Abstract
Background
Physical activity is critical for the management of knee osteoarthritis, and the spouse may play a role in encouraging or discouraging physical activity.
Purpose
To examine four types of spousal influence—spouses' daily activity, autonomy support, pressure, and persuasion--on the daily physical activity of adults living with knee osteoarthritis.
Methods
A total of 141 couples reported their daily experiences for 22 days using a handheld computer, and wore an accelerometer to measure moderate activity and steps.
Results
Spouses' autonomy support for patient physical activity, as well as their own level of activity, was concurrently associated with patients' greater daily moderate activity and steps. In addition, on days when male patients perceived that spouses exerted more pressure to be active, they spent less time in moderate activity.
Conclusions
Couple-oriented interventions for knee osteoarthritis should target physical activity in both partners and spousal strategies for helping patients stay active.
Keywords: couples, physical activity, daily diary, arthritis, autonomy support, social control
Lack of physical activity influences the course and symptoms of many chronic health conditions, including knee osteoarthritis, whereas increased physical activity can aid in the management of these conditions (1). It has been known for some time that family relationships have an impact on activity and exercise behavior (2,3). However, the specific ways in which family members negatively or positively influence patients' daily level of physical activity are unknown. In the present study we examined how spouses' autonomy support and social control (persuasion and pressure), as well as their own level of activity, are associated with the daily physical activity of adults living with knee osteoarthritis. We also examined gender differences in daily spousal influence on patient physical activity.
Osteoarthritis is the most prevalent form of arthritis in the United States and causes significant activity limitations, resulting in billions of dollars of medical care expenditures and lost earnings (4). Due in part to trends in obesity, nearly half of adults are projected to develop symptomatic osteoarthritis in one or both knees during their lifetime (5). Because physical activity strengthens the muscles that support joints and facilitates weight loss, staying active is one of the most effective long-term strategies for managing knee osteoarthritis (6,7). Two indicators of daily physical activity are especially important for health: amount of time spent in moderate-intensity activity, and daily steps taken. The Surgeon General recommends that adults of all ages, including those with arthritis, accumulate at least 30 minutes of moderate-intensity physical activity on most days of the week (8,9). Meeting the recommended level of physical activity has been shown to enhance older adults' long-term physical function (10,11). Moreover, a greater number of steps per day is associated with improved blood pressure and metabolic control (12,13).
Theoretical Basis for Spousal Influence on Behavior
The marital relationship is a significant one for many adults living with arthritis, in that both supportive and insensitive responses from the spouse are associated with patients' emotional well-being and pain expression (14–16). An important yet unexplored question is the extent to which spousal communications also influence patients' level of physical activity. Contemporary models of social influence on health behavior may be usefully applied here. First, research originating from Self-Determination Theory suggests that spouses may have a positive impact on patient activity by providing autonomy support for this behavior (17,18). Autonomy support is defined as actions that are characterized by empathy and understanding for an individual's situation and the provision of choices for making health behavior changes. Individuals whose family members or health care providers show autonomy support for health behavior changes are more likely to make those changes for reasons that come from within themselves and are freely chosen (19,20). Such individuals have been shown to be more successful at smoking cessation (21), diabetes management (22), and exercise (23,24). This program of research suggests that the benefits of autonomy support may extend to knee osteoarthritis patients, to the extent that their spouse fosters choices and independence in decisions regarding physical activity.
Another interpersonal process that may affect level of physical activity is health-related social control, which refers to an individual's attempts to regulate or influence the behaviors of another person. The concept of social control and its effect on health behaviors emerged from social control theories which posit that social relationships such as marriage serve to regulate partners' behavior through explicit requests or demands (25–27). Among married individuals, the spouse is the most frequently named source of social control (28,29). Recent work has focused on distinguishing the effects of positive social control from those of negative social control. In contrast to autonomy support's encouragement of independent action, positive control strategies refer to one person's attempts to persuade another to make improvements in his or her health behaviors. Negative control strategies involve one person's attempts to pressure or coerce another to make improvements (30).
Positive control strategies have been associated with improvement in HIV self-care (31), adherence to postsurgical medical recommendations after total knee replacement surgery (e.g., physical therapy exercises and physical activity [30], and more exercise [32]). Although negative control has sometimes been associated with improvement in health behaviors (30), it is most often associated with undesirable behavior change, ignoring requests for behavior change, and hiding unhealthy behaviors (33–35). Recent studies have linked negative control with poorer dietary adherence, specifically (34,36). These findings suggest that daily physical activity may also be associated with positive and negative social control strategies of the spouse.
The distinction between positive and negative control largely mirrors the two forms of social control examined in this study—persuasion and pressure. We favor the latter terms because they are more neutral with respect to the direction of effects on patients' behavior. We prefer the term persuasion over the term positive control as it avoids possible confusion between the nature of the influence attempt and its presumed impact. For that same reason, we prefer the term pressure over the term negative control.
There are good reasons to believe that knee osteoarthritis patients' level of physical activity is responsive not just to what spouses say but also to what they do. Specifically, spouses' own level of day-to-day physical activity is likely to be positively associated with patient activity level (37). Older adults who report that their family members make time to be physically active are more active themselves (38), and highly active individuals are almost three times as likely to have a similarly active spouse (39). Determining the extent to which spouses' influence stems from their own activity level, communications regarding physical activity, or both would suggest clear avenues for couple-oriented interventions with this patient population (40).
Current Study
The purpose of the current study was to examine these four types of daily spousal influence on patients' physical activity. We predicted that more autonomy support, persuasion control, and spouse activity on a given day, as well as less pressure control, would be associated with greater patient physical activity on that day (i.e., time spent in moderate-intensity activity, and number of steps taken). We used data collected over a 22-day period with handheld computers and accelerometers to examine within-couple associations between spousal influence and patient physical activity. To provide the strongest test of our hypotheses, we examined daily spousal influence independent of the general quality of marital interactions that day (i.e., tension and enjoyment) as well as common correlates of physical activity (i.e., age, physical comorbidity, and daily pain).
We also examined the moderating role of patient gender in spousal influence. Specifically, we predicted gender differences in the effects of spouse social control. According to gender-role theory, men are more likely than women to be characterized by agency and a focus on instrumentality and separation or individuation from others (41,42). By extension, male patients may react more strongly than female patients to coercive strategies aimed at changing their behavior (to become more active) when they would prefer to make their own decisions in this domain. In accordance with gender-role theory we predicted that spouse pressure would be more detrimental, and spouse persuasion would be more beneficial, for the physical activity of male patients than female patients.
Self-Determination Theory does not posit gender differences in the need for, or effects of, autonomy support. In addition, previous research is not highly instructive regarding a potential gender difference in the effect of spouse activity level on patient activity level. That is, research on new relationships indicates that women's health behaviors are more affected by men's health behaviors than vice versa (43), but it is not clear whether gender would play a similar role in long-term relationships. Thus, we explored whether gender would moderate the effects of spouse autonomy support and activity level but we offer no specific prediction for the direction of these effects.
Method
Study Design
Data presented in this report are from a larger study of couples and knee osteoarthritis that combined in-person interviews conducted over an 18-month period (i.e., T1, T2 at a 6 month follow-up, and T3 at an 18 month follow-up) with a 22-day assessment of daily experiences immediately after the T1 interview. During the daily assessment protocol, patients and spouses used a handheld computer to answer questions regarding health and affect 3 times per day (i.e., beginning-of-day, afternoon, and end-of-day), and questions regarding marital interactions at end-of-day. Each patient and spouse also wore an accelerometer in order to provide objective data on daily physical activity during the 22-day period. The current report utilizes data from the T1 interviews, end-of-day diary assessments, and accelerometers.
Participants
To be eligible for the study, patients had to be diagnosed with knee osteoarthritis by a physician, experience usual knee pain of moderate or greater intensity, be at least 50 years of age, and be married or in a long-term relationship (self-defined) in which they shared a residence with their partner. Exclusion criteria were a comorbid diagnosis of fibromyalgia or rheumatoid arthritis, use of a wheelchair to get around, and a plan to have hip or knee surgery within the following six months. Couples were excluded from the study if the spouse had arthritis pain of moderate or greater intensity, used a wheelchair to get around, or required assistance with personal care activities. Both partners had to be cognitively functional as indicated by the accuracy of their answers to questions regarding the current date, day of the week, their age, and birthdate. Both partners also had to be free of any major hearing, speech, or language problems that would interfere with the comprehension and completion of data collection conducted in English.
Primary sources of recruitment were research registries for rheumatology clinic patients and older adults interested in research; flyers distributed to University of Pittsburgh staff and faculty, and word of mouth. A total of 606 couples were screened for eligibility. Of these, 221 couples declined to participate, and the most frequent reasons were lack of interest (N = 87) or illness in the family (N = 55). A total of 233 couples were not eligible, and the most frequent reasons were lack of osteoarthritis in the knee (N = 55) or knee osteoarthritis pain that was mild (N = 47). The total enrolled sample comprised 152 couples (i.e., 304 individuals) which included 3 same-sex couples. A total of 145 couples completed the diary assessment component of the study, and 141 of these couples provided sufficient activity data for our analyses (see Data Collection Procedures). Table 1 provides background information for patients and their spouses.
Table 1.
Demographic Characteristics of Patients and Spouses (N = 141)
| Variable | Patients M (SD) or % | Spouses M (SD) or % |
|---|---|---|
| Age | 65.4 (9.8) | 65.1 (11.5) |
| Gender = male | 43% | 58% |
| Years of education | 16.0 (2.0) | 15.9 (2.1) |
| Race = Caucasian | 87% | 86% |
| Years married/in relationship | 34.0 (16.7) | |
| Household income | $40,000–59,000 | |
| Employed | 43% | 47% |
| Body mass index | 31.4 (5.8) | 28.8 (4.7) |
| Duration of knee OA (years) | 12.7 (11.3) |
Note.
OA = osteoarthritis
Data Collection Procedures
Trained staff interviewed patients and spouses independently in their home. Following these interviews, couples were trained in use of the handheld computer (i.e., the Palm TX) as well as the format and content of the diary questions. The handheld computer and questionnaire were designed for easy use by older adults and people with minimal computer experience; accessible features included large font size and an oversized stylus for registering responses. Each patient and spouse was provided with a handheld computer that was clearly labeled with his or her name, and the importance of completing diary assessments independently was emphasized.
Our goal was to capture participants' experiences within the general time frames of morning, afternoon, and evening. Therefore, participants were instructed to answer questions: 1) within 60 minutes of rising in the morning (i.e., beginning-of-day), 2) between 2:00 and 4:00 p.m. (i.e., afternoon), and 3) upon retiring at night (i.e., end-of-day). Participants were instructed to place the accelerometer on the hip within 60 minutes of rising in the morning and to remove it at bedtime. Participants used a written log to record their daily rise time and bed time, as well as the time that they placed and removed the accelerometer. As stated above, the current report utilizes data from the T1 interviews, end-of-day diary assessments, and accelerometers.
Completion and compliance rates were examined for the diary data. Out of a potential 6380 end-of-day observations (290 individuals × 22 days), a total of 5863 were completed (92%). Compliance with the requested timing of the end-of-day assessment was evaluated by comparing the time of the handheld computer entries with participants' written log of daily bedtimes. End-of-day assessments that were completed more than 120 minutes before bedtime were excluded from analysis. Using this criterion, 5327 of the 5863 completed observations were included in analysis (i.e., 92% of the completed observations, or 83% of the total possible observations). Completion and compliance rates were virtually identical for patient and spouse.
As noted above, accelerometers were used to assess patients' and spouses' daytime physical activity during the 22-day diary assessment period. Accelerometers are motion-sensitive monitors that count the number of movements or steps taken per pre-specified time interval. Self-reports of physical activity are often overestimated (44), and thus accelerometers are considered the best way to objectively measure free-living physical activity (45,46). Participants wore the GT1M or GT3X model of the CSA/MTI tri-axial ActiGraph, with placement on the hip in order to best capture ambulatory activities (47). Data were collected in 1-minute epochs.
Participants were instructed to wear the monitor during the day and remove it at night; a reminder to put the monitor on in the morning was provided electronically via the handheld computers. Participants used a written log to record any periods during which they did not wear the accelerometer. All times when the monitor was not worn were removed from data analysis. Data were then screened for anomalous values (activity counts greater than 6000 at any given minute), which affected less than 1% of the activity data. Remaining data were coded to determine the total number of hours of wear time for use as a covariate in multilevel models.
A total of 4 couples did not have sufficient physical activity data due to less than 10 hours of wear time, a standard requirement in physical activity research (45), or due to accelerometer malfunction. The average number of days that the accelerometer was worn was 17.5 (SD = 4.0) for patients and 15.8 (SD = 4.8) for spouses. Average daily accelerometer wear time was 14.7 hours (SD = 1.1) for patients and 14.8 hours (SD = 1.2) for spouses.
Interview and Daily Diary Measures
Data on patient age, gender, education, employment status, and physical comorbidity were collected during the in-person interview. The physical comorbidity measure consists of 24 questions assessing current problems of different physiological systems (e.g., cardiovascular or cerebrovascular; musculoskeletal; respiratory; digestive, endocrine) and yields a count of 0 to 24 (M = 2.4; SD = 1.9; range = 0 – 10) (48). All other measures were collected daily and are described below.
A total of nine questions were developed for the current study to assess daily spouse autonomy support, persuasion, and pressure, with three questions intended to assess each type of spouse behavior. All items had a 3-point response option (1 = not at all, 2 = somewhat, 3 = very much). Items assessing autonomy support were taken from the Important Other Climate Questionnaire for diet and smoking (49) and modified for daily physical activity. Items assessing persuasion and pressure were derived from prior research on social control strategies (30,50).
To determine the within-person factor structure of this scale, we conducted a confirmatory factor analysis on the spouse support and control items. A three factor structure fit the data well (χ2 = 5.9, p = .99; CFI = 1.00; SRMR = .01) with 3 items loading on autonomy support, 2 items loading on pressure control, and 4 items loading on persuasion control. Items are described below.
Activity-related autonomy support
Patients reported the extent to which the spouse had provided autonomy support for physical activity that day. This scale is the average of three items (showed understanding for how physically active I wanted to be, respected my decisions or choices about physical activity, and listened to how I would like to do things with regard to being more or less physically active) (M = 2.09, SD = .51). The between-person reliability of this measure is .82. Averaging across the three items, autonomy support behaviors occurred on 76% of the days of the diary period (i.e., behaviors were endorsed by patients as having occurred somewhat or very much on a given day).
Activity-related persuasion
Patients reported the extent to which the spouse had tried to convince or motivate them to be physically active that day. This scale is the average of four items (tried to persuade me to be more physically active, encouraged me to be more physically active, let me know that my lack of physical activity worried him/her, and created a situation where I had to be physically active) (M = 1.19, SD = .27). The between-person reliability of this measure is .70. Averaging across the four items, persuasion control occurred on 17% of the days of the diary period.
Activity-related pressure
Patients reported the extent to which the spouse had tried to force or coerce them to be physically active that day. This scale is the average of two items (criticized, made fun of, or teased me for not being more physically active; and nagged me to be more physically active) (M = 1.05, SD = .15). The between-person reliability of this measure is .68. Averaging across the two items, pressure control occurred on 5% of the days of the diary period.
The within-patient correlations among spouse autonomy support, persuasion, and pressure ranged from r = .08 (p = .04) between autonomy support and persuasion, to r = .33 (p < .001) between pressure and persuasion. The within-person variability in these three behaviors ranged from 37% for persuasion to 50% for pressure.
Pain
Patients' reports of pain or tenderness at the end of day for 10 sets of joints (e.g., knees, hips, hands) were collected using the Rapid Assessment of Disease Activity in Rheumatology(51), in which separate ratings are made for multiple joints or joint groups on a scale from 0 to 3 (no pain/tenderness to severe pain/tenderness). The average level of pain was 5.99 (SD = 4.78; range = .11 – 29.63).
Marital tension and enjoyment
At the end of the day patients reported how tense and how enjoyable their interactions were with their spouse throughout the day, on a scale from 1 to 3 (not at all to very much)(52). Average tension was 1.22 (SD = .27; range = 1 – 2.26) and average enjoyment was 2.43 (SD = .45; range = 1.28 – 3.0).
Physical Activity Measures
Our dependent variables consisted of two indicators of patients' daily physical activity: number of minutes in moderate-intensity activity, and number of steps taken. Although these variables are highly correlated in the current study (i.e., within-patient correlation r = .77, p < .001), data on physical activity in older adults with knee osteoarthritis are rare and we believe that it is important to examine spousal influence on both indicators. Moderate activity and steps have each been linked with different health outcomes(11,13) and both describe physical activity in metrics that are readily understood and have real-world referents.
Intensity of physical activity is commonly defined using an activity count cut point that corresponds to a range of metabolic equivalents (METs). There are over 15 published equations for calculating amount of time spent in light, moderate, and vigorous activity which create very different cut points, and most of the calibration studies supporting this work were conducted with younger adults or in laboratory settings(53). The most common cut points are 100 – 1,952 activity counts per minute for low-intensity activity (1 – 3 METs); 1,952 – 5,724 for moderate-intensity (3 – 6 METs; the equivalent of brisk walking for most healthy adults) and 5,725+ for vigorous activity (> 6 METs)(54). Our previous work confirms that this moderate activity cut point underestimates walking intensity in older adults as measured by oxygen consumption during treadmill tests(55). In addition, accelerometry research shows that physical activity which does not meet the standard cut point is associated with better self-rated health and less arterial stiffness in older adults(56,57) and is equally protective against future arthritis-related disability as moderate-intensity activity(58). In light of these findings, we relied on work by Matthews and colleagues(59,60) which combined information from laboratory and field studies to determine a cut point that may better capture moderate-intensity activities of daily living. Specifically, we defined 760 activity counts per minute or greater as moderate-intensity activity (i.e., moderate-to-vigorous, hereafter referred to as moderate for simplicity).
In regard to daily steps, researchers have argued that the goal of 10,000 steps per day that is popular in the media may not be sustainable for older adults and those living with chronic disease(61). Moreover, it has been argued that older adults can achieve a beneficial level of physical activity by taking 5,000–10,000 steps per day(62).
Data Analysis
Multilevel modeling(63) was used to examine same-day (i.e., concurrent) associations between spousal influence and patient physical activity, and analyses were conducted using SAS PROC MIXED. The dependent variables were modeled separately. In these analyses we modeled within-couple variability in associations between spousal influence and patient physical activity at Level 1, and between-couple variability at Level 2 (i.e., whether within-couple slopes were moderated by between-couple differences in patient gender). The ESTIMATE command from SAS PROC MIXED was used to generate slope estimates and standard errors for male versus female patients.
In these multilevel models we controlled for patients' reports of how tense and enjoyable marital interactions were on that day to ensure that the effects of spousal communications regarding patient physical activity were independent of more general relationship quality. We also controlled for patients' daily pain and accelerometer wear time because of their likely association with daily physical activity. In order to identify additional covariates for our models, we examined bivariate correlations between the dependent variables and multiple background variables (e.g., patient age, education, employment status, physical comorbidity, daily negative affect, and physical activity recommendations from a health care provider). A correlation of r > .30 with at least one of the dependent variables was selected as the criterion for inclusion as a control variable(64). Patient age, employment status, and physical comorbidity met this criterion and thus were included as control variables in the multilevel models. Finally, each participant's diary day was consecutively numbered and this variable was included in analyses to adjust for potential temporal effects of repeated assessments.
In each analysis the patient's dependent variable was modeled as a simultaneous function of the four types of spousal influence (i.e., spouse autonomy support, persuasion, pressure, and minutes of moderate activity/steps), which were all within-person centered; the interaction of each type of influence with patient gender; and day in study. Models included four level 1 covariates that were within-person centered: patient pain, marital tension, marital enjoyment, and accelerometer wear time. Models also included three Level 2 covariates that were grand-mean centered: patient age, gender, and physical comorbidity.
Results
On average, male patients reported receiving more persuasion control (MMales = 1.27, MFemales = 1.13; p = .001) and pressure control (MMales= 1.09, MFemales = 1.02; p = .01) from their spouse than did female patients, consistent with previous research(29,65). The difference between male and female patients in reports of spouse autonomy support was not statistically significant (MMales= 2.01, MFemales = 2.14; p = .14).
For patients, the average amount of time in daily moderate-intensity activity (i.e., 760 activity counts or greater) was 64.45 minutes (SD = 38.93; range = 1.67 – 194.57) and the average number of steps was 4329.5 (SD = 1998.2; range = 152.67 – 9992.90). For spouses, the average amount of moderate activity per day was 67.84 minutes (SD = 41.55; range = 3.05 – 241.35) and the average number of steps was 4856.13 (SD = 2430.08; range = 285.0 – 11856.29). For patients, the average activity count per minute over all days was 188.21 and the average steps per minute was 5.07 For spouses, the average activity count over all days was 200.41 and the average steps per minute was 5.69. Patients and spouses accumulated at least 30 minutes of moderate activity on 64% and 59% of days, respectively. Table 2 presents the within-person correlations among key study variables.
Table 2.
Within-Person Correlations Between Key Variables
| Patient Moderate Minutes | Patient Daily Steps | Autonomy Support | Persuasion Control | Pressure Control | Tension | |
|---|---|---|---|---|---|---|
| Patient Daily Steps | .77* | |||||
| Autonomy Support | .04 | .04 | ||||
| Persuasion Control | .00 | .01 | .08* | |||
| Pressure Control | −.02 | −.01 | −.04 | .34* | ||
| Tension | −.02 | −.02 | −.16* | .02 | .12* | |
| Enjoyment | .00 | .00 | .23* | .05* | −.03 | −.33* |
p < .05.
Table 3 presents the fixed effects for each of the predictors and covariates in the multilevel models. These trimmed models do not include the following nonsignificant predictors at the daily level: marital tension and enjoyment; spouse persuasion control; and interactions of gender with spouse moderate activity/steps, autonomy support, and persuasion control. Our findings did not differ according to whether these terms were included; therefore, we present trimmed models.
Table 3.
Trimmed Multilevel Models of Daily Spousal Influence on Patient Physical Activity
| Minutes in Moderate Activity | Step Count | |||
|---|---|---|---|---|
| Fixed Effects | estimate | (SE) | estimate | (SE) |
| Intercept | 62.18 | 11.77*** | 3483.87 | 584.25*** |
| Age | −1.86 | 0.39*** | –49.51 | 19.45** |
| Gender | 5.08 | 6.06 | −7.97 | 300.48 |
| Physical comorbidity | −2.12 | 1.69 | −305.76 | 83.65*** |
| Employment | 0.51 | 7.46 | 652.66 | 369.61 |
| Daily Measures | ||||
| Pain | 2.14 | 0.44*** | 81.85 | 21.99*** |
| Spouse moderate activity/steps | 0.24 | 0.02*** | 0.34 | 0.02*** |
| Spouse autonomy support | 5.19 | 2.44* | 372.87 | 122.21** |
| Spouse pressure control | 7.62 | 8.55 | 113.90 | 427.83 |
| Spouse pressure control × Gender | −28.16 | 11.44** | −736.62 | 572.07 |
Notes.
All analyses control for minutes of wear time for patient accelerometer, and day in diary study. These trimmed models do not include the following nonsignificant predictors at the daily level: marital tension and enjoyment; spouse persuasion control; and interactions of gender with spouse moderate activity/steps, autonomy support, and persuasion control. Findings did not differ with these terms included.
Ncouples = 141, Nobservations = 1805. Gender: 1 = male, 2 = female. Employment: 1 = not employed, 2 = employed.
p <.05.
p ≤.01.
p < .001.
Among the covariates, patient age was associated with both indicators of physical activity, revealing that there were approximately 2 fewer minutes of daily moderate activity and 49 fewer steps with each additional year of age. With each physical comorbidity, patients took approximately 306 fewer daily steps. Moreover, a higher level of daily pain was associated with a greater level of physical activity on that day, consistent with previous research on lower extremity osteoarthritis(66).
The left half of Table 3 presents the multilevel results for number of minutes of moderate-intensity activity. As predicted, the effect of spouses' moderate activity was positive and significant (estimate = 0.24, p <.001) indicating that on days when spouses spent one more minute in moderate activity than usual, patients increased their time in moderate activity by approximately 15 seconds. The effect of spousal autonomy support also was significant (estimate = 5.19, p < .05), indicating that on days when spouses were more supportive than usual of patients being active in their own way, patients spent approximately 5 more minutes in moderate physical activity. Contrary to prediction, spouses' daily pressure and persuasion were not related to patient moderate activity. However, there was a significant interaction between spouse pressure and patient gender (estimate = −28.16, p < .01). Compared to female patients, and as predicted, greater spouse pressure to be active was associated with less physical activity among men. Figure 1 depicts this interaction, showing that male patients spent approximately 21 fewer minutes in moderate-intensity activity on days when spouses exerted more pressure than usual (estimate = −20.5, p < .01), or 34% fewer minutes than the sample average. Among female patients, however, there was no association between spouse pressure and patient daily activity (estimate = 7.62, p = .37).
Figure 1.
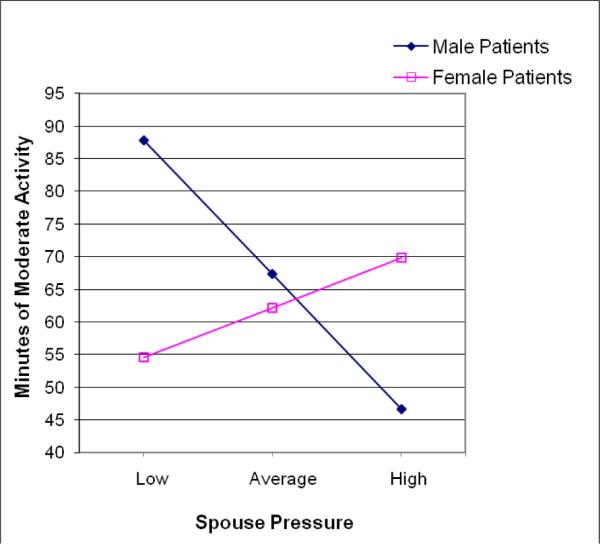
The moderating effect of gender for minutes of patient moderate physical activity. High and low levels of pressure were calculated as 1 standard deviation above and below the mean using the within-person standard deviation to indicate daily deviations in pressure (rather than between person differences). The figure presents estimated values for male and female patients at low, average, and high levels of pressure.
The right half of Table 3 presents the multilevel results for number of daily steps. Our findings were similar to those for moderate physical activity. The effect of spouses' daily steps was positive and significant (estimate = 0.34, p <.001) indicating that on days when spouses took one more step than usual, patients took less than half of an additional step. The effect of spousal autonomy support also was significant (estimate = 372.87, p < .01), showing that on days when spouses were more supportive than usual of patients being active in their own way, patients took approximately 373 more steps. Spouses' daily pressure and persuasion were not associated with patients' daily steps. The interaction between spouse pressure and patient gender was similar to the one found for moderate activity, but it did not reach statistical significance (estimate = −736.62, p = .20). Male patients took approximately 623 fewer steps on days when spouses exerted more pressure to be active (estimate = −622.72; p = .10), or 18% fewer steps than the sample average, whereas there was no significant effect of spouse pressure on female patients' daily steps (estimate = 113.90; p = .79).
We also tested bidirectional, lagged (next-day) effects for spousal influence and patient physical activity, but found no significant main effects or interactions.
Discussion
Close relationships are likely to have an impact on adults' level of activity and are also feasible targets for intervention. In this study we examined associations between patient-perceived spouse behaviors and daily physical activity in knee osteoarthritis because many patients are partnered and this relationship has been shown to be important for patient well-being. We found that patients spent more time in moderate-intensity activity and took more steps on days when they perceived that spouses supported their autonomy in being active and were more active themselves. We also found that male patients spent less time in moderate-intensity activity on days when they perceived that spouses pressured them to be active. Importantly, these associations between spousal influence and patient activity emerged even after adjusting for the effects of demographic factors, health, and daily relationship quality.
We conducted a strong test of the hypothesis that the spouse plays a role in daily physical activity by examining the simultaneous effects of different types of health-related communications that have received much attention in the literature. Contemporary theory and research regarding the influence of social relationships on health behavior have focused on autonomy support and social control (18,26). We found low to moderate intercorrelations among our support and control measures, suggesting that these constructs do tap unique spousal behaviors. Autonomy support, which involves helping patients to find their own ways to be active, was the spousal communication most consistently associated with higher levels of patients' daily physical activity. This finding extends a literature that has largely focused on autonomy support communicated by health care professionals (cf.67). A consistent pattern of findings has shown that such support from a health care provider enhances a patient's perceived competence for diabetes self-care and tobacco abstinence, as well as subsequent behavioral change in these domains (68). Although we do not know of studies comparing the effectiveness of autonomy support communicated by health care professionals to that communicated by family members, we believe that spouses are likely to have a greater impact on patients' daily functioning, due to their daily contact and involvement in patients' illness management (15,69), in comparison to a physician who might only see the patient several times per year.
We found that male patients engaged in less moderate activity on days when they perceived that spouses exerted pressure in this domain. Patients reported that spouses pressured them infrequently, yet pressure was associated with less activity in male patients when it did occur. This finding is consistent with gender-role theory which posits men are more likely than women to be characterized by agency and a focus on instrumentality and separation or individuation from others (41,42) and, by extension, may react more strongly to coercive strategies aimed at changing their behavior. However, this finding is inconsistent with a study by Westmaas and colleagues (70) which found that spousal pressure had a stronger influence on men's smoking cessation than on women's smoking cessation. One explanation for these discrepant findings is that gender may play a different role depending on the nature of the behavior, in that Westmaas and colleagues focused on cessation of an unhealthy behavior whereas we examined enactment of a healthy behavior. That is, women may be more successful in pressuring their husbands to stop behaviors that put themselves and the larger family at risk than in exerting pressure to adopt a healthier lifestyle. Given the number of interactions with gender that were tested in this study, and the low frequency of pressure control observed in this study, caution is warranted in drawing conclusions from this finding until it is replicated.
We did not find that spouses' efforts to persuade were differentially associated with patient physical activity depending on gender, nor did we find main effects of persuasion control on patient physical activity. Looking across studies of health-related social control in couples (30,31,69,71), the nagging and critical tactics that spouses use to influence patient health behaviors seem to be the most impactful type of social control. In this study, such tactics were associated with 21 fewer minutes of daily moderate activity in male patients (i.e., 147 fewer minutes per week), which seems to be a clinically significant decrease given the importance of moderate activity for health. Our findings regarding spouse autonomy support suggest another important facet of social regulation. Although the additional 5 minutes of moderate activity and 373 steps per day associated with greater autonomy support may seem to be of low magnitude, such daily changes likely accumulate over time to protect health.
Our study is one of a few examining spousal influence at the within-couple level, using multilevel analysis of repeated measures data. Most previous research on couples and chronic illness has focused on differences between couples, which can mask variation in within-couple associations in terms of both magnitude and direction. For example, a positive association between spouse behavior and patient outcomes might be observed at the between-couple level whereas the association is negative at the within-couple level (72). An additional strength of our study is the use of accelerometry to measure daily physical activity in both patient and spouse, which avoids the0 bias inherent in self-reported physical activity (44,45). Studies of physical activity in older adults that use accelerometry are rare. Similar to our findings for autonomy support, spouses' own physical activity level was associated with patients' daily moderate activity as well as steps taken. Importantly, we found that spouses' activity level and behaviors toward the patient independently predicted patient physical activity.
We used a criterion for moderate-intensity activity that is designed to capture a broad range of activities during daily life (59) and that is likely to be more appropriate for older adults with knee osteoarthritis than common criteria (54). Using this criterion we found that patients and spouses had approximately an hours' worth of moderate activity during a typical day, but there was also much variability within and between individuals. The average number of steps per day was approximately 4,300 and 4,800 steps for patients and spouses, respectively. Reflecting the level of impairment in our sample, one recent study using accelerometry found that healthy men and women between the ages of 70 and 75 years took 5,661 steps per day on average (73). The similar level of activity in patients and spouses in our study may be due to the fact that approximately 50% of the spouses reported having osteoarthritis or another musculoskeletal problem (with less than moderate pain intensity, as required for study participation).
Despite the daily assessment of spouse and patient behavior, it is important to acknowledge the cross-sectional nature of the daily associations observed in this study. That is, our findings reveal linkages between partners' behaviors occurring on the same day. Thus, we cannot rule out the possibility that the associations between spousal influence and patient activity reflect the reverse temporal ordering. It remains plausible, for example, that on days when male patients were less active than usual, they perceived that spouses exerted pressure to be active in response. Most likely, the association between spouse communication and patient activity is bidirectional.
We tested but did not find lagged effects of spousal influence on patients' physical activity on the next day. Some studies of daily support process in couples have found lagged effects of spouse support on the recipient's emotional well-being and relationship satisfaction (74,75). Perhaps lagged effects do not occur for the types of spousal influence that were examined in this study, or are not observed with objectively-assessed health behaviors. Alternatively, the effects of spouse influence on behavior may be short-term (e.g., within the day). Our study was not designed to examine lagged, within-day effects of spousal support and control. It is also possible that the effects of support or control accumulate over several days' time, or carry over into the next day for only specific types of couples (e.g., those who collaborate in illness management). Future research that is able to examine different time scales for the effects of support and control on health, as well as the frequency of different types of marital interactions, is much needed.
Our focus on couples' experiences as they went about their daily lives yields data with high ecological validity, and examining couple-level predictors of daily within-couple variability is critical for the future development of tailored couple-oriented interventions. Our recent meta-analysis of randomized trials testing fixed (i.e., non-tailored) couple-oriented interventions for chronic illness showed significant but small benefits for patient depressive symptoms, marital functioning, and pain (40). One avenue for strengthening the impact of these interventions is to take a tailored approach in targeting marital or spouse predictors of proximal indicators of health and illness management. Findings from the current study suggest that couple-oriented interventions for knee osteoarthritis should aim to enhance the physical activity level of both patient and spouse, as well as spousal strategies for helping patients find ways to stay active.
Marital functioning is clearly predictive of psychological well-being, physiological reactivity during conflict, and changes in health status (76), and there is a high rate of concordance between partners' health-enhancing and health-compromising behaviors (39,77,78). However, it has been unclear which spousal strategies are associated with daily health behaviors such as physical activity, dietary adherence, smoking or alcohol cessation, medication adherence, and good sleep practices. Studies like the current one, which used a daily assessment approach and measured a health behavior objectively, are important for examining a process by which marriage affects health.
Acknowledgments
This research was supported in part by a grant from the National Institutes of Health (R01 AG026010).
Footnotes
Conflict of Interest Statement: The authors have no conflict of interest to disclose.
References
- 1.U.S. Department of Health and Human Services . Physical Activity Guidelines Advisory Committee Report. Washington, DC: 2008. [Google Scholar]
- 2.Eyler AA, Bronson RC, Donatelle RJ, et al. Physical activity social support and middle- and older-aged minority women: Results from a U.S. survey. Social Science & Medicine. 1999;49:781–789. doi: 10.1016/s0277-9536(99)00137-9. [DOI] [PubMed] [Google Scholar]
- 3.Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health Services Research. 2008;43:96–116. doi: 10.1111/j.1475-6773.2007.00754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis & Rheumatism. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Care and Research. 2008;59(9):1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Steultjens MP, Dekker J, Bijlsma JW. Avoidance of activity and disability in patients with osteoarthritis of the knee: The mediating role of muscle strength. Arthritis & Rheumatism. 2002;46:1784–1788. doi: 10.1002/art.10383. [DOI] [PubMed] [Google Scholar]
- 7.Dunlop DD, Semanik P, Song J, et al. Risk factors for functional decline in older adults with arthritis. Arthritis & Rheumatism. 2005;52:1274–1282. doi: 10.1002/art.20968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: A recommendation from the Centers for Disease Control and the American College of Sports Medicine. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. Centers for Disease Control and Prevention . Physical activity and health: A report of the Surgeon General. Atlanta, GA: 1996. [Google Scholar]
- 10.Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. Journal of the American Geriatrics Society. 2000;48:493–498. doi: 10.1111/j.1532-5415.2000.tb04994.x. [DOI] [PubMed] [Google Scholar]
- 11.Brach JS, FitzGerald S, Newman AB, et al. Physical activity and functional status in community-dwelling older women: A fourteen-year prospective study. Archives of Internal Medicine. 2003;163:2565–2571. doi: 10.1001/archinte.163.21.2565. [DOI] [PubMed] [Google Scholar]
- 12.Iwane M, Arita M, Tomimoto S, et al. Taking 10,000 steps a day or more reduces blood pressur e and sympathetic nerve activity in mild essential hypertension. Hypertension Research. 2000;23:5 73–580. doi: 10.1291/hypres.23.573. [DOI] [PubMed] [Google Scholar]
- 13.Moreau K, Degarmo R, Langley J, et al. Increasing daily walking lowers blood pressure in postmenopausal women. Medicine & Science in Sports & Exercise. 2001;11:1825–1831. doi: 10.1097/00005768-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Sherman AM. Social relations and depressive symptoms in older adults with osteoarthritis. Social Science & Medicine. 2003;56:247–257. doi: 10.1016/s0277-9536(02)00023-0. [DOI] [PubMed] [Google Scholar]
- 15.Holtzman S, DeLongis A. One day at a time: The impact of daily satisfaction with spouse responses on pain, negative affect and catastrophizing among individuals with rheumatoid arthritis. Pain. 2007;131:202–213. doi: 10.1016/j.pain.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 16.Martire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychology. 2002;21:167–176. [PubMed] [Google Scholar]
- 17.Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. Plenum; New York, NY: 1985. [Google Scholar]
- 18.Sheldon KM, Williams GC, Joiner T. Self-determination theory in the clinic: Motivating physical and mental health. Yale University Press; New Haven, CT: 2003. [Google Scholar]
- 19.Fortier MS, Sweet SN, O'Sullivan TL, Williams GC. A self-determination process model of physical activity adoption in the context of a randomized controlled trial. Psychology of Sport and Exercise. 2007;8:741–757. [Google Scholar]
- 20.Ryan RM, Williams GC, Patrick H, Deci EL. Self-determination theory and physical activity: The dynamics of motivation in development and wellness. Hellenic Journal of Psychology. 2009;6:107–124. [Google Scholar]
- 21.Williams GC, Gagne M, Ryan RM, Deci EL. Facilitating autonomous motivation for smoking cessation. Health Psychology. 2002;21:40–50. [PubMed] [Google Scholar]
- 22.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–1651. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 23.Russell KL, Bray SR. Promoting self-determined motivation for exercise in cardiac rehabilitation: The role of autonomy support. Rehabilitation Psychology. 2010;55:74–80. doi: 10.1037/a0018416. [DOI] [PubMed] [Google Scholar]
- 24.Rouse PC, Ntoumanis NL, Duda JL, Jolly K, Williams GC. In the beginning: Role of autonomy support on the motivation, mental health and intentions of participnts entering an exercise referral scheme. Psychology & Health. 2011;26:729–749. doi: 10.1080/08870446.2010.492454. [DOI] [PubMed] [Google Scholar]
- 25.Umberson D. Family status and health behaviors: Social control as a dimension of social integration. Journal of Health and Social Behavior. 1987;28:306–319. [PubMed] [Google Scholar]
- 26.Rook KS. Social networks as a source of social control in older adults' lives. In: Giles H, Coupland N, Wiemann J, editors. Communication, health, and the elderly. University of Manchester Press; Manchester, England: 1990. pp. 45–63. [Google Scholar]
- 27.Hughes M, Gove WR. Living alone, social integration, and mental health. American Journal of Sociology. 1981;87:48–74. doi: 10.1086/227419. [DOI] [PubMed] [Google Scholar]
- 28.Tucker JS, Anders SL. Social control of health behaviors in marriage. Journal of Applied Social Psychology. 2001;31(3):467–485. [Google Scholar]
- 29.Umberson D. Gender, marital status and the social control of health behavior. Social Science & Medicine. 1992;34(8):907–917. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- 30.Stephens MAP, Fekete EM, Franks MM, et al. Spouses' use of pressure and persuasion to promote osteoarthritis patients' medical adherence after orthopedic surgery. Health Psychology. 2009;28:48–55. doi: 10.1037/a0012385. [DOI] [PubMed] [Google Scholar]
- 31.Fekete EM, Geaghan TR, Druley JA. Affective and behavioral reactions to positive and negativ e social control in HIV+ men. Psychology and Health. 2009;24(501–515) doi: 10.1080/08870440801894674. [DOI] [PubMed] [Google Scholar]
- 32.Novak SA, Webster GD. Spousal social control during a weight loss attempt: A daily diary study. Personal Relationships. 2011;18(2):224–241. doi: 10.1111/j.1475-6811.2011.01358.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tucker JS, Orlando M, Elliott MN, Klein DJ. Affective and behavioral responses to health-related social control. Health Psychology. 2006;25:715–722. doi: 10.1037/0278-6133.25.6.715. [DOI] [PubMed] [Google Scholar]
- 34.Tucker JS. Health-related social control within older adults' relationships. Journal of Gerontology: Psychological Sciences. 2002;57:387–395. doi: 10.1093/geronb/57.5.p387. [DOI] [PubMed] [Google Scholar]
- 35.Thorpe C, Lewis M, Sterba K. Reactions to health-related social control in young adults with Type 1 diabetes. Journal of Behavioral Medicine. 2008;31:93–103. doi: 10.1007/s10865-007-9125-4. [DOI] [PubMed] [Google Scholar]
- 36.Stephens MAP, Rook KS, Franks MM, Khan CM, Iida M. Spouses' use of social control to improve diabetic patients' dietary adherence. Families, Systems & Health. 2010;28:199–208. doi: 10.1037/a0020513. [DOI] [PubMed] [Google Scholar]
- 37.Macken LC, Yates B, Blancher S. Concordance of risk factors in female spouses of male partners with coronary disease. Journal of Cardiopulmonary Rehabilitation. 2000;20:361–368. doi: 10.1097/00008483-200011000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: The influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychology. 2006;25:510–520. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- 39.Pettee KK, Brach JS, Kriska AM, et al. Influence of marital status on physical activity levels among older adults. Medicine & Science in Sports & Exercise. 2006;38(3):541–546. doi: 10.1249/01.mss.0000191346.95244.f7. [DOI] [PubMed] [Google Scholar]
- 40.Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Spence JT, Helmreich RL, Holahan CK. Negative and positive components of psychological masculinity and femininity and their relationships to neurotic and acting out behaviors. Journal of Personality and Social Psychology. 1979;37:1673–1682. [PubMed] [Google Scholar]
- 42.Bakan D. The duality of human existence: Isolation and communion in Western man. Rand McNally; Chicago, IL: 1966. [Google Scholar]
- 43.The NS, Gordon-Larsen P. Entry into romantic partnership is associated with obesity. Obesity. 2009;17(7):1441–1447. doi: 10.1038/oby.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ewald B, McEvoy M, Attia J. Pedometer counts superior to physical activity scale for identifying health markers in older adults. British Journal of Sports Medicine. 2010;44(10):756–761. doi: 10.1136/bjsm.2008.048827. [DOI] [PubMed] [Google Scholar]
- 45.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 46.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Medicine & Science in Sports & Exercise. 2002;34(8):1376–1381. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 47.Swartz AM, Strath SJ, Bassett DR, Jr., et al. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Medicine & Science in Sports & Exercise. 2000;32:450–456. doi: 10.1097/00005768-200009001-00003. [DOI] [PubMed] [Google Scholar]
- 48.Martire LM, Scheier MF. Physical comorbidity index. 2000. [Google Scholar]
- 49.Williams GC, Lynch MF, McGregor HA, et al. Validation of the “important other” climate questionnaire: Assessing autonomy support for health-related change. Families, Systems & Health. 2006;24(2):179–194. [Google Scholar]
- 50.Lewis MA, Rook KS. Social control in personal relationships: Impact on health behaviors. Health Psychology. 1999;18:63–71. doi: 10.1037//0278-6133.18.1.63. [DOI] [PubMed] [Google Scholar]
- 51.Mason JH, Anderson JJ, Meenan RF, et al. The rapid assessment of disease activity in rheumatology (RADAR) questionnaire: Validity and sensitivity to change of a patient self-report measure of joint count and clinical status. Arthritis & Rheumatism. 1992;35(2):156–162. doi: 10.1002/art.1780350206. [DOI] [PubMed] [Google Scholar]
- 52.Prager KJ, Buhrmester D. Intimacy and need fulfillment in couple relationships. Journal of Social and Personal Relationships. 1998;15(4):435–469. [Google Scholar]
- 53.Crouter SE, Churilla JR, Bassett DR., Jr. Estimating energy expenditure using accelerometers. European Journal of Applied Physiology. 2006;98:602–612. doi: 10.1007/s00421-006-0307-5. [DOI] [PubMed] [Google Scholar]
- 54.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Medicine & Science in Sports & Exercise. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 55.Brach JS, Wert D, VanSwearingen JM, Studenski SA. The Compendium of Physical Activity underestimates walking intensity in old more so than in young. Journal of the American Geriatrics Society. 2009;57:S110. [Google Scholar]
- 56.Buman MP, Hekler EB, Haskell WL, et al. Objective light-intensity physical activity associations with rated health in older adults. American Journal of Epidemiology. 2010;172:1155–1165. doi: 10.1093/aje/kwq249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gando Y, Yamamoto K, Murakami H, et al. Longer time spent in light physical activity is associated with reduced arterial stiffness in older adults. Hypertension. 2010;56:540–546. doi: 10.1161/HYPERTENSIONAHA.110.156331. [DOI] [PubMed] [Google Scholar]
- 58.Feinglass J, Thompson JA, He XZ, et al. Effect of physical activity on functional status among older middle-age adults with arthritis. Arthritis & Rheumatism. 2005;53:879–885. doi: 10.1002/art.21579. [DOI] [PubMed] [Google Scholar]
- 59.Matthews CE. Calibration of accelerometer output for adults. Medicine & Science in Sports & Exercise. 2005;37(11):S512–S522. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 60.Matthews CE, Ainsworth BE, Hanby C, et al. Development and testing of a short physical activity recall questionnaire. Medicine & Science in Sports & Exercise. 2005;37(6):986–994. [PubMed] [Google Scholar]
- 61.Tudor-Locke C, Bassett DR., Jr. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Medicine. 2004;34:1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- 62.Payn T, Pfeiffer KA, Hutto B, et al. Daily steps in midlife and older adults: Relationship with demographic, self-rated health, and self-reported physical activity. Research Quarterly for Exercise and Sport. 2008;79:128–132. doi: 10.1080/02701367.2008.10599475. [DOI] [PubMed] [Google Scholar]
- 63.Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- 64.Reichardt CS. The statistical analysis of data from nonequivalent group designs. In: Cook TD, Campbell DT, editors. Quasi-experimentation: Design & analysis issues for field settings. Houghton Mifflin; Boston, MA: 1979. pp. 147–205. [Google Scholar]
- 65.August KJ, Sorkin DH. Marital status and gender differences in managing a chronic illness: The function of health-related social control. Social Science & Medicine. 2010;71:1831–1838. doi: 10.1016/j.socscimed.2010.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Murphy SL, Smith DM, Clauw DJ, Alexander NB. The impact of momentary pain and fatigue on physical activity in women with osteoarthritis. Arthritis & Rheumatism. 2008;59(6):849–856. doi: 10.1002/art.23710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kasser VG, Ryan RM. The relation of psychosocial needs for autonomy and relatedness to vitality, well-being, and mortality in a nursing home. Journal of Applied Social Psychology. 1999;29(5):935–954. [Google Scholar]
- 68.Williams GC, McGregor HA, Sharp D, et al. Testing a self-determination theory intervention for motivating tobacco cessation: Supporting autonomy and competence in a clinical trial. Health Psychology. 2006;25:91–101. doi: 10.1037/0278-6133.25.1.91. [DOI] [PubMed] [Google Scholar]
- 69.Stephens MAP, Franks MM, Rook KS, et al. Spouses' attempts to regulate day-today dietary adherence among patients with Type 2 diabetes. Health Psychology. doi: 10.1037/a0030018. doi: 10.1037/a003 0018. [DOI] [PubMed] [Google Scholar]
- 70.Westmaas J, Wild T, Ferrence R. Effects of gender in social control of smoking cessation. Health Psychology. 2002;21:368–376. doi: 10.1037//0278-6133.21.4.368. [DOI] [PubMed] [Google Scholar]
- 71.Tucker JS, Edelen MO, Elliott MN, Klein DJ. Affective and behavioral responses to health-related social control. Health Psychology. 2006;25(6):715–722. doi: 10.1037/0278-6133.25.6.715. [DOI] [PubMed] [Google Scholar]
- 72.Nezlek JB. Using multilevel random coefficient modeling to analyze social interaction diary data. Journal of Social and Personal Relationships. 2003;20(4):437–469. [Google Scholar]
- 73.Davis MG, Fox KR, Hillsdon M, et al. Objectively measured physical activity in a diverse sample of older urban UK adults. Medicine & Science in Sports & Exercise. 2011;43(4):647–654. doi: 10.1249/MSS.0b013e3181f36196. [DOI] [PubMed] [Google Scholar]
- 74.Gleason MEJ, Iida M, Shrout PE, Bolger N. Receiving support as a mixed blessing: Evidence for dual effects of support on psychological outcomes. Journal of Personality and Social Psychology. 2008;94:824–838. doi: 10.1037/0022-3514.94.5.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rafaeli E, Cranford JA, Green AS, Shrout PE, Bolger N. The good and bad of relationships: How social hindrance and social support affect relationship feelings in daily life. Personality and Social Psychology Bulletin. 2008;34(12):1703–1718. doi: 10.1177/0146167208323742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kiecolt-Glaser JK, Newton TL. Marriage and Health: His and Hers. Psychological Bulletin. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 77.Franks MM, Pienta AM, Wray LA. It takes two: Marriage and smoking cessation in the middle years. Journal of Aging and Health. 2002;14(3):336–354. doi: 10.1177/08964302014003002. [DOI] [PubMed] [Google Scholar]
- 78.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]


