Abstract
Despite the large burden of chronic kidney disease (CKD) in Hispanics, this population has been underrepresented in research studies. We describe the recruitment strategies employed by the Hispanic Chronic Renal Insufficiency Cohort Study, which led to the successful enrollment of a large population of Hispanic adults with CKD into a prospective observational cohort study. Recruitment efforts by bilingual staff focused on community clinics with Hispanic providers in high-density Hispanic neighborhoods in Chicago, academic medical centers, and private nephrology practices. Methods of publicizing the study included church meetings, local Hispanic print media, Spanish television and radio stations, and local health fairs. From October 2005 to July 2008, we recruited 327 Hispanics aged 21–74 years with mild-to-moderate CKD as determined by age-specific estimated glomerular filtration rate (eGFR). Of 716 individuals completing a screening visit, 49% did not meet eGFR inclusion criteria and 46% completed a baseline visit. The mean age at enrollment was 57.1 and 67.1% of participants were male. Approximately 75% of enrolled individuals were Mexican American, 15% Puerto Rican, and 10% had other Latin American ancestry. Eighty two percent of participants were Spanish-speakers. Community-based and academic primary care clinics yielded the highest percentage of participants screened (45.9% and 22.4%) and enrolled (38.2% and 24.5%). However, academic and community-based specialty clinics achieved the highest enrollment yield from individuals screened (61.9% to 71.4%). A strategy focused on primary care and nephrology clinics and the use of bilingual recruiters allowed us to overcome barriers to the recruitment of Hispanics with CKD.
Introduction
Hispanics are the largest and fastest growing ethnic minority group in the United States.1 Given the health care needs associated with the growth and disease burden of this population, the inclusion of Hispanics in health-related research studies is necessary to identify specific risk factors and health care challenges that may be specific to this population. Hispanics with chronic kidney disease (CKD) are more likely to progress to end stage renal disease than non-Hispanics.2 Yet, limited data are available regarding the risk factors for progression of CKD in Hispanics because historically they have been underrepresented in CKD studies.3;4 Several barriers have been identified in the recruitment of Hispanics into clinical studies including costs of participation, lack of transportation, limited English language proficiency, low health literacy, and decreased trust.5–7 However, successful strategies to circumvent these barriers are poorly described.8
To better understand the natural history and risk factors associated with CKD in Hispanics, the Hispanic Chronic Renal Insufficiency (CRIC) Study9 was established at the University of Illinois at Chicago (UIC) as an ancillary study to a multi-center observational study of CKD, the Chronic Renal Insufficiency Cohort (CRIC) Study.10;11 In this manuscript, we characterize our approach to the successful recruitment of a large cohort of adult Hispanics with mild-to-moderate CKD into the Hispanic CRIC Study.
Methods
Study Setting and Eligibility Criteria
Recruitment for the Hispanic CRIC Study was conducted in the greater Chicago area between October 2005 and July 2008. Details regarding the design, methods, and baseline characteristics of the cohort have been previously described.9–11 Briefly, eligible participants were self-reported Hispanics aged 21–74 years with mild to moderate CKD as defined by age-based estimated glomerular filtration rate (eGFR) entry criteria (eGFR of 20–70 ml/1.73m2 for ages 21–44; 20–60 ml/1.73m2 for ages 45 to 54; and 20–50 ml/1.73m2 for ages 65–74). The primary exclusion criteria were: inability to provide consent, New York Heart Association (NYHA) Class III or IV heart failure, cirrhosis/chronic active hepatitis, known HIV infection, prior dialysis, organ/bone marrow transplant, use of immunosuppressives for renal disease within 6 months, chemotherapy for malignancy within 2 years, and polycystic kidney disease. Participants attend annual visits at the UIC Clinical Research Center and are contacted by phone every six months. The study was approved by the UIC institutional review board (IRB) and the research was conducted in accordance with the ethical principles of the Declaration of Helsinki. Written informed consent was obtained from all participants.
Recruitment Team
The Hispanic CRIC Study recruitment team was comprised of two full-time bilingual Hispanic individuals of Mexican and Puerto Rican background who grew up in Hispanic neighborhoods in Chicago. During the 33 months of recruitment, these two recruitment team members, a medical assistant and a recent college graduate, each devoted 50% of their effort to recruitment activities and 50% to study visits, including screening visits and subsequent follow-up. In addition, an office manager devoted 75% effort to recruitment activities (mailings, speaking to potential participants, tracking physician referrals, and scheduling visits). Lastly, local internal medicine residents and nephrology fellows volunteered on an ad-hoc basis to discuss the need for referral of patients to the study with primary care providers in the community
Recruitment Strategies at Academic Medical Centers
Two academic centers participated in the recruitment of the cohort: UIC Medical Center and John Stroger Hospital of Cook Country (JSH). At UIC, we obtained an IRB waiver of the Health Insurance Portability and Accountability Act of 1996 to allow retrospective review of the electronic medical records (EMR) of individuals with scheduled appointments in the general medicine, family practice, nephrology and cardiology clinics. Study staff reviewed the EMR to identify eligible individuals based on the last available creatinine-based eGFR. Potentially eligible participants were approached directly at their scheduled clinic appointment. Those who did come in for the appointment were mailed a letter by their physicians stating that they had been identified as potentially eligible for the study and would be receiving a phone call by study staff. This letter also contained the goals of the studies and a return postcard for requesting additional information. The postcard did not provide an opt-out option. At JSH, eligible participants were identified directly by health care providers at the time of their regular general medicine, family practice or nephrology clinic visit, and referred to the study staff for further discussion. A study staff member was present during most clinic sessions.
Recruitment from Primary Care and Nephrology Physicians in High-Density Hispanic Communities
We selected zip codes for communities with greater than 40% Hispanic population using data from the 2000 United States Census.12 Using internet search engines and based on a list of common Hispanic surnames,13 we identified and contacted primary care and nephrology providers with Hispanic surnames within these zip codes. Study staff met in person with the providers and clinic staff to discuss the study goals and procedures. Clinics interested in facilitating study recruitment were asked to generate a list of eligible patients through their own internal chart review. A standard letter with information regarding the study and the study’s contact number was mailed by the provider to potentially eligible participants. Potential participants who contacted the study staff were screened via telephone for exclusion criteria. Those not meeting exclusion criteria were scheduled for a screening visit.
Other Community Outreach
The study investigators worked with community organizations including the Chicago Hispanic Health Coalition, the Midwest Latino Health and Policy Training Center, and the National Kidney Foundation of Illinois (NKFI). These organizations served to introduce the study to key members of the Hispanic community. The study was also publicized in local Hispanic printed media. An article regarding CKD in Hispanics and the goals of the Hispanic CRIC study was published in the newspaper La Raza which is the leading Spanish newspaper in the Chicago area. A similar article was also published in the free monthly health magazine Un Buen Doctor which is delivered to primary care clinics for display in the waiting area and is also available online. Lastly, a study investigator was interviewed on the leading Spanish radio station in Chicago, WOJO 105.1 FM.
Other sites of recruitment included free health fairs in the Chicago area and a local church. Study staff volunteered in three free health screening fairs in Hispanic neighborhoods and one health fair in the Mexican Consulate sponsored by the NKFI. Health fair attendees who had self-reported kidney disease or proteinuria by urine dipstick were informed about the study and, if interested, were scheduled for a screening visit. Study recruiters also spoke about the study at a Catholic church located in a Hispanic neighborhood on two separate Sundays. In addition, we actively sought referrals of family and friends of participants already enrolled in the study using word of mouth and an IRB approved letter addressed to participants.
Discussion with Potential Participants
Potentially eligible individuals who expressed interest in the study were approached by recruitment staff, in person or by phone, to discuss the study goals in their language of preference (English or Spanish). Special emphasis was placed on describing the study design as strictly observational. The recruitment script also included a brief explanation of the burden of kidney disease in the Hispanic community and the benefits of participation, including reimbursement for time and transportation, and mailing of test results to primary care physicians. At the end of an in-person encounter, individuals were given written bilingual recruitment material with a description of the study and a telephone number to contact if interested. Potential participants who demonstrated immediate interest in the study were scheduled for a screening visit. Individuals who did not show immediate interest were encouraged to discuss the study with their family.
RESULTS
Participant Characteristics
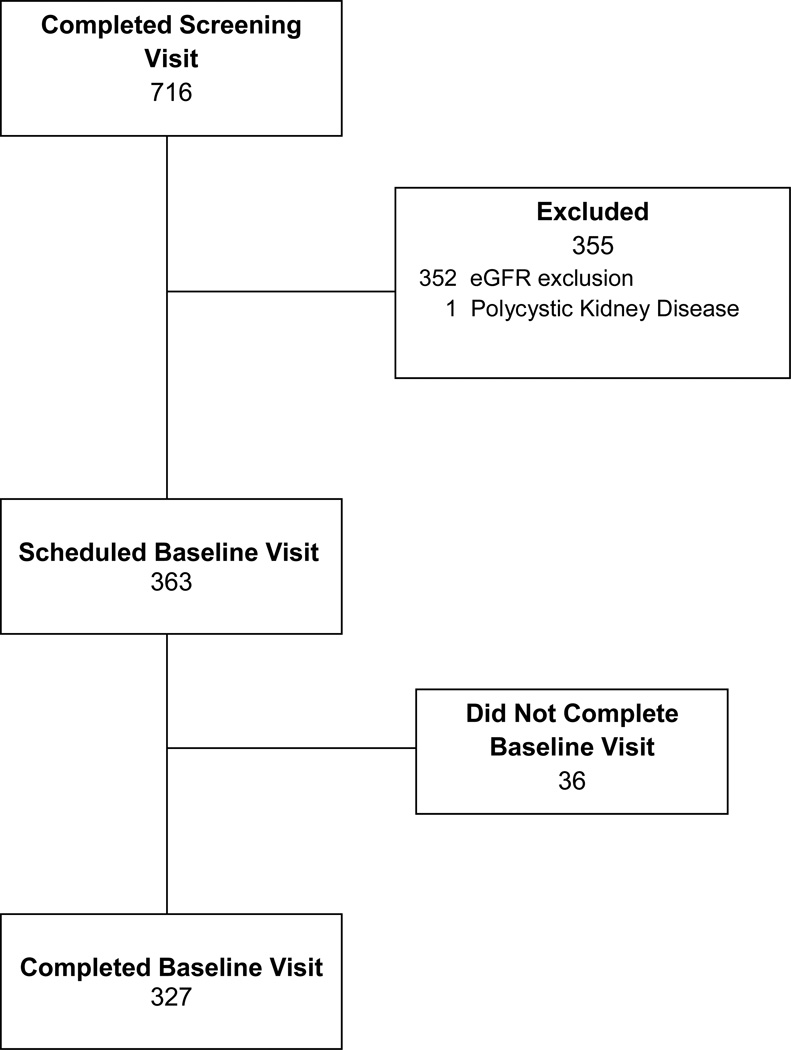
Over a period of 34 months, 716 individuals agreed to a screening visit at the UIC Clinical Research Center. Of those, 352 were ineligible based on level of kidney function (322 above the upper eGFR limit and 30 below the lower limit), one had polycystic kidney disease, (Figure 1). A total of 363 individuals met inclusion criteria (50.7% of persons screened) and were scheduled for a baseline visit. Thirty-six eligible individuals were no longer interested in participating and did not complete a baseline visit. Out of 327 individuals who enrolled in the study and completed a baseline visit, 82% were primary Spanish speakers. Most participants were Mexican American (75%), while the remainder were either were Puerto Rican (15%), or of other Latin American ancestry (10%). The mean age of the cohort at baseline was 57.1 years and 67.1% of participants were male. Nearly 80% of the cohort reported an annual household income of $20,000 or less; almost half (47%) had an educational attainment of sixth grade or less, and 38% were uninsured.
Figure 1.
Participant Recruitment Flow Diagram
Screening and Enrollment by Recruitment Strategy
The majority of individuals not meeting eGFR inclusion criteria had an eGFR which was too high for inclusion. All individuals screened from non-clinic sources (e.g., health fairs, advertisements) had an eGFR which was too high for inclusion. However, among individuals from nephrology clinics who failed screening due to eGFR inclusion criteria, 73.1% had an eGFR above the inclusion criteria and 26.9% had an eGFR which was too low.
Community- and academic-based primary care clinics were the largest sources of participants screened (45.9% and 22.4%) and had the highest yield of persons screened (38.2% and 24.5%) (Table 1). However, nephrology clinics (academic- and community-based) and cardiology clinics achieved the highest enrollment yield from individuals screened (68.1%, 61.9% and 71.4%, respectively). Health fairs, church, and media advertisement were the source of the smallest number of participants screened, as well as the lowest enrollment yield.
Table 1.
Screening and Enrollment Results by Recruitment Strategy
| Source of Recruitment | Screened N (%) |
Enrolled N (%) |
Enrolled from Screened (%) |
|---|---|---|---|
| Overall | 716 (100) | 327 (100) | 45.5 |
| Academic Medical Center Clinics | |||
| Primary Care | 161 (22.4) | 80 (24.5) | 49.6 |
| Nephrology | 69 (9.7) | 47 (14.4) | 68.1 |
| Cardiology | 7 (<1) | 5 (1.5) | 71.4 |
| Community-Based Clinics | |||
| Primary Care | 328 (45.9) | 125 (38.2) | 38.1 |
| Nephrology | 110 (15.4) | 69 (21.1) | 61.9 |
| Cardiology | 0 (0) | 0 (0) | 0 |
| Other Sources | |||
| Health Fairs | 7 (<1) | 0 | 0 |
| Church | 12 (1.7) | 0 | 0 |
| Family | 16 (2.2) | 0 | 0 |
| Referrals | |||
| Media | 4 (<1) | 0 | 0 |
| Other | 2 (<1) | 1 (<1) | 50 |
DISCUSSION
We successfully recruited a cohort of 327 Hispanics with mild-to-moderate CKD using bilingual study staff and a strategy focused on academic medical centers and community-based primary care practices serving a large Hispanic population. Whereas primary care clinics yielded the largest numbers of participants screened and enrolled, academic specialty clinics had the highest enrollment yield from individuals screened. As a result of these efforts, the study assembled the first cohort of Hispanics with mildto-moderate CKD to be followed prospectively in the United States (U.S.).
Hispanics in the U.S. face multiple system-level barriers to participation in clinical research. The costs associated with research study participation, including transportation, child care and loss of wages, may be more significant for Hispanic individuals6 who have a poverty rate almost double that of non-Hispanic Whites.14 In addition, almost 60% of Hispanic adults living in the U.S. have inadequate or no health insurance15 which has been found to be a barrier to participation in cancer clinical trials.16 Moreover, lack of health insurance is associated with decreased use of health services which may limit exposure to research enrollment opportunities.17 As expected, Hispanic CRIC Study participants are burdened by low income, low educational attainment, and lack of health insurance.9 Reimbursement for time and transportation likely played an important role in reducing barriers to participation related to low socioeconomic status. Similar strategies have been successful in overcoming economic barriers to the recruitment of minorities into other clinical research studies.18;19 Additionally, free health testing and reporting offered by the study likely appealed to underinsured and uninsured participants.
Hispanics also face individual-level barriers to enrollment in clinical research studies related to English language proficiency, health literacy, and disease-related knowledge.7;20 In the Hispanic CRIC Study, greater than 80% of participants reported Spanish language preference, and close to 60% percent had marginal or inadequate health literacy.21 We believe that the use of culturally competent, bilingual recruitment staff was an essential component to overcome challenges related to language and literacy and successfully engage this underprivileged population in a research study. Others have reported similar success with using culturally competent bilingual staff to successfully recruit Hispanics.22
Mistrust is a known barrier to the recruitment of Hispanics into clinical studies.5;23 Securing the endorsement of primary care providers was essential to the success of recruitment. Hispanics view health care providers as authority figures and trust that their advice is caring because of their strong belief in respect and paternalism.24;25 Furthermore, it is well established that Hispanic patients prefer providers of Hispanic origin.26 Identifying and engaging the support of Hispanic providers was an important component of our recruitment strategy. Although we were not able to capture the impact of provider ethnicity on study recruitment, it is reasonable to hypothesize that recruitment involving Hispanic providers was more successful because of greater enthusiasm about clinical research involving Hispanics and more effective patient-provider communication and trust. We found community-based providers to be highly committed to improving health outcomes in the Hispanic community and that they embraced the study’s aims. In addition, the presence of our clinic staff during clinic visits further augmented potential participant’s trust in the study. While this strategy required more effort from the study team, it emphasized to the potential participant that their provider endorsed the study. Lastly, by encouraging the discussion of the study with family members, our study staff acknowledged Hispanics’ strong attachment to the family unit.27
In the Hispanic CRIC Study, recruitment from nephrology and cardiology clinics yielded the highest percentages of participants enrolled from screened because these clinics are enriched with CKD patients. This suggests that it may be cost-effective to focus on specialty clinics when recruiting Hispanics with CKD. However, limiting recruitment to these types of clinics may introduce selection bias and result in the recruitment of a cohort that is not representative of the Hispanic CKD population. Other recruitment strategies that were non-clinical were not as successful. This was likely due to the low prevalence of moderate CKD in the general population28 and is consistent with the recruitment experience of other CKD studies.29 Nonetheless, our efforts involving churches, health fairs and the media were well received by the Hispanic community. While these efforts may not have been successful in terms of recruitment, we believed that they provided an educational opportunity to increase awareness of kidney disease among Hispanics and to raise the visibility of the study in the community. Additionally, lack of awareness of clinical research is a known barrier to minority participation in research,5 and this may be more pronounced among Spanish speaking or low acculturation Hispanics. We believe that our recruitment efforts had a positive impact upon community awareness of clinical research.
This report has a few limitations. We did not track the total number of informational letters mailed, consequently, we are unable to determine the response rate for this approach. Additionally, we did not track the response rate for the return postcards which were utilized at the academic center. Because we did not completely capture data prior to the screening visit, we were not able to evaluate the characteristics of non-participants and reasons for non-participation. Similarly, we were also not able to quantify the efficacy and costs of different recruitment approaches (e.g., on site recruitment, letters, phone calls). In addition, we did not comprehensively evaluate provider characteristics associated with willingness to endorse study recruitment. Furthermore, we have described a single center’s experience in an urban setting and our methods may not be successful in a rural setting. Similarly, because of potential selection bias introduced by the predominate methods used for cohort recruitment, our findings may not be generalizable to the entire Hispanic CKD population. However, the composition of the cohort by country of origin is generally reflective of the heterogeneity of U.S. Hispanics and the socioeconomic disparities observed in the cohort are of a similar magnitude to those found in Hispanics in NHANES III, a well recognized nationally representative sample of U.S. adults.30;31 For these reasons, we believe that the study sample is adequately representative of the population of U.S. Hispanics with CKD.
In conclusion, a strategy focused on clinical practices with large Hispanic populations and the use of bilingual recruiters led to successful recruitment of Hispanics into clinical research. It is our hope that implementation of similar strategies will insure that Hispanics will be more adequately represented in future CKD research studies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.U.S. Census. [Accessed February 26, 2009];Nation's population one-third minority. 2008 http://www census gov/Press-Release/www/releases/archives/population/006808 html [serial online]
- 2.U S Renal Data System. USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States http://www.usrds.org/adr.htm. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2010. 6-30-2011. Ref Type: Online Source. [Google Scholar]
- 3.NIH policy and guidelines on the inclusion of women and minorities as subjects in clinical research. 6-10-1993. 11-15-2009. Ref Type: Internet Communication. [Google Scholar]
- 4.Kopple JD, Berg R, Houser H, Steinman TI, Teschan P. Nutritional status of patients with different levels of chronic renal insufficiency. Modification of Diet in Renal Disease (MDRD) Study Group. Kidney Int Suppl. 1989;27:S184–S194. [PubMed] [Google Scholar]
- 5.Ford JG, Howerton MW, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer. 2008;112:228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- 6.Ramirez AG, McAlister A, Gallion KJ, Villarreal R. Targeting Hispanic populations: future research and prevention strategies. Environ Health Perspect. 1995;103(Suppl 8):287–290. doi: 10.1289/ehp.95103s8287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown DR, Fouad MN, Basen-Engquist K, Tortolero-Luna G. Recruitment and retention of minority women in cancer screening, prevention, and treatment trials. Ann Epidemiol. 2000;10:S13–S21. doi: 10.1016/s1047-2797(00)00197-6. [DOI] [PubMed] [Google Scholar]
- 8.Ndumele CD, Ableman G, Russell BE, Gurrola E, Hicks LS. Publication of recruitment methods in focus group research of minority populations with chronic disease: a systematic review. J Health Care Poor Underserved. 2011;22:5–23. doi: 10.1353/hpu.2011.0031. [DOI] [PubMed] [Google Scholar]
- 9.Fischer MJ, Go AS, Lora CM, et al. CKD in Hispanics: Baseline Characteristics From the CRIC (Chronic Renal Insufficiency Cohort) and Hispanic-CRIC Studies. Am J Kidney Dis. 2011 doi: 10.1053/j.ajkd.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldman HI, Appel LJ, Chertow GM, et al. The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and Methods. J Am Soc Nephrol. 2003;14:S148–S153. doi: 10.1097/01.asn.0000070149.78399.ce. [DOI] [PubMed] [Google Scholar]
- 11.Lash JP, Go AS, Appel LJ, et al. Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol. 2009;4:1302–1311. doi: 10.2215/CJN.00070109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NIPC ReGIS. Hispanic Population as Percent of 2000 Total by Suburban Municipality and Chicago Community Area. 3-15-2002. Chicago, Illinois, Northeastern Illinois Planning Commission. Ref Type: Map. [Google Scholar]
- 13.Most Common Last Names for Latinos in the U.S. http://names.mongabay.com/data/hispanic.html. 2011 Ref Type: Online Source.
- 14.U.S. Census Bureau. The 2011 Statistical Abstract. http://www.census.gov/compendia/statab/cats/income_expenditures_poverty_we alth.html. 1-20-2011. 3-14-2011. Ref Type: Online Source.
- 15.Livingston G. Hispanics, Health Insurance and Health Care Access. http://pewhispanic.org/reports/report.php?ReportID=113. 9-25-2009. 8-18-2011. Ref Type: Online Source. [Google Scholar]
- 16.Sateren WB, Trimble EL, Abrams J, et al. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. J Clin Oncol. 2002;20:2109–2117. doi: 10.1200/JCO.2002.08.056. [DOI] [PubMed] [Google Scholar]
- 17.McWilliams JM. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443–494. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ejiogu N, Norbeck JH, Mason MA, Cromwell BC, Zonderman AB, Evans MK. Recruitment and retention strategies for minority or poor clinical research participants: lessons from the Healthy Aging in Neighborhoods of Diversity across the Life Span study. Gerontologist. 2011;51(Suppl 1):S33–S45. doi: 10.1093/geront/gnr027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toobert DJ, Strycker LA, Glasgow RE, et al. Viva bien!: Overcoming recruitment challenges in a multiple-risk-factor diabetes trial. Am J Health Behav. 2010;34:432–441. doi: 10.5993/ajhb.34.4.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Link MW, Mokdad AH, Stackhouse HF, Flowers NT. Race, ethnicity, and linguistic isolation as determinants of participation in public health surveillance surveys. Prev Chronic Dis. 2006;3:A09. [PMC free article] [PubMed] [Google Scholar]
- 21.Lora CM, Daviglus ML, Kusek JW, et al. Chronic kidney disease in United States Hispanics: a growing public health problem. Ethn Dis. 2009;19:466–472. [PMC free article] [PubMed] [Google Scholar]
- 22.Chasan-Taber L, Fortner RT, Hastings V, Markenson G. Strategies for recruiting Hispanic women into a prospective cohort study of modifiable risk factors for gestational diabetes mellitus. BMC Pregnancy Childbirth. 2009;9:57. doi: 10.1186/1471-2393-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin MA, Swider SM, Olinger T, et al. Recruitment of Mexican American adults for an intensive diabetes intervention trial. Ethn Dis. 2011;21:7–12. [PMC free article] [PubMed] [Google Scholar]
- 24.Vega WA, Sallis JF, Patterson T, Rupp J, Atkins C, Nader PR. Assessing knowledge of cardiovascular health-related diet and exercise behaviors in Angloand Mexican-Americans. Prev Med. 1987;16:696–709. doi: 10.1016/0091-7435(87)90052-1. [DOI] [PubMed] [Google Scholar]
- 25.Larkey LK, Gonzalez JA, Mar LE, Glantz N. Latina recruitment for cancer prevention education via Community Based Participatory Research strategies. Contemp Clin Trials. 2009;30:47–54. doi: 10.1016/j.cct.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Evans BC, Coon DW, Crogan NL. Personalismo and breaking barriers: accessing Hispanic populations for clinical services and research. Geriatr Nurs. 2007;28:289–296. doi: 10.1016/j.gerinurse.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 27.Phillips AK, Fischer BA, Baxter RJ, Shafranski SA, Coe CL, Kling PJ. Recruiting Latina families in a study of infant iron deficiency: a description of barriers, study adjustments and review of the literature. WMJ. 2011;110:26–31. [PMC free article] [PubMed] [Google Scholar]
- 28.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–2047. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 29.Phillips RA, Faulkner M, Gassman J, et al. Recruitment of African Americans with chronic renal insufficiency into a multicenter clinical trial: the african american study of kidney disease and hypertension. J Clin Hypertens (Greenwich ) 2004;6:430–436. doi: 10.1111/j.1524-6175.2004.03555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population. 2010 Ríos-Vargas,andNora G.Albert. 2011. 4-26-2012. Ref Type: Online Source. [Google Scholar]
- 31.Mehrotra R, Kermah D, Fried L, Adler S, Norris K. Racial differences in mortality among those with CKD. J Am Soc Nephrol. 2008;19:1403–1410. doi: 10.1681/ASN.2007070747. [DOI] [PMC free article] [PubMed] [Google Scholar]