Abstract
Objective
To examine and compare the family environment of preschool- and school-age children with cochlear implants and assess its influence on children’s executive function and spoken language skills.
Study Design
Retrospective between-subjects design.
Setting
Outpatient research laboratory.
Patients
Prelingually deaf children with cochlear implants and no additional disabilities, and their families.
Intervention(s)
Cochlear implantation and speech-language therapy.
Main Outcome Measures
Parents completed the Family Environment Scale and the Behavior Rating Inventory of Executive Function (or the preschool version). Children were tested using the Peabody Picture Vocabulary Test-4 and either the Preschool Language Scales-4 or the Clinical Evaluation of Language Fundamentals–4.
Results
The family environments of children with cochlear implants differed from normative data obtained from hearing children, but average scores were within one standard deviation of norms on all subscales. Families of school-age children reported higher levels of control than those of preschool-age children. Preschool-age children had fewer problems with emotional control when families reported higher levels of support and lower levels of conflict. School-age children had fewer problems with inhibition but more problems with shifting of attention when families reported lower levels of conflict. School-age children’s receptive vocabularies were enhanced by families with lower levels of control and higher levels of organization.
Conclusions
Family environment and its relation to language skills and executive function development differed across the age groups in this sample of children with cochlear implants. Because family dynamics is one developmental/environmental factor that can be altered with therapy and education, the present results have important clinical implications for family-based interventions for deaf children with cochlear implants.
Introduction
Enormous individual differences exist in the degree to which deaf children fully benefit from early intervention, despite significant advances in hearing technology including cochlear implantation. Children with similar audiological profiles who receive the same intervention often have drastically different communication, language, social, cognitive, educational, literacy, and vocational outcomes. Although many factors that contribute to outcomes have been identified, one area of children’s lives that has only recently been explored in the context of cochlear implant outcomes is the child’s family environment. The purpose of this investigation was twofold: first, to examine and compare the family environments of deaf preschool- and school-age children with cochlear implants and second, to identify possible developmental differences in the relations between family environment and post-implant language skills and executive function in preschoolers compared to school-age children with cochlear implants.
Much of the outcomes research on speech and language development involving hearing-impaired children has assumed that the developing child with hearing loss is a “closed-loop” system (see review of General Systems Theory1) – a system that is autonomous and disembodied from her/his immediate environment. Although the closed-loop system approach has led to important discoveries concerning spoken language development in isolation, this approach does not take the full scope of the child’s developmental experiences into account. One important factor that shapes children’s development is the family environment in which they are raised2. Most research on the family’s role in children’s cochlear implantation outcomes has emphasized the role of family in therapy3,4, support provided at home5,6, use of oral language7,8,9,10, family size7,8, education level7, socioeconomic status7,8,9, and several maternal factors including attachment and sensitivity11,12,13, qualitative and quantitative linguistic input to the child14,15, and sensitivity and self-efficacy15,16. Several proximal family factors that are positively related to children’s language development have emerged from these studies11,12,13,14,15,16, including the quality of talk between parents and children, mothers’ use of scaffolding, and maternal sensitivity. Expanding upon these established findings, one of the objectives of this study was to measure the impact of more global family factors (e.g., supportiveness and cohesion among family members, and organization and control in the home) on known areas of difficulty in children with cochlear implants (e.g., language and executive function). Family environment routinely has been used as a strong predictor of outcome in clinical populations (e.g., ADHD, cancer, spina bifida), but it has been overlooked in earlier outcome studies of children with deafness17,18,19,20,21,22.
In a preliminary investigation23, we examined family environments of 45 children with cochlear implants using a psychometrically rigorous, self-report questionnaire (the Family Environment Scale [FES] – 4th Edition24). The results revealed that families differed in non-clinically significant ways from children with normal hearing. Further, families with higher levels of self-reported control had children with smaller vocabularies. Families that reported a higher emphasis on achievement had children with fewer executive function and working memory problems. Finally, families that reported a higher emphasis on organization had children with fewer problems with inhibition. These preliminary results suggest that variability in cochlear implantation outcomes is related to specific aspects of the family environment. The importance of these findings lies in their application to aural (re-)habilitation. Specifically, family environment is dynamic and can be modified with education and therapy. If families function in ways that do not maximize their child’s potential with a cochlear implant, they can learn alternative ways to interact within their family unit that will increase their child’s likelihood of success. Other than our preliminary work, little is known about the role of the family environment on speech and language skills of deaf children with cochlear implants, including whether its influence on outcomes is consistent across development. Certainly, the developmental needs of children vary from infancy through young adulthood and thus, the influence of family environment should differ, as well.
The purpose of this investigation is to examine the influence of family environment on spoken language development and executive function in two groups of deaf children with cochlear implants – those who are preschool-age and those who are school-age. It is expected that the relations revealed between family environment and executive function and language in our preliminary study23 will be replicated and that differences in family functioning between families of preschoolers and school-age children will differentially be related to executive function and language development in these two groups of children with cochlear implants.
Method and Materials
Participants
Families of 59 prelingually deaf children with cochlear implants who had no additional disabilities were enrolled in the study because the parents had completed the FES (described below) as part of a longitudinal study on cochlear implant outcomes. The children comprised a wide age range (M=8.2 yrs; SD= 4.6 yrs; range = 1 – 18 years) and length of device use (M= 6.0 yrs; SD= 4.4 yrs; range = .5 – 16 years); 46 used oral communication strategies; 18 were binaurally implanted; and 5 used hearing aids in their nonimplanted ears. To examine differences across two important early developmental periods, children were separated into two groups: Preschool-Age (5 years and younger who had not started kindergarten; n = 20) and School-Age (5 years and older who were in kindergarten or grade school; n = 39). Table 1 displays a summary of the demographic characteristics of the children and their families. The school-age children were, by design, significantly older than the preschool-age children, t (57) = −9.118, p <.0001. As expected, the school-age children had used their cochlear implants longer, t (57) = −7.132, p <.0001, and were fit at an older age than the preschool-age children, t (57) = −3.431, p <.0001. The mothers of the preschool-age children (M = 3.9) had significantly higher levels of education than the school-age children (M = 3.0), t (57) = 2.240, p = .029 (although the difference was small: Associate Degree completion versus completed some college). The average maternal education levels of both groups approximated (p > .05) those achieved by women ages 18 years and older (M = 3.3) in the 2011 US Census (http://www.census.gov/hhes/socdemo/education/data/cps/2011/tables.html). In other words, the average education level of the mothers in both groups of children with cochlear implants is reflective of the average education level of women in the United States.
Table 1.
Family and child demographics
| Preschool-Age
|
School-Age
|
|||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age at test (yrs) | 3.3 | 1.2 | 10.7 | 3.5 |
| Age at implantation (yrs) | 1.4 | 0.6 | 2.6 | 1.4 |
| Duration of implant use (yrs) | 1.9 | 1.2 | 8.1 | 3.8 |
| Unaided better-ear PTA (dB HL) | 105.0 | 12.6 | 106.5 | 15.1 |
| * Maternal education | 3.9 | 1.6 | 3.0 | 1.3 |
| Percent oral communicators | 70.0 | 82.1 | ||
| Percent female | 35.0 | 48.7 | ||
| Percent single-parent homes | 40.0 | 12.8 | ||
Maternal education was coded based on levels of formal education: 1 = some high school, 2 = high school diploma, 3 = some college, 4 = Associate degree, 5 = Bachelor’s degree, 6 = Master’s degree, 7 = Doctorate degree.
Materials
The Family Environment Scale (FES)24, a 90-item self-report true-false questionnaire, assesses three dimensions of family environment: (a) the emphasis on interpersonal relationships within the family (Relationship), (b) goals, activities and interests within the family (Personal Growth), and (c) the emphasis on structure, organization and rules in running the family (System Maintenance) using 10 subscales (see Table 2). Parents completed the FES Real Form (Form R), which assesses how parents view how their family really is, as opposed to how they wish it would be. Raw scores were converted to T-scores, which were based on a heterogeneous sample of 1432 families. T-scores above 60 or below 40 are considered clinically significant. Four factor scores (used previously24,25,26,27) were calculated by combining the standard scores of particular subscales: the Family Relationship Index (FRI), and Supportive, Conflicted, and Controlling factors. The FES was selected to investigate family environment because of its widespread use, predictive validity and reliability17,18,19,20,21,22.
Table 2.
Family Environment Scale24 dimensions and subscales
| Dimensions
|
|||
|---|---|---|---|
| Relationship | Personal Growth | System Maintenance | |
| Subscales | Cohesion Expressiveness Conflict |
Independence Achievement Orientation Intellectual-Cultural Orientation Active-Recreational Orientation Moral-Religious Emphasis |
Organization Control |
Receptive vocabulary, language skills and executive function were evaluated with norm-referenced tests. Receptive vocabulary was assessed with the Peabody Picture Vocabulary Test–4 (PPVT–4)29. The language of children up to 6-years-old was measured using the Auditory Comprehension, Expressive Communication and Total Language subscales of the Preschool Language Scales-4 (PLS–4)30. The Clinical Evaluation of Language Fundamentals–4 (CELF–4)31 Core Language Score (a standard score based on an age-based normative sample) was used to assess global language skills in children ages 5 to 18 years. Due to the overlap in the age ranges included in the PLS and the CELF, speech-language pathologists familiar with the children and experienced in testing young children with cochlear implants determined if a 5- to 6-year-old child would be best assessed with the CELF or the PLS.
The Behavior Rating Inventory of Executive Function (BRIEF)32, an 86-item parent-report questionnaire, was used to assess everyday real-world executive function behaviors of children ages 5 to 18 years (School-Age). The preschool version, the 63-item parent BRIEF-P33, was used with children ages 2;0 to 5;11 not presently in kindergarten (Preschool-Age). The BRIEF measures eight core domains of executive functioning, whereas the BRIEF-P measures a subset of five. Only the five domains that appear on both inventories (Inhibit, Shift, Emotional Control, Working Memory, and Planning/Organize) were used in the data analyses. Domain scores are converted to T scores using gender- and age-specific norms32. T-scores above 60 are considered elevated and those above 65 are clinically significant. The BRIEF has been used in several clinical populations including children with ADHD, autism spectrum disorder, TBI, and cochlear implants34,35,36,37,38.
Procedure
Caregivers completed the FES and the BRIEF or BRIEF-P, while the children were administered the PPVT-4 and either the PLS-4 or the CELF-4 by experienced speech-language pathologists in our center. Some children were unable to complete both the vocabulary and the language measures due to time constraints and/or child behavior and attention. For oral communicators, language and vocabulary tests were administered with auditory and visual cues; Total communicators were administered the language and vocabulary tests with auditory, visual, and sign cues. Both spoken and signed responses were accepted for the PLS-4 and the CELF-4.
Results
Family environments of children with cochlear implants
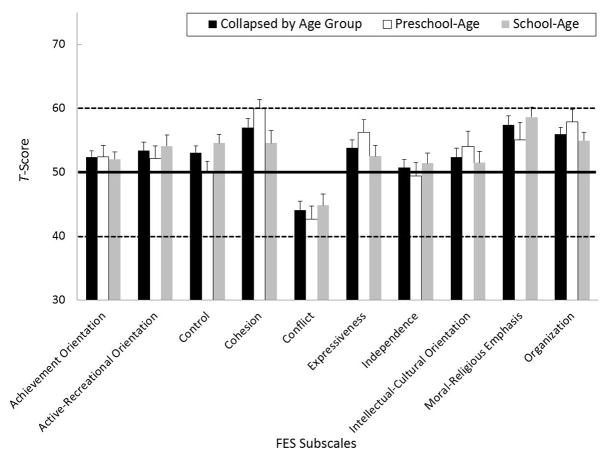
The black-filled bars in Figure 1 display the mean T-scores (+1 standard error) for each of the 10 FES subscales for the families collapsed by age group. On average, families scored within one standard deviation of the mean on all subscales of the FES indicating healthy and typical family environments. The scores on 8 of the subscales were not normally distributed. One-sample t-tests and one-sample Wilcoxon Signed Rank tests (for those scales that were not distributed normally) revealed that as a group, families of children with cochlear implants reported significantly higher (p ≤ .05) FES scores than the normative sample of families with typically hearing children on the Achievement, Active-Recreational, Control, Cohesion, Expressiveness, Moral-Religious, and Organization subscales, and significantly lower scores on the Conflict subscale.
Figure 1.
Mean T-Scores (+1 SE) for the preschool-age children with cochlear implants (unfilled bars) and the school-age children with cochlear implants (gray-filled bars) on each of the FES subscales. The black bars display data for the children collapsed by age group. The normative mean and +/− 1 standard deviation (obtained from 1432 children with normal hearing24) are indicated by the dark solid and dashed lines, respectively.
The unfilled and gray-filled bars in Figure 1 display mean FES subscale and factor scores for the preschool- and school-age children’s families, respectively. Families of school-age children with cochlear implants (M = 54.54) reported higher levels of control than families of preschool-age children (M = 50.10), t = −1.97, p = .041. The groups were not significantly different on any of the other subscales or the four FES factor scores (which combine specific FES subscales).
Language of children with cochlear implants
As expected, children with cochlear implants scored more than one standard deviation below the normative mean of 100 on the PPVT-4 (M = 83.46) and the PLS-4 (Total Language score M = 73.42), and were right at one standard deviation below the mean on CELF-4 (Core Language score M = 85.00). Because the preschool-age children typically received the PLS-4 for language testing and the school-age children received the CELF-4, direct comparisons between the two groups using the same language test were not possible. However, to determine whether the preschool- and school-age groups differed in their respective language abilities, standard scores on the two language measures were converted to z-scores. An independent-samples t-test revealed that the two groups’ language z-scores were not significantly different from one another. Descriptively, approximately 70% of the 17 preschoolers with scores on the PLS-4 and 48% of the 31 school-age children with scores on the CELF-4 were more than one standard deviation below the normative mean. With regard to vocabulary, 44% of the 11 preschoolers with scores on the PPVT and 60% of the 28 school-age children were more than one standard deviation below the normative mean. An independent samples t-test revealed that school-age and preschool-age children’s PPVT standard scores were not significantly different from one another. These results suggest that the two groups were similarly delayed in their language and vocabulary development. Consequently, developmental differences observed in family environment and/or executive function are unlikely to be related to language and vocabulary delay in this sample.
Executive function of children with cochlear implants
With regard to executive function, our sample scored significantly above the normative mean of 50 indicating more difficulties than expected with Inhibiting behaviors (M = 54.07), t (54) = 2.65, p = .011, Shifting attention (M = 53.65), t (54) = 2.65, p = .01, and Working Memory (M = 54.54), t (54) = 3.40, p <.001. No significant differences were observed in the means of preschoolers and school-age children on any of the five shared BRIEF/BRIEF-P scales of executive function. Although the scores on the subscales were normally distributed (according to Kolmogorov-Smirnov tests), the distributions for both groups were bimodal indicating that whereas the majority of the scores clustered around the mean, several children scored much higher (greater disturbances) than would be expected. Children whose scores fell in the upper tail of the distribution scored at least 1 standard deviation above the mean, indicating elevated to clinically significant difficulties with executive function. Table 3 shows a comparison of the percent of preschool- and school-age children scoring in the elevated range (i.e., one standard deviation above the mean) on each of the BRIEF/BRIEF-P scales. In a normal distribution, one would expect these percentages to be approximately 16% on the positive tail of the distribution. There was a trend for more preschool-age children to score at least one standard deviation above the mean than school-age children on all BRIEF-P scales with the exception of emotional control.
Table 3.
Percentage of preschool- and school-age children with cochlear implants scoring more than 1 standard deviation above the mean on the shared BRIEF/BRIEF-P scales
| Preschool-Age | School-Age | |
|---|---|---|
| Inhibit | 29.4% | 21.1% |
| Shift | 29.4% | 18.4% |
| Emotional Control | 17.6% | 21.1% |
| Working Memory | 47.1% | 28.9% |
| Plan/Organize | 29.4% | 21.1% |
The relation between executive function and family environment in children with cochlear implants
In order to further investigate the age-effects found in executive function, Pearson correlations were carried out between BRIEF/BRIEF-P scores and the four factors of the FES in both preschoolers and school-age children. The FES factor scores were chosen over the subscale scores to reduce the total number of correlation analyses run (thereby reducing the family-wise error rate). Note that corrections were not made for multiple analyses, so appropriate cautions should be taken in interpreting the results. This approach was used here because although this was a highly novel investigation, the factors of interest were driven by theory, thereby reducing the need for statistical correction. Families high in supportiveness and mutual interest (Supportive factor) and those that were low in conflict and high on cohesiveness and organization (Conflicted factor) tended to have preschoolers with fewer problems with emotional control, r = −.603, p = .01 and r = .518, p = .033, respectively. Families who were low in conflict and high on cohesiveness and organization (Conflicted factor) tended to have school-age children with fewer problems with inhibitory control, r = .388, p = .016, but more problems with shifting attention, r = −.355, p = .029. In addition to zero-order correlations, partial correlations controlling for language development were carried out between family environment and executive function, because neurocognitive development and language are interdependent44,45. When language of preschoolers (PLS-4 Total Language score) was statistically controlled, families high in supportiveness and mutual interest continued to have preschoolers with fewer problems with emotional control, r = −.573, p = .032. In contrast, the Conflicted factor was no longer significantly correlated with emotional control in preschoolers. When language of school-age children (CELF-4 scores) was statistically controlled, the same relations as the zero-order correlations were found: families who were low in conflict and high on cohesiveness and organization were more likely to have school-age children with fewer problems with inhibitory control, r = .391, p = .036, but more problems with shifting attention, r = −.397, p = .033. These results suggest differential relations between family environment and executive function in families with preschool-age children compared to those with school-age children who have cochlear implants, even when controlling for language development.
The relation between language and family environment in children with cochlear implants
There was no direct relationship between family environment and language for the preschoolers. For the school-age children, none of the FES factor scores were correlated with language or vocabulary, but two individual subscales were: families reporting higher levels of control had children with smaller receptive vocabularies, r = −.464, p = .013; and those reporting higher levels of organization within the family unit had children with larger receptive vocabularies, r = .440, p = .019. These subscale analyses were carried out on both the preschool and school-age children’s data to compare with the results from our previous investigation23.
Discussion
As a group, families of children with cochlear implants differ from families of children with normal hearing, but not in clinically significant ways. Within the relationship dimension of the FES, families of children with cochlear implants had higher levels of cohesiveness and expressiveness, and lower levels of conflict compared to the norms, indicating the existence of overall positive relationships within the family system. Within the system maintenance dimension, families of children with cochlear implants had higher levels of organization and control compared to the norms, suggesting fairly structured and rule-bound day-to-day family environments. Finally, within the personal growth dimension which reflects the relationship between the family and the larger social context, families of children with cochlear implants scored higher on achievement orientation, active-recreational orientation, and moral-religious orientation than the normative sample, suggesting an emphasis on competition, participation in activities outside the home, and an emphasis on moral or religious values within the home.
As a group, deaf children with cochlear implants in our sample were delayed in receptive vocabulary and global language and showed more difficulties than typically hearing children of the same age in specific areas of executive function, including inhibition, shifting attention, and working memory. The language and executive function scores of children in this sample were atypical, but generally consistent with the body of literature on outcomes after cochlear implantation9,34,38,39,40. Furthermore, we replicated previous findings from our lab, in which we found a larger-than-expected percentage of children, particularly preschool-age children, with scores in the elevated range on executive function34. It is possible that the atypical executive function scores observed in our study could be attributed to the language delays evident in our sample of children. One investigation41, which sought to disentangle executive function from language development, reported that executive function of 8- to 12-year-old children with deafness (who used hearing aids or cochlear implants) was not significantly different from their normal-hearing peers when language was statistically controlled. Certainly further more detailed investigations are needed to better understand the complicated developmental interactions between executive function and language in both preschool and school-age children with cochlear implants.
Our first objective was to examine and compare the family environments of preschool-and school-age children with cochlear implants. The only significant developmental difference that emerged was that families of school-age children reported higher levels of control than those with preschool-age children. This developmental difference in family structure could be attributed to more rules needed as children gain independence. Although younger children need monitoring and oversight because of their adaptive-independent behavior, older children need to know what is expected of them even when a parent is not physically present. The FES Control subscale essentially measures inflexibility and emphasis on rules and order in the family. At preschool ages, this degree of inflexibility and rule-emphasis may be less manifest in the family because parents are obviously in charge and because there needs to be some flexibility in parenting a preschooler. However, for school age children there is a need for more obvious manifestations of rules, and better behavior is generally expected, leading to increased inflexibility in expectations for rule-following.
Our second objective was to identify possible developmental differences in the relations between family environment and post-implant language skills and executive function in our sample of preschoolers and school-age children with cochlear implants. We found no direct relationship between family environment and global language for either age group or between family environment and vocabulary for the preschool-age children. However, families of school-age children who reported higher levels of organization within the family unit had children with larger receptive vocabulary abilities, and those families that reported higher degrees of control within the family unit had school-age children with smaller receptive vocabularies, both supporting and extending our previous results23. The Organization and Control subscales of the FES together comprise the System Maintenance dimension of the FES, which indexes how the family governs and sustains itself. FES Control implies inflexibility, rule emphasis, and obvious hierarchy of power. FES Organization implies more planning, clear expectations, and neatness without the control-power component. Organization keeps order by prevention and planning, whereas Control keeps order by imposing rules. Presumably, the more Organization in a family, the less Control that is needed. These underlying dimensions of the family environment appear to have differential effects on receptive vocabulary in school-age children with cochlear implants. Higher degrees of structure and organization within the family appear to promote better vocabulary in our sample, whereas attempts to maintain internal family functioning through unbalanced control and rigidly fixed rules may in fact have the opposite effect on vocabulary development. The data for both the Control and Organization subscales were normally distributed with scores ranging from 32 to 70 and from 37 to 69 for each subscale, respectively. Therefore, it is unlikely that the results are due to limited range of variability in the FES scores on these two subscales. However, future investigations with a larger sample, along with observations of family interactions, will explore the influence of these two family factors on vocabulary development.
The finding that family environment was not related to receptive vocabulary outcomes in the preschool-age children could reflect the operation of at least two possible underlying factors. First, a smaller percentage of the participants in the preschool-age group (55%) completed the PPVT-4 than the school-age group (72%). Therefore, the power was reduced in the preschool children’s analysis relative to the school-age children’s analysis. Second, the school-age children’s families had significantly higher levels of control than the preschool-age group. If higher levels of control within the family unit fail to support good receptive vocabulary in children as this investigation and our previous investigation23 suggest, and school-age children’s families assert more control than preschool-age families, then it would not be entirely surprising to find developmental differences in the relation between levels of control in the family and receptive vocabulary growth. No clear developmental trends were noted in the relationship between organization within the family and receptive vocabulary across the two age groups.
Although the Control subscale score on the FES reflects how a family functions internally rather than assessing a style of communication, these results are particularly interesting in light of a large body of previous work that suggests that word-learning and both expressive and receptive language skills are enhanced more when mothers are sensitive to what the child focuses on rather than redirecting the child’s selective/focused attention to a different item42,43,44. The current investigation was not designed to tease apart communication style from family interaction style, but the results support and extend previous published findings that families that assert more control are more likely to have children who display a more impoverished vocabulary. It should be noted, however, that the observed relationship could go in the opposite direction too: children with cochlear implants who have limited language skills may perhaps drive family members to assert more control and oversight.
Using established factors (Supportive, Conflicted, and Controlling) derived through factor analysis of the FES26, we observed developmental differences in the relations between the family environments and executive function of children with cochlear implants. We found that supportive families (Supportive factor) and families with low levels of conflict (Conflicted factor) had preschool-age children with fewer problems related to emotional control. For school-age children, we found that only the Conflicted factor was significantly related to executive function: families with low conflict and high cohesiveness had children with fewer problems related to inhibitory control, but reported more problems with shifting behavior. This finding is consistent with earlier work in children who have chronic illnesses26: children with behavior problems had families that were less supportive and had higher levels of conflict than those who did not have behavior problems. The unexpected relationship between lower FES Conflicted scores and higher BRIEF Shift scores reflects a difficulty maintaining response set (e.g., shifting attention too easily) in children from families with low degrees of conflict coupled with high amounts of cohesion and organization. Although this finding requires further exploration, the percentage of school-age children with cochlear implants scoring in the elevated range on shifting behaviors (one standard deviation or more above the mean) is approximately the value expected for the norm sample (18% versus 16%). Hence, high Shift scores in the school-age group would be high not only for school-aged children with cochlear implants but also for the norm group.
There is now a growing body of evidence that the quality and quantity of communication directed at normal-hearing children facilitates language acquisition45 and executive function46,47,48. The present study provides additional evidence of a relationship between family environment and both language and executive function in children with cochlear implants. The literature on both healthy and other clinical populations suggests that children with fewer behavior problems and better executive function tend to have families that provide support, scaffolding, consistency, and structure. That being said, one would expect that these relations would differ in families of children who are deaf based on a social constructivist perspective that considers the social experiences within which individual executive processes and language learning develop49. We have adopted this theoretical perspective because we believe it will allow us to better understand and predict individual differences in outcomes that are so pervasive in children after cochlear implantation. The experiences of deaf children and their families differ from one another, and they differ from those of families with typically hearing children. Understanding how these differences impact language and cognitive development over time is an important unexplored area of study that has significant impact for the development of novel interventions designed to meet the needs of individual families.
There is mounting evidence that a period of auditory deprivation affects the development of core neurocognitive processes including foundational aspects of executive function50,51. These domain-general processes are responsible for domain-specific learning and information processing skills such as learning spoken language – a primary expectation of families who choose cochlear implantation as a treatment for their deaf children. Our findings offer further evidence for the existence of a subpopulation of deaf children with cochlear implants that are at high risk for executive function difficulties, particularly preschool-age children. Further research is necessary to understand the bi-directional relations between spoken language development and executive function. It is possible that increased proficiency in spoken language after implantation will allow the child to use language and verbal coding as a mediating tool for self-regulatory processes such as emotional and cognitive control. It is also very likely that increases in these cognitive control processes will positively impact the child’s ability to actively listen to and use spoken language.
The results of this study suggest that family environment of deaf children with cochlear implants impacts the development of these executive processes and does so differentially in preschool- and school-age children, supporting Vygotskian developmental theory52, as well as recent findings on the social origins of the development of executive function, in which experiences and activities in the family support the development of executive control processes across early childhood49,53. In addition to global family measures such as the FES, future research should include more specific measures of the family dynamics such as parenting style, parent-child relations, child temperament, and direct observations of family interactions. Continued research in this area using larger, longitudinal samples and more sophisticated statistical modeling techniques will enable us to address some of these complex multidimensional developmental questions in this clinical population. The clinical implications of this work lie in its potential to shape more targeted and innovative intervention and rehabilitation strategies for families of children with cochlear implants. If a family presents with interaction styles pre- or post-implantation that are found be less supportive of optimal outcomes in children with cochlear implants than other types of family dynamics, Otologists, Neurotologists, Audiologists and Speech-Language Pathologists could recommend that families seek education and/or counseling on specific strategies for modifying their family dynamics to facilitate the best possible outcomes for their child.
Acknowledgments
Sources of Support for this work:
National Institutes of Health, NIH-NIDCD T32 DC00012 and R01 DC009581 (to D.B. Pisoni)
We are grateful to Shirley Henning and Bethany Colson for their contribution to data collection and Anh Nguyen for her assistance in data entry. This work was supported by the NIH-NIDCD T32 DC00012 and DC009581. Portions of this work were presented at the 13th Symposium of Cochlear Implants in Children, Chicago, IL (July, 2011).
Contributor Information
Rachael Frush Holt, Department of Speech and Hearing Sciences, Indiana University
Jessica Beer, DeVault Otologic Research Laboratory, Department of Otolaryngology-Head and Neck Surgery, Indiana University School of Medicine
William G. Kronenberger, Department of Psychiatry, Indiana University School of Medicine
David B. Pisoni, DeVault Otologic Research Laboratory, Department of Otolaryngology- Head and Neck Surgery, Indiana University School of Medicine
References
- 1.von Bertalanffy L. General System Theory: Foundations, Development, Applications: Revised Edition. New York: George Braziller; 1968. [Google Scholar]
- 2.Belsky J. Early human experience: A family perspective. Dev Psychol. 1981;17:3–23. [Google Scholar]
- 3.Bertram B, Päd D. Importance of auditory-verbal education and parents’ participation after cochlear implantation of very young children. Ann Otol Rhinol Laryngol Suppl. 1995;166:97–100. [PubMed] [Google Scholar]
- 4.Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106:1–9. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- 5.Edwards L, Thomas F, Rajput K. Use of revised children’s implant profile (GPSHChIP) in candidacy for paediatric cochlear implantation and in predicting outcome. Int J Audiol. 2009;48:554–60. doi: 10.1080/14992020902894533. [DOI] [PubMed] [Google Scholar]
- 6.Nikolopoulos TP, Gibbin KP, Dyar D. Predicting speech perception outcomes following cochlear implantation using Nottingham Children’s Implant Profile (NChIP) Int J Ped Otorhinolaryngol. 2004;68:137–41. doi: 10.1016/j.ijporl.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 7.Geers A, Brenner C, Davidson L. Factors associated with development of speech perception skills in children implanted by age five. Ear Hear Suppl. 2003;24:24S–35S. doi: 10.1097/01.AUD.0000051687.99218.0F. [DOI] [PubMed] [Google Scholar]
- 8.Geers AE, Strube MJ, Tobey EA, Pisoni DB, Moog JS. Epilogue: Factors Contributing to Long-Term Outcomes of Cochlear Implantation in Early Childhood. Ear Hear Suppl. 2011;32:84S–92S. doi: 10.1097/AUD.0b013e3181ffd5b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holt RF, Svirsky MA. An exploratory look at pediatric cochlear implantation: Is earliest always best? Ear Hear. 2008;29:492–511. doi: 10.1097/AUD.0b013e31816c409f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirk KI, Miyamoto RT, Lento CL, Ying E, O’Neill T, Fears B. Effects of age at implantation in young children. Ann Otol Rhinol Laryngol Suppl. 2002;189:69–73. doi: 10.1177/00034894021110s515. [DOI] [PubMed] [Google Scholar]
- 11.Lederberg AR, Mobley CE. The effect of hearing impairment on the quality of attachment and mother-toddler interaction. Child Dev. 1990;61:1596–604. doi: 10.1111/j.1467-8624.1990.tb02886.x. [DOI] [PubMed] [Google Scholar]
- 12.Pratt S. Nonverbal play interaction between hearing mothers and young deaf children. Ear Hear. 1991;12:328–36. doi: 10.1097/00003446-199110000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Pressman L, Pipp-Siegel S, Yoshinaga-Itano C, Deas A. Maternal sensitivity predicts language gain in preschool children who are deaf and hard of hearing. J Deaf Stud Deaf Educ. 1999;2:27–36. doi: 10.1093/deafed/4.4.294. [DOI] [PubMed] [Google Scholar]
- 14.DesJardin JL, Ambrose SE, Eisenberg LS. Literacy skills in children with cochlear implants: The importance of early oral language and joint storybook reading. J Deaf Stud Deaf Educ. 2008;14:22–43. doi: 10.1093/deafed/enn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DesJardin JL, Eisenberg LS. Maternal contributions: Supporting language development in young children with cochlear implants. Ear Hear. 2007;28:456–69. doi: 10.1097/AUD.0b013e31806dc1ab. [DOI] [PubMed] [Google Scholar]
- 16.Desjardin JL. Maternal Perceptions of Self-Efficacy and Involvement in the Auditory Development of Young Children with Prelingual Deafness. J Early Intervention. 2005;27:193–209. [Google Scholar]
- 17.Biederman J, Milberger S, Faraone SV, et al. Family environment risk factors for attention-deficit hyperactivity disorder: A test of Rutter’s indicators of adversity. Arch Gen Psychiatry. 1995;52:464–70. doi: 10.1001/archpsyc.1995.03950180050007. [DOI] [PubMed] [Google Scholar]
- 18.Loomis JW, Javornisky JG, Monahan JJ, Burke G, Lindsay A. Relations between family environment and adjustment outcomes in young adults with spina bifida. Dev Med Child Neurol. 1997;39:620–7. doi: 10.1111/j.1469-8749.1997.tb07498.x. [DOI] [PubMed] [Google Scholar]
- 19.Rice F, Harold GT, Shelton KH, Thapar A. Family conflict interacts with genetic liability in predicting childhood and adolescent depression. J Am Acad Child Adolesc Psychiatry. 2006;45:841–8. doi: 10.1097/01.chi.0000219834.08602.44. [DOI] [PubMed] [Google Scholar]
- 20.Rivara JB, Jaffe KM, Polissar NL, Fay GC, Liao S, Martin KM. Predictors of family functioning and change 3 years after traumatic brain injury in children. Arch Phys Med Rehabil. 1996;77:754–64. doi: 10.1016/s0003-9993(96)90253-1. [DOI] [PubMed] [Google Scholar]
- 21.Rousey AM, Wild M, Blacher J. Stability of measures of the home environment for families of children with severe disabilities. Res Dev Disabilities. 2002;23:17–35. doi: 10.1016/s0891-4222(01)00089-0. [DOI] [PubMed] [Google Scholar]
- 22.Varni JW, Katz ER, Colegrove R, Dolgin M. Family functioning predictors of adjustment in children with newly diagnosed cancer: A prospective analysis. J Child Psychol Psychiatry. 1996;37:321–8. doi: 10.1111/j.1469-7610.1996.tb01409.x. [DOI] [PubMed] [Google Scholar]
- 23.Holt RF, Beer J, Kronenberger WG, Pisoni DB, Lalonde K. Contribution of family environment to pediatric cochlear implant users’ speech and language outcomes: Some preliminary findings. J Speech Lang Hear Res. 2012 doi: 10.1044/1092-4388(2011/11-0143). (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moos RH, Moos BS. Family Environment Scale manual. 4. Menlo Park, CA: Mind Garden, Inc; 2009. [Google Scholar]
- 25.Holahan CJ, Moos RH. Social support and psychological distress: A longitudinal analysis. J Abnorm Psychol. 1981;90:365–70. doi: 10.1037//0021-843x.90.4.365. [DOI] [PubMed] [Google Scholar]
- 26.Kronenberger WG, Thompson RJ., Jr Dimensions of family functioning with chronically ill children: A higher order factor analysis of the Family Environment Scale. J Clin Child Psychol. 1990;19:380–8. [Google Scholar]
- 27.Olson DH. Circumplex model VII: Validation studies and FACES III. Fam Process. 1986;25:337–51. doi: 10.1111/j.1545-5300.1986.00337.x. [DOI] [PubMed] [Google Scholar]
- 28.Olson DH, Sprenkle DH, Russell CS. Circumplex model of marital and family systems I: Cohesion and adaptability dimensions, family types, and clinical applications. Fam Process. 1979;18:3–28. doi: 10.1111/j.1545-5300.1979.00003.x. [DOI] [PubMed] [Google Scholar]
- 29.Dunn LM, Dunn DM. Peabody Picture Vocabulary Test. 4. Minneapolis, MN: Pearson; 2007. [Google Scholar]
- 30.Zimmerman IL, Steiner BS, Pond R. Preschool Language Scale Fourth Edition (PLS-4) San Antonio, TX: PsychCorp; 2002. [Google Scholar]
- 31.Semel E, Wiig EH, Secord W. Clinical Evaluation of Language Fundamentals. 4. San Antonio, TX: PsychCorp; 2003. [Google Scholar]
- 32.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function (BRIEF) Torrence, CA: Psychological Assessment Resources, Inc; 2000. [Google Scholar]
- 33.Gioia GA, Espy KA, Isquith PK. Behavior Rating Inventory of Executive Function -Preschool Version (BRIEF-P) Torrence, CA: Psychological Assessment Resources, Inc; 2003. [Google Scholar]
- 34.Beer J, Kronenberger WG, Pisoni DB. Executive function in everyday life: Implications for young cochlear implant users. Cochlear Implants Int Suppl. 2011;12:S89–S91. doi: 10.1179/146701011X13001035752570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilotty L, Kenworthy L, Sirian L, Black DO, Wagner AE. Adaptive skills and executive function in autism spectrum disorders. Child Neuropsychol. 2002;8:241–8. doi: 10.1076/chin.8.4.241.13504. [DOI] [PubMed] [Google Scholar]
- 36.Jarratt KP, Riccio CA, Siekierski B. Assessment of Attention Deficit Hyperactivity Disorder (ADHD) using the BASC and BRIEF. Appl Neuropsychol. 2005;12:83–93. doi: 10.1207/s15324826an1202_4. [DOI] [PubMed] [Google Scholar]
- 37.Mangeot S, Armstrong K, Colvin AN, Yeates KW, Taylor HG. Long-term executive function deficits in children with traumatic brain injuries: Assessment using the Behavior Rating Inventory of Executive Function (BRIEF) Child Neuropsychol. 2002;8:271–84. doi: 10.1076/chin.8.4.271.13503. [DOI] [PubMed] [Google Scholar]
- 38.Pisoni DB, Conway CM, Kronenberger W, Henning S, Anaya E. Executive function and cognitive control in deaf children with cochlear implants. In: Marschark MS, editor. Oxford Handbook of Deaf Studies, Language, and Education. 2. Vol. 1. New York: Oxford University Press; 2010. [Google Scholar]
- 39.Svirsky MA, Teoh S-W, Neuburger H. Development of language and speech perception in congenitally, profoundly deaf children as a function of age at cochlear implantation. Audiol Neurootol. 2004;9:224–33. doi: 10.1159/000078392. [DOI] [PubMed] [Google Scholar]
- 40.Dettman SJ, Pinder D, Briggs RJS, Dowell RC, Leigh JR. Communication development in children who receive the cochlear implant younger than 12 months: Risks versus benefits. Ear Hear Suppl. 2007;28:11S–18S. doi: 10.1097/AUD.0b013e31803153f8. [DOI] [PubMed] [Google Scholar]
- 41.Figuera B, Edwards L, Langdon D. Executive function and language in deaf children. J Deaf Stud Deaf Educ. 2008;13:362–77. doi: 10.1093/deafed/enm067. [DOI] [PubMed] [Google Scholar]
- 42.Akhtar N, Dunham F, Dunham P. Directive interactions and early vocabulary development: The role of joint attentional focus. J Child Lang. 1991;18:41–9. doi: 10.1017/s0305000900013283. [DOI] [PubMed] [Google Scholar]
- 43.Kaiser A, Hemmeter M, Ostrosky M, Fischer R, Yoder P, Keeper M. The effects of teaching parents to use responsive interaction strategies. Topics in Early Childhood Special Educ. 1996;16:375–406. [Google Scholar]
- 44.Tomasello M, Farrar M. Joint attention and early language. Child Dev. 1986;57:1454–63. [PubMed] [Google Scholar]
- 45.Bates E, Bretherton I, Beeghly-Smith M, McNew S. Social bases of language development: A reassessment. In: Reuse HW, Lipsitt LP, editors. Adv in Child Dev Behavior. Vol. 16. 1982. pp. 8–75. [DOI] [PubMed] [Google Scholar]
- 46.Bernier A, Carlson SM, Whipple N. From external regulation to self-regulation: Early parenting precursors of young children’s executive functioning. Child Dev. 2010;81:326–339. doi: 10.1111/j.1467-8624.2009.01397.x. [DOI] [PubMed] [Google Scholar]
- 47.Bibcok MB, Carpendale JM, Muller U. Parental scaffolding and the development of executive function. In: Lewis C, Carpendale JM, editors. Social Interaction and the Development of Executive Function. New Dir Child Adolesc Dev. Vol. 123. 2009. pp. 17–34. [DOI] [PubMed] [Google Scholar]
- 48.Landry SH, Miller-Loncar CL, Smith KE, Swank PR. The Role of Early Parenting in Children’s Development of Executive Processes. Developmental Neuropsychol. 2002;21:15–41. doi: 10.1207/S15326942DN2101_2. [DOI] [PubMed] [Google Scholar]
- 49.Carlson SM. Social origins of executive function development. In: Lewis C, Carpendale JM, editors. New Dir Child Adolesc Dev. Vol. 123. 2009. pp. 87–98. [DOI] [PubMed] [Google Scholar]
- 50.Pisoni DB, Kronenberger WG, Roman AS, Geers AE. Measures of Digit Span and Verbal Rehearsal Speed in Deaf Children After More Than 10 Years of Cochlear Implantation. Ear Hear Suppl. 2011;32:60S–74S. doi: 10.1097/AUD.0b013e3181ffd58e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Beer J, Pisoni DB, Kronenberger WG, Geers AE. New research findings: Executive functions of adolescents who use cochlear implants. ASHA Leader. 2010 Dec 21; [PMC free article] [PubMed] [Google Scholar]
- 52.Vygotsky L. Mind and Society. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- 53.Hughes CH, Ensor RA. How do families help or hinder the emergence of early executive function? In: Lewis C, Carpendale JM, editors. New Dir Child Adolesc Dev 2009. Vol. 123. 2009. pp. 35–50. [DOI] [PubMed] [Google Scholar]