Abstract
Background
The goal of this study was to extend our previous findings of abnormal prefrontal function in methamphetamine (MA) abusers and controls and to link the imaging data to behavioral, demographic and drug use variables.
Methods
We employed a fast-event related fMRI design to examine trial to trial reaction time (RT) adjustments in 30 MA abusers and 30 controls. A variant of the Stroop task was employed to measure influence of response conflict on RT, including the level of trial-to-trial RT adjustments seen after conflict trials.
Results
Compared to control subjects, MA abusers exhibited reduced RT adjustments and reduced activation in the prefrontal cortex (PFC) after conflict trials. RT adjustment correlated negatively with PFC brain activity in the MA group, while a trend for a positive correlation was observed in controls. No correlations were observed between task performance or brain activity and age, education or drug use variables.
Conclusions
These data support our previous findings that the ability to adapt a behavioral response based on prior experience is compromised in MA abusers. Interestingly, these impairments do not appear to be linked to drug use patterns or to educational levels.
Keywords: Methamphetamine, prefrontal, cognitive control, fMRI, imaging
1. Introduction
Worldwide use of methamphetamine (MA) is now estimated to be at 51 million users (Degenhardt et al., 2008; Roehr, 2005; United, 2008, 2009), with global abuse of amph/methamphetamines now surpassing that of cocaine and opiates combined (United, 2009). Approximately 5% of the adult population in the United States has used MA on at least one occasion and Emergency Department admissions related to MA use have doubled during the period of 1994 to 2002 (SAMSHA, 2004). Numerous imaging studies suggest that frontocingulate regions of the brain are affected by MA abuse (Ernst et al., 2000; London et al., 2004; Nordahl et al., 2005; Salo et al., 2007; Volkow et al., 2001). Consistent with abnormalities in brain structure and function, cognitive impairments have also been observed in MA abusers on tasks that require the suppression of task irrelevant information (Monterosso et al., 2005; Salo et al., 2007), decision-making (Kalechstein et al., 2003; Paulus et al., 2003), working memory (McKetin and Mattick, 1998) and cognitive control (Nestor et al., 2011; Salo et al., 2009a). Neurobiological models of addiction propose that ventral brain regions (i.e., orbital frontal cortex and nucleus accumbens) contribute to the impulse to seek drugs, whereas the recruitment of fronto-cingulate regions may be critical to control those prepotent impulses (i.e., cognitive control) (Jentsch and Taylor, 1999). In the context of addiction, cognitive control can be interpreted as the inhibition of a prepotent response (e.g., habitual drug use) in order to carry out behaviors associated with long-term rewards and positive outcomes (e.g., abstaining from drug use).
1.1 Study Rationale
The goal of the current study was to replicate and extend our preliminary findings that examined cortical mechanisms of cognitive control in a small group of MA abusers (Salo et al., 2009b). In the current study we increased our sample significantly in order to examine correlations between brain activity and behavior. In order to examine the neural substrates of cognitive control relevant to addiction, we conducted a fast-event related fMRI study in which we examined trial to trial RT adjustments using a variant of the single-trial Stroop task in 30 chronic MA abusers and 30 controls. This version of the Stroop task (Kerns et al., 2004) creates conditions in which performance (RT and accuracy) reflects the ability to recognize and resolve conflict at the time of response selection (i.e., within a trial), as well as the ability to flexibly adapt behavior, such as using exposure to conflict situations to change subsequent behavior (i.e., trial-to-trial adjustments after conflict trials). Many lines of research have shown that the information-processing system can adjust its strategy on a trial-to-trial basis and that the utilization of such a plan of action may be coupled with the subjective view that a particular strategy will produce a positive outcome (Gratton et al., 1992). Given that one of the hallmark behaviors associated with addiction is the failure to choose adaptive strategies to achieve future positive outcomes, this paradigm is well suited to examine the role of cognitive control in MA dependence. We hypothesized that in this increased sample of MA abusers we would observe correlations between abnormal patterns of trial to trial reaction time (RT) adjustments (i.e., conflict adaptation) and reduced PFC activity. Given the recent claim that many cognitive studies in MA abuse are confounded by group differences in age and education, we also wanted to test these relationships directly.
2. Materials and Methods
2.1. Subjects
Two groups were studied: 30 MA abusing subjects and 30 age-matched non-substance abusing control subjects. Data from 12 MA subjects and 16 controls were reported in our previous preliminary findings (Salo et al., 2009b). The MA abusers met DSM-IV criteria for lifetime MA dependence determined from the Structured Clinical Interview (SCID) (Spitzer et al., 1992) but were currently drug abstinent a minimum of 3 weeks. See Table 1 for demographic and drug use characteristics.
Table 1.
Demographic and clinical characteristics of 30 methamphetamine (MA) abusers and 30 control subjects.
| Methamphetamine Abusers (n =30 ) | Control Subjects (n = 30) | |
|---|---|---|
| Demographic Variables | ||
| Age, y, mean (SD) | 35.5 (7.9) † | 29.0 (7.7) |
| Range | 21 to 48 years | 20 to 48 years |
| Females | 15 | 13 |
| Subject’s education, y, mean | 12.5 (1.6) † | 15.2 (1.3) |
| Parental education, y, mean (SEM) | 13.2 (2.3) | 14.3 (2.5 ) |
| NART | 108.2 (5.0) † | 111.6 (4.7 ) |
| Clinical Variables | ||
| Methamphetamine use | -- | |
| Duration, y, mean (SD) | 14.0 (6.4) | -- |
| Range | 4 to 28 years | |
| Months Abstinent, mean (SD) | 13.7 (15.4) | -- |
| Range | 2 to 60 months | |
| Age of 1st MA use, y, mean (SD) | 17.7 (4.4) | -- |
| Mean daily MA dosage (grams) | 1.3 (0.85) | -- |
| History of Cannabis Abuse | 24 | -- |
| Age of 1st Cannabis Use. Y, mean | 15.0 (3.8) | |
Significantly different from control group.
2.2. Procedure
A single-trial Stroop task was administered during the scanning session that employed both Incongruent (conflict) and Congruent (non-conflict) trials (see Supplemental Material for detailed task description). Behavioral analyses contrasted the groups on RT Stroop conflict effect (Conflict minus non-conflict), mean error rates and the level of trial-to-trial adjustments seen after conflict trials. Analysis of variance procedures (ANOVA) for repeated measures were used to analyze the data in a 2 × 2 mixed ANOVA with group as a between subjects factor (patients vs controls) and word type (incongruent vs congruent) as within subjects variables. Incorrect responses were not included within the analysis of variance for RT. Analyses were carried out to examine trial to trial adjustments to conflict-conflict (iI) compared to non-conflict-conflict (cI) sequences. Accuracy data were analyzed using the same design.
2.2.1. Imaging
Functional MRI data were collected on a 3T Siemens Trio Total imaging matrix (Tim) MRI System (Erlangen, Germany: see Supplemental Material for scanning parameters and image preprocessing details). Analyses were performed using a General Linear Model (GLM) as implemented in SPM5. In a first-level analysis, individual subject GLMs were fitted to each subject’s functional data. The statistical models included regressors coding for 7 covariates (cC, iC, iI, cI, Errors, Post-Errors and Non-Responses). Parameter estimates obtained from this first level analysis were used to compute maps of the contrasts of interest for effects of conflict and trial-to-trial effects (I-C for RT conflict, and iI-cI for trial to trial RT adjustments). Maps of the contrasts of interest for effects of error conflict were also computed. Hypotheses put forth within this proposal regarding activity in specific regions of interest (ROIs) including anterior cingulate cortex (ACC) and PFC were tested in a second level random-effects analysis of these contrast maps. The volume of search was restricted to areas for which we had specific hypotheses by using an explicit mask of lateral and medial prefrontal cortical areas. The mask used was the same as employed in our 2009 study and was built using the AAL atlas in the SPM5 toolbox (see supplemental material for details). Clusters of active voxels reported were corrected for multiple comparisons at a set level of p < 0.05 (Friston et al., 1996).
3. Results
3.1. Behavioral data
3.1.1. Reaction time analyses
Analyses revealed main effects of Stroop word type [F (1,58) = 157.49, p< .0001] and trial to trial adjustments [F (1,58 ) = 14.58, p< .0001]. Planned analyses also revealed that the trial to trial adjustment RT effect (cI-iI) differed significantly between the MA abusers and controls [F (1,58 ) = 4.37 ; p < .05]). While the controls showed an RT advantage (26 msec benefit) to conflict trials that were preceded by conflict trials (iI) the MA abusers showed no advantage and were actually slower (4 msec cost). These group differences in Stroop endured with age, education, NART scores as covariates. Correlational analyses revealed no relationship between education levels and trial to trial adjustments in the MA abusers [r = .11; p =.57] or the controls [r = .15; p = .44]. No correlations were observed between measures of age and premorbid IQ (i.e., NART scores) and trial to trial adjustments in either group. Similar to our previous published findings, no group differences were observed on within-trial Stroop conflict effects (F < 1).
3.1.2. Error analyses
Analyses revealed a main effect of word type [F (1,58) = 36.13, p =. 0001] with both groups making significantly more errors in the incongruent condition (6%) than in the congruent condition (3%). There were no group differences in incongruent [F(1,58) = 2.28; p = .13] or congruent errors [F(1,58) = 1.5 ; p = .22]. There was no evidence of a speed-accuracy trade-off for both groups (MA abusers; r=.293; p =.10, controls: r=.096; p =.61].
3.2. Imaging results
We first examined whether activity within the ACC and PFC was associated with within-trial conflict monitoring (I-C) and trial-to-trial adjustments (iI-cI). Using ANOVA procedures with subject as a random variable, significant activation to conflict contrasts (I-C) was observed in the ACC in both groups with no differences observed between groups. In contrast, when we examined the pattern of activation for the trial to trial RT adjustments we found that controls exhibited increased PFC activity on iI sequences compared to the cI sequences. In contrast the MA abusers showed little or no activation within the PFC region (See Figure 1). We then ran a second-level random-effects analysis to explore group differences across the contrasts of interest. Between group differences emerged in activation in the prefrontal regions centered in right and left Brodmann areas 6 and 8 (p =.001, corrected) (Friston et al., 1996). (See figure 2). These regions showed lower levels of activation in the MA abusers after iI trial sequences relative to cI trial sequences. Table 3 summarizes the data for frontal regions with significantly different activation between the MA abusers and controls.
Figure 1.
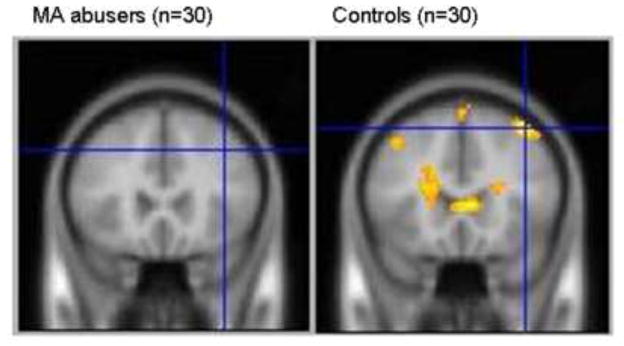
Regions of Increased Activation Associated with Trial to Trial Adjustments (iI– cI) in Methamphetamine Abusers and Controls
Figure 2.
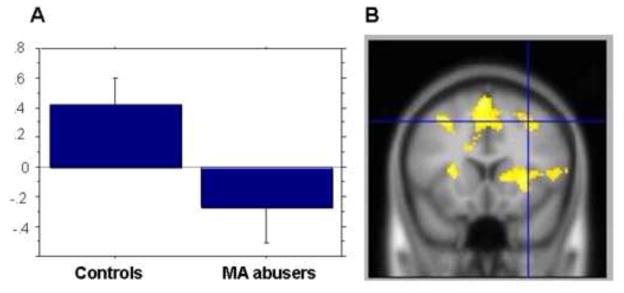
DLPFC region showing increased activity related to trial to trial adjustments (iI-cI) in control subjects relative to methamphetamine (MA) abusers. 2a) Graph of the average coefficients for the iI-cI statistical contrast in the two groups, averaged within group for the voxels of the DLPFC activation showed in panel 2a.
Table 3.
Brain regions with significant group differences associated with trial to trial adjustments in 30 methamphetamine (MA) abusers and 30 control subjects.
| MNI Coordinates
|
|||||
|---|---|---|---|---|---|
| Region | Brodmann’s Area | No. Voxels | x | y | z |
| Right Frontal Gyrus | 8 | 28 | 32 | 16 | 46 |
| Right Superior Frontal | 6 | 21 | 26 | 12 | 52 |
| Right Mid Frontal Gyrus | 6 | 40 | 18 | −12 | 76 |
| Right Cingulate Gyrus | 32 | 14 | 8 | 16 | 44 |
| Right Cingulate Gyrus | 24 | 28 | 14 | −24 | 46 |
| Left Frontal Gyrus | 8 | 69 | −32 | 16 | 46 |
| Left Superior Frontal | 6 | 28 | −14 | −6 | 72 |
| Left Mid Frontal Gyrus | -- | 26 | −36 | 44 | −14 |
| Left Cingulate Gyrus | -- | 11 | −14 | −42 | 48 |
3.3. Correlations
In this expanded dataset significant negative correlations were observed between the PFC beta coefficients and the corresponding behavioral data for the trial to trial adjustments in the MA abusers [r=−.375, p < .05]. A trend significant positive correlation was also observed in the controls [r=−.33, p =.07). A direct statistical analysis of correlation coefficients between groups reached significance (p = .003). These results suggest that while the MA group failed to activate the PFC in order to sustain adaptive trial to trial RT adjustments, the controls exhibited increased PFC activation in response to trial to trial RT adjustments. Give the physiological interaction between medial and lateral frontal cortices and striatum in mediating cognitive control, we wanted to examine the specificity of brain behavior relationship within the PFC (Frank et al., 2005; Pasupathy and Miller, 2005). In order to do this we conducted correlations within a striatal cluster that showed activation during trial to trial adjustments within both MA abusers and controls, but did not differ between groups. In this correlational analysis, no significant correlations emerged in the MA abusers (r=.15; p = .44) or the controls (r = .12; p = .54).
4. Discussion
This study replicates and extends our previously published finding of reduced PFC activation in MA abusers compared to non-substance abusing controls when contrasting conditions that measure how prior exposure to conflict modulated subsequent behavior. In this new dataset we also observed differences in more anterior brain regions including bilateral BA8 and BA10. Significant correlations were also observed between trial to trial behavioral RTs and activity within the PFC of the MA abusers, providing further support to the hypothesis that a PFC dysfunction underlies the deficit in conflict adaptation of MA abusers. Similar analyses within striatal regions failed to reach significance in either group, suggesting a degree of specificity of the PFC dysfunction relative to trial-to-trial behavioral regulation. Given that frontally-mediated behavioral regulation assists with maintenance of goal-directed behavior, it is not surprising that the pattern of deficits in the MA abusers involve reduced activation in frontal regions.
This new dataset also provides statistical evidence that years of education and premorbid IQ are not related to the deficits observed in the current study. These relationships were tested directly with robust statistical methods and none were found to exist. As our subjects were MA abstinent at the time of study, we are unable to examine the acute effects of MA abuse nor can the findings rule out pre-existing vulnerabilities that could have predated the MA abuse. The failure to detect group difference in within-trial conflict effects may be due in part to gender effects. Post-Hoc analyses suggested that male and female MA abusers may process conflict information differently, and we are currently examining this relationship further. Furthermore, future studies that include at- risk populations are needed to determine how deficits in conflict adaptation and behavioral control may contribute to the development and sustainment of addictive behaviors.
4.1. Limitations
One limitation of this study is that our subject groups were not matched on nicotine and cannabis use patterns. As published studies have shown that abrupt cessation from smoking tobacco can impact performance on the Stroop task, future studies should consider time since last cigarette consumed as an experimental variable (Azizian et al., 2010; Domier et al., 2007). However, in this current study none of our subjects reported that they had recently stopped smoking tobacco prior to the time of study. In order to minimize any effects of cannabis use, exclusion criteria required that none of the subjects met criteria for cannabis dependence. In addition no subjects reported smoking cannabis in the past month and none tested positive for cannabis on the toxicology screens.
4.2. Conclusion
It cannot be disputed that MA abuse is a public health issue of vast proportions (Nations, 2004). This worldwide epidemic brings with it collateral health issues, including MA-induced cardiovascular disease (Treweek et al., 2007; Wijetunga et al., 2004), increased rates of HIV infection (Colfax and Shoptaw, 2005; Huff, 2006; Jones, 2005), and prominent psychiatric symptoms (Chen et al., 2005; Chen et al., 2003; Iyo et al., 2004; McKetin et al., 2006; Sato et al., 1992; Srisurapanont et al., 2003). The highly addictive nature of MA, and its profound negative impact on society makes this drug a major public health concern in the 21st century (United, 2009). Increased knowledge of how alterations in brain function following extended periods of MA abuse impact behavior have the potential to inform treatment interventions and contribute to the field of addiction research.
Supplementary Material
Table 2.
Behavioral results from 30 methamphetamine (MA) abusers and 30 control subjects.
| Methamphetamine Abusers (n =30) | Control Subjects (n = 30) | |
|---|---|---|
| Within-Trial Stroop Effects, median (SD)s (msec) | ||
| Incongruent | 767.6 (140.7) | 752.5 (156.9) |
| Congruent | 629.4 (80.1) | 626.7 (118.8) |
| Stroop Conflict Effect | 138.2 | 125.8 |
| Conflict Errors | .05 (.04) | .07 (.07) |
| Non Conflict Errors | .02 (.02) | .03 (.05) |
| Trial to Trial RT adjustments median (SD)s (msec) | ||
| Congruent-Incongruent (cI) | 765.5 (140.2) | 765.4 (167.2) |
| Incongruent-Incongruent (iI) | 769.7 (147.1) | 739.7 (150.2) |
| Trial to Trial Adjustment (cI-iI) | − 4.2† | 25.8 |
Significantly different from control group.
Acknowledgments
We would like to thank Jerry Sonico for his support and technical assistance with MR data collection.
Footnotes
Disclosure/Conflict of Interest
The authors declare that this work was funded by NIDA grant DA021847 to RS. There are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Azizian A, Nestor LJ, Payer D, Monterosso JR, Brody AL, London ED. Smoking reduces conflict related anterior cingulate activity in abstinent cigarette smokers performing a Stroop task. Neuropsychopharmacology. 2010;35:775–782. doi: 10.1038/npp.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CK, Lin SK, Sham PC, Ball D, Loh el W, Murray RM. Morbid risk for psychiatric disorder among the relatives of methamphetamine users with and without psychosis. Am J Med Genet B Neuropsychiatr Genet. 2005;136:87–91. doi: 10.1002/ajmg.b.30187. [DOI] [PubMed] [Google Scholar]
- Chen CK, Lin SK, Sham PC, Ball D, Loh EW, Hsiao CC, Chiang YL, Ree SC, Lee CH, Murray RM. Pre morbid characteristics and co morbidity of methamphetamine users with and without psychosis. Psychological medicine. 2003;33:1407–1414. doi: 10.1017/s0033291703008353. [DOI] [PubMed] [Google Scholar]
- Colfax G, Shoptaw S. The methamphetamine epidemic: implications for HIV prevention and treatment. Current HIV/AIDS reports. 2005;2:194–199. doi: 10.1007/s11904-005-0016-4. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Baker A, Maher L. Methamphetamine: geographic areas and populations at risk, and emerging evidence for effective interventions. Drug and alcohol review. 2008;27:217–219. doi: 10.1080/09595230801956538. [DOI] [PubMed] [Google Scholar]
- Domier CP, Monterosso JR, Brody AL, Simon SL, Mendrek A, Olmstead R, Jarvik ME, Cohen MS, London ED. Effects of cigarette smoking and abstinence on Stroop task performance. Psychopharmacology. 2007;195:1–9. doi: 10.1007/s00213-007-0869-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst T, Chang L, Leonido Yee M, Speck O. Evidence for long term neurotoxicity associated with methamphetamine abuse: A 1H MRS study. Neurology. 2000;54:1344–1349. doi: 10.1212/wnl.54.6.1344. [DOI] [PubMed] [Google Scholar]
- Frank MJ, Woroch BS, Curran T. Error related negativity predicts reinforcement learning and conflict biases. Neuron. 2005;47:495–501. doi: 10.1016/j.neuron.2005.06.020. [DOI] [PubMed] [Google Scholar]
- Friston KJ, Holmes A, Poline JB, Price CJ, Frith CD. Detecting activations in PET and fMRI: levels of inference and power. NeuroImage. 1996;4:223–235. doi: 10.1006/nimg.1996.0074. [DOI] [PubMed] [Google Scholar]
- Gratton G, Coles MG, Donchin E. Optimizing the use of information: strategic control of activation of responses. J Exp Psychol Gen. 1992;121:480–506. doi: 10.1037//0096-3445.121.4.480. [DOI] [PubMed] [Google Scholar]
- Huff B. Methamphetamine and HIV. Beta. 2006;18:42–47. [PubMed] [Google Scholar]
- Iyo M, Sekine Y, Mori N. Neuromechanism of developing methamphetamine psychosis: a neuroimaging study. Annals of the New York Academy of Sciences. 2004;1025:288–295. doi: 10.1196/annals.1316.036. [DOI] [PubMed] [Google Scholar]
- Jentsch JD, Taylor JR. Impulsivity resulting from frontostriatal dysfunction in drug abuse: implications for the control of behavior by reward related stimuli. Psychopharmacology. 1999;146:373–390. doi: 10.1007/pl00005483. [DOI] [PubMed] [Google Scholar]
- Jones K. Methamphetamine, the brain, HIV, and mental health. Focus (San Francisco, Calif. 2005;20:1–5. [PubMed] [Google Scholar]
- Kalechstein AD, Newton TF, Green M. Methamphetamine dependence is associated with neurocognitive impairment in the initial phases of abstinence. The Journal of neuropsychiatry and clinical neurosciences. 2003;15:215–220. doi: 10.1176/jnp.15.2.215. [DOI] [PubMed] [Google Scholar]
- Kerns JG, Cohen JD, MacDonald AW, Cho RY, Stenger VA, Carter CS. Anterior cingulate conflict monitoring and adjustments in control. Science. 2004;303:1023–1026. doi: 10.1126/science.1089910. [DOI] [PubMed] [Google Scholar]
- London ED, Simon SL, Berman SM, Mandelkern MA, Lichtman AM, Bramen J, Shinn AK, Miotto K, Learn J, Dong Y, Matochik JA, Kurian V, Newton T, Woods R, Rawson R, Ling W. Mood disturbances and regional cerebral metabolic abnormalities in recently abstinent methamphetamine abusers. Archives of general psychiatry. 2004;61:73–84. doi: 10.1001/archpsyc.61.1.73. [DOI] [PubMed] [Google Scholar]
- McKetin R, Mattick RP. Attention and memory in illicit amphetamine users: comparison with non drug using controls. Drug and alcohol dependence. 1998;50:181–184. doi: 10.1016/s0376-8716(98)00022-2. [DOI] [PubMed] [Google Scholar]
- McKetin R, McLaren J, Lubman DI, Hides L. The prevalence of psychotic symptoms among methamphetamine users. Addiction (Abingdon, England) 2006;101:1473–1478. doi: 10.1111/j.1360-0443.2006.01496.x. [DOI] [PubMed] [Google Scholar]
- Monterosso JR, Aron AR, Cordova X, Xu J, London ED. Deficits in response inhibition associated with chronic methamphetamine abuse. Drug and alcohol dependence. 2005;79:273–277. doi: 10.1016/j.drugalcdep.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Nations U. Crime, U.N.O.o.D.a. 2004 World Drug Report. Vol. 1. United Nations; Vienna: 2004. The world drug problem: A status report; pp. 25–26. [Google Scholar]
- Nestor LJ, Ghahremani DG, Monterosso J, London ED. Prefrontal hypoactivation during cognitive control in early abstinent methamphetamine dependent subjects. Psychiatry research. 2011;194:287–295. doi: 10.1016/j.pscychresns.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordahl TE, Salo R, Natsuaki Y, Galloway GP, Waters C, Moore CD, Kile S, Buonocore MH. Methamphetamine users in sustained abstinence: a proton magnetic resonance spectroscopy study. Archives of general psychiatry. 2005;62:444–452. doi: 10.1001/archpsyc.62.4.444. [DOI] [PubMed] [Google Scholar]
- Pasupathy A, Miller EK. Different time courses of learning related activity in the prefrontal cortex and striatum. Nature. 2005;433:873–876. doi: 10.1038/nature03287. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Hozack N, Frank L, Brown GG, Schuckit MA. Decision making by methamphetamine dependent subjects is associated with error rate independent decrease in prefrontal and parietal activation. Biological psychiatry. 2003;53:65–74. doi: 10.1016/s0006-3223(02)01442-7. [DOI] [PubMed] [Google Scholar]
- Roehr B. Half a million Americans use methamphetamine every week. BMJ (Clinical research ed. 2005:476. doi: 10.1136/bmj.331.7515.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salo R, Nordahl TE, Buonocore MH, Natsuaki Y, Waters C, Moore CD, Galloway GP, Leamon MH. Cognitive control and white matter callosal microstructure in methamphetamine dependent subjects: a diffusion tensor imaging study. Biological psychiatry. 2009a;65:122–128. doi: 10.1016/j.biopsych.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salo R, Nordahl TE, Natsuaki Y, Leamon MH, Galloway GP, Waters C, Moore CD, Buonocore MH. Attentional control and brain metabolite levels in methamphetamine abusers. Biological psychiatry. 2007;61:1272–1280. doi: 10.1016/j.biopsych.2006.07.031. [DOI] [PubMed] [Google Scholar]
- Salo R, Ursu S, Buonocore MH, Leamon MH, Carter C. Impaired prefrontal cortical function and disrupted adaptive cognitive control in methamphetamine abusers: a functional magnetic resonance imaging study. Biological psychiatry. 2009b;65:706–709. doi: 10.1016/j.biopsych.2008.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMSHA; Administration, S.S.A.a.M.H.S. The DASIS report: primary methamphetamine/amphetamine treatment admissions: 1992 2002. Office of Applied Studies; 2004. [Google Scholar]
- Sato M, Numachi Y, Hamamura T. Relapse of paranoid psychotic state in methamphetamine model of schizophrenia. Schizophrenia bulletin. 1992;18:115–122. doi: 10.1093/schbul/18.1.115. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM III R (SCID). I: History, rationale, and description. Archives of general psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Srisurapanont M, Ali R, Marsden J, Sunga A, Wada K, Monteiro M. Psychotic symptoms in methamphetamine psychotic in patients. Int J Neuropsychopharmacol. 2003;6:347–352. doi: 10.1017/S1461145703003675. [DOI] [PubMed] [Google Scholar]
- Treweek J, Wee S, Koob GF, Dickerson TJ, Janda KD. Self vaccination by methamphetamine glycation products chemically links chronic drug abuse and cardiovascular disease. Proceedings of the National Academy of Sciences of the United States of America. 2007;104:11580–11584. doi: 10.1073/pnas.0701328104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United N. Crime, U.N.O.o.D.a. Global ATS Assessment. United Nations; Vienna: 2008. Amphetamines and Ecstasy 2008. [Google Scholar]
- United N. Crime, U.N.O.o.D.a. World Drug Report 2009. United Nations; Vienna: 2009. The world drug problem: A status report. [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Ding YS, Sedler M, Logan J, Franceschi D, Gatley J, Hitzemann R, Gifford A, Wong C, Pappas N. Low level of brain dopamine D2 receptors in methamphetamine abusers: association with metabolism in the orbitofrontal cortex. The American journal of psychiatry. 2001;158:2015–2021. doi: 10.1176/appi.ajp.158.12.2015. [DOI] [PubMed] [Google Scholar]
- Wijetunga M, Bhan R, Lindsay J, Karch S. Acute coronary syndrome and crystal methamphetamine use: a case series. Hawaii medical journal. 2004;63:8–13. 25. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


