Abstract
Objective
The purpose of this study was to evaluate the effect of casein phosphopeptide amorphous calcium phosphate (CPP-ACP) on the shear bond strength (SBS) of brackets bonded to non-demineralized teeth with either phosphoric acid etching or self-etching primer.
Methods
Sixty human premolars were randomly assigned to 1 of 4 treatment groups (n = 15 each): phosphoric acid etching (group 1); self-etching primer (group 2); CPP-ACP for 2 weeks + phosphoric acid etching (group 3), and CPP-ACP for 2 weeks + self-etching primer (group 4). After bonding of the maxillary premolar metal brackets, specimens were subjected to shear forces in a testing machine. Scanning electron microscopy was used to observe etching patterns on the enamel surfaces of all teeth. A 2-way analysis of variance was used to test for effects of CPP-ACP and etching system on SBS.
Results
Significantly higher mean SBSs were observed in groups subjected to phosphoric acid etching (i.e., groups 1 and 3; p < 0.05). On the other hand, SBSs did not appear to be influenced by CPP-ACP (i.e., groups 3 and 4; p > 0.05). We observed a uniform and clear etched pattern on the enamel surface of the phosphoric acid etching groups.
Conclusions
CPP-ACP does not significantly affect the SBS of orthodontic brackets bonded to non-demineralized teeth, regardless of which adhesive method is used to bond the brackets.
Keywords: CPP-ACP, Shear bond strength, Self-etching primer, Bracket
INTRODUCTION
Casein phosphopeptide amorphous calcium phosphate (CPP-ACP) is a dental product that strengthens and remineralizes teeth while also acting as an anticariogenic agent.1-3 CPP-ACP can dramatically decrease lesion depth and increase both remineralization and mineral content of enamel, thereby improving ratios of both calcium and phosphate.4-7 Both of these minerals form a complex with CPP-ACP on the dental plaque of tooth surfaces, creating a supersaturated state that resists acid challenges and prevents demineralization; the calcium and phosphate ions themselves also enhance remineralization by penetrating the demineralized enamel structure.2,4 Further, enamel surfaces remineralized by CPP-ACP are more resistant to acid challenges with hydroxyapatite of high concentrations of calcium and phosphate ions.8
CPP-ACP application is one of many techniques that have been proposed for simultaneously enhancing remineralization and reducing the occurrence of dental caries and white spot lesions (i.e., the decalcification of enamel that often occurs adjacent to orthodontic brackets).9-11 Such lesions are a significant clinical problem for orthodontists; in one study population, an increase in the number of white spots was observed in 50% of patients who underwent fixed orthodontic treatments.12
There is much interest in using CPP-ACP as a prophylactic for preventing decalcification during orthodontic treatments. However, this will not be feasible if the compound negatively impacts bracket adhesion. Of the 3 phases of the orthodontic adhesion process (i.e., etching, priming, and bonding), the first seems most likely to be impacted by CPP-ACP, which increases mineral content and acid resistance of enamel. Such interference could ultimately reduce the shear bond strength (SBS) of bracket bonding, though the extent of this effect might be expected to vary depending on the type of etching technique employed - for example, phosphoric acid or a self-etching primer can be used, the latter of which combines the etching and priming events into a single step.
We developed the current study to evaluate the effects of both CPP-ACP and different etching processes on the SBS of brackets attached to non-demineralized teeth. We also explored whether SBS was impacted by interactions between these 2 factors.
MATERIALS AND METHODS
Our sample was comprised of 60 human maxillary and mandibular premolars that had been extracted for orthodontic reasons from patients aged between 18 and 28 years; all individuals provided informed consent prior to the study. Teeth were only included in the study if they had an intact buccal surface and were free of caries, cracks, and enamel defects. The teeth were cleaned after extraction and any residual soft tissues were removed. They were then stored in distilled water according to ISO standards 11405/2003. All teeth were tested within 1 month of extraction after being embedded in cold acrylic resin with a mounting jig, such that the labial surface was perpendicular to the bottom of the mold.
Teeth were randomly assigned to 1 of 4 treatment groups (n = 15 each): 35% phosphoric acid + Transbond XT primer + Transbond XT resin (group 1); Transbond Plus Self-etching Primer (TPSEP) + Transbond XT resin (group 2); CPP-ACP paste applied for 2 weeks + 35% phosphoric acid + Transbond XT (group 3); and CPP-ACP paste applied for 2 weeks + TPSEP + Transbond XT resin (group 4).
Teeth in group 1 were etched with 35% phosphoric acid for 15 seconds, washed for 10 seconds, and air-dried. Transbond XT primer was applied and light-cured for 10 seconds. Brackets were bonded with Transbond XT resin. Teeth in Group 2 were treated with TPSEP, which was rubbed on the enamel surfaces for 5 seconds and gently air-dried for 5 seconds. Brackets were bonded with Transbond XT resin. Maxillary premolar metal brackets (Victory Series™ brackets; 3M Unitek, Monrovia, CA, USA) were positioned parallel to the base of the acrylic block. In groups 3 and 4, the teeth were pre-treated with CPP-ACP paste (Toothmousse; GC Co., Tokyo, Japan) for 2 weeks before the brackets were bonded. This protocol was selected because previous work has shown that the remineralizing effects of CPP-ACP last for at least 2 weeks after its application.5,7,13 CPP-ACP was applied twice a day according to the manufacturer's instructions. Three minutes after application, the specimens were stored in artificial saliva in a 37℃ incubator; the saliva was changed daily, and the enamel surface was cleaned with distilled water prior to application of the CPP-ACP paste.
All specimens were stored in artificial saliva for 24 hours in a 37℃ incubator prior to undergoing shear force testing in a universal testing machine with a crosshead speed of 0.5 mm/minute; each trial lasted until bracket failure occurred (Figure 1). Once the debonding was complete, we examined the enamel surface of the tooth under a stereomicroscope at 50 × magnification. We used the modified adhesive remnant index (ARI) to evaluate the amount of residual adhesive on each tooth surface. Classifications were as follows: 1, the entire composite, with an impression of the bracket base, remained on the tooth; 2, > 90% of the composite remained; 3, > 10% but < 90% of the composite remained on the tooth; 4, < 10% of composite remained on the tooth surface; 5, no composite remained on the tooth. We also examined the acid-etched enamel surfaces with scanning electron microscopy (SEM) in order to compare the differences between group1/group2 (no CPP-ACP) and group 3/group 4 (CPP-ACP).
Figure 1.

Shear bond strength test with the Instron machine showing where the debonding force was applied.
We used Levene variance homogeneity and Shapiro-Wilk's tests to investigate the homogeneity of variance and distribution, respectively, of bond strength data. Two-way analysis of variance (ANOVA) tests were used to test for differences between groups and to explore any interactions between CPP-ACP pre-treatment and etching type. A Fisher's exact test was used to evaluate differences in ARI scores between groups. Significance was defined as p < 0.05.
RESULTS
Mean SBS values and standard deviations are shown in Table 1. Bond strength was not significantly affected by pre-treatment with CPP-ACP (Table 2). However, SBS was impacted by etching system. Bond strengths were significantly higher for teeth prepared with phosphoric acid etching (group 1: 18.66 ± 2.31 megapascal [MPa]; group 3: 18.48 ± 2.19 MPa) than with the self-etch adhesive system (group 2: 15.75 ± 1.77 MPa; group 4: 15.51 ± 1.71 MPa) (p < 0.05). CPP-ACP and type of adhesive system did not interact to affect SBS (p > 0.05) (Table 2).
Table 1.
Shear bond strength values (MPa) of the 4 treatment groups
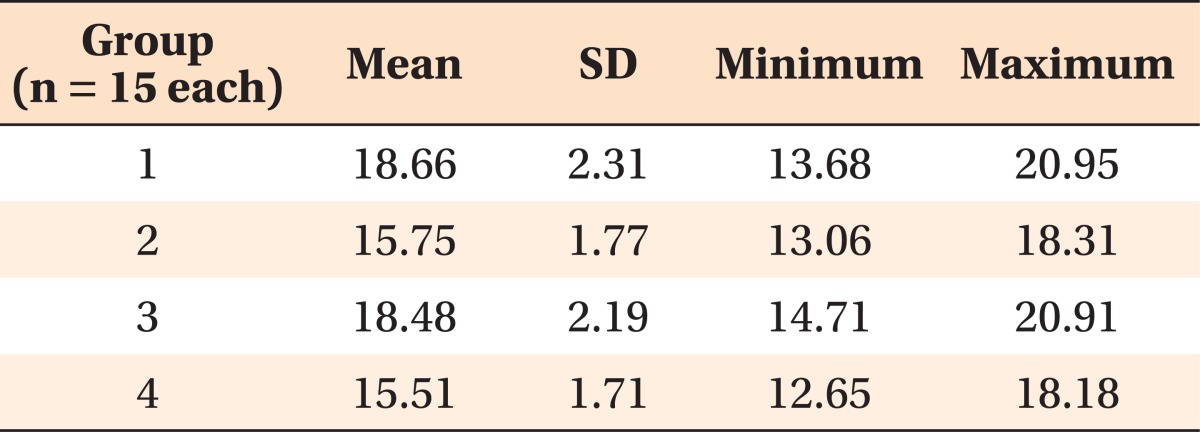
MPa, Megapascal; SD, standard deviation.
Table 2.
Results from two-way ANOVA test investigating the effects of our explanatory variables (presence/absence of CPP-ACP pre-treatment, type of etching system, and the interaction between these) on SBS
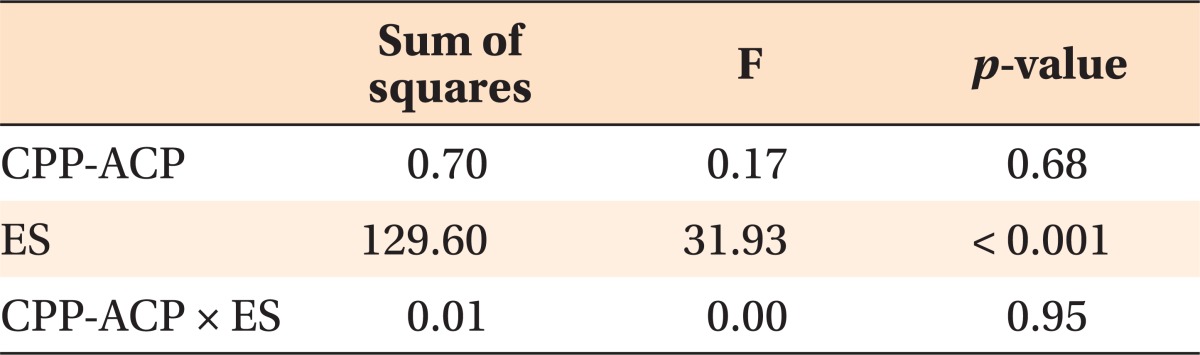
Anova, Analysis of variance; CPP-ACP, casein phosphopeptide amorphous calcium phosphate; SBS, shear bond strength; ES, etching system.
ARI values were similar across all groups (Table 3), though we did notice that the self-etch adhesive system group (group 2 and group 4) tended to display adhesive failure at the enamel/adhesive interface.
Table 3.
Frequency distribution of ARI scores for each of the 4 treatment groups
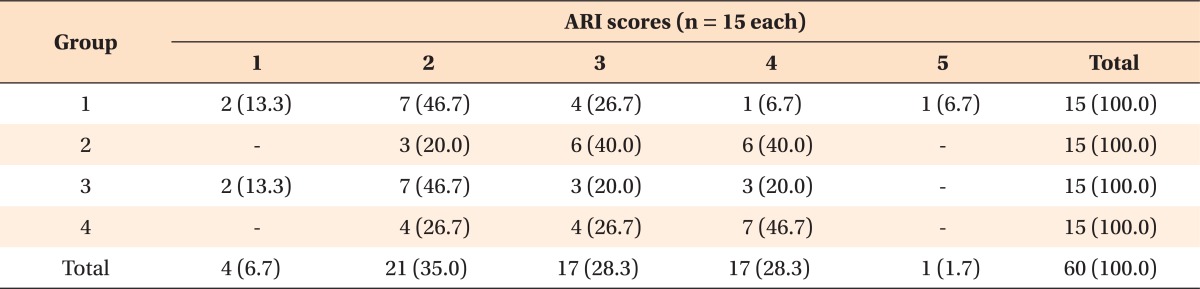
Data are presented as number (% of total). Fisher's exact test; p > 0.05.
Adhesive remnant index (ARI) scores: 1, the entire composite, with an impression of the bracket base, remained on the tooth; 2, > 90% of the composite remained on the tooth; 3, > 10% but < 90% of the composite remained on the tooth; 4, < 10% of composite remained on the tooth; 5, no composite remained on the tooth.
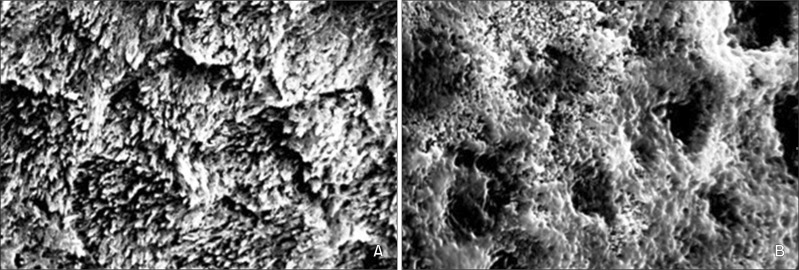
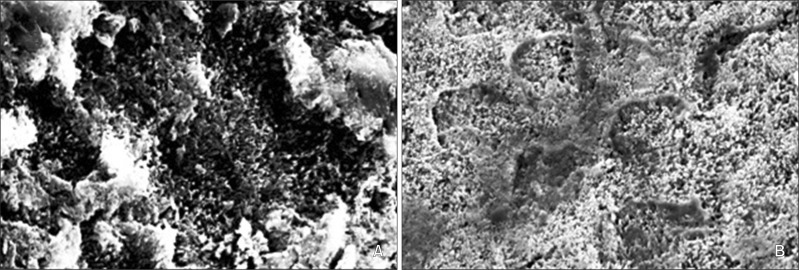
Our SEM analysis revealed no significant difference associated with CPP-ACP preparation. We only noticed different enamel surfaces between the 35% phosphoric acid treatment groups (group 1 and 3) and the TPSEP groups (group 2 and 4) that etching was much more pronounced, uniform, and clear on enamel etched with 35% phosphoric acid, while enamel prepared with TPSEP was characterized by much shallower etching (Figures 2 and 3).
Figure 2.
Scanning electron microscopy images of acid-etched enamel tooth surfaces. A, Surface of a tooth etched with 35% phosphoric acid (×5,000). B, Surface of a tooth etched with Transbond Plus Self-Etching Primer (×5,000).
Figure 3.
Scanning electron microscopy images of acid-etched enamel surfaces after 2 weeks of pre-treatment with casein phosphopeptide amorphous calcium phosphate. A, Surface of a tooth etched with 35% phosphoric acid (×5,000). B, Surface of a tooth etched with Transbond Plus Self-Etching Primer (×5,000).
DISCUSSION
Our results indicate that SBS is impacted more by etching technique than by use of CPP-ACP. This suggests that there will not be negative orthodontic side effects of employing CPP-ACP to reduce the likelihood of decalcification and/or prevent formation of dental caries. This is true regardless of whether teeth are prepared with a phosphoric acid or self-etching primer system, the latter of which appears to be associated with lower SBS.
Our CPP-ACP results are in agreement with previous findings demonstrating that CPP-ACP does not compromise bracket bond strength when a 3-step bonding procedure is used.14-17 In fact, the authors of these studies all suggested that pre-treatment with CPP-ACP before bonding actually increased bracket SBS.14-16 As in the current study, CPP-ACP was used in these instances as a prophylactic prior to bonding. However, because the previous authors stored specimens in distilled water, they were unable to consider the impacts of saliva, which enhances the effectiveness of CPP-ACP.
Demand for a simpler and more effective bonding technique has led to the development of self-etching primers, which are comprised of phosphoric acid and a methacrylate group. When these primers are applied to enamel, the phosphate group dissolves and removes the calcium from the hydroxyapatite, forming a complex that is incorporated into the network during primer polymerization: etching and monomer diffusion occur simultaneously. By decreasing the number of steps required during the adhesion process (e.g., etching, rinsing, and drying), these primers potentially reduce the likelihood of contamination - an important factor deter mining SBS.18 While there is no question that self-etching primers are effective,19-21 SEM examinations of etched enamel have revealed primer-dependent variations in etching patterns. Surfaces etched with 35% phosphoric acid tend to be very porous, characterized by long resin tags and numerous enamel prisms that form a typical honeycomb pattern. Surfaces prepared with TPSEP, on the other hand, have less prominent etching patterns, with short resin tags and very thin hybrid layers.20,22,23
Thus, a combination technique of CPP-ACP pre-treatment (which increases enamel acid resistance and mineral content) and TPSEP etching seemed likely to reduce bracket SBS.
Surprisingly, however, we did not find any evidence that a CPP-ACP pre-treatment reduced SBS for teeth prepared with the self-etch adhesive system (p > 0.05 for a comparison of groups 2 and 4). Additionally, our SEM analysis revealed similar etching patterns in groups that did and did not receive the CPP-ACP pre-treatment (i.e., groups 1 vs. 3/groups 2 vs. 4). These results add to the growing body of literature suggesting that CPP-ACP does not compromise SBS.24-26 However, we did find that mean SBS was higher in the phosphoric acid etching groups (groups 1 and 3) than in the self-etch adhesive system groups (groups 2 and 4; p < 0.05) - an observation also consistent with previous study.27
The higher SBS values reported here were primarily a result of the location at which the debonding force was applied. Klocke and Kahl-Nieke28 noted that SBS dropped by 41.5% when debonding forces were moved from a position close to the enamel to the bracket wing. In vitro conditions are difficult to reproduce in a laboratory set ting because forces would need to be applied from multiple directions at once. Under clinical conditions, bond failures are usually caused by the application of force loads to the wings. To standardize the test as much as possible and to exert a pure shear force, we chose to apply a debonding force to the interface of the bracket and the tooth surface.
CONCLUSION
The use of CPP-ACP did not affect mean SBS, regard less of the adhesive system used to bond brackets to the teeth in our study sample (p > 0.05). All SBS values were clinically acceptable.
Significantly lower SBS values were observed in the groups prepared with the self-etch adhesive system (Group 2: 15.75 ± 1.77 MPa; Group 4: 15.51 ± 1.71 MPa) than in those bonded with phosphoric acid etching (Group 1: 18.66 ± 2.31 MPa; Group 3: 18.48 ± 2.19 MPa) (p < 0.05).
There were no significant differences in the ARI values of the 4 treatment groups. However, the self-etch adhesive system group tended to display adhesive failure at the enamel/adhesive interface.
Enamel etching patterns were similar on teeth that were and were not pre-treated with CPP-ACP.
Based on these results, we conclude that pre-treatment with CPP-ACP does not significantly affect the SBS of orthodontic brackets. Additionally, given the values of SBS observed for the self-etching primer groups, we advocate the use of both this method and 35% phosphoric acid etching for bonding orthodontic brackets.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Reynolds EC, del Rio A. Effect of casein and whey-protein solutions on caries experience and feeding patterns of the rat. Arch Oral Biol. 1984;29:927–933. doi: 10.1016/0003-9969(84)90093-1. [DOI] [PubMed] [Google Scholar]
- 2.Reynolds EC, Cain CJ, Webber FL, Black CL, Riley PF, Johnson IH, et al. Anticariogenicity of calcium phosphate complexes of tryptic casein pho sphopeptides in the rat. J Dent Res. 1995;74:1272–1279. doi: 10.1177/00220345950740060601. [DOI] [PubMed] [Google Scholar]
- 3.Reynolds EC. Anticariogenic complexes of amorphous calcium phosphate stabilized by casein phosphopeptides: a review. Spec Care Dentist. 1998;18:8–16. doi: 10.1111/j.1754-4505.1998.tb01353.x. [DOI] [PubMed] [Google Scholar]
- 4.Choi HJ, Choi YC, Kim KC, Choi SC. Remineralization depth of CPP-ACP on demineralization human enamel in vitro. J Korean Acad Pediatr Dent. 2008;35:278–286. [Google Scholar]
- 5.Shen P, Cai F, Nowicki A, Vincent J, Reynolds EC. Remineralization of enamel subsurface lesions by sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2001;80:2066–2070. doi: 10.1177/00220345010800120801. [DOI] [PubMed] [Google Scholar]
- 6.Kumar VL, Itthagarun A, King NM. The effect of casein phosphopeptide-amorphous calcium phosphate on remineralization of artificial caries-like lesions: an in vitro study. Aust Dent J. 2008;53:34–40. doi: 10.1111/j.1834-7819.2007.00006.x. [DOI] [PubMed] [Google Scholar]
- 7.Zabokova-Bilbilova E, Stafilov T, Sortirovska-Ivkovska A, Sokolovska F. Prevention of enamel demineralization during orthodontic treatment: an in vitro study using GC tooth mousse. Balkan J Stomatol. 2008;12:133–137. [Google Scholar]
- 8.Iijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phos phate. Caries Res. 2004;38:551–556. doi: 10.1159/000080585. [DOI] [PubMed] [Google Scholar]
- 9.White JM, Eakle WS. Rationale and treatment approach in minimally invasive dentistry. J Am Dent Assoc. 2000;131(Suppl):13S–19S. doi: 10.14219/jada.archive.2000.0394. [DOI] [PubMed] [Google Scholar]
- 10.Zero DT, Fontana M, Martínez-Mier EA, Ferreira-Zandoná A, Ando M, González-Cabezas C, et al. The biology, prevention, diagnosis and treatment of dental caries: scientific advances in the United States. J Am Dent Assoc. 2009;140(Suppl 1):25S–34S. doi: 10.14219/jada.archive.2009.0355. [DOI] [PubMed] [Google Scholar]
- 11.Sudjalim TR, Woods MG, Manton DJ. Prevention of white spot lesions in orthodontic practice: a contemporary review. Aust Dent J. 2006;51:284–289. doi: 10.1111/j.1834-7819.2006.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 12.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds EC. Remineralization of enamel subsurface lesions by casein phosphopeptide-stabilized calcium phosphate solutions. J Dent Res. 1997;76:1587–1595. doi: 10.1177/00220345970760091101. [DOI] [PubMed] [Google Scholar]
- 14.Xiaojun D, Jing L, Xuehua G, Hong R, Youcheng Y, Zhangyu G, et al. Effects of CPP-ACP paste on the shear bond strength of orthodontic brackets. Angle Orthod. 2009;79:945–950. doi: 10.2319/101108-573.1. [DOI] [PubMed] [Google Scholar]
- 15.Keçik D, Cehreli SB, Sar C, Unver B. Effect of acidulated phosphate fluoride and casein phosphopeptide-amorphous calcium phosphate application on shear bond strength of orthodontic brackets. Angle Orthod. 2008;78:129–133. doi: 10.2319/122506-529.1. [DOI] [PubMed] [Google Scholar]
- 16.Tabrizi A, Cakirer B. A comparative evaluation of casein phosphopeptide-amorphous calcium pho sphate and fluoride on the shear bond strength of orthodontic brackets. Eur J Orthod. 2011;33:282–287. doi: 10.1093/ejo/cjq062. [DOI] [PubMed] [Google Scholar]
- 17.Uysal T, Baysal A, Uysal B, Aydınbelge M, Al-Qunaian T. Do fluoride and casein phosphopeptide-amorphous calcium phosphate affect shear bond strength of orthodontic brackets bonded to a demineralized enamel surface? Angle Orthod. 2011;81:490–495. doi: 10.2319/090510-520.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buyukyilmaz T, Usumez S, Karaman AI. Effect of self-etching primers on bond strength--are they reliable? Angle Orthod. 2003;73:64–70. doi: 10.1043/0003-3219(2003)073<0064:EOSEPO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Arnold RW, Combe EC, Warford JH., Jr Bonding of stainless steel brackets to enamel with a new self-etching primer. Am J Orthod Dentofacial Orthop. 2002;122:274–276. doi: 10.1067/mod.2002.125712. [DOI] [PubMed] [Google Scholar]
- 20.Bishara SE, VonWald L, Laffoon JF, Warren JJ. Effect of a self-etch primer/adhesive on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2001;119:621–624. doi: 10.1067/mod.2001.113269. [DOI] [PubMed] [Google Scholar]
- 21.Grubisa HS, Heo G, Raboud D, Glover KE, Major PW. An evaluation and comparison of orthodontic bracket bond strengths achieved with self-etching primer. Am J Orthod Dentofacial Orthop. 2004;126:213–219. doi: 10.1016/j.ajodo.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Iijima M, Ito S, Yuasa T, Muguruma T, Saito T, Mizoguchi I. Bond strength comparison and scanning electron microscopic evaluation of three orthodontic bonding systems. Dent Mater J. 2008;27:392–399. doi: 10.4012/dmj.27.392. [DOI] [PubMed] [Google Scholar]
- 23.Triolo PT, Jr, Swift EJ, Jr, Mudgil A, Levine A. Effects of etching time on enamel bond strengths. Am J Dent. 1993;6:302–304. [PubMed] [Google Scholar]
- 24.Al-Twaijri S, Viana G, Bedran-Russo AK. Effect of prophylactic pastes containing active ingredients on the enamel-bracket bond strength of etch- and-rinse and self-etching systems. Angle Orthod. 2011;81:788–793. doi: 10.2319/101210-598.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cehreli SB, Sar C, Polat-Özsoy O, Unver B, Ozsoy S. Effects of a fluoride-containing casein phosphopeptide-amorphous calcium phosphate complex on the shear bond strength of orthodontic brackets. Eur J Orthod. 2012;34:193–197. doi: 10.1093/ejo/cjq183. [DOI] [PubMed] [Google Scholar]
- 26.Adebayo OA, Burrow MF, Tyas MJ. An SEM evaluation of conditioned and bonded enamel following carbamide peroxide bleaching and casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) treatment. J Dent. 2009;37:297–306. doi: 10.1016/j.jdent.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 27.Holzmeier M, Schaubmayr M, Dasch W, Hirschfelder U. A new generation of self-etching adhesives: com parison with traditional acid etch technique. J Orofac Orthop. 2008;69:78–93. doi: 10.1007/s00056-008-0709-6. [DOI] [PubMed] [Google Scholar]
- 28.Klocke A, Kahl-Nieke B. Influence of force location in orthodontic shear bond strength testing. Dent Mater. 2005;21:391–396. doi: 10.1016/j.dental.2004.07.004. [DOI] [PubMed] [Google Scholar]