma. 2009;66:1461–7. doi: 10.1097/TA.0b013e318184821d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Annals of Surgery. 1999;230:473–80. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Zatzick D, Roy-Byrne P, Russo J, et al. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Archives of General Psychiatry. 2004;61:498–506. doi: 10.1001/archpsyc.61.5.498. [DOI] [PubMed] [Google Scholar]
- [10].Schermer CR, Moyers TB, Miller WR, Bloomfield LA. Trauma center brief interventions for alcohol disorders decrease subsequent driving under the influence arrests. J Trauma. 2006;60:29–34. doi: 10.1097/01.ta.0000199420.12322.5d. [DOI] [PubMed] [Google Scholar]
- [11].Saitz R, Alford DP, Bernstein J, et al. Screening and brief intervention for unhealthy drug use in primary care settings: Randomized clinical trials are needed. Journal of Addiction Medicine. 2010;4:123–30. doi: 10.1097/ADM.0b013e3181db6b67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Field CA, Baird J, Saitz R, Caetano R, Monti PM. The mixed evidence for brief intervention in emergency departments, trauma care centers, and inpatient hospital settings: What should we do? Alcoholism, Clinical and Experimental Research. 2010;34:2004–10. doi: 10.1111/j.1530-0277.2010.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zatzick D, Jurkovich G, Rivara FP, et al. A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Ann Surg. doi: 10.1097/SLA.0b013e31826bc313. Accepted for Publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gentilello LM, Ebel BE, Wickizer TM, Salkever DS, Rivara FP. Alcohol interventions for trauma patients treated in emergency departments and hospitals: A cost benefit analysis. Annals of Surgery. 2005;241:541–50. doi: 10.1097/01.sla.0000157133.80396.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Gentilello LM, Donovan DM, Dunn CW, Rivara FP. Alcohol interventions in trauma centers: Current practice and future directions. JAMA. 1995;274:1043–8. [PubMed] [Google Scholar]
- [16].Koepsell TD, Zatzick DF, Rivara FP. Estimating the population impact of preventive interventions from randomized trials. Am J Prev Med. 2011;40:191–8. doi: 10.1016/j.amepre.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].American College of Surgeons Committee on Trauma . Resources for the optimal care of the injured patient: 2006. American College of Surgeons Committee on Trauma; Chicago: 2006. [Google Scholar]
- [18].United States Congress . The patient protection and affordable care act. 2010. [Google Scholar]
- [19].Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In: Miller WR, Heather N, editors. Treating addictive behaviors: Processes of change. Plenum Press; New York: 1986. pp. 3–27. [Google Scholar]
- [20].Simpson DD. A conceptual framework for transferring research to practice. Journal of Substance Abuse Treatment. 2002;22:171–82. doi: 10.1016/s0740-5472(02)00231-3. [DOI] [PubMed] [Google Scholar]
- [21].Simpson DD, Flynn PM. Moving innovations into treatment: A stage-based approach to program change. J Subst Abuse Treat. 2007;33:111–20. doi: 10.1016/j.jsat.2006.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Aarons GA, Horowitz JD, Dlugosz LR, Ehrhart MG. The role of organizational processes in dissemination and implementation research. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: Translating science to practice. Oxford University Press; New York: 2012. pp. 128–53. [Google Scholar]
- [23].Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The re-aim framework. Am J Public Health. 1999;89:1322–7. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Glisson C, Schoenwald SK. The arc organizational and community intervention strategy for implementing evidence-based children’s mental health treatments. Mental Health Services Research. 2005;7:243–59. doi: 10.1007/s11020-005-7456-1. [DOI] [PubMed] [Google Scholar]
- [25].Porras JI, Robertson PJ. Organizational development: Theory, practice, and research. In: Dunnette MD, Hough LM, editors. Handbook of industrial and organizational psychology. Consulting Psychologists Press, Inc; Palo Alto: 1992. [Google Scholar]
- [26].Rogers EM. Diffusion of innovations. The Free Press; New York: 1995. [Google Scholar]
- [27].Terrell F, Zatzick DF, Jurkovich GJ, et al. Nationwide survey of alcohol screening and brief intervention practices at us level i trauma centers. J Am Coll Surg. 2008;207:630–8. doi: 10.1016/j.jamcollsurg.2008.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kettinger WJ, Teng JTC, Guha S. Business process change: A study of methodologies, techniques, and tools. Mis Quarterly. 1997;21:55–80. [Google Scholar]
- [29].Zatzick D, Rivara F, Jurkovich G, et al. Enhancing the population impact of collaborative care interventions: Mixed method development and implementation of stepped care targeting posttraumatic stress disorder and related comorbidities after acute trauma. Gen Hosp Psychiatry. 2011;33:123–34. doi: 10.1016/j.genhosppsych.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Dunn C. Brief motivational interviewing interventions targeting substance abuse in the acute care medical setting. Semin Clin Neuropsychiatry. 2003;8:188–96. doi: 10.1016/s1084-3612(03)00025-x. [DOI] [PubMed] [Google Scholar]
- [31].Miller WR, Yahne CE, Moyers TB, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J Consult Clin Psychol. 2004;72:1050–62. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- [32].Glisson C, Schoenwald SK, Hemmelgarn A, et al. Randomized trial of mst and arc in a two-level evidence-based treatment implementation strategy. J Consult Clin Psychol. 2010;78:537–50. doi: 10.1037/a0019160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Babor TF, De La Fuente JR, Saunders J, Grant M. The alcohol use disorders identification test: Guidelines for use in primary health care. World Health Organization; Geneva: 1989. [Google Scholar]
- [34].Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- [35].Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. J Consult Clin Psychol. 2009;77:1113–24. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Sommers MS, Dyehouse JM, Howe SR, Wekselman K, Fleming M. “Nurse, i only had a couple of beers”: Validity of self-reported drinking before serious vehicular injury. American Journal of Critical Care. 2002;11:106–14. [PubMed] [Google Scholar]
- [37].Donovan DM, Dunn CW, Rivara FP, et al. Comparison of trauma center patient self-reports and proxy reports on the alcohol use identification test (audit) Journal of Trauma. 2004;56:873–82. doi: 10.1097/01.ta.0000086650.27490.4b. [DOI] [PubMed] [Google Scholar]
- [38].Sobell LC, Sobell MB, Connors GJ, Agrawal S. Assessing drinking outcomes in alcohol treatment efficacy studies: Selecting a yardstick of success. Alcoholism, Clinical and Experimental Research. 2003;27:1661–6. doi: 10.1097/01.ALC.0000091227.26627.75. [DOI] [PubMed] [Google Scholar]
- [39].Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project match posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- [40].Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences (drinc): An instrument for assessing adverse consequences of alcohol abuse: Test manual. US Government Printing Office; Washington, DC: 1995. [Google Scholar]
- [41].Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The ptsd checklist: Reliability, validity, and diagnostic utility; The 9th Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio. 1994. [Google Scholar]
- [42].Kroenke K, Spitzer RL, Williams JB. The phq-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–3. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- [44].Glisson C, Landsverk J, Schoenwald S, et al. Assessing the organizational social context (osc) of mental health services: Implications for research and practice. Adm Policy Ment Health. 2008;35:98–113. doi: 10.1007/s10488-007-0148-5. [DOI] [PubMed] [Google Scholar]
- [45].Caldwell SD, Herold DM, Fedor DB. Toward an understanding of the relationships among organizational change, individual differences, and changes in person-environment fit: A cross-level study. Journal of Applied Psychology. 2004;89:868–82. doi: 10.1037/0021-9010.89.5.868. [DOI] [PubMed] [Google Scholar]
- [46].Hom P, Griffeth R. Employee turnover. Addison-Wesley; Reading, MA: 1995. [Google Scholar]
- [47].Gibbons RD, Hedeker D, DuToit S. Advances in analysis of longitudinal data. Annu Rev Clin Psychol. 2010;6:79–107. doi: 10.1146/annurev.clinpsy.032408.153550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Gibbons RD, Hedeker D. Application of random-effects probit regression models. Journal of Consulting and Clinical Psychology. 1994;62:285–96. doi: 10.1037//0022-006x.62.2.285. [DOI] [PubMed] [Google Scholar]
- [49].Murray DM. Design and analysis of group-randomized trials. New York: : Oxford University Press: 1998. Research designs; pp. 65–75. [Google Scholar]
- [50].Murray DM, Varnell SP, Blitstein JL. Design and analysis of group-randomized trials: A review of recent methodological developments. American Journal of Public Health. 2004;94:423–32. doi: 10.2105/ajph.94.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Varnell SP, Murray DM, Janega JB, Blitstein JL. Design and analysis of group-randomized trials: A review of recent practices. American Journal of Public Health. 2004;94:393–9. doi: 10.2105/ajph.94.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Roudsari B, Nathens A, Koepsell T, Mock C, Rivara F. Analysis of clustered data in multicentre trauma studies. Injury. 2006;37:614–21. doi: 10.1016/j.injury.2006.02.010. [DOI] [PubMed] [Google Scholar]
- [53].Zatzick D, Rivara FP, Nathens AB, et al. A nationwide us study of post-traumatic stress after hospitalization for physical injury. Psychol Med. 2007;37:1469–80. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- [54].Hintze JL. Pass user’s guide. NCSS; Kaysville: 2000. [Google Scholar]
- [55].Machin D. Sample size tables for clinical studies. Blackwell Science; Malden: 1997. [Google Scholar]
- [56].Baer JS, Rosengren DB, Dunn CW, et al. An evaluation of workshop training in motivational interviewing for addiction and mental health clinicians. Drug and Alcohol Dependence. 2004;73:99–106. doi: 10.1016/j.drugalcdep.2003.10.001. [DOI] [PubMed] [Google Scholar]
- [57].Zatzick D, Roy-Byrne P, Russo J, et al. Collaborative interventions for physically injured trauma survivors: A pilot randomized effectiveness trial. General Hospital Psychiatry. 2001;23:114–23. doi: 10.1016/s0163-8343(01)00140-2. [DOI] [PubMed] [Google Scholar]
- [58].Hemmelgarn AL, Glisson C, Dukes D. Emergency room culture and the emotional support component of family-centered care. Children’s Health Care. 2001;30:93–110. [Google Scholar]
- [59].Organization WH. Brief intervention for hazardous harmful drinking: A manual for use in primary care. World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- [60].Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: Systematic review and recommendations. The Milbank Quarterly. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]