Abstract
Although the hematopoietic stem cell (HSC) niche has been an active area of study, the concept of the bone marrow microenvironment (BMM) harboring a niche for solid metastatic tumor cells has only recently been considered. The HSC niche and microenvironment that is thought to constitute the solid tumor niche share many of the same structural and functional components, suggesting the possibility that the HSC and tumor niche are one in the same. The osteoblast is a critical component for each of these niches, and is important for regulating cellular processes such homing and migration, growth and survival, and quiescence and dormancy. Current understanding of the HSC niche may provide more insight to better defining the solid tumor niche. As role of the niche in regulating these processes is better understood, new insights to the role of the BMM in metastatic disease may be gained, and provide more potential targets for therapy.
Keywords: niche, bone marrow microenvironment, hematopoietic stem cell, metastasis, disseminated tumor cell
2. INTRODUCTION
In 1889, Stephen Paget observed distinct metastatic patterns of 735 breast cancer patients. He found that breast cancer had a high propensity to spread to certain secondary sites, such as the marrow, while growth in other secondary sites was less common. This led him to famously state that metastatic cells, or “seeds”, must fall on “congenial soil” (1). Paget was among the first to propose that the bone marrow must have specific factors conducive to metastatic growth. The concept of a specialized cellular “niche” was then proposed in 1978 by Richard Schofield when he observed that parenchymal cells in association with a stem cell can affect and determine stem cell behavior (2). Today, the concept of a stem cell niche is better understood, yet remains an active area of investigation (3–5). Likewise, the microenvironment of secondary growth and metastasis in epithelial tumors is a rapidly expanding field of research, but only recently has this microenvironment been considered in the context of a solid tumor niche (6). Primary tumors are known to interact with a diverse population of non-malignant cells, forming a tumor ecosystem (7). This ecosystem interaction is also observed in the bone marrow, a secondary site in which many types of metastatic tumor cells take up residence. This bone marrow ecosystem plays a significant role in regulating the activity of metastatic tumor cells (8), similar to the way the hematopoietic stem cell niche regulates stem cell activity. In this review, we will discuss the regulatory factors of the bone marrow microenvironment (BMM) that potentially comprise a niche for metastatic solid tumor cells.
2.1 The HSC niche
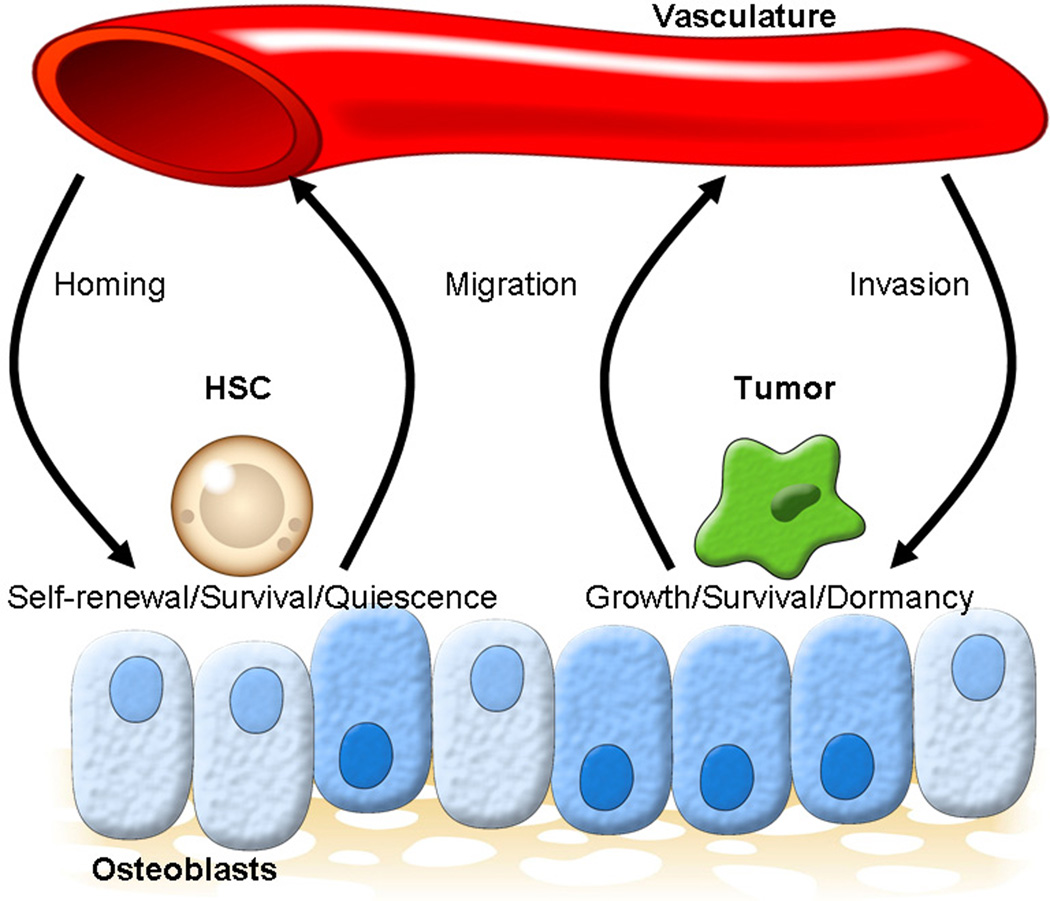
Interactions between hematopoietic stem cells (HSCs) and their bone marrow niche serves as a paradigm for how cancer cells may interact with their microenvironment. Metastases from several types of solid tumors, including prostate cancers, use similar pathways to home to and take up residence in the bone (9). The BMM has long been known to regulate the activity of HSCs. HSCs are retained in the bone marrow until maturation, whereupon they are then released into circulation. The population of supportive cells that facilitate HSC retention bone marrow is what is known as the HSC niche. The HSC niche believed to be responsible for regulating activities that allow an HSC to retain its multipotency, engage in self-renewal, and regulate quiescence, proliferation, and differentiation. In homeostasis, HSCs are found in the endosteum of bone, where they transition to a state of quiescence to protect their long-term self-renewing capabilities (4). This “endosteal niche” is believed to be regulated mainly by osteoblasts and maintain HSC quiescence (Figure 1), yet the precise location and phenotype of these niche cells remains to be determined. HSCs have also been detected adjacent to sinusoidal endothelial cells in the “vascular niche”, where proliferation and differentiation of HSCs is regulated (10).
Figure 1.
refer to figure1.gif. The hematopoietic stem cell niche and the solid tumor niche in marrow.
The hematopoietic stem cell (HSC) niche provides insight to the structure and function of the solid tumor niche. The HSC niche regulates homing, self-renewal and quiescence to preserve the multipotency of the HSCs. Likewise, the solid tumor niche probably regulates invasion, survival, and dormancy to allow a metastatic cell to acclimate to the bone marrow microenvironment (BMM). In both cases, adhesion to the osteoblasts is critical.
2.2 Metastatic tumor cells in the bone marrow microenvironment (BMM)
For most solid tumors, the lymph nodes, lung, liver, bone, adrenal, kidney and brain are believed to be the common sites of metastasis (11). However, the bone marrow is also appreciated as a common site for solid tumors to metastasize (11, 12). Although bone marrow metastases are considered a a subform of the bone metastases, growing evidence suggests that bone marrow involvement may represent a a precondition for bone metastasis (12). As a rich vascular bed with terminal sinusoidal endothelium and abundant growth factors, the BMM is also host to metastatic tumor cells. Tumor cells can survive in the bone marrow as overt, clinically detectable metastases, or as micrometastases, which may be composed of a single cell or small population of cells. For a tumor cell to metastasize, it must first leave the primary tumor and cross through the surrounding tissue to gain access to peripheral circulation. After entering circulation, the cell must then cross the vascular barrier and invade extravascular tissues to access a secondary site (6). If a cell can manage to survive through this process and lodge in a secondary site, such as the bone marrow, it can either proliferate into an overt metastatic growth or become dormant until proliferation is possible (13). Successful metastasis requires the ability of tumor cells to survive in many different environments, yet the microenvironment of the bone marrow is the most conducive to metastatic outgrowth, as this is where the majority of overt metastases are present.
Single metastatic cells that lodge in a secondary site are known as disseminated tumor cells (DTCs). In the bone marrow, DTCs derived from epithelial cancers including prostate, breast, gliomas and gastrointestinal cancer have been detected (14–17). In theory, DTCs can become overt and clinically relevant metastases (16), and lead to disease recurrence, where these cells begin proliferating even after treatment (18). Importantly, DTCs have been shown to express genetic heterogeneity, implying that the populations of cells that clonally expand into overt metastases are selected early in the dissemination process (17). This selection of viable DTC populations may be environmentally directed by pressures from the BMM. The presence of DTCs in the bone marrow has been correlated with a poor prognosis (19), as DTCs frequently lead to lethal bone metastases (20).
2.3 Priming or parasitism?
As observed by Paget and modern researchers alike, the distribution of metastatic cells in the bone marrow is highly specific (21–23), and only a tiny population of disseminated tumor cells is able to take up residence to survive. It is not completely understood whether an invading tumor cell dictates the location of its new home by first altering the secondary site to prepare it for metastasis, thus effectively establishing a pre-metastatic niche (24), or if it takes over an area that is already conducive to growth and survival, such as the HSC niche (6). Evidence exists for both the establishment of a pre-metastatic niche and for molecular parasitism of the HSC niche. While these are differing concepts of how a migratory tumor cells selects its niche in the bone marrow, they are not exclusive, and may be different steps in the complex process of tumor cell invasion of the marrow.
A particularly interesting set of findings relates to observations that demonstrate that primary tumors in some fashion appear to prepare or prime select tissues for metastasis (25). The most defined of these interactions have demonstrated that hematopoietic bone marrow progenitors expressing vascular endothelial growth factor receptor-1 (VEGFR-1) home to distinct sites in the bone marrow and cluster before the arrival of metastatic tumor cells (24). By some mechanism which remains unclear, these early arriving hematopoietic cells are thought to prime areas of the bone marrow for the arrival of a tumor cell, suggesting that a pre-metastatic niche is constructed by non-malignant cells (24). The phenotype of these cells is not very different from that of early hematopoietic bone marrow progenitors such that, hematopoietic progenitors and perhaps HSCs themselves unwittingly prime the bone marrow for metastatic growth when they are in close proximity to their niche. In this sense, the HSC niche may participate or serve as a target for metastasis. As a result of these observations and in light of findings that homing, adhesive, and regulatory mechanism of invading tumor cells mimic closely with functions normally ascribed to HSCs, our group recently proposed that invading tumor cells are able to take over and parasitize the HSC niche in order to facilitate their own growth (6). As an entity, the HSC niche is a dynamically involved in and responds to the needs of the cell which it is hosting. In this review, we will focus on the structure and function of the endosteal niche as regulator of HSC activity and target for parasitism of metastatic tumor cells.
3. STRUCTURE OF THE NICHE
Both HSCs and metastatic cells localize to the endosteum in trabecular bone with a high propensity. The metastatic BMM is composed of many cells that are critical to regulating solid tumor metastasis. At present the niche which serves as a basis for metastases from solid tumors is thought to be comprised of components of the extracellular matrix, cells anchored in the bone, infiltrating and migratory cells, and both soluble and insoluble factors (6). Cells found within the BMM include mesenchymal cells, such as mesenchymal stem cells, osteoblasts, fibroblasts, reticular cells, and adipocytes. Mesenchymally derived cells are believed to provide for the physical structural of the niche (6). Cells of hematopoietic origin also play a prominent role in the bone marrow ecosystem, and include hematopoietic stem cells, macrophages, T and B lymphocytes, megakaryocytes, dendritic cells, and osteoclasts (7). Soluble factors critical to niche function consist of oxygen, chemokines and cytokines, growth factors, hormones, and nutrients. Insoluble factors include components found in the calcified bone matrix, such as collagen and pyrophosphate (3, 7). Solid tumor cells invading the bone microenvironment are known to locate in close proximity with these elements, and interact with them in order to modify and optimize the complex ecosystem that develops to form a niche that supports dormancy in some cases, and growth in others.
3.1 Osteoblasts
Osteoblasts are a major regulatory component of the endosteal niche. They are mesenchymal in origin, and their main role in the BMM is to synthesize the extracellular matrix of bone. They have been demonstrated to play critical role in regulation of hematopoiesis (3) and formation of the HSC niche (3, 4). Their specific role in tumor metastasis is now becoming better understood (6, 22). Recent studies also show that osteoblasts are also thought to serve as a major niche component for leukemia cells and their stem cells (6, 26–28) (Figure 1).
In homeostasis, osteoblasts produce a multitude of growth factors and cytokines, such as insulin-like growth factors (IGF), bone morphogenic proteins (BMP), transforming growth factor (TGF)-beta, fibroblast growth factors (FGF) (29, 30). Importantly, osteoblasts are also a major source of CXCL12, or SDF-1, a critical molecule in HSC and tumor engraftment to the niche (9, 31, 32). As a component of the HSC niche, cellular adhesion to osteoblasts (opposed to only the extracellular matrix) is required to maintain HSCs (33). In addition, osteoblasts have been shown to secrete soluble factors only when HSCs are present, and do not secrete the factors when HSCs are absent, perhaps in order to keep HSCs quiescent (3). These factors include interleukin (IL)-6, IL-7 (32), macrophage inflammatory protein (MIP)-1-alpha and leukemia inhibitory factor (LIF) (34). Activation of osteoblasts through the PTH/PTHrP receptors by parathyroid hormone (PTH) and parathyroid hormone related protein (PTHrP) has been shown to expand HSC numbers (35). Ablating osteoblasts in vivo severely alters hematopoiesis (36).
The rich supply of growth factors secreted by osteoblasts is thought to promote tumor growth in metastatic cancer (37). When present in the BMM, breast and prostate (37) cancer cells are known to stimulate osteoblasts to produce factors that stimulate tumor growth and even inhibit osteoblast apoptosis. Among numerous other factors, PTHrP are produced by cancer cells to promote an osteoblastic phenotype in metastatic cancer by increasing the number of osteoblasts present (37). If osteoblasts play the same critical support role in the solid tumor niche as they do in the HSC niche, metastatic cancers may possibly be utilizing the PTH/PTHrP axis to effectively induce more niche cells. The increased number of niche cells may then increase the growth factors and molecules critical for tumor cell survival. Complete molecular characterization of the osteoblastic or endosteal niche is an ongoing area of investigation, and more study is necessary to define the solid tumor niche in the bone marrow. Characterization of the HSC osteoblastic niche is still an active area of debate; for instance, the role of N-cadherin as an osteoblastic niche marker is ambiguous (35, 38). Considering the fact that osteoblasts are a heterogeneous population it is likely that not all osteoblasts exhibit niche capabilities, but only a small subset of specialized cells (39). In fact, what defines an osteoblast that functions with niche capacity remains unclear, as do the markers that will be needed to delineate these activities.
3.2 The extracellular matrix and other marrow cells
Osteoblasts are not the sole supportive cells that make up the HSC and solid tumor niche. The extracellular matrix of bone provides structural support for cells both occupying the niche and creating the niche. It is comprised of fibronectin and integrins to which HSCs and tumor cells can bind. Mesenchymal stem cells (MSCs) are residents of a normal marrow, and tumor cells appear to have several important interactions that have only recently come to light. Primary tumor cells recruit MSCs from the bone marrow through vascular endothelial growth factor (VEGF), stromal derived factor-1 (SDF-1), and monocyte chemotactic protein-1 (MCP-1) (40, 41). Once these MSCs arrive at the primary tumor site, the possibility exists that they may differentiate into cancer-associated fibroblasts (CAFs) and thus contributes to the primary tumor microenvironment.
MSCs in the marrow also produce a multitude of growth factors that can be utilized by migratory tumor cells once they take up residence in the secondary growth site of the marrow (42). In the marrow, MSCs may differentiate into fibroblasts and support tumor cell proliferation at the metastatic site (43). VEGFR1-positive cells, such as those that prime the pre-metastatic niche, can induce fibronectin expression by fibroblasts, which in turn enhances tumor cell binding at secondary sites (43). Modified TGF-beta expression in microenvironment fibroblasts and endothelial cells also plays a role in regulating tumor growth (44). Macrophages derived from the bone marrow can contribute to angiogenesis, invasion, and metastasis, and are termed tumor-associated macrophages (TAMs) (8). TAMs are not normally present in the BMM, but are often found in the marrow at secondary sites of metastasis, where they are considered an invasive species like the tumor cell (7). Endothelial cells in the BMMprovide a vascular niche for hematopoetic stem cells in normal physiology (4), but contribute to angiogenesis and vasculature development of metastatic outgrowths in the tumor BMM (7). In addition, other hematopoietic cells such as T and B lymphocytes, dendritic cells, megakaryocytes, neutrophils, and eosinophils all are present in the BMM and may contribute to the regulation of cells occupying the bone marrow niche (7).
3.3. Osteoclasts
Osteoclasts are critical in the hematopoietic microenvironment. Osteoclasts are multinucleated cells formed from fused monocytes, and require activation using the receptor activator of nuclear factor kappa-beta (RANK) ligand (and macrophage colony-stimulating factor (M-CSF). Osteoclasts are responsible for degrading the calcified organic bone matrix, a process known as bone resorption. Recent studies suggest that osteoclasts may interact with cells occupying the HSC/solid tumor niche both directly and indirectly. Osteoclasts mediate HSC activity by mobilizing them out of the niche, where they can proliferate and differentiate (45). It is possible that osteoclast-induced mobilization may also open HSC the niche for parasitic tumor cells. Direct and indirect cross-talk between osteoclasts and tumor cells is well known and thought responsible for much of the bone resorption exhibited by metastatic tumors with an osteolytic phenotype (37). Inhibition of osteoclastic activities by bisphosphonates is currently one of the few effective methods used today to treat skeletal metastases (46). Osteoclasts make the BMM much more conducive to tumor growth (47), as resorbing bone is much more susceptible to metastasis (37), more adhesive (48), and results in more pronounced chemotaxis (49). In addition, osteoclasts release the growth factors from the calcified bone matrix, which in turn increases proliferation of tumor cells (50).
4. FUNCTION OF THE NICHE
In addition to being structurally defined, the HSC and solid tumor niche is also functionally defined. Aside from regulating self-renewal and stem cell differentiation, the HSCs also regulates homing, adhesion, survival, and quiescence. Parallel to the HSC niche, the solid tumor niche regulates migration, adhesion, survival and growth, and tumor dormancy. Many of the molecular mechanisms and pathways that have been established as HSC-niche interactions are believed to represent similar tumor cell-niche interactions. Although there are differences in tumor and stem cell biology, and further investigation is necessary, there are shared functional relationships that are believed to facilitate tumor cells to “hijack” the pathways used by HSCs and parasitize the niche (6).
4.1 Homing, migration and retention
The ability to target and localize to the niche is critical to metastatic tumor cells. Many of the molecular pathways used by HSCs to home to the niche and are also used by solid tumor cells to migrate to the marrow and remain there (Figure 1).
The stromal-derived factor-1 (SDF-1 or CXCL12) axis is one of the most prominent shared mechanisms of HSC regulation and regulation of tumor metastasis to the BMM. CXCL12 is secreted by both endothelial cells and bone marrow stromal cells including osteoblasts, fibroblasts, and MSCs. Notably, SDF-1 expression is particularly high in osteoblasts (3). Its main receptor, CXCR4, is expressed on hematopoietic stem cells and mature cells (31), is overexpressed in metastatic solid tumors such as prostate (9) and breast (51), and is correlated with increasing tumor grade (52). Its role as a chemoattractant for both HSCs and mature hematopoietic cells is well defined (53–55), and it is also a very strong chemoattractant for metastatic cells (9). The SDF-1/CXCR4 axis is critical for homing to the marrow, as deletion of SDF-1 (56), or its receptor CXCR4 (57) results in an inability for engraftment of hematopoietic cells. Likewise, blocking this axis in metastatic epithelial tumor cells inhibits establishment of growth in the marrow (58, 59). In fact, SDF-1 gradients have been shown to regulate metastatic patterns. In sites where PCa lesions are often seen, including the bone marrow of the pelvis, tibia, femur, there are elevated levels of SDF-1 (59). Increasing SDF-1 endogenously through inhibition of CD26 also enhances metastasis to the bone (60). In addition, CXCR7, also known RDC-1, serves as another receptor for SDF-1, and is expressed in metastatic prostate (61), breast, and lung cells (62). Other important functions of SDF-1/CXCR4 axis support tumor activity in the niche. Signaling through CXCR4 activates CD164 (63) and alpha-v-beta3 integrins (64), allowing for adhesion and tight binding the osteoblasts and the extracellular matrix. In addition to attracting tumor cells, SDF-1 also attracts CAFs, which serve to enhance cancer survival in the bone (65). VEGF has also been thought to play a role in directing osteotropism of metastatic cells. The population of cells thought to induce a pre-metastatic niche, VEGFR-1-positive hematopoietic progenitors, are associated with an increase of SDF-1 (66). These cells are also thought to mediate osteolysis (67) and thus release growth factors from the bone, further contributing to an environment conducive to metastatic growth.
Osteopontin (OPN) also is a protein that is highly expressed in trabecular bone along the endosteum (68). As the name suggests (“osteo" meaning bone and “pontin” from Latin for “-bridge”), it is an extracellular linking protein responsible for cell-to-extracelluar matrix adhesion. It has been implicated as an important regulator of migration of HSCs through the marrow and functionality of the HSC niche (68, 69). In OPN knockout mice, HSCs were unable to engraft in the endosteal region, revealing that OPN is critical for HSC homing and retention. Based upon its role in HSC biology, it is not surprising then that the molecule also plays a significant role in metastasis of solid tumors (70). In fact, it is expressed by many solid tumors (71) and plays a role in tumor progression and invasiveness in epithelial cancers including breast (72), prostate (73) and mammary carcinoma (74, 75). OPN regulates homing and invasion through integrin activation (70), in particular alpha-V and beta integrins, which have been implicated in both HSC and metastatic tumor cell retention and function. Integrins are cell-surface proteins that are allow for cellular adhesion, and are comprised of non-covalently associated alpha and beta subunits (76). Alpha-4-beta-1 integrin, or very late antigen-4 (VLA-4) and its ligand fibronectin are important for HSC localization and retention to osteoblasts and the endosteal niche (3, 77). VLA-4 receptor expression on hematopoietic progenitors and engagement of its ligand is also a characteristic of pre-metastatic niche-inducing cells (24). Integrin and VLA-4 disregulation is consistently found solid tumors (78–80), leukemia (81) and in bone metastases. Expression of alpha-v-beta-3 integrins is correlated with highly aggressive and invasive metastases, and this combination of integrins serves to anchor metastatic cells to the niche (64, 82).
In addition to integrins, cadherins are calcium-dependent binding proteins that allow for cell-cell adhesion and typically serve as both a ligand and receptor, as cadherin-cadherin binding between different cell types is observed. Bone-associated cadherins have been implicated metastatic progression. OB-cadherin, or cadherin-11, is an osteoblast-derived cadherin that has recently been shown to increase migration invasiveness in breast and prostate cancer metastasis (83–85). In the context of HSCs, progenitor cells and MSCs also exhibit OB-cadherin and N-cadherin (86), yet their role as niche regulators remains highly controversial as to whether or not they regulate the HSC niche or not (38). If not, these data suggest a point of divergence between the two systems.
In order to further understand the functional capacity of the niche for solid tumors to target and retain metastatic cells, homing and adhesion molecules that functionally characterize the HSC niche may provide some insight. For many of the molecular mechanisms that regulate HSC activity in the niche are potentially parasitized by tumor cells. These molecular mechanisms are known include SDF-1/CXCR4, OPN, VLA-4/fibronectin, VLA-4/vascular cell adhesion molecule-1 (VCAM-1), intercellular adhesion molecule-1 (ICAM-1) (6), Angiopoietin-1 (Ang-1)/Tie-2 (87), canonical Wnt signaling (88), Notch/Jagged signaling (89), thrombopoietin (TPO)/Mpl receptor (90), stem cell factor (SCF/cKit receptor (3, 27),) and annexin II/annexin II receptor (91).
4.2. Survival and growth
The bone marrow is a rich reservoir of nutrients and growth factors that can be released to promote cellular growth and survival. The marrow microenvironment is critical for maintaining long-term HSC survival, but metastatic tumor cells also take advantage of this nutrient source. Direct binding to osteoblasts can also promote growth and survival of metastases using many of the aforementioned molecular mechanisms involved in homing and migration. Additionally, metastatic tumors activate osteoclasts to release matrix-bound growth factors through induction of the pro-osteoclastogenic molecule known as receptor activator of NF-kappa-beta ligand (RANKL) (37).
One pertinent example is interleukin-6 (IL-6), a growth factor that serves to support growth and survival in the HSC and tumor niche. It has been shown to promote growth and survival of cancer cells in the marrow (92–95). VEGF and HSCs are known to stimulate IL-6 production in osteoblasts and bone marrow stromal cells (34, 93), and increased IL-6 production by bone marrow stromal cells stimulates VEGF production, creating a cycle of growth factor production to amplify itself (96). Moreover, high IL-6 levels in the marrow appear to promote tumor survival and osteoclast activation (97, 98).
Another example could be the polycomb family proto-oncogene, Bmi-1. Bmi-1 is consistently required for the self-renewal of diverse adult stem cells, as well as for the proliferation of cancer cells in the same tissues. Bmi-1 promotes HSC self-renewal partly by repressing the expression of Ink4a and Arf, tumor suppressor genes that are commonly deleted in cancer (99, 100). Such similarities in regulation of cancer cell proliferation and stem cell renewal indicates that growth and survival in cancer and HSCs are regulated by analogous networks of molecules.
One more molecule that we believe is particularly important as a tether for HSCs to the niche and in metastasis is annexin II (Anxa2). Anxa2 is an adhesion molecule that is highly expressed in the bone marrow by osteoblasts and endothelial cells (101). It has been shown to have many roles in hematopoiesis and the marrow, including osteoclast activation and osteoblast mineralization (102, 103). Expression of Anxa2 by osteoblasts has been shown to regulation homing, migration and retention of HSCs after transplantation to the endosteal niche (91). In anxa2-deficient animals, fewer HSCs are found in the marrow, suggesting that this molecule plays a role in HSC niche selection. Anxa2 is also expressed in many solid tumors, and is associated with high invasiveness and tumor progression (104) in cancers including prostate, lung, pancreatic, and brain cancers (105). In prostate cancer, inhibiting Anxa2 function inhibits metastatic ability of the tumor cells, and growth at a secondary site. Anxa2-mediated proliferation and survival occurs via the MAPK signaling pathway, and Anxa2 receptor engagement in prostate cancer may stimulate expression of other receptors and adhesion molecules (105). This may contribute to the growth and proliferation of solid tumors in the niche in both direct and indirect ways, as Anxa2-mediated activation of osteoclasts may indirectly enhance secondary tumor growth through the release of the matrix-bound growth factors during osteoclastic bone resorption (102).
4.3 Quiescence and dormancy
The ability to engage in a state of G0 growth arrest is a characteristic of stem cells known as quiescence. Quiescence is critical for protecting stem cells so they can retain their long-term self-renewal capacity. Most HSCs are in a quiescent G0 state within marrow, cycling approximately every 57 days (106). Similarly, disseminated tumor cells that invade the bone marrow exhibit G0 growth arrest, termed “cellulardormancy” (19). Most disseminated tumor cells that arrive at a distant site undergo apoptosis, but cellular dormancy appears to be a way for tumor cells to evade apoptosis and survive until they can adequately survive in their new environment (107) (Figure 1). In fact based on clinical observations, many patients maintain viable disseminated tumor cells, even after treatment, a phenomenon known minimal residual disease (MRD) (19). Both HSC quiescence and tumor dormancy are reversible states of growth arrest (opposed to irreversible growth arrest as seen in apoptosis or senescence). HSCs must retain their ability to differentiate and self-renew, and proliferation is necessary for a dormant tumor cell to exhibit disease recurrence. For tumors, reactivation of a proliferative state often indicates disease relapse.Quiescent HSCs are thought to be localized in the endosteal region of the bone marrow (4). Recent studies have shown that this region is extremely hypoxic and hypoxia-inducible factor-1α (HIF-1α) regulates the cell-cycle quiescence of HSCs in these areas (108, 109). Similarly it has been shown that tumor micrometastases can exist in dormant state within hypoxic microenvironments. Such dormant micrometastases may become activated by an “angiogenic switch” triggered by changes in the balance between pro- and anti-angiogenic factors (110). This indicates that dormancy is regulated in similar fashion between cancer cells and HSCs.
In both HSCs and tumor cells, activation of cyclin-dependent kinase (CDK) inhibitors p27Kip1 and p21Cif result in G0/G1 growth arrest (111, 112). Adhesion molecules in the endosteal niche engage receptors that activate pathways to upregulate these molecules. Osteoblasts are the primary producers of angiopoietin-1 (Ang-1), the ligand to Tie2. Tie2 is expressed on quiescent HSCs (87), and engagement of the Tie2 receptor enhances beta-1-integrin adhesion to osteoblasts. Beta-1-integrin adhesion has been shown to lead to cell cycle arrest via p27Kip1 activity (113). Tie2 receptor engagement also activates the phosphatidylinositol 3-kinase (PI3-K)/Akt signaling pathway, which in turn regulates CDK activity (114). In Tie2-positive quiescent HSCs, Tie2 activation is thought to activate CDK inhibitor p21Cip1 through the PI3-K/Akt pathway (112). Activation of p21Cip1 is thought to induce a quiescent state, because p21Cip1 deficiency results in HSCs that are unable to remain in G0. These cells exhibit loss of their stem cell function, as they cannot engage in long-term self renewal or reconstitute lethally irradiated mice (115). Tie2 is also present on many types of cancer and higher expression correlates to metastatic tumor progression and invasiveness (116–118). Similar to quiescent HSCs, upregulation of Tie2 on tumor cells also results in expression of beta-1-integrins on tumor cells (119). While it is not yet known if Tie2 stimulation directly results in tumor dormancy, it is feasible that Tie2 signaling may also result in CDK inhibitor activation in tumor cells in a fashion similar to that proposed in HSCs. In addition to p21Cip activation, p27Kip1 activation also results in cell cycle arrest. Beta-1-integrin-mediated adhesion in tumor has been shown to regulate CDK activity and result in upregulation of p27Kip (113). This is confirmed in studies that show induction of p21 or p27 in colon cancer cells stimulates G1 arrest (120). The Notch signaling pathway has also been implicated in HSC quiescence and niche regulation. The Notch receptor is expressed on HSCs, and its ligand Jagged-1 is expressed by osteoblasts (35). In HSCs and tumors, the Notch signaling pathway has shown to activate both p27Kip and p21Cip1 (121–123), suggesting another mechanism for adhesion-induced quiescence in the niche.
FoxO proteins are a group of transcription factors which mediate cell-cycle regulation via p27Kip1 (124). FoxO play essential roles in the response to physiologic oxidative stress and thereby mediate quiescence and enhanced survival in the HSC compartment, a function that is required for its long-term regenerative potential (125). FoxO proteins are also tumor suppressors, the levels of which are regulated by the PI3K-AKT pathway (126). The chromosome translocations that disrupt the human FOXO gene have been associated with leukemia and the solid tumor alveolar rhabdomyosarcoma, and misregulation of FoxOs has been associated with a variety of tumor types, including those of the prostate, stomach, brain, and breast (127). Thus FoxO impedes cell proliferation in both cancer and HSCs most likely by similar downstream mechanisms.
Molecules which regulate HSC and tumor migration and survival have also been shown to exhibit quiescence-inducing functions. SDF-1 and CXCR4 have also been implicated in regulation of growth arrest in HSCs and cancer cells. CXCR4-deficient mice proliferate excessively and do not respond to SDF-1-stimulated induction into the cell cycle (128). In vitro growth arrest specific 6 (GAS6), a common ligand for the Axl/Sky/Mer receptor tryrosine kinase family, stimulation of prostate cancer cells and leukemia cells allowed the cells to evade apoptosis and enter a G0 growth arrest state (129, 130). It is evident that these niche molecules have multifaceted roles and are critical to HSC and tumor cell survival in multiple ways.
5. CONCLUSIONS AND IMPLICATIONS
5.1 Targets for therapy
Due to the ability for tumor cells to utilize the bone marrow niche to engage in dormancy, metastatic tumor cells can acquire cell adhesion-mediated drug resistance, or de novo drug resistance. Because the majority of standard cytotoxics target rapidly dividing cells, cells that are in a state of growth arrest are immune to these therapies (131, 132). Adhesion molecules including beta-integrins, VLA-4, and fibronectin have demonstrated that a reversible drug-resistant phenotype can be conferred upon epithelial tumors when these molecules are engaged (79, 80, 133). Thus, interfering with the ability for tumor cells to engage in cellular adhesion through these molecules has been an attractive target. Recent tests in mouse models have shown some promise. PSK1404, an antagonist of alpha-V-beta-3 integrin significantly inhibits bone metastasis in animal models of metastatic breast and ovarian cancer (134). While induced VLA-4 adhesion promoted drug resistance to cytarabine in acute myeloid leukemia (81) and melphalan in myeloma (135), anti-VLA-4 antibodies have been proposed to reverse drug resistance and minimize tumor burden (81). Looking to the HSC niche for therapy targets, agents used to induce HSC mobilization out of niche axis may also be useful for mobilizing tumor cells out of the bone marrow niche, and preventing them from engaging in growth arrest. Currently, granulocyte-colony stimulating factor (G-CSF) and AMD3100, a small molecule inhibitor of CXCR4 both inhibit the SDF-1/CXCR4 axis in HSCs (31, 136, 137). In animal models, using AMD3100 increased AML and myleoma chemosensitivity (138, 139) and AMD3100 disrupts metastatic lung cancer binding to stromal cells in coculture (140). Additionally, interferon gamma has been shown to reduce Anxa2 expression in cells and thus limit the invasive capacity of prostate cancer cells (141). These findings suggest that therapies that target tumor-niche cell binding may be promising.
At present, few if any therapies specifically target the HSC niche for chemotherapy of cancer. One such target includes CNTO328, an anti-IL-6 antibody which interferes with osteoblastic IL-6 activity (97, 98). Another molecule, Denosumab, targets the RANK/RANKL axis to inhibit osteoclast activation (142). Lerdelimumab, an anti TGF-beta antibody to inhibit TGF-beta signaling in bone marrow stromal cells has also been tested (44, 143). Together, tumor-niche interactions and noncancerous niche components provide many options for therapeutic targets. Since the tumor-niche ecosystem is dynamic, and both tumor and niche cells are able to adapt and evolve to changes in the microenvironment, it is important to have multiple therapeutic targets for each aspect of the ecosystem.
5.2 Cancer stem cell niche
A growing body of evidence suggests that a subpopulation of cells in a tumor have self-renewing capabilities similar to those of hematopoietic stem cells. These tumor cells are termed cancer stem cells (CSCs) and are thought to initiate tumor metasatases (144). Evidence for a leukemic stem cell (LSC) has been demonstrated (145), and osteoblasts have been shown to support niche activity of these LSCs (26). While the characterization of epithelial CSCs is a topic of debate, CD133 is thought to be a marker of many tumor-initiating epithelial CSCs (146). LSCs and metastatic solid tumor cells are both thought to hijack the HSC niche (6, 27), so it makes inherent sense that a solid tumor CSCs would be able to do the same. Thus, the HSC niche, solid tumor niche, and CSC niche most likely are comprised of the same cells and elements in the BMM (Figure 1).
5.3 Models to study the niche
As more is learned about the tumor niche and more targets for therapy are revealed, it is important to have sufficient models to study the microenvironment. Unfortunately, there are inadequate cell lines for many cell types and inadequate animal models, which provide barriers to further study. For prostate cancer this is particularly true, because few if any tumor cell lines recapitulate each of the stages of tumor progression. A model that we have recently developed which we believe is particularly instructive is an in vivo mouse model for prostate cancer metastasis (147) can be combined with transgenic tissues to explore targets and ultimately therapy (148, 149). In this model, there is a BMM that can easily be manipulated to study the bone marrow niche (150). In the in vivo mouse model, cancer cells from human cell lines are implanted into collagen scaffolds, then implanted subcutaneously in severe combined immune deficient (SCID) mice. This model recapitulates the events of early metastasis, as tumor cells must escape from the “primary” tumor, enter the circulation, and invade secondary tissues. The cancer cells can be then be detected in the peripheral blood and bone marrow by QPCR using the human-specific sequence Alu, or by bioluminescent imaging if the cells are tagged with luciferase. The ossicle model is derived from bone marrow stromal cells (149) or uses a tissue-engineered model (148) and the vossicle model is established using neonatal vertebral bone transplants, all of which can be implanted subcutaneously into SCID mice. Specific cellular and molecular factors involved in niche regulation can be manipulated in an ossicle or vossicle transplant. For instance, conditional ablation of osteoblasts is possible using vossicle transplants from Col2.3deltaTK transgenic mice (36). Since ossicles and vossicles are implanted subcutaneously, they provide convenient access to the bone microenvironment in vivo. These models provide effective ways to explore the events of metastasis and how these metastatic tumor cells interact in the solid tumor niche.
5.4 Summary
It is evident that the solid tumor niche shares many characteristics as the HSC niche, and may in fact parasitize the HSC niche to establish growth in the bone marrow (6). The HSC and solid tumor niche are defined by many cells and factors in the endosteal region, with osteoblasts playing an especially important role (6). The niche has many specialized molecules that regulate multiple functions and exhibit functional overlap (6). Especially important molecules that regulate tumor cell survival and dormancy in the niche include SDF-1 and its receptor CXCR4, annexin II and its receptor, and integrins. As the concept of the solid tumor niche is studied further, more light undoubtedly will be shed on the complicated mechanisms of metastatic dormancy and growth in the marrow. In turn, this will lead to better understanding of how tumor cells to evade current therapies through niche-mediated drug resistance, and the development of new niche-related therapies.
ACKNOWLEDGEMENTS
The authors would like to thank their families for support during the preparation of this work. In addition, this work was directly supported by a Pediatric Oncology Research Fellowship (Y.S), the Department of Defense (PC073952) and National Institutes of health (DK082481, DE020721, 1RC1DE020721, CA141426 and CA093900).
Abbreviations
- HSC
hematopoietic stem cell
- BMM
bone marrow microenvironment
- DTC
disseminated tumor cell
- VEGF
vascular endothelial growth factor
- VEGFR-1
vascular endothelial growth factor receptor-1
- IGF
insulin-like growth factor
- BMP
bone morphogenic protein
- TGF-beta
transforming growth factor-beta
- IL
interleukin
- MIP-1-alpha
macrophage inflammatory protein-1-alpha
- LIF
leukemia inhibitor factor
- PTH
parathyroid hormone
- PTHrP
parathyroid hormone related protein
- MSC
mesenchymal stem cell
- SDF-1
stromal derived factor-1
- MCP-1
monocyte chemotactic protein-1
- CAF
cancer associated fibroblast
- TAM
tumor associated macrophage
- RANK
receptor activator of nuclear factor-kappa-beta
- RANKL
receptor activator of nuclear factor- kappa-beta ligand
- M-CSF
macrophage-colony stimulating factor
- G-CSF
granulocyte-colony stimulating factor
- OPN
osteopontin
- VLA-4
very late antigen-4
- Anxa2
Annexin II
- CDk
cyclin-dependent kinase
- PI3-K
phosphatidylinositol 3-kinase
- CSC
cancer stem cell
- LSC
leukemic stem cell
REFERENCES
- 1.Paget S. The distribution of secondary growths in cancer of the breast. Lancet. 1889;1:571–573. [PubMed] [Google Scholar]
- 2.Schofield R. The relationship between the spleen colony-forming cell and the haemopoietic stem cell. Blood Cells. 1978;4(1–2):7–25. [PubMed] [Google Scholar]
- 3.Taichman RS. Blood and bone: two tissues whose fates are intertwined to create the hematopoietic stem-cell niche. Blood. 2005;105(7):2631–2639. doi: 10.1182/blood-2004-06-2480. doi: 2004-06-2480 [pii] 10.1182/blood-2004-06-2480. [DOI] [PubMed] [Google Scholar]
- 4.Yin T, Li L. The stem cell niches in bone. J Clin Invest. 2006;116(5):1195–201. doi: 10.1172/JCI28568. doi: 10.1172/JCI28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiel MJ, Morrison SJ. Uncertainty in the niches that maintain haematopoietic stem cells. Nat Rev Immunol. 2008;8(4):290–301. doi: 10.1038/nri2279. doi:nri2279 [pii] 10.1038/nri2279. [DOI] [PubMed] [Google Scholar]
- 6.Shiozawa Y, Havens AM, Pienta KJ, Taichman RS. The bone marrow niche: habitat to hematopoietic and mesenchymal stem cells, and unwitting host to molecular parasites. Leukemia. 2008;22(5):941–950. doi: 10.1038/leu.2008.48. doi:leu200848 [pii] 10.1038/leu.2008.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pienta KJ, McGregor N, Axelrod R, Axelrod DE. Ecological therapy for cancer: defining tumors using an ecosystem paradigm suggests new opportunities for novel cancer treatments. Transl Oncol. 2008;1(4):158–164. doi: 10.1593/tlo.08178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joyce JA, Pollard JW. Microenvironmental regulation of metastasis. Nat Rev Cancer. 2009;9(4):239–252. doi: 10.1038/nrc2618. doi:nrc2618 [pii] 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taichman RS, Cooper C, Keller ET, Pienta KJ, Taichman NS, McCauley LK. Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastasis to bone. Cancer Res. 2002;62(6):1832–7. [PubMed] [Google Scholar]
- 10.Kopp HG, Avecilla ST, Hooper AT, Rafii S. The bone marrow vascular niche: home of HSC differentiation and mobilization. Physiology (Bethesda) 2005;20:349–56. doi: 10.1152/physiol.00025.2005. doi: 20/5/349 [pii] 10.1152/physiol.00025.2005. [DOI] [PubMed] [Google Scholar]
- 11.Wong KF, Chan JK, Ma SK. Solid tumour with initial presentation in the bone marrow--a clinicopathologic study of 25 adult cases. Hematol Oncol. 1993;11(1):35–42. doi: 10.1002/hon.2900110105. [DOI] [PubMed] [Google Scholar]
- 12.Papac RJ. Bone marrow metastases. A review. Cancer. 1994;74(9):2403–2413. doi: 10.1002/1097-0142(19941101)74:9<2403::aid-cncr2820740904>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 13.Fidler IJ. Critical determinants of cancer metastasis: rationale for therapy. Cancer Chemother Pharmacol. 1999;43(Suppl):S3–S10. doi: 10.1007/s002800051091. [DOI] [PubMed] [Google Scholar]
- 14.Ellis WJ, Pfitzenmaier J, Colli J, Arfman E, Lange PH, Vessella RL. Detection and isolation of prostate cancer cells from peripheral blood and bone marrow. Urology. 2003;61(2):277–81. doi: 10.1016/s0090-4295(02)02291-4. doi:S0090429502022914 [pii] [DOI] [PubMed] [Google Scholar]
- 15.Morgan TM, Lange PH, Vessella RL. Detection and characterization of circulating and disseminated prostate cancer cells. Front Biosci. 2007;12:3000–3009. doi: 10.2741/2290. doi: 2290 [pii] [DOI] [PubMed] [Google Scholar]
- 16.Schmidt-Kittler O, Ragg T, Daskalakis A, Granzow M, Ahr A, Blankenstein TJ, Kaufmann M, Diebold J, Arnholdt H, Muller P, Bischoff J, Harich D, Schlimok G, Riethmuller G, Eils R, Klein CA. From latent disseminated cells to overt metastasis: genetic analysis of systemic breast cancer progression. Proc Natl Acad Sci U S A. 2003;100(13):7737–7742. doi: 10.1073/pnas.1331931100. doi: 10.1073/pnas.1331931100 1331931100 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klein CA, Blankenstein TJ, Schmidt-Kittler O, Petronio M, Polzer B, Stoecklein NH, Riethmuller G. Genetic heterogeneity of single disseminated tumour cells in minimal residual cancer. Lancet. 2002;360(9334):683–689. doi: 10.1016/S0140-6736(02)09838-0. doi: S0140-6736(02)09838-0 [pii] 10.1016/S0140-6736(02)09838-0. [DOI] [PubMed] [Google Scholar]
- 18.Morgan TM, Lange PH, Porter MP, Lin DW, Ellis WJ, Gallaher IS, Vessella RL. Disseminated tumor cells in prostate cancer patients after radical prostatectomy and without evidence of disease predicts biochemical recurrence. Clin Cancer Res. 2009;15(2):677–83. doi: 10.1158/1078-0432.CCR-08-1754. doi: 15/2/677 [pii] 10.1158/1078-0432.CCR-08-1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aguirre-Ghiso JA. Models, mechanisms and clinical evidence for cancer dormancy. Nat Rev Cancer. 2007;7(11):834–46. doi: 10.1038/nrc2256. doi: nrc2256 [pii] 10.1038/nrc2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. doi: CA.2007.0010 [pii] 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 21.Coleman RE, Rubens RD. The clinical course of bone metastases from breast cancer. Br J Cancer. 1987;55(1):61–6. doi: 10.1038/bjc.1987.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neiva K, Sun YX, Taichman RS. The role of osteoblasts in regulating hematopoietic stem cell activity and tumor metastasis. Braz J Med Biol Res. 2005;38(10):1449–54. doi: 10.1590/s0100-879x2005001000001. doi: S0100-879X2005001000001 [pii] /S0100-879X2005001000001. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Y, Ma B, Fan Q. Mechanisms of breast cancer bone metastasis. Cancer Lett. 2010;292(1):1–7. doi: 10.1016/j.canlet.2009.11.003. doi: S0304-3835(09)00662-4 [pii] 10.1016/j.canlet.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, MacDonald DD, Jin DK, Shido K, Kerns SA, Zhu Z, Hicklin D, Wu Y, Port JL, Altorki N, Port ER, Ruggero D, Shmelkov SV, Jensen KK, Rafii S, Lyden D. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438(7069):820–7. doi: 10.1038/nature04186. doi: nature04186 [pii] 10.1038/nature04186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaplan RN, Rafii S, Lyden D. Preparing the "soil": the premetastatic niche. Cancer Res. 2006;66(23):11089–93. doi: 10.1158/0008-5472.CAN-06-2407. doi: 66/23/11089 [pii] 10.1158/0008-5472.CAN-06-2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ninomiya M, Abe A, Katsumi A, Xu J, Ito M, Arai F, Suda T, Kiyoi H, Kinoshita T, Naoe T. Homing, proliferation and survival sites of human leukemia cells in vivo in immunodeficient mice. Leukemia. 2007;21(1):136–42. doi: 10.1038/sj.leu.2404432. doi: 2404432 [pii] 10.1038/sj.leu.2404432. [DOI] [PubMed] [Google Scholar]
- 27.Lane SW, Scadden DT, Gilliland DG. The leukemic stem cell niche: current concepts and therapeutic opportunities. Blood. 2009;114(6):1150–7. doi: 10.1182/blood-2009-01-202606. doi: blood-2009-01-202606 [pii] 10.1182/blood-2009-01-202606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raaijmakers MH, Mukherjee S, Guo S, Zhang S, Kobayashi T, Schoonmaker JA, Ebert BL, Al-Shahrour F, Hasserjian RP, Scadden EO, Aung Z, Matza M, Merkenschlager M, Lin C, Rommens JM, Scadden DT. Bone progenitor dysfunction induces myelodysplasia and secondary leukaemia. Nature. 2010;464(7290):852–7. doi: 10.1038/nature08851. doi: nature08851 [pii] 10.1038/nature08851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Linkhart TA, Mohan S, Baylink DJ. Growth factors for bone growth and repair: IGF, TGF beta and BMP. Bone. 1996;19(1 Suppl):1S–12S. doi: 10.1016/s8756-3282(96)00138-x. [DOI] [PubMed] [Google Scholar]
- 30.Martinez J, Fuentes M, Cambiazo V, Santibanez JF. Bone extracellular matrix stimulates invasiveness of estrogen-responsive human mammary MCF-7 cells. Int J Cancer. 1999;83(2):278–82. doi: 10.1002/(sici)1097-0215(19991008)83:2<278::aid-ijc21>3.0.co;2-7. doi: 10.1002/(SICI)1097-0215(19991008)83:<2-278::AID-IJC21>3.0.CO;2-7 [pii] [DOI] [PubMed] [Google Scholar]
- 31.Lapidot T, Dar A, Kollet O. How do stem cells find their way home? Blood. 2005;106(6):1901–10. doi: 10.1182/blood-2005-04-1417. doi: 2005-04-1417 [pii] 10.1182/blood-2005-04-1417. [DOI] [PubMed] [Google Scholar]
- 32.Zhu J, Garrett R, Jung Y, Zhang Y, Kim N, Wang J, Joe GJ, Hexner E, Choi Y, Taichman RS, Emerson SG. Osteoblasts support B-lymphocyte commitment and differentiation from hematopoietic stem cells. Blood. 2007;109(9):3706–12. doi: 10.1182/blood-2006-08-041384. doi: blood-2006-08-041384 [pii] 10.1182/blood-2006-08-041384. [DOI] [PubMed] [Google Scholar]
- 33.Jung Y, Wang J, Havens A, Sun Y, Jin T, Taichman RS. Cell-to-cell contact is critical for the survival of hematopoietic progenitor cells on osteoblasts. Cytokine. 2005;323(3–4):155–62. doi: 10.1016/j.cyto.2005.09.001. doi: S1043-4666(05)00287-5 [pii] 10.1016/j.cyto.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 34.Taichman RS, Reilly MJ, Verma RS, Emerson SG. Augmented production of interleukin-6 by normal human osteoblasts in response to CD34+ hematopoietic bone marrow cells in vitro. Blood. 1997;89(4):1165–72. [PubMed] [Google Scholar]
- 35.Calvi LM, Adams GB, Weibrecht KW, Weber JM, Olson DP, Knight MC, Martin RP, Schipani E, Divieti P, Bringhurst FR, Milner LA, Kronenberg HM, Scadden DT. Osteoblastic cells regulate the haematopoietic stem cell niche. Nature. 2003;425(6960):841–6. doi: 10.1038/nature02040. doi: 10.1038/nature02040 nature02040 [pii] [DOI] [PubMed] [Google Scholar]
- 36.Visnjic D, Kalajzic Z, Rowe DW, Katavic V, Lorenzo J, Aguila HL. Hematopoiesis is severely altered in mice with an induced osteoblast deficiency. Blood. 2004;103(9):3258–64. doi: 10.1182/blood-2003-11-4011. doi: 10.1182/blood-2003-11-40112003-11-4011 [pii] [DOI] [PubMed] [Google Scholar]
- 37.Keller ET, Zhang J, Cooper CR, Smith PC, McCauley LK, Pienta KJ, Taichman RS. Prostate carcinoma skeletal metastases: cross-talk between tumor and bone. Cancer Metastasis Rev. 2001;20(3–4):333–49. doi: 10.1023/a:1015599831232. [DOI] [PubMed] [Google Scholar]
- 38.Kiel MJ, Acar M, Radice GL, Morrison SJ. Hematopoietic stem cells do not depend on N-cadherin to regulate their maintenance. Cell Stem Cell. 2009;4(2):170–9. doi: 10.1016/j.stem.2008.10.005. doi: S1934-5909(08)00528-6 [pii]10.1016/j.stem.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakamura Y, Arai F, Iwasaki H, Hosokawa K, Kobayashi I, Gomei Y, Matsumoto Y, Yoshihara H, Suda T. Isolation and characterization of endosteal niche cell populations that regulate hematopoietic stem cells. Blood. 2010 doi: 10.1182/blood-2009-08-239194. doi: blood-2009-08-239194 [pii] 10.1182/blood-2009-08-239194. [DOI] [PubMed] [Google Scholar]
- 40.Dwyer RM, Potter-Beirne SM, Harrington KA, Lowery AJ, Hennessy E, Murphy JM, Barry FP, O'Brien T, Kerin MJ. Monocyte chemotactic protein-1 secreted by primary breast tumors stimulates migration of mesenchymal stem cells. Clin Cancer Res. 2007;13(17):5020–7. doi: 10.1158/1078-0432.CCR-07-0731. doi: 13/17/5020 [pii] 10.1158/1078-0432.CCR-07-0731. [DOI] [PubMed] [Google Scholar]
- 41.Spaeth E, Klopp A, Dembinski J, Andreeff M, Marini F. Inflammation and tumor microenvironments: defining the migratory itinerary of mesenchymal stem cells. Gene Ther. 2008;15(10):730–8. doi: 10.1038/gt.2008.39. doi: gt200839 [pii] 10.1038/gt.2008.39. [DOI] [PubMed] [Google Scholar]
- 42.Bergfeld SA, DeClerck YA. Bone marrow-derived mesenchymal stem cells and the tumor microenvironment. Cancer Metastasis Rev. 2010;29(2):249–61. doi: 10.1007/s10555-010-9222-7. doi: 10.1007/s10555-010-9222-7. [DOI] [PubMed] [Google Scholar]
- 43.Wels J, Kaplan RN, Rafii S, Lyden D. Migratory neighbors and distant invaders: tumor-associated niche cells. Genes Dev. 2008;22(5):559–74. doi: 10.1101/gad.1636908. doi: 22/5/559 [pii] 10.1101/gad.1636908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stover DG, Bierie B, Moses HL. A delicate balance: TGF-beta and the tumor microenvironment. J Cell Biochem. 2007;101(4):851–61. doi: 10.1002/jcb.21149. doi: 10.1002/jcb.21149. [DOI] [PubMed] [Google Scholar]
- 45.Kollet O, Dar A, Shivtiel S, Kalinkovich A, Lapid K, Sztainberg Y, Tesio M, Samstein RM, Goichberg P, Spiegel A, Elson A, Lapidot T. Osteoclasts degrade endosteal components and promote mobilization of hematopoietic progenitor cells. Nat Med. 2006;12(6):657–64. doi: 10.1038/nm1417. doi: nm1417 [pii] 10.1038/nm1417. [DOI] [PubMed] [Google Scholar]
- 46.Papapoulos SE, Hamdy NA, van der Pluijm G. Bisphosphonates in the management of prostate carcinoma metastatic to the skeleton. Cancer. 2000;88(12 Suppl):3047–53. doi: 10.1002/1097-0142(20000615)88:12+<3047::aid-cncr22>3.3.co;2-l. doi: 10.1002/1097-0142(20000615)88:12+<3047::AID-CNCR22>3.0.CO;2-U [pii] [DOI] [PubMed] [Google Scholar]
- 47.Manishen WJ, Sivananthan K, Orr FW. Resorbing bone stimulates tumor cell growth. A role for the host microenvironment in bone metastasis. Am J Pathol. 1986;123(1):39–45. [PMC free article] [PubMed] [Google Scholar]
- 48.Magro C, Orr FW, Manishen WJ, Sivananthan K, Mokashi SS. Adhesion, chemotaxis, and aggregation of Walker carcinosarcoma cells in response to products of resorbing bone. J Natl Cancer Inst. 1985;74(4):829–38. [PubMed] [Google Scholar]
- 49.Orr W, Varani J, Gondex MK, Ward PA, Mundy GR. Chemotactic responses of tumor cells to products of resorbing bone. Science. 1979;203(4376):176–9. doi: 10.1126/science.569363. [DOI] [PubMed] [Google Scholar]
- 50.Korpal M, Yan J, Lu X, Xu S, Lerit DA, Kang Y. Imaging transforming growth factor-beta signaling dynamics and therapeutic response in breast cancer bone metastasis. Nat Med. 2009;15(8):960–6. doi: 10.1038/nm.1943. doi: nm.1943 [pii] 10.1038/nm.1943. [DOI] [PubMed] [Google Scholar]
- 51.Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordon-Cardo C, Guise TA, Massague J. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. 2003;3(6):537–49. doi: 10.1016/s1535-6108(03)00132-6. doi: S1535610803001326 [pii] [DOI] [PubMed] [Google Scholar]
- 52.Sun YX, Wang J, Shelburne CE, Lopatin DE, Chinnaiyan AM, Rubin MA, Pienta KJ, Taichman RS. Expression of CXCR4 and CXCL12 (SDF-1) in human prostate cancers (PCa) in vivo. J Cell Biochem. 2003;89(3):462–73. doi: 10.1002/jcb.10522. doi: 10.1002/jcb.10522. [DOI] [PubMed] [Google Scholar]
- 53.Imai K, Kobayashi M, Wang J, Ohiro Y, Hamada J, Cho Y, Imamura M, Musashi M, Kondo T, Hosokawa M, Asaka M. Selective transendothelial migration of hematopoietic progenitor cells: a role in homing of progenitor cells. Blood. 1999;93(1):149–56. [PubMed] [Google Scholar]
- 54.Lataillade JJ, Clay D, Dupuy C, Rigal S, Jasmin C, Bourin P, Le Bousse-Kerdiles MC. Chemokine SDF-1 enhances circulating CD34(+) cell proliferation in synergy with cytokines: possible role in progenitor survival. Blood. 2000;95(3):756–68. [PubMed] [Google Scholar]
- 55.Lataillade JJ, Clay D, Bourin P, Herodin F, Dupuy C, Jasmin C, Le Bousse-Kerdiles MC. Stromal cell-derived factor 1 regulates primitive hematopoiesis by suppressing apoptosis and by promoting G(0)/G(1) transition in CD34(+) cells: evidence for an autocrine/paracrine mechanism. Blood. 2002;99(4):1117–29. doi: 10.1182/blood.v99.4.1117. [DOI] [PubMed] [Google Scholar]
- 56.Nagasawa T, Hirota S, Tachibana K, Takakura N, Nishikawa S, Kitamura Y, Yoshida N, Kikutani H, Kishimoto T. Defects of B-cell lymphopoiesis and bone-marrow myelopoiesis in mice lacking the CXC chemokine PBSF/SDF-1. Nature. 1996;382(6592):635–8. doi: 10.1038/382635a0. doi: 10.1038/382635a0. [DOI] [PubMed] [Google Scholar]
- 57.Peled A, Petit I, Kollet O, Magid M, Ponomaryov T, Byk T, Nagler A, Ben-Hur H, Many A, Shultz L, Lider O, Alon R, Zipori D, Lapidot T. Dependence of human stem cell engraftment and repopulation of NOD/SCID mice on CXCR4. Science. 1999;283(5403):845–8. doi: 10.1126/science.283.5403.845. [DOI] [PubMed] [Google Scholar]
- 58.Liang Z, Wu T, Lou H, Yu X, Taichman RS, Lau SK, Nie S, Umbreit J, Shim H. Inhibition of breast cancer metastasis by selective synthetic polypeptide against CXCR4. Cancer Res. 2004;64(12):4302–8. doi: 10.1158/0008-5472.CAN-03-3958. doi: 10.1158/0008-5472.CAN-03-3958. [DOI] [PubMed] [Google Scholar]
- 59.Sun YX, Schneider A, Jung Y, Wang J, Dai J, Cook K, Osman NI, Koh-Paige AJ, Shim H, Pienta KJ, Keller ET, McCauley LK, Taichman RS. Skeletal localization and neutralization of the SDF-1(CXCL12)/CXCR4 axis blocks prostate cancer metastasis and growth in osseous sites in vivo. J Bone Miner Res. 2005;20(2):318–29. doi: 10.1359/JBMR.041109. doi: 10.1359/JBMR.041109. [DOI] [PubMed] [Google Scholar]
- 60.Sun YX, Pedersen EA, Shiozawa Y, Havens AM, Jung Y, Wang J, Pienta KJ, Taichman RS. CD26/dipeptidyl peptidase IV regulates prostate cancer metastasis by degrading SDF-1/CXCL12. Clin Exp Metastasis. 2008;25(7):765–76. doi: 10.1007/s10585-008-9188-9. doi: 10.1007/s10585-008-9188-9. [DOI] [PubMed] [Google Scholar]
- 61.Wang J, Shiozawa Y, Wang Y, Jung Y, Pienta KJ, Mehra R, Loberg R, Taichman RS. The role of CXCR7/RDC1 as a chemokine receptor for CXCL12/SDF-1 in prostate cancer. J Biol Chem. 2008;283(7):4283–94. doi: 10.1074/jbc.M707465200. doi: M707465200 [pii] 10.1074/jbc.M707465200. [DOI] [PubMed] [Google Scholar]
- 62.Miao Z, Luker KE, Summers BC, Berahovich R, Bhojani MS, Rehemtulla A, Kleer CG, Essner JJ, Nasevicius A, Luker GD, Howard MC, Schall TJ. CXCR7 (RDC1) promotes breast and lung tumor growth in vivo and is expressed on tumor-associated vasculature. Proc Natl Acad Sci U S A. 2007;104(40):15735–40. doi: 10.1073/pnas.0610444104. doi: 0610444104 [pii] 10.1073/pnas.0610444104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Havens AM, Jung Y, Sun YX, Wang J, Shah RB, Buhring HJ, Pienta KJ, Taichman RS. The role of sialomucin CD164 (MGC-24v or endolyn) in prostate cancer metastasis. BMC Cancer. 2006;6:195. doi: 10.1186/1471-2407-6-195. doi: 1471-2407-6-195 [pii] 10.1186/1471-2407-6-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sun YX, Fang M, Wang J, Cooper CR, Pienta KJ, Taichman RS. Expression and activation of alpha v beta 3 integrins by SDF-1/CXC12 increases the aggressiveness of prostate cancer cells. Prostate. 2007;67(1):61–73. doi: 10.1002/pros.20500. doi: 10.1002/pros.20500. [DOI] [PubMed] [Google Scholar]
- 65.Ostman A, Augsten M. Cancer-associated fibroblasts and tumor growth--bystanders turning into key players. Curr Opin Genet Dev. 2009;19(1):67–73. doi: 10.1016/j.gde.2009.01.003. doi: S0959-437X(09)00004-5 [pii] 10.1016/j.gde.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 66.Kaplan RN, Psaila B, Lyden D. Bone marrow cells in the 'pre-metastatic niche': within bone and beyond. Cancer Metastasis Rev. 2006;25(4):521–9. doi: 10.1007/s10555-006-9036-9. doi: 10.1007/s10555-006-9036-9. [DOI] [PubMed] [Google Scholar]
- 67.Aldridge SE, Lennard TW, Williams JR, Birch MA. Vascular endothelial growth factor acts as an osteolytic factor in breast cancer metastases to bone. Br J Cancer. 2005;92(8):1531–7. doi: 10.1038/sj.bjc.6602417. doi: 6602417 [pii] 10.1038/sj.bjc.6602417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Nilsson SK, Johnston HM, Whitty GA, Williams B, Webb RJ, Denhardt DT, Bertoncello I, Bendall LJ, Simmons PJ, Haylock DN. Osteopontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood. 2005;106(4):1232–9. doi: 10.1182/blood-2004-11-4422. doi: 2004-11-4422 [pii] 10.1182/blood-2004-11-4422. [DOI] [PubMed] [Google Scholar]
- 69.Stier S, Ko Y, Forkert R, Lutz C, Neuhaus T, Grunewald E, Cheng T, Dombkowski D, Calvi LM, Rittling SR, Scadden DT. Osteopontin is a hematopoietic stem cell niche component that negatively regulates stem cell pool size. J Exp Med. 2005;201(11):1781–91. doi: 10.1084/jem.20041992. doi: jem.20041992 [pii] 10.1084/jem.20041992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wai PY, Kuo PC. The role of Osteopontin in tumor metastasis. J Surg Res. 2004;121(2):228–41. doi: 10.1016/j.jss.2004.03.028. doi: S0022-4804(04)00136-2 [pii] 10.1016/j.jss.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 71.Fedarko NS, Jain A, Karadag A, Van Eman MR, Fisher LW. Elevated serum bone sialoprotein and osteopontin in colon, breast, prostate, and lung cancer. Clin Cancer Res. 2001;7(12):4060–6. [PubMed] [Google Scholar]
- 72.Rudland PS, Platt-Higgins A, El-Tanani M, De Silva Rudland S, Barraclough R, Winstanley JH, Howitt R, West CR. Prognostic significance of the metastasis-associated protein osteopontin in human breast cancer. Cancer Res. 2002;62(12):3417–27. [PubMed] [Google Scholar]
- 73.Thalmann GN, Sikes RA, Devoll RE, Kiefer JA, Markwalder R, Klima I, Farach-Carson CM, Studer UE, Chung LW. Osteopontin: possible role in prostate cancer progression. Clin Cancer Res. 1999;5(8):2271–7. [PubMed] [Google Scholar]
- 74.Tuck AB, O'Malley FP, Singhal H, Tonkin KS, Harris JF, Bautista D, Chambers AF. Osteopontin and p53 expression are associated with tumor progression in a case of synchronous, bilateral, invasive mammary carcinomas. Arch Pathol Lab Med. 1997;121(6):578–84. [PubMed] [Google Scholar]
- 75.Tuck AB, Arsenault DM, O'Malley FP, Hota C, Ling MC, Wilson SM, Chambers AF. Osteopontin induces increased invasiveness and plasminogen activator expression of human mammary epithelial cells. Oncogene. 1999;18(29):4237–46. doi: 10.1038/sj.onc.1202799. doi: 10.1038/sj.onc.1202799. [DOI] [PubMed] [Google Scholar]
- 76.Giancotti FG, Ruoslahti E. Integrin signaling. Science. 1999;285(5430):1028–32. doi: 10.1126/science.285.5430.1028. doi: 7724 [pii] [DOI] [PubMed] [Google Scholar]
- 77.Verfaillie CM. Adhesion receptors as regulators of the hematopoietic process. Blood. 1998;92(8):2609–12. [PubMed] [Google Scholar]
- 78.Sethi T, Rintoul RC, Moore SM, MacKinnon AC, Salter D, Choo C, Chilvers ER, Dransfield I, Donnelly SC, Strieter R, Haslett C. Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: a mechanism for small cell lung cancer growth and drug resistance in vivo. Nat Med. 1999;5(6):662–8. doi: 10.1038/9511. doi: 10.1038/9511. [DOI] [PubMed] [Google Scholar]
- 79.Hodkinson PS, Elliott T, Wong WS, Rintoul RC, Mackinnon AC, Haslett C, Sethi T. ECM overrides DNA damage-induced cell cycle arrest and apoptosis in small-cell lung cancer cells through beta1 integrin-dependent activation of PI3-kinase. Cell Death Differ. 2006;13(10):1776–88. doi: 10.1038/sj.cdd.4401849. doi: 4401849 [pii] 10.1038/sj.cdd.4401849. [DOI] [PubMed] [Google Scholar]
- 80.Aoudjit F, Vuori K. Integrin signaling inhibits paclitaxel-induced apoptosis in breast cancer cells. Oncogene. 2001;20(36):4995–5004. doi: 10.1038/sj.onc.1204554. doi: 10.1038/sj.onc.1204554. [DOI] [PubMed] [Google Scholar]
- 81.Matsunaga T, Takemoto N, Sato T, Takimoto R, Tanaka I, Fujimi A, Akiyama T, Kuroda H, Kawano Y, Kobune M, Kato J, Hirayama Y, Sakamaki S, Kohda K, Miyake K, Niitsu Y. Interaction between leukemic-cell VLA-4 and stromal fibronectin is a decisive factor for minimal residual disease of acute myelogenous leukemia. Nat Med. 2003;9(9):1158–65. doi: 10.1038/nm909. doi: 10.1038/nm909. [DOI] [PubMed] [Google Scholar]
- 82.Furger KA, Allan AL, Wilson SM, Hota C, Vantyghem SA, Postenka CO, Al-Katib W, Chambers AF, Tuck AB. Beta(3) integrin expression increases breast carcinoma cell responsiveness to the malignancy-enhancing effects of osteopontin. Mol Cancer Res. 2003;1(11):810–9. [PubMed] [Google Scholar]
- 83.Tamura D, Hiraga T, Myoui A, Yoshikawa H, Yoneda T. Cadherin-11-mediated interactions with bone marrow stromal/osteoblastic cells support selective colonization of breast cancer cells in bone. Int J Oncol. 2008;33(1):17–24. [PubMed] [Google Scholar]
- 84.Huang CF, Lira C, Chu K, Bilen MA, Lee YC, Ye X, Kim SM, Ortiz A, Wu FL, Logothetis CJ, Yu-Lee LY, Lin SH. Cadherin-11 Increases Migration and Invasion of Prostate Cancer Cells and Enhances their Interaction with Osteoblasts. Cancer Res. 2010 doi: 10.1158/0008-5472.CAN-09-3016. doi: 0008-5472.CAN-09-3016 [pii] 10.1158/0008-5472.CAN-09-3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chu K, Cheng CJ, Ye X, Lee YC, Zurita AJ, Chen DT, Yu-Lee LY, Zhang S, Yeh ET, Hu MC, Logothetis CJ, Lin SH. Cadherin-11 promotes the metastasis of prostate cancer cells to bone. Mol Cancer Res. 2008;6(8):1259–1267. doi: 10.1158/1541-7786.MCR-08-0077. doi: 6/8/1259 [pii] 10.1158/1541-7786.MCR-08-0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wein F, Pietsch L, Saffrich R, Wuchter P, Walenda T, Bork S, Horn P, Diehlmann A, Eckstein V, Ho AD, Wagner W. N-cadherin is expressed on human hematopoietic progenitor cells and mediates interaction with human mesenchymal stromal cells. Stem Cell Res. 2010;4(2):129–39. doi: 10.1016/j.scr.2009.12.004. doi: S1873-5061(09)00142-1 [pii] 10.1016/j.scr.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 87.Arai F, Hirao A, Ohmura M, Sato H, Matsuoka S, Takubo K, Ito K, Koh GY, Suda T. Tie2/angiopoietin-1 signaling regulates hematopoietic stem cell quiescence in the bone marrow niche. Cell. 2004;118(2):149–61. doi: 10.1016/j.cell.2004.07.004. doi: 10.1016/j.cell.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 88.Suda T, Arai F. Wnt signaling in the niche. Cell. 2008;132(5):729–30. doi: 10.1016/j.cell.2008.02.017. doi: S0092-8674(08)00265-1 [pii] 10.1016/j.cell.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 89.Yu X, Alder JK, Chun JH, Friedman AD, Heimfeld S, Cheng L, Civin CI. HES1 inhibits cycling of hematopoietic progenitor cells via DNA binding. Stem Cells. 2006;24(4):876–88. doi: 10.1634/stemcells.2005-0598. doi: 2005-0598 [pii] 10.1634/stemcells.2005-0598. [DOI] [PubMed] [Google Scholar]
- 90.Yoshihara H, Arai F, Hosokawa K, Hagiwara T, Takubo K, Nakamura Y, Gomei Y, Iwasaki H, Matsuoka S, Miyamoto K, Miyazaki H, Takahashi T, Suda T. Thrombopoietin/MPL signaling regulates hematopoietic stem cell quiescence and interaction with the osteoblastic niche. Cell Stem Cell. 2007;1(6):685–97. doi: 10.1016/j.stem.2007.10.020. doi: S1934-5909(07)00237-8 [pii] 10.1016/j.stem.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 91.Jung Y, Wang J, Song J, Shiozawa Y, Havens A, Wang Z, Sun YX, Emerson SG, Krebsbach PH, Taichman RS. Annexin II expressed by osteoblasts and endothelial cells regulates stem cell adhesion, homing, and engraftment following transplantation. Blood. 2007;110(1):82–90. doi: 10.1182/blood-2006-05-021352. doi: blood-2006-05-021352 [pii] 10.1182/blood-2006-05-021352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Frassanito MA, Cusmai A, Iodice G, Dammacco F. Autocrine interleukin-6 production and highly malignant multiple myeloma: relation with resistance to drug-induced apoptosis. Blood. 2001;97(2):483–9. doi: 10.1182/blood.v97.2.483. [DOI] [PubMed] [Google Scholar]
- 93.Lu Y, Zhang J, Dai J, Dehne LA, Mizokami A, Yao Z, Keller ET. Osteoblasts induce prostate cancer proliferation and PSA expression through interleukin-6-mediated activation of the androgen receptor. Clin Exp Metastasis. 2004;21(5):399–408. doi: 10.1007/s10585-005-0056-6. [DOI] [PubMed] [Google Scholar]
- 94.Ara T, Song L, Shimada H, Keshelava N, Russell HV, Metelitsa LS, Groshen SG, Seeger RC, DeClerck YA. Interleukin-6 in the bone marrow microenvironment promotes the growth and survival of neuroblastoma cells. Cancer Res. 2009;69(1):329–37. doi: 10.1158/0008-5472.CAN-08-0613. doi: 69/1/329 [pii] 10.1158/0008-5472.CAN-08-0613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cheung WC, Van Ness B. Distinct IL-6 signal transduction leads to growth arrest and death in B cells or growth promotion and cell survival in myeloma cells. Leukemia. 2002;16(6):1182–8. doi: 10.1038/sj.leu.2402481. doi: 10.1038/sj.leu.2402481. [DOI] [PubMed] [Google Scholar]
- 96.Bisping G, Leo R, Wenning D, Dankbar B, Padro T, Kropff M, Scheffold C, Kroger M, Mesters RM, Berdel WE, Kienast J. Paracrine interactions of basic fibroblast growth factor and interleukin-6 in multiple myeloma. Blood. 2003;101(7):2775–83. doi: 10.1182/blood-2002-09-2907. doi: 10.1182/blood-2002-09-2907. [DOI] [PubMed] [Google Scholar]
- 97.Adachi Y, Yoshio-Hoshino N, Nishimoto N. The blockade of IL-6 signaling in rational drug design. Curr Pharm Des. 2008;14(12):1217–24. doi: 10.2174/138161208784246072. [DOI] [PubMed] [Google Scholar]
- 98.Wallner L, Dai J, Escara-Wilke J, Zhang J, Yao Z, Lu Y, Trikha M, Nemeth JA, Zaki MH, Keller ET. Inhibition of interleukin-6 with CNTO328, an anti-interleukin-6 monoclonal antibody, inhibits conversion of androgen-dependent prostate cancer to an androgen-independent phenotype in orchiectomized mice. Cancer Res. 2006;66(6):3087–95. doi: 10.1158/0008-5472.CAN-05-3447. doi: 66/6/3087 [pii] 10.1158/0008-5472.CAN-05-3447. [DOI] [PubMed] [Google Scholar]
- 99.Bruggeman SW, Hulsman D, Tanger E, Buckle T, Blom M, Zevenhoven J, van Tellingen O, van Lohuizen M. Bmi1 controls tumor development in an Ink4a/Arf-independent manner in a mouse model for glioma. Cancer Cell. 2007;12(4):328–41. doi: 10.1016/j.ccr.2007.08.032. doi: S1535-6108(07)00264-4 [pii] 10.1016/j.ccr.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 100.Park IK, Qian D, Kiel M, Becker MW, Pihalja M, Weissman IL, Morrison SJ, Clarke MF. Bmi-1 is required for maintenance of adult self-renewing haematopoietic stem cells. Nature. 2003;423(6937):302–5. doi: 10.1038/nature01587. doi: 10.1038/nature01587. [DOI] [PubMed] [Google Scholar]
- 101.Raynal P, Pollard HB. Annexins: the problem of assessing the biological role for a gene family of multifunctional calcium- and phospholipid-binding proteins. Biochim Biophys Acta. 1994;1197(1):63–93. doi: 10.1016/0304-4157(94)90019-1. doi: 0304-4157(94)90019-1 [pii] [DOI] [PubMed] [Google Scholar]
- 102.Takahashi S, Reddy SV, Chirgwin JM, Devlin R, Haipek C, Anderson J, Roodman GD. Cloning and identification of annexin II as an autocrine/paracrine factor that increases osteoclast formation and bone resorption. J Biol Chem. 1994;269(46):28696–701. [PubMed] [Google Scholar]
- 103.Wang W, Kirsch T. Retinoic acid stimulates annexin-mediated growth plate chondrocyte mineralization. J Cell Biol. 2002;157(6):1061–9. doi: 10.1083/jcb.200203014. doi: 10.1083/jcb.200203014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mai J, Waisman DM, Sloane BF. Cell surface complex of cathepsin B/annexin II tetramer in malignant progression. Biochim Biophys Acta. 2000;1477(1–2):215–30. doi: 10.1016/s0167-4838(99)00274-5. doi: S0167-4838(99)00274-5 [pii] [DOI] [PubMed] [Google Scholar]
- 105.Shiozawa Y, Havens AM, Jung Y, Ziegler AM, Pedersen EA, Wang J, Lu G, Roodman GD, Loberg RD, Pienta KJ, Taichman RS. Annexin II/annexin II receptor axis regulates adhesion, migration, homing, and growth of prostate cancer. J Cell Biochem. 2008;105(2):370–80. doi: 10.1002/jcb.21835. doi: 10.1002/jcb.21835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Allsopp RC, Cheshier S, Weissman IL. Telomere shortening accompanies increased cell cycle activity during serial transplantation of hematopoietic stem cells. J Exp Med. 2001;193(8):917–24. doi: 10.1084/jem.193.8.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Townson JL, Chambers AF. Dormancy of solitary metastatic cells. Cell Cycle. 2006;5(16):1744–50. doi: 10.4161/cc.5.16.2864. doi: 2864 [pii] [DOI] [PubMed] [Google Scholar]
- 108.Takubo K, Goda N, Yamada W, Iriuchishima H, Ikeda E, Kubota Y, Shima H, Johnson RS, Hirao A, Suematsu M, Suda T. Regulation of the HIF-1alpha level is essential for hematopoietic stem cells. Cell Stem Cell. 2010;7(3):391–402. doi: 10.1016/j.stem.2010.06.020. doi: S1934-5909(10)00344-9 [pii] 10.1016/j.stem.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 109.Simsek T, Kocabas F, Zheng J, Deberardinis RJ, Mahmoud AI, Olson EN, Schneider JW, Zhang CC, Sadek HA. The distinct metabolic profile of hematopoietic stem cells reflects their location in a hypoxic niche. Cell Stem Cell. 2010;7(3):380–90. doi: 10.1016/j.stem.2010.07.011. doi: S1934-5909(10)00347-4 [pii] 10.1016/j.stem.2010.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Li XF, O'Donoghue JA. Hypoxia in microscopic tumors. Cancer Lett. 2008;264(2):172–80. doi: 10.1016/j.canlet.2008.02.037. doi: S0304-3835(08)00134-1 [pii] 10.1016/j.canlet.2008.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Schmidt M, Lu Y, Parant JM, Lozano G, Bacher G, Beckers T, Fan Z. Differential roles of p21(Waf1) and p27(Kip1) in modulating chemosensitivity and their possible application in drug discovery studies. Mol Pharmacol. 2001;60(5):900–6. doi: 10.1124/mol.60.5.900. [DOI] [PubMed] [Google Scholar]
- 112.Arai F, Suda T. Maintenance of quiescent hematopoietic stem cells in the osteoblastic niche. Ann N Y Acad Sci. 2007;1106:41–53. doi: 10.1196/annals.1392.005. doi: annals.1392.005 [pii] 10.1196/annals.1392.005. [DOI] [PubMed] [Google Scholar]
- 113.Hazlehurst LA, Damiano JS, Buyuksal I, Pledger WJ, Dalton WS. Adhesion to fibronectin via beta1 integrins regulates p27kip1 levels and contributes to cell adhesion mediated drug resistance (CAM-DR) Oncogene. 2000;19(38):4319–27. doi: 10.1038/sj.onc.1203782. doi: 10.1038/sj.onc.1203782. [DOI] [PubMed] [Google Scholar]
- 114.Shiojima I, Walsh K. Role of Akt signaling in vascular homeostasis and angiogenesis. Circ Res. 2002;90(12):1243–50. doi: 10.1161/01.res.0000022200.71892.9f. [DOI] [PubMed] [Google Scholar]
- 115.Cheng T, Rodrigues N, Shen H, Yang Y, Dombkowski D, Sykes M, Scadden DT. Hematopoietic stem cell quiescence maintained by p21cip1/waf1. Science. 2000;287(5459):1804–8. doi: 10.1126/science.287.5459.1804. doi: 8339 [pii] [DOI] [PubMed] [Google Scholar]
- 116.Muller A, Lange K, Gaiser T, Hofmann M, Bartels H, Feller AC, Merz H. Expression of angiopoietin-1 and its receptor TEK in hematopoietic cells from patients with myeloid leukemia. Leuk Res. 2002;26(2):163–8. doi: 10.1016/s0145-2126(01)00110-2. doi: S0145212601001102 [pii] [DOI] [PubMed] [Google Scholar]
- 117.Mitsutake N, Namba H, Takahara K, Ishigaki K, Ishigaki J, Ayabe H, Yamashita S. Tie-2 and angiopoietin-1 expression in human thyroid tumors. Thyroid. 2002;12(2):95–9. doi: 10.1089/105072502753522310. doi: 10.1089/105072502753522310. [DOI] [PubMed] [Google Scholar]
- 118.Wang J, Wu K, Zhang D, Tang H, Xie H, Hong L, Pan Y, Lan M, Hu S, Ning X, Fan D. Expressions and clinical significances of angiopoietin-1-2 and Tie2 in human gastric cancer. Biochem Biophys Res Commun. 2005;337(1):386–93. doi: 10.1016/j.bbrc.2005.09.051. doi: S0006-291X(05)02008-5 [pii] 10.1016/j.bbrc.2005.09.051. [DOI] [PubMed] [Google Scholar]
- 119.Lee OH, Xu J, Fueyo J, Fuller GN, Aldape KD, Alonso MM, Piao Y, Liu TJ, Lang FF, Bekele BN, Gomez-Manzano C. Expression of the receptor tyrosine kinase Tie2 in neoplastic glial cells is associated with integrin beta1-dependent adhesion to the extracellular matrix. Mol Cancer Res. 2006;4(12):915–26. doi: 10.1158/1541-7786.MCR-06-0184. doi: 4/12/915 [pii] 10.1158/1541-7786.MCR-06-0184. [DOI] [PubMed] [Google Scholar]
- 120.Schmidt M, Lu Y, Liu B, Fang M, Mendelsohn J, Fan Z. Differential modulation of paclitaxel-mediated apoptosis by p21Waf1 and p27Kip1. Oncogene. 2000;19(20):2423–9. doi: 10.1038/sj.onc.1203546. doi: 10.1038/sj.onc.1203546. [DOI] [PubMed] [Google Scholar]
- 121.Nefedova Y, Cheng P, Alsina M, Dalton WS, Gabrilovich DI. Involvement of Notch-1 signaling in bone marrow stroma-mediated de novo drug resistance of myeloma and other malignant lymphoid cell lines. Blood. 2004;103(9):3503–10. doi: 10.1182/blood-2003-07-2340. doi: 10.1182/blood-2003-07-2340. [DOI] [PubMed] [Google Scholar]
- 122.Jundt F, Probsting KS, Anagnostopoulos I, Muehlinghaus G, Chatterjee M, Mathas S, Bargou RC, Manz R, Stein H, Dorken B. Jagged1-induced Notch signaling drives proliferation of multiple myeloma cells. Blood. 2004;103(9):3511–5. doi: 10.1182/blood-2003-07-2254. doi: 10.1182/blood-2003-07-22542003-07-2254 [pii] [DOI] [PubMed] [Google Scholar]
- 123.Lwin T, Hazlehurst LA, Dessureault S, Lai R, Bai W, Sotomayor E, Moscinski LC, Dalton WS, Tao J. Cell adhesion induces p27Kip1-associated cell-cycle arrest through down-regulation of the SCFSkp2 ubiquitin ligase pathway in mantle-cell and other non-Hodgkin B-cell lymphomas. Blood. 2007;110(5):1631–8. doi: 10.1182/blood-2006-11-060350. doi: blood-2006-11-060350 [pii] 10.1182/blood-2006-11-060350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Medema RH, Kops GJ, Bos JL, Burgering BM. AFX-like Forkhead transcription factors mediate cell-cycle regulation by Ras and PKB through p27kip1. Nature. 2000;404(6779):782–7. doi: 10.1038/35008115. doi: 10.1038/35008115. [DOI] [PubMed] [Google Scholar]
- 125.Tothova Z, Kollipara R, Huntly BJ, Lee BH, Castrillon DH, Cullen DE, McDowell EP, Lazo-Kallanian S, Williams IR, Sears C, Armstrong SA, Passegue E, DePinho RA, Gilliland DG. FoxOs are critical mediators of hematopoietic stem cell resistance to physiologic oxidative stress. Cell. 2007;128(2):325–39. doi: 10.1016/j.cell.2007.01.003. doi: S0092-8674(07)00050-5 [pii] 10.1016/j.cell.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 126.Paik JH, Kollipara R, Chu G, Ji H, Xiao Y, Ding Z, Miao L, Tothova Z, Horner JW, Carrasco DR, Jiang S, Gilliland DG, Chin L, Wong WH, Castrillon DH, DePinho RA. FoxOs are lineage-restricted redundant tumor suppressors and regulate endothelial cell homeostasis. Cell. 2007;128(2):309–23. doi: 10.1016/j.cell.2006.12.029. doi: S0092-8674(07)00047-5 [pii] 10.1016/j.cell.2006.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Arden KC. FoxOs in tumor suppression and stem cell maintenance. Cell. 2007;128(2):235–7. doi: 10.1016/j.cell.2007.01.009. doi: S0092-8674(07)00065-7 [pii] 10.1016/j.cell.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 128.Nie Y, Han YC, Zou YR. CXCR4 is required for the quiescence of primitive hematopoietic cells. J Exp Med. 2008;205(4):777–83. doi: 10.1084/jem.20072513. doi: jem.20072513 [pii] 10.1084/jem.20072513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shiozawa Y, Pedersen EA, Taichman RS. GAS6/Mer axis regulates the homing and survival of the E2A/PBX1-positive B-cell precursor acute lymphoblastic leukemia in the bone marrow niche. Exp Hematol. 2010;38(2):132–40. doi: 10.1016/j.exphem.2009.11.002. doi: S0301-472X(09)00427-5 [pii] 10.1016/j.exphem.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Shiozawa Y, Pedersen EA, Patel LR, Ziegler AM, Havens AM, Jung Y, Wang J, Zalucha S, Loberg RD, Pienta KJ, Taichman RS. GAS6/AXL axis regulates prostate cancer invasion, proliferation, and survival in the bone marrow niche. Neoplasia. 2010;12(2):116–27. doi: 10.1593/neo.91384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Meads MB, Hazlehurst LA, Dalton WS. The bone marrow microenvironment as a tumor sanctuary and contributor to drug resistance. Clin Cancer Res. 2008;14(9):2519–26. doi: 10.1158/1078-0432.CCR-07-2223. doi: 14/9/2519 [pii] 10.1158/1078-0432.CCR-07-2223. [DOI] [PubMed] [Google Scholar]
- 132.Felsher DW. Tumor dormancy: death and resurrection of cancer as seen through transgenic mouse models. Cell Cycle. 2006;5(16):1808–11. doi: 10.4161/cc.5.16.3111. doi: 3111 [pii] [DOI] [PubMed] [Google Scholar]
- 133.Hoyt DG, Rusnak JM, Mannix RJ, Modzelewski RA, Johnson CS, Lazo JS. Integrin activation suppresses etoposide-induced DNA strand breakage in cultured murine tumor-derived endothelial cells. Cancer Res. 1996;56(18):4146–9. [PubMed] [Google Scholar]
- 134.Zhao Y, Bachelier R, Treilleux I, Pujuguet P, Peyruchaud O, Baron R, Clement-Lacroix P, Clezardin P. Tumor alphavbeta3 integrin is a therapeutic target for breast cancer bone metastases. Cancer Res. 2007;67(12):5821–30. doi: 10.1158/0008-5472.CAN-06-4499. doi: 67/12/5821 [pii] 10.1158/0008-5472.CAN-06-4499. [DOI] [PubMed] [Google Scholar]
- 135.Mori Y, Shimizu N, Dallas M, Niewolna M, Story B, Williams PJ, Mundy GR, Yoneda T. Anti-alpha4 integrin antibody suppresses the development of multiple myeloma and associated osteoclastic osteolysis. Blood. 2004;104(7):2149–54. doi: 10.1182/blood-2004-01-0236. doi: 10.1182/blood-2004-01-02362004-01-0236 [pii] [DOI] [PubMed] [Google Scholar]
- 136.Petit I, Szyper-Kravitz M, Nagler A, Lahav M, Peled A, Habler L, Ponomaryov T, Taichman RS, Arenzana-Seisdedos F, Fujii N, Sandbank J, Zipori D, Lapidot T. G-CSF induces stem cell mobilization by decreasing bone marrow SDF-1 and up-regulating CXCR4. Nat Immunol. 2002;3(7):687–94. doi: 10.1038/ni813. doi: 10.1038/ni813ni813 [pii] [DOI] [PubMed] [Google Scholar]
- 137.Abkowitz JL, Robinson AE, Kale S, Long MW, Chen J. Mobilization of hematopoietic stem cells during homeostasis and after cytokine exposure. Blood. 2003;102(4):1249–53. doi: 10.1182/blood-2003-01-0318. doi: 10.1182/blood-2003-01-0318. [DOI] [PubMed] [Google Scholar]
- 138.Nervi B, Ramirez P, Rettig MP, Uy GL, Holt MS, Ritchey JK, Prior JL, Piwnica-Worms D, Bridger G, Ley TJ, DiPersio JF. Chemosensitization of acute myeloid leukemia (AML) following mobilization by the CXCR4 antagonist AMD3100. Blood. 2009;113(24):6206–14. doi: 10.1182/blood-2008-06-162123. doi: blood-2008-06-162123 [pii] 10.1182/blood-2008-06-162123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Azab AK, Runnels JM, Pitsillides C, Moreau AS, Azab F, Leleu X, Jia X, Wright R, Ospina B, Carlson AL, Alt C, Burwick N, Roccaro AM, Ngo HT, Farag M, Melhem MR, Sacco A, Munshi NC, Hideshima T, Rollins BJ, Anderson KC, Kung AL, Lin CP, Ghobrial IM. CXCR4 inhibitor AMD3100 disrupts the interaction of multiple myeloma cells with the bone marrow microenvironment and enhances their sensitivity to therapy. Blood. 2009;113(18):4341–51. doi: 10.1182/blood-2008-10-186668. doi: blood-2008-10-186668 [pii] 10.1182/blood-2008-10-186668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Burger JA, Stewart DJ. CXCR4 chemokine receptor antagonists: perspectives in SCLC. Expert Opin Investig Drugs. 2009;18(4):481–90. doi: 10.1517/13543780902804249. doi: 10.1517/13543780902804249. [DOI] [PubMed] [Google Scholar]
- 141.Hastie C, Masters JR, Moss SE, Naaby-Hansen S. Interferon-gamma reduces cell surface expression of annexin 2 and suppresses the invasive capacity of prostate cancer cells. J Biol Chem. 2008;283(18):12595–603. doi: 10.1074/jbc.M800189200. doi: M800189200 [pii] 10.1074/jbc.M800189200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gallagher JC. Advances in bone biology and new treatments for bone loss. Maturitas. 2008;60(1):65–9. doi: 10.1016/j.maturitas.2008.04.005. doi: S0378-5122(08)00118-7 [pii] 10.1016/j.maturitas.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 143.Biswas S, Guix M, Rinehart C, Dugger TC, Chytil A, Moses HL, Freeman ML, Arteaga CL. Inhibition of TGF-beta with neutralizing antibodies prevents radiation-induced acceleration of metastatic cancer progression. J Clin Invest. 2007;117(5):1305–13. doi: 10.1172/JCI30740. doi: 10.1172/JCI30740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414(6859):105–11. doi: 10.1038/35102167. doi: 10.1038/3510216735102167 [pii] [DOI] [PubMed] [Google Scholar]
- 145.Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997;3(7):730–7. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 146.Liao Y, Hu X, Huang X, He C. Quantitative analyses of CD133 expression facilitate researches on tumor stem cells. Biol Pharm Bull. 2010;33(5):738–42. doi: 10.1248/bpb.33.738. doi: JST.JSTAGE/bpb/33.738 [pii]] [DOI] [PubMed] [Google Scholar]
- 147.Havens AM, Pedersen EA, Shiozawa Y, Ying C, Jung Y, Sun Y, Neeley C, Wang J, Mehra R, Keller ET, McCauley LK, Loberg RD, Pienta KJ, Taichman RS. An in vivo mouse model for human prostate cancer metastasis. Neoplasia. 2008;10(4):371–80. doi: 10.1593/neo.08154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Song J, Kiel MJ, Wang Z, Wang J, Taichman RS, Morrison SJ, Krebsbach PH. An in vivo model to study and manipulate the hematopoietic stem cell niche. Blood. 2010;115(13):2592–600. doi: 10.1182/blood-2009-01-200071. doi: blood-2009-01-200071 [pii] 10.1182/blood-2009-01-200071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pettway GJ, McCauley LK. Ossicle and vossicle implant model systems. Methods Mol Biol. 2008;455:101–10. doi: 10.1007/978-1-59745-104-8_7. doi: 10.1007/978-1-59745-104-8_7. [DOI] [PubMed] [Google Scholar]
- 150.Havens AM, Pedersen EA, Shiozawa Y, Taichman RS. Innovative mouse models for metastatic disease. Drug Discov Today Dis Models. 2009;6(1):27–31. [Google Scholar]