Abstract
Objective
To describe outcomes of the conservative treatment of patients who had the clinical presentation of a prearthritic, intra-articular hip disorder, including acetabular labral tears, developmental hip dysplasia, and femoroacetabular impingement.
Design
Prospective observational clinical outcomes study.
Setting
Outpatient orthopedic clinic at a tertiary university hospital.
Patients
Patients presenting with prearthritic, intra-articular hip disorders were recruited. Fifty-eight consecutive patients were enrolled; 6 were lost to follow-up, and 52 subjects completed the study.
Methods
Patients were recruited on the basis of symptoms, distribution of pain, and the findings of a physical examination. Radiographic measurements of the hip were obtained for all subjects to describe the presence or absence and extent of deformity and/or osteoarthritis. All subjects completed a directed course of conservative treatment. After 3 months of conservative care, subjects with continued limitations, reduction of symptoms with a diagnostic intra-articular hip injection, and a surgically amenable lesion found on a magnetic resonance arthrogram proceeded to surgery.
Main Outcome Measurements
Numeric Pain Score (0–10), Short Form-12, Modified Harris Hip Score, Western Ontario and McMaster Universities Osteoarthritis Index, Nonarthritic Hip Score, Baecke Questionnaire of Habitual Activity, and patient choice to have surgery.
Results
Fifty-eight patients (9 men and 49 women) with a mean age of 35 ± 11 years (range, 18–50 years) enrolled in the study. Fifty-two subjects completed the study. Twenty-three subjects (44%) reported satisfaction with conservative care. Twenty-nine subjects (56%) chose to have surgery. Both groups demonstrated equally significant improvement (P value ranges: P = .03 to P = .0001) in all outcome measures from baseline to 1-year follow-up. Subjects who chose surgery had higher baseline activity scores compared with the conservative treatment group (P = .02).
Conclusion
All subjects with signs and symptoms of prearthritic, intra-articular hip disorders who were treated with conservative treatment alone and with conservative treatment followed by surgery demonstrated significant improvement in pain and functioning from baseline to 1 year. Forty-four percent of patients improved with conservative care alone, and 56% chose to have surgery after receiving conservative care. Persons with more active lifestyles were more likely to choose surgery. These data suggest that a trial of conservative management for persons with prearthritic, intra-articular hip disorders should be considered before engaging in surgical intervention.
INTRODUCTION
Advancements in imaging and arthroscopy techniques have improved health care providers’ understanding of hip disorders that occur before the onset of arthritis [1–8]. Prearthritic hip disorders are defined as abnormalities of the articulating surfaces of the acetabulum and femur before the onset of osteoarthritis, including intra-articular structures such as the acetabular labrum and chondral surfaces. Abnormalities of these structures can lead to a continuum of biomechanical changes and extra-articular adaptations that can cause significant hip pain and dysfunction in young adults [9–12].
An evolving body of literature has emerged that correlates subtle osseous abnormalities of the acetabulum and femur to acetabular labral and chondral abnormalities [13,14]. Developmental dysplasia of the hip (DDH) results from decreased acetabular coverage of the femoral head and predisposes the labrum and articular cartilage to abnormal forces and therefore early degeneration [15,16]. Femoroacetabular impingement (FAI) results from excessive femoral head coverage, aspherical femoral head, and/or insufficient offset of the femoral head–neck junction and resultant repetitive abutment of the acetabular labral–femoral articulation. FAI is widely accepted as a cause of prearthritic hip disorders, and some investigators postulate that it causes secondary osteoarthritis [17].
Peelle et al [13] studied the radiographs of 78 patients who were treated arthroscopically for labral tears. Forty-nine percent of patients with symptomatic labral tears were found to have at least one radiographic abnormality; 17% occurred at the acetabulum, 14% at the femur, and 18% at both locations. Thirty-six percent of patients had mild hip dysplasia, and 29% had FAI. Controversy still exists regarding the consequence of labral tears alone on the development of osteoarthritis. In several studies, investigators suggest that acetabular labral tears are a precursor to hip arthritis [15,16,18,19], but no study has been performed in which investigators definitively demonstrate that isolated acetabular labral tears without osseous deformity result in early arthritis of the hip.
To date, patient outcomes after treatment of prearthritic hip disorders have been limited to outcomes after surgery [1–4,6–11,20–22]. As a result, comprehensive treatment outside of surgery remains ill-defined. Surgical treatment of prearthritic hip disorders is still evolving and includes a wide array of surgical techniques that are dependent on the presence of structural osseous abnormalities such as DDH or FAI. Only a few researchers have recommended that patients undergo a trial of conservative treatment before surgery [2,4]. The authors of many studies have reported that they believe conservative treatment of labral tears has no utility, and they advocate surgical intervention for all patients with labral tears [1,6,8,20–22]. It is likely that a continuum of care needs to be outlined to help determine which patients have good prognostic indicators for optimal outcomes with conservative care and which patients will do best with surgical intervention.
The purpose of this study is twofold. First, the study will describe characteristics, imaging findings, pain, and function before and after conservative treatment for patients presenting with the clinical indicators of intra-articular hip pain before the onset of osteoarthritis. Second, this study will compare characteristics, pain reports, function, and radiographic findings of patients who did and did not choose surgery to predict which patients respond best to conservative treatment and which patients should have surgery.
MATERIALS AND METHODS
Institutional review board approval at Washington University School of Medicine was obtained before this study was conducted. Adult volunteers between the ages of 18 and 50 years were recruited from an orthopedic department at a tertiary university hospital setting. Recruitment took place at the time of their initial consultation with 1 of 2 physical medicine and rehabilitation physicians (D.H., H.P.) with expertise in prearthritic hip disorders or an orthopedic surgeon (J.C.C.) with expertise in prearthritic hip disorders, joint-preservation surgery, and joint arthroplasty. Patients with clinical indicators of prearthritic, intra-articular hip pain were recruited. These clinical indicators included (1) anterior or lateral hip pain; (2) a history of pain that worsened with activity, pivoting, hip flexion, or weight bearing; (3) pain-associated mechanical symptoms, including popping, clicking, or locking; (4) pain at rest; (5) physical examination findings of reproduction of pain in the groin or lateral hip with the anterior hip impingement test, FABER test, log roll, or resisted straight leg-raise test; and (6) physical examination findings that excluded the spine and other lower extremity disorders as a potential source of pain and dysfunction. Patients who were older than 50 years and had a history of ipsilateral hip surgery, inflammatory arthropathy, hip infection or tumor, current lumbar radiculopathy, existing extra-articular hip disorders, major structural deformity of the hip, or moderate to advanced degenerative disease of the hip (Tönnis classification 2–3) were excluded.
All patients underwent standard radiographic imaging, which included a standing anteroposterior radiograph of the pelvis and hip, frog lateral, cross-table lateral, and false profile views of the hip. An independent, fellowship-trained orthopedic surgeon measured the lateral center edge angle of Wiberg, the alpha angle, the acetabular index, the head neck offset ratio and Tönnis grade for each subject [23–30]. Patients were classified into the following 3 categories on the basis of these radiographic measurements (Table 1) and Tönnis grade assessment: (1) no structural abnormalities, (2) mild DDH, and (3) mild FAI. If the measurements were conflicting, the examiner chose the category on the basis of repeat overall assessment of the radiograph.
Table 1.
Radiographic measurement values
| DDH | Borderline DDH |
Normal | Pincer FAI |
FAI | Borderline FAI |
Normal | |
|---|---|---|---|---|---|---|---|
| Lateral center edge angle of Wiberg | ≤19° | 20°–24° | 25°–35° | ≥36° | |||
| Acetabular index | >10° | 0°–10° | <0° | ||||
| Head neck offset ratio | <0.17 | ≤0.17 | |||||
| Alpha angle | ≥55° | 50°–54° | ≤49° |
DDH = developmental dysplasia of the hip; FAI = femoroacetabular impingement.
A 3-phase treatment protocol was initiated by the examining physician. Phase I treatment focused on conservative interventions, including patient education, activity modification, a directed physical therapy protocol (Table 2), and medications, including anti-inflammatory drugs and narcotics as necessary. On the basis of the findings of Lewis and Sahrmann [31], a basic protocol was distributed with the prescription to the patient’s physical therapist. The physical therapist was asked to follow the protocol but was allowed to individualize the program on the basis of patient-specific physical examination findings. All precautions were to be followed.
Table 2.
Physical therapy protocol
| Precautions |
| No straight leg raise |
| Only pain-free hip range of motion during exercise or functional skills |
| Avoid rotation of acetabulum on femur under load |
| Avoid hip hyperextension during functional skills and exercise activities |
| Avoid anterior translation of femur |
| Goals of therapy |
| Improve precision of hip motion |
| Prevent hip hyperextension with active or passive (standing postures) motion |
| Prevent rotation of acetabulum on femur under load |
| Optimize hamstring length and extensibility; must maintain pain-free hip flexion when lengthening hamstrings |
| Prevent dominance of quadriceps and/or hamstrings |
| Improve performance of iliopsoas, gluteus maximus, gluteus medius, intrinsic hip lateral rotators (if not short), and abdominals |
| Decrease anterior glide of femur with appropriate muscle retraining during active motions and sustained postures |
| Education on day-to-day activity modification |
| Home exercise program |
The goals of physical therapy included educating the patient regarding day-to-day activity modification (eg, getting in and out of a car and sitting ergonomics) and avoidance of aggravating factors (eg, crossing the legs and pivoting). Improving the motion of the femoral head within the acetabulum—specifically, decreasing anterior femoral glide with appropriate muscle retraining and optimizing the balance of muscle strength and length at the pelvis—were key components of the protocol [31].
At 3-month follow-up, if symptoms continued and function remained impaired, patients entered phase II, which included a fluoroscopically guided, diagnostic, intra-articular hip injection (with 4 mL of 1% lidocaine). The Numeric Pain Scale (NPS) score for pain that day was reported by the patient, and provocative hip tests were performed before and within 30 minutes after the injection. A positive response was defined as a patient’s report of ≥50% reduction in pain with the provocative tests and at rest. If a positive response was obtained, a magnetic resonance arthrogram (MRA) of the hip (if one had not been obtained previously) was performed. Patients with continued pain, functionally limiting symptoms, and a surgically amenable lesion were offered the opportunity to enter phase III, which was surgical intervention. Patients with early arthritic changes on radiographs and MRA who did not want surgery were offered a fluoroscopically guided therapeutic hip injection (triamcinolone, 1 mL of 40 mg/mL, and 3 mL of 1% lidocaine) as a means of reducing pain and enhancing participation in therapeutic exercise.
Outcomes were measured by a series of standardized and validated outcome questionnaires for hip disorders to assess pain, function, and quality of life. Questionnaires were completed by the patients at baseline and at 3-month, 6-month, and 1-year intervals. The questionnaires included the NPS, Short Form-12, Modified Harris Hip Score [32,33], Western Ontario and McMaster Universities Osteoarthritis Index [34,35], Nonarthritic Hip Score [36], and Baecke Questionnaire of Habitual Activity [37] (Table 3). The treating physical therapists were asked to record range of motion parameters, NPS, number of sessions attended, and percent compliance with the physical therapy program. Patients who chose conservative treatment alone were monitored for 1 year after the initiation of treatment, whereas patients who elected surgical intervention completed outcome measures at 1 year after surgery.
Table 3.
Outcome measures
| Outcome Measure | Assesment | Scoring |
|---|---|---|
| Numeric Pain Scale | Used to assess pain | 0–10, 0 indicates no pain, 10 indicates the most severe pain |
| Short Form-12 Health Survey | Used to assess the physical and psychological impact of the condition on the patients | 0–100, with a score <50 in each subgroup indicating below-average physical (PCS) and emotional (MCS) function |
| Modified Harris Hip Score | Used to assess the effect of symptoms on daily activities | 0–100, with a greater score indicating better function |
| Western Ontario and McMaster Universities Osteoarthritis Index | Used to assess pain, stiffness and function | 0–96, with a lower score indicating better function |
| Nonarthritic Hip Score | Used to assess functional activities in a young adult population | 0–100, with a greater score indicating better function |
| Baecke Questionnaire of Habitual Activity | Used to assess limitations specific to work, sports, and leisure-related activities | 0–15, with a greater score indicating a more active lifestyle |
PCS = physical health composite; MCS = mental health composite.
Statistical Analyses
Descriptive statistics for reported measures and scatter plots for outliers were completed. Cross-sectional comparisons of measures for patient groups used unpaired t-tests (for continuous measures) and χ2 tests (for categorical measures). When required conditions were not satisfied, the Wilcoxon or Fisher exact test was used as a nonparametric alternative. Logistic regression was used to compare baseline characteristics for patients who chose surgery or did not choose surgery. The change between baseline and 1 year was assessed within groups by paired t-tests. Analysis of covariance was used to compare the 1-year outcomes between groups after adjusting for the baseline value. The data analysis was generated using SAS software (SAS Institute Inc., Cary, NC).
RESULTS
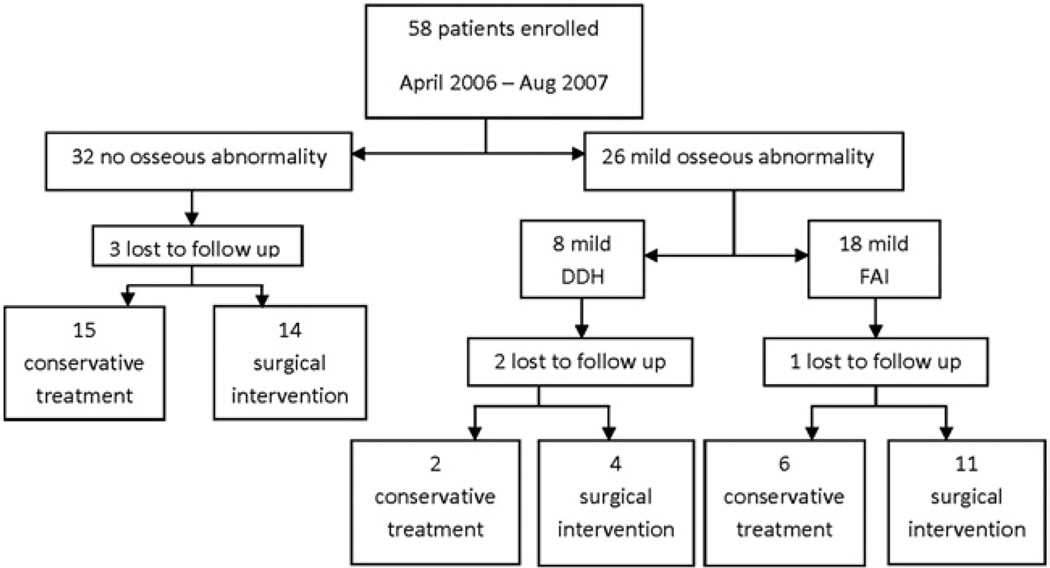
Fifty-eight consecutive patients (49 women and 9 men) with clinical indicators of a prearthritic, intra-articular hip disorder were enrolled between April 2006 and August 2007. Six patients were lost to follow-up or chose not to continue participation in the study before the 3-month follow-up (3 had no osseous deformity, 2 had mild DDH, and 1 had mild FAI; Figure 1). Radiographic evaluation revealed 32 subjects with no structural deformity, 8 subjects with mild hip dysplasia, and 18 subjects with mild FAI. No significant difference in baseline demographics was found between the radiographic classification groups except for gender (Table 4). All subjects with mild hip dysplasia were female (8/8), and 61% of the subjects with mild FAI were female (11/18). Ninety-four percent (30/32) of the no-deformity group were female (P = .007). The gender differences were consistent with previous findings for dysplasia, FAI, and acetabular labral tears [9–11].
Figure 1.
Patient grouping after enrollment: DDH = developmental dysplasia of the hip; FAI = femoroacetabular impingement.
Table 4.
Baseline characteristics by radiographic classification
| Radiographic Classification |
||||
|---|---|---|---|---|
| Baseline Characteristics | No Deformity, n = 32 |
Mild Dysplasia, n = 8 |
Mild FAI, n = 18 |
P Value* |
| Female gender | 30 (94%) | 8 (100%) | 11 (61%) | .007 |
| White race | 27 (84%) | 8 (100%) | 18 (100%) | .15 |
| Age (y) | 35.6 ± 12 | 37.3 ± 7 | 32.9 ± 10 | .56 |
| BMI (kg/m2) | 25.8 ± 7 | 25.4 ± 3 | 25.5 ± 5 | .97 |
| Duration of pain (mo) | 14.9 ± 17 | 28.6 ± 23 | 13.4 ± 10 | .23† |
| Mechanical symptoms | 18 (69%) | 5 (63%) | 13 (72%) | .88 |
| Positive hip impingement test | 24/27 (89%) | 6/6 (100%) | 16/17 (94%) | .999 |
FAI = femoroacetabular impingement; BMI = body mass index.
P value compares groups by Fisher exact test (for categorical variables) or unpaired t-test (for continuous variables).
P value by the Wilcoxon test.
Baseline outcome measures based on radiographic classifications are presented in Table 5. All groups demonstrated a moderate degree of pain (mean NPS of 6.6 ± 2) and impact on psychological and physical well-being, with mean below-average scoring. A significant difference (P = .02) was found in the NPS at baseline between the subjects without deformity (6.6 ± 2) and with deformity (5.4 ± 2). A significant difference (P = .02) also was observed in the baseline Total Baecke Questionnaire Score. Participants without deformity were less active (with a score of 7.4 ± 1) than were participants with deformity (who had a score of 8.3 ± 1), suggesting that subjects with structural osseous deformity had less pain and were more active at baseline.
Table 5.
Baseline outcome measures by radiographic classification
| Baseline Outcome Measures |
No Osseous Deformity n = 32 |
Mild Osseous Deformity n = 26 |
P Value* |
|---|---|---|---|
| Numeric Pain Scale (0–10) | 6.6 ± 2 | 5.4 ± 2 | .02† |
| SF-12 PCS | 39.8 ± 6 | 42.8 ± 7 | .11 |
| SF-12 MCS | 40.5 ± 7 | 40.7 ± 9 | .93 |
| Harris Hip total score | 63.6 ± 13 | 66.2 ± 10 | .41 |
| WOMAC total score | 30.5 ± 18 | 26.5 ± 15 | .38 |
| Nonarthritic hip score | 62.5 ± 14 | 68.4 ± 13 | .11 |
| Baecke questionnaire total score | 7.4 ± 1 | 8.3 ± 1 | .02 |
SF-12 PCS = physical composite subscore; SF-12 MCS = mental health composite subscore; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
P value between groups by unpaired t-test unless otherwise indicated.
P value by the Wilcoxon test.
Ninety-four percent (49/52) of the subjects received physical therapy, with an average of 6.4 physical therapy sessions and a range of 1 to 19 sessions. Three patients chose not to participate in additional physical therapy upon evaluation because they had undergone a trial of physical therapy before presenting to the examiner. All 3 of these patients had early arthritic changes (Tönnis grade I) on radiographs and were educated on relative rest and activity modification and underwent a trial of anti-inflammatory medication. These patients also chose to receive a fluoroscopically guided intra-articular injection of 40 mg of triamcinolone with 3 mL of lidocaine as a method of modifying pain. At 3-month follow-up, 14 patients were satisfied with their conservative treatment outcome and did not require any further intervention.
Thirty-eight subjects (73%) progressed to phase II of treatment, which included a fluoroscopically guided hip injection and/or MRA. Diagnostic hip injections were performed in 21 of 38 patients in whom the diagnosis of an intra-articular problem was still in question or to confirm an intra-articular etiology before progressing to MRA or surgery. Eighty-six percent of subjects (18/21) had a positive provocative test preinjection followed by a negative provocative test after injection, indicating that their pain had an intra-articular source. Of the 3 subjects with a negative response, 2 had labral tears on MRA and underwent arthroscopy for labral debridement, and the remaining subject underwent surgical repair for FAI.
During phase II, 35 of 38 subjects had an MRA. Three subjects declined further imaging; 2 had a previous magnetic resonance imaging scan that indicated a labral tear, and 1 underwent a diagnostic hip injection with a positive response. All subjects who had an MRA were found to have an intra-articular abnormality. Acetabular labral tears were found in 25 of 35 subjects; in addition, 6 had both labral tears and chondral abnormalities, 4 had only chondral abnormalities, and 2 had mild FAI without labral or chondral abnormality.
Twenty-nine subjects (56%) progressed to phase III and had surgery to repair or debride a labral tear or chondral abnormality with or without surgical correction of an osseous deformity. The latter included periacetabular osteotomies or femoral osteochondroplasty, depending on the extent of the deformity. One of the 29 subjects taken to surgery had only chondral abnormalities on the femoral and acetabular side without a labral tear or structural osseous abnormality. The time from study enrollment to surgery was a mean of 154 days (range, 39–483 days) for subjects with no osseous abnormality, 256 days (151–344 days) for the mild dysplasia group, and 121 days (76–223 days) for the mild FAI group.
Twenty-three subjects (44%) were satisfied with the results of conservative treatment and did not pursue surgical intervention. Fourteen of these subjects did not progress to phase II (MRA and/or diagnostic image-guided hip injection). They improved and were satisfied with the results of conservative care. Nine of these subjects progressed to phase II, and all subjects had a positive diagnostic hip injection and an intra-articular abnormality confirmed by MRA. These 9 subjects remained in the conservative treatment arm of the study and did not choose to pursue surgery.
No statistically significant difference was found between baseline demographics or physical examination findings between the nonsurgical and surgical groups (Table 6). The presence of a structural deformity did not increase the likelihood of a subject to choose surgery. Fifty-two percent of the surgery group had a structural abnormality, and 35% of the nonsurgical group had a structural abnormality. However, this trend was not statistically significant. Participants who chose to have surgery were more active at baseline (the Baecke total score for the nonsurgical group was 7.4 ± 1, whereas the Baecke total score for the surgical group was 8.4 ± 1, P = .02). The adjusted odds ratio was 1.89 with a 95% confidence interval from 1.11–3.22. No other statistical differences were found between their baseline pain and functional outcome measures.
Table 6.
Baseline characteristics of surgical and nonsurgical groups
| Surgery |
||||
|---|---|---|---|---|
| Baseline Characteristics |
No n = 23 |
Yes n = 29 |
P Value* | Unadjusted OR (95% CI) |
| No deformity | 15 (65%) | 14 (48%) | .22 | |
| Borderline deformity | 8 (35%) | 15 (52%) | ||
| Female | 21 (91%) | 27 (79%) | .28† | |
| Age (y) | 32.8 ± 11 | 35.8 ± 11 | .30 | |
| BMI (kg/m2) | 25.3 ± 7 | 25.9 ± 5 | .70 | |
| Duration of pain (mo) | 17.4 ± 21 | 16.1 ± 14 | .79 | |
| Numeric Pain Scale, 0–10 | 7.22 ± 2.5 | 6.75 ± 2.2 | .47 | |
| SF-12 PCS | 42.2 ± 7 | 40.2 ± 7 | .30 | |
| SF-12 MCS | 40.2 ± 8 | 40.6 ± 8 | .87 | |
| Nonarthritic hip score | 67.3 ± 14 | 63.3 ± 14 | .32 | |
| Baecke total score | 7.35 ± 1.2 | 8.40 ± 1.4 | .02 | 1.89 (1.11–3.22) |
OR = odds ratio; CI = confidence interval; BMI = body mass index; SF-12 PCS = physical composite subscore; SF-12 MCS = mental health composite subscore.
P value compares groups by logistic regression predicting surgery. Unadjusted ORs reflect the increased odds of undergoing surgery for a 1-unit increase in the variable and are reported when the P value is significant.
P value by exact logistic regression.
At 1 year follow-up (from enrollment for the nonsurgical group and from surgery for the surgical group), both groups had statistically significant and equal improvement in all outcome measures (Table 7). Both groups also had a significant decrease in activity (P = .0003 for the nonsurgical group and P = .0006 for the surgical group), as indicated by a decrease in the total Baecke score.
Table 7.
One-year outcomes between surgical and nonsurgical groups
| Outcome Measure | Baseline | 12 Mo |
P Value Within Groups* |
P Value Between Groups† |
|---|---|---|---|---|
| Numeric Pain Scale (0–10) | ||||
| Surgical group | 5.6 ± 3 | 2.8 ± 3 | .0002‡ | |
| Nonsurgical group | 6 ± 3 | 3.3 ± 3 | .0001‡ | .67‡ |
| Harris Hip score | ||||
| Surgical group | 61.3 ± 13 | 81.1 ± 17 | <.0001 | |
| Nonsurgical group | 69.4 ± 11 | 78.9 ± 14 | .006 | .45 |
| WOMAC | ||||
| Surgical group | 29.2 ± 16 | 15.3 ± 16 | .008 | |
| Nonsurgical group | 25.1 ± 17 | 13.5 ± 14 | .001 | .91 |
| Baecke questionnaire | ||||
| Surgical group | 8.5 ± 1 | 7.9 ± 1 | .006 | |
| Nonsurgical group | 7.4 ± 1 | 6.9 ± 1 | .002 | .48 |
| SF-12 PCS | ||||
| Surgical group | 39.7 ± 7 | 48.0 ± 9 | .0001 | |
| Nonsurgical group | 42.7 ± 9 | 47.6 ± 9 | .08 | .53 |
| SF-12 MCS | ||||
| Surgical group | 40.8 ± 8 | 48.1 ± 10 | .003 | |
| Nonsurgical group | 38.3 ± 8 | 45.1 ± 8 | .03 | .42 |
| Nonarthritic hip score | ||||
| Surgical group | 63.2 ± 14 | 76.7 ± 19 | .005 | |
| Non-surgical group | 70.4 ± 12 | 81.6 ± 12 | .0006 | .77 |
WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; SF-12 PCS = physical composite subscore; SF-12 MCS = mental health composite subscore.
Within groups P value by paired t-test.
Between groups P value by analysis of covariance.
Data rank-transformed prior to analysis.
DISCUSSION
This study is the first to report outcomes of comprehensive conservative care of patients with clinical indicators of prearthritic, intra-articular hip pain and the first to compare characteristics, pain, and functional outcomes of patients who chose conservative care and of patients who chose surgical intervention. All patients treated with either conservative treatment alone or with conservative treatment followed by surgery demonstrated significant improvement in pain and function from baseline to 1-year follow-up. Within this population, 44% of patients were successful in improving their function and decreasing their pain with conservative measures, and 56% chose surgical intervention. The presence of subtle osseous abnormalities such as borderline or mild DDH or FAI did not predict the failure of conservative treatment or the choice of surgical intervention. The only predictor of surgical intervention was the subjects’ baseline activity level. Subjects with higher baseline activity scores were more likely to choose surgery.
Interestingly, both the conservative and surgical groups demonstrated an overall decrease in activity at 1-year follow-up with a corresponding decrease in pain and improvement in function. This finding may be a reflection of the educational information given to all patients enrolled in this study, as well as counseling and observation of pain-relieving hip and postural position changes discussed by the physical therapist. Future studies that measure patient compliance regarding activity modification and therapeutic exercise would best determine the impact of activity modification in this patient population. Further follow-up is necessary to see if this trend continues for both groups. Current literature supports continued improvement in function and pain in patients undergoing hip arthroscopy with debridement or repair of labral tears or open procedures for DDH and FAI at 2-year follow-up and 5-year follow-up [38,39]. No long-term studies of outcomes for conservative treatment for patients with clinical indicators of prearthritic hip disorders are available. The lack of long-term follow-up is a limitation of this study.
This study has several limitations. AnMRAwas not obtained for all patients in the study; therefore, a structural diagnosis or specific pathological finding was not objectively identified in all patients. This approach mimics our clinical practice but does not produce a homogeneous study population based on a structural diagnosis. Instead, we focused on a specific patient population with specific clinical indicators of intra-articular hip pain (ie, anterior groin or lateral hip pain and a positive provocative hip test) with the goal of improving cost-effective and appropriate clinical practice. Twenty-seven percent of patients (14/52) who completed the study were satisfied with their results, had improved outcome measures, and did not require costly imaging beyond standard radiographs. Activity modification, medications for pain reduction, and physical therapy were the primary interventions. Only 3 patients chose an intra-articular injection to manage pain. These data suggest that it may not be necessary to obtain an MRA for every patient who initially presents with clinical indicators of prearthritic intra-articular hip disorders and that an MRA may be needed only if the initial conservative measures fail.
Another limitation of this study is the variability of the number of physical therapy sessions attended by subjects. Ninety-four percent of subjects completed a trial of physical therapy, with the primary focus on educating the participant regarding day-to-day activity modification (eg, getting in and out of a car and sitting ergonomics) and avoidance of aggravating factors (eg, crossing legs and pivoting), as well as improving the motion of the femoral head with in the acetabulum, specifically by decreasing anterior femoral glide [31]. The range of therapy visits was 1 to 19, with an average of 6.4 visits. Although one visit does not represent a full course of therapy, a significant part of the protocol focuses on education and activity modification, which could be accomplished in one visit. The patients were given a specific protocol; however, we were unable to control for potential deviations because patients went to varying physical therapy facilities. The physical therapy protocol used remains a difficult aspect of the study to objectively qualify and measure and illustrates one of the difficulties of studying conservative treatment. Further biomechanical analysis is needed to ascertain why 44% of the subjects improved with this minimal intervention.
A third limitation is the small patient sample size. One specific aim of the study was to determine whether structural abnormalities were associated with a poorer response to conservative treatment. We did not see a correlation of osseous structural abnormality with the patient’s choice of surgical treatment [1].Wewere only able to analyze the osseous abnormality group compared with the normal structure group because the sample sizes were too small to specifically analyze the subgroups of borderline or mild DDH or FAI. This inability to analyze subgroups remains a limitation of the study because these 2 subgroups are distinct in their clinical presentation, hip pathomechanics, and treatment modalities.
Fourth, the surgeon could potentially influence the patient’s decision to choose surgery. When the patient determined the he or she was not satisfied with the results of comprehensive conservative treatment and an MRA and radiographs identified a surgically amendable structural abnormality, surgical options were discussed. All patients in this study who opted for a surgical consult were evaluated by the senior author (J.C.), who routinely counsels patients regarding options, risks, and benefits of surgical treatment. Although the goal of returning to a high level of activity is discussed, this outcome is not guaranteed, and patients are counseled that the goal of surgery is to return the patient to usual activities of daily living with reduced pain and improved function. Despite this approach, physician influence could remain a factor in the patient’s decision to choose surgery.
Finally, the data show that the more active a subject was, the more likely he or she was to choose surgery. This finding was only seen on the Baecke questionnaire of physical activity. This finding may be a result of suboptimal outcome measures available to study this young, active population. More sensitive hip outcome measures for activity and function are needed. Also, with larger numbers, we may have been able to answer questions related to subgroups of interest such as very active subjects versus sedentary subjects, specific athletic populations, or age-dependant variables.
CONCLUSION
This study is the first to report outcomes of comprehensive, conservative care of patients with clinical indicators of prearthritic, intra-articular hip pain. Patients were more commonly women (85%), although the subgroup of patients with FAI had a higher percentage of men (39% compared with 15% in the total cohort). No differences were found between the conservative treatment alone and surgical groups with regard to their baseline pain and function with the exception of the Baecke activity score. Subjects who eventually chose surgical intervention were more active at baseline (P = .02). The degree or presence of deformity was not found to correlate with the subject’s choice to proceed to surgery. Subjects treated with conservative treatment alone and with conservative treatment followed by surgery for signs and symptoms of prearthritic, intra-articular hip disorders demonstrated significant improvement from baseline to 1-year follow-up. Forty-four percent of subjects were satisfied with the results of conservative measures and did not choose to pursue surgical intervention. This finding is an important addition to the literature because before this study, many hip experts had concluded that no role exists for conservative treatment. Our data suggest that a trial of conservative management for patients presenting with clinical indicators of prearthritic, intra-articular hip disorders should be considered before engaging in surgical intervention. Longer-term follow-up studies are needed to document the lasting effects of conservative treatment.
ACKNOWLEDGMENTS
We acknowledge the work of Nancy J. Bloom, PT, DPT, MSOT, and Shirley A. Sahrmann, PT, PhD, who provided input regarding the physical therapy protocol.
D.H.
Disclosure: 8A, 2007 Scott F. Nadler, DO, research grant, Physiatric Association of Spine, Sports and Occupational Rehabilitation (PASSOR)
H.P.
Disclosure: 8A, 2010 Scott F. Nadler, DO, research grant, Foundation of PM&R; 8A, 2010–2011 ICTS JIT Core Usage Funding RFA Research Design and Biostatistics Group; 9A, secretary, NASS Board of Directors, PM&R senior editor, Spineline editor
M.H.H.
Disclosure: 7B, NIH-NICHD/NCMRR (K12 HD055931; 1 K23 HD067343-01), NIH-NCRR (1 UL1 RR 024992-01)
J.C.C.
Disclosure: 2A, Biomet; 7B, Zimmer, Wright Medical; 8B, OREF, OMeGA, NFL, Hip Society
Footnotes
Peer reviewers and all others who control content have no relevant financial relationships to disclose
Disclosure Key can be found on the Table of Contents and at www.pmrjournal.org
Contributor Information
Devyani Hunt, Physical Medicine and Rehabilitation, Department of Orthopaedic Surgery, Washington University School of Medicine, One Barnes Jewish Hospital Plaza, Suite 11300, Campus Box 8233, St. Louis, MO 63110.
Heidi Prather, Physical Medicine and Rehabilitation, Department of Orthopaedic Surgery, Washington University School of Medicine, St. Louis, MO.
Marcie Harris Hayes, Program in Physical Therapy, Washington University School of Medicine, St. Louis, MO.
John C. Clohisy, Department of Orthopaedic Surgery, Washington University School of Medicine, St. Louis, MO.
REFERENCES
- 1.Byrd JW. Hip arthroscopy: Surgical indications. Arthroscopy. 2006;22:1260–1262. doi: 10.1016/j.arthro.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Clohisy JC, Keeney JA, Schoenecker PL. Preliminary assessment and treatment guidelines for hip disorders in young adults. Clin Orthop Relat Res. 2005;441:168–179. doi: 10.1097/01.blo.0000193511.91643.2a. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgerald RH., Jr Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res. 1995;311:60–68. [PubMed] [Google Scholar]
- 4.Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2:105–117. doi: 10.1007/s12178-009-9052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keeney JA, Peelle MW, Jackson J, Rubin D, Maloney WJ, Clohisy JC. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004;429:163–169. doi: 10.1097/01.blo.0000150125.34906.7d. [DOI] [PubMed] [Google Scholar]
- 6.McCarthy J, Noble P, Aluisio FV, Schuck M, Wright J, Lee JA. Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orthop Relat Res. 2003;406:38–47. doi: 10.1097/01.blo.0000043042.84315.17. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy JC, Lee JA. Arthroscopic intervention in early hip disease. Clin Orthop Relat Res. 2004;429:157–162. doi: 10.1097/01.blo.0000150118.42360.1d. [DOI] [PubMed] [Google Scholar]
- 8.Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: A systematic review of the literature. Clin Orthop Relat Res. 2007;455:88–92. doi: 10.1097/BLO.0b013e31802c7e0f. [DOI] [PubMed] [Google Scholar]
- 9.Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457. doi: 10.2106/JBJS.D.02806. [DOI] [PubMed] [Google Scholar]
- 10.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nunley RM, Prather H, Hunt D, Schoenecker PL, Clohisy JC. Clinical presentation of symptomatic acetabular dysplasia in skeletally mature patients. J Bone Joint Surg Am. 2011;93(Suppl 2):17–21. doi: 10.2106/JBJS.J.01735. [DOI] [PubMed] [Google Scholar]
- 12.Prather H, Hunt D, Fournie A, Clohisy JC. Early intra-articular hip disease presenting with posterior pelvic and groin pain. PM R. 2009;1:809–815. doi: 10.1016/j.pmrj.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Peelle MW, Della Rocca GJ, Maloney WJ, Curry MC, Clohisy JC. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333. doi: 10.1097/01.blo.0000181147.86058.74. [DOI] [PubMed] [Google Scholar]
- 14.Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–150. doi: 10.1097/01.blo.0000136903.01368.20. [DOI] [PubMed] [Google Scholar]
- 15.Dorrell JH, Catterall A. The torn acetabular labrum. J Bone Joint Surg Br. 1986;68:400–403. doi: 10.1302/0301-620X.68B3.3733805. [DOI] [PubMed] [Google Scholar]
- 16.Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120–1129. doi: 10.2106/JBJS.G.00144. [DOI] [PubMed] [Google Scholar]
- 17.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH, Bourne RB, Oh I. Intra-articular acetabular labrum: A possible etiological factor in certain cases of osteoarthritis of the hip. J Bone Joint Surg Am. 1979;61:510–514. [PubMed] [Google Scholar]
- 19.Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232–240. doi: 10.1097/00003086-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 20.Hickman JM, Peters CL. Hip pain in the young adult: Diagnosis and treatment of disorders of the acetabular labrum and acetabular dysplasia. Am J Orthop (Belle Mead NJ) 2001;30:459–467. [PubMed] [Google Scholar]
- 21.Kelly BT, Williams RJ, 3rd, Philippon MJ. Hip arthroscopy: Current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 22.Safran MR. The acetabular labrum: Anatomic and functional characteristics and rationale for surgical intervention. J Am Acad Orthop Surg. 2010;18:338–345. doi: 10.5435/00124635-201006000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 24.Stulberg SD, Harris WH. Proceedings of the Second Open Scientific Meeting of the Hip Society. St. Louis, MO: Mosby; 1974. Acetabular dysplasia and development of osteoarthritis of the hip. [Google Scholar]
- 25.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;58(Suppl):5–135. [Google Scholar]
- 26.Beaule PE, Zaragoza E, Motamedi K, Copelan N, Dorey FJ. Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2005;23:1286–1292. doi: 10.1016/j.orthres.2005.03.011.1100230608. [DOI] [PubMed] [Google Scholar]
- 27.Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669–675. doi: 10.1016/j.arthro.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 29.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 30.Tannast M, Siebenrock KA. Conventional radiographs to assess femoroacetabular impingement. Instr Course Lect. 2009;58:203–212. [PubMed] [Google Scholar]
- 31.Lewis CL, Sahrmann SA. Acetabular labral tears. Phys Ther. 2006;86:110–121. doi: 10.1093/ptj/86.1.110. [DOI] [PubMed] [Google Scholar]
- 32.Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 33.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 34.Bellamy N, Buchanan WW. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol. 1986;5:231–241. doi: 10.1007/BF02032362. [DOI] [PubMed] [Google Scholar]
- 35.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 36.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: Reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. doi: 10.1097/01.blo.0000043047.84315.4b. [DOI] [PubMed] [Google Scholar]
- 37.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 38.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: A systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052. doi: 10.1007/s11999-009-0842-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: A systematic review of the literature. Clin Orthop Relat Res. 2010;468:555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]