Abstract
Mobile technologies hold promise for improving diet and physical activity, but little attention is given to creating programs that adolescents like and will use. This study developed a personal digital assistant (PDA) program to promote increased intake of fruits and vegetables (FV) in predominately low-income, ethnic minority girls. This study used a three-phase community-engaged process, including (i) engagement of a Student Advisory Board (SAB) to determine comfort with PDAs; (ii) early testing of Prototype I and rapid re-design by the SAB and (iii) feasibility testing of Prototype II in a new sample of girls. Phase 1 results showed that girls were comfortable with the PDA. Testing of Prototype I in Phase 2 showed that acceptability was mixed, with girls responding to 47.3% of the prompts. Girls wanted more reminders, accountability in monitoring FV, help in meeting daily goals and free music downloads based on program use. The PDA was reprogrammed and testing of Prototype II in Phase 3 demonstrated marked improvement in use (78.3%), increases in FV intake (1.8 ± 2.6 daily servings) and good overall satisfaction. Findings suggest that mobile technology designed with the early input of youth is a promising way to improve adolescent health behaviors.
Introduction
One-third of US children and adolescents are overweight or obese [1]. Overweight and obese children are more likely than normal weight children to experience significant health problems in childhood [2] and are at increased risk for heart disease, diabetes and some cancers in adulthood [3]. Although the prevention and treatment of childhood obesity is a national priority for all children, it is especially important for low-income [4–6] and racial/ethnic minority children. This is especially true for African American girls, who have the highest rates of obesity and the largest rate of increase in obesity—from 16.3% in 1994 to 29.2% in 2007–2008—compared with all other racial/ethnic subgroups [1, 7].
Technology plays an increasingly important role in the lives of adolescents and may be a promising avenue for health interventions. The majority (95%) of girls, 95% of African American youth and 93% of teens from low-income households (<$30 000 per year) are regular online users [8, 9]. A recent review article identified 24 studies that have used electronic media alone or as an adjunct intervention for the prevention and treatment of pediatric obesity [10]. Results from these studies have been mixed, with only three finding a significant reduction in body mass index (BMI) in the electronic intervention group relative to the comparison group [11–13] and 10 reporting no clear impact of the electronic interventions on diet and/or physical activity outcomes [11, 12, 14–21]. Notably, nearly all the studies used the internet or a CD-ROM, with only one using mobile technologies (e.g. text messaging [22]).
Interactive mobile technologies (e.g. cell phone, handheld computers/personal digital assistant [PDA]) have advantages over traditional computer-based approaches. Texting is the preferred method of communication among teens, with the volume of texting increasing from 50 texts per day in 2009 to 60 texts per day in 2011 for the median teen text user [8]. African American teens are leading the increase, with African American teen text users sending a median of 80 texts per day in 2011. Among adolescents, behavioral approaches that incorporate goal setting, self-monitoring, personalized feedback and acquisition of behavior change skills have been found to be more effective than traditional educational strategies for promoting health behavior change [23–25]. Goal setting, self-monitoring and problem solving are the cornerstones of behavior change, but individuals have difficulty implementing and adhering to these principles in their daily lives [23, 26, 27]. The portability and programmability of mobile technologies makes it possible to deliver these elements in ‘real-time’ when they are the most likely to be needed and to be effective. Mobile technologies also have the ability to deliver immediate feedback and point-in-time tips and strategies for problem solving around triggers and barriers, which has been shown to increase the timeliness and accuracy of self-monitoring and the overall relevance and effectiveness of the intervention [28, 29]. Mobile technologies are also proactive. Messages can prompt interaction with the program as opposed to internet-based approaches that rely on the user to initiate use.
Mobile technology interventions for weight loss are in their infancy, although results from existing studies are promising. Studies in adults have found that PDA and text messaging interventions increase self-monitoring and compliance with dietary goals [29], improve diet and physical activity [30, 31] and facilitate weight loss [32]. Formative work with overweight and obese adolescents’ suggests they are enthusiastic about receiving automated messages to improve diet, physical activity and enhance weight loss efforts [33, 34]. Only one known study has been conducted in children, finding that children randomized to use text messaging to monitor their sugar-sweetened beverage, physical activity and screen time behaviors showed significantly greater adherence to self-monitoring and lower attrition at 8 weeks than children randomized to a paper-diary or no-monitoring control conditions [35].
These findings suggest that mobile technologies, particularly those using real time reminder and proactive messaging capabilities, hold promise for improving diet and physical activity in children and adolescents, although careful attention is needed to create programs that adolescents like and will use. Ample evidence suggests a relationship between intervention use and adolescent behavior change [36–41], yet little attention is given to program use in the literature. Of 24 known studies examining electronic pediatric obesity interventions, only seven reported program use and, among them, use was modest, ranging from 33% to 75% [12–14, 18, 41–43]. Community engagement approaches are defined as ‘the process of working collaboratively with groups of people who are affiliated by geographic proximity, special interests, or similar situations with respect to issues affecting their well-being’ [44]. These approaches provide the opportunity for the individuals for whom a program is developed to participate in all phases of development, implementation and evaluation. Community-engaged approaches help to ensure that the program is tailored to meet the needs of those it was designed to help and, subsequently, may enhance acceptability, salience and adoption/use in the target individuals/communities.
Given the promise of mobile technologies and the need to develop effective programs for the prevention of obesity among low-income and ethnic minority girls, the purpose of this study was to develop ‘Growing Up Strong’, a handheld computer program grounded in the behavior modification principles of goal setting, self-monitoring and cues to action, to increase fruits and vegetables (FV) in adolescent girls using a three step process that would maximize usability, appeal and result in a program that had a meaningful impact on behavior. FV were selected as the initial behavioral target because it was of most interest to our community partner, with the goal of later adding other relevant behaviors (e.g. sugar-sweetened beverages and TV/screen time) to a more comprehensive obesity prevention program. The objectives, methods and results of each phase are described, including how results from earlier phases were used to inform program development in subsequent phases.
Contextual background
Community partner
Our community partner throughout this project was The Young Women’s Christian Association (YWCA) of Greater Kansas City. Situated in the heart of Wyandotte County at the juncture between a historically African American neighborhood and an economically deprived downtown area, the YWCA of Greater Kansas City serves the needs of a predominately low-income population. Of 105 Kansas counties, Wyandotte County ranked last (105th) in overall health of its residents in 2009 [45]. Driving forces in this ranking included having the lowest levels of educational attainment and highest rates of unemployment, divorce and children living in poverty of all Kansas counties (105th out of 105). Wyandotte County also had among the highest rates of poor health care, physical inactivity, overweight and obesity and low levels of fruit and vegetable consumption, ranking 101st–103rd out of 105 on these factors [45].
Community advisory board
Initial meetings with the YWCA Executive Director and Women’s and Girls’ Health Education Director solidified the focus on healthy lifestyle programming for adolescent girls and led to the creation of a 12-member Community Advisory Board (CAB). The CAB, comprised YWCA staff, parents, teachers, health care professionals and professionals from other organizations promoting health and wellness among adolescent girls, met to refine the agenda. Through a series of four meetings, a number of themes emerged. First, technology was discussed. CAB members felt that majority of their adolescent population did not have access to cellular telephones, and their families lacked financial resources to support a cell phone plan. Concern was raised about providing cell phones, including girls having unsupervised access to the internet and text messaging and the fact that policies prohibiting cell phones were common and routinely enforced in area schools. Computer/internet strategies were also discussed. The CAB was uncertain about access at home and was concerned about the extent to which girls would use an internet-based program. Third, the group felt it was important to focus on positive behaviors that involved adding components to their lifestyle (e.g. adding FV, milk and water) as opposed to taking things away (e.g. cutting back on calories). The CAB believed that some concepts lent themselves better to their existing health behavior focused programs and to girls’ current knowledge base. Specifically, they felt like FV were tangible and generally easy for girls to recognize, whereas other dietary components (e.g. fat) were harder for girls to understand or recognize in their food.
Diets rich in FV protect against increased adiposity and are promoted for the prevention of childhood obesity because they have low energy density but a high satiety value that replaces the consumption of more popular high fat and calorie foods [46, 47]. More importantly, addressing FV within the context of a program targeting other health behaviors (e.g. sugar-sweetened beverages, screen time and physical activity) is strongly recommended for the prevention of childhood obesity [46]. Development of the FV module, described in detail in this article, was the first of three modules developed for a larger pilot study that is examining the use of handheld computers to attenuate weight gain in low-income, ethnic minority children by targeting FV, sugar-sweetened beverages, and sedentary behaviors.
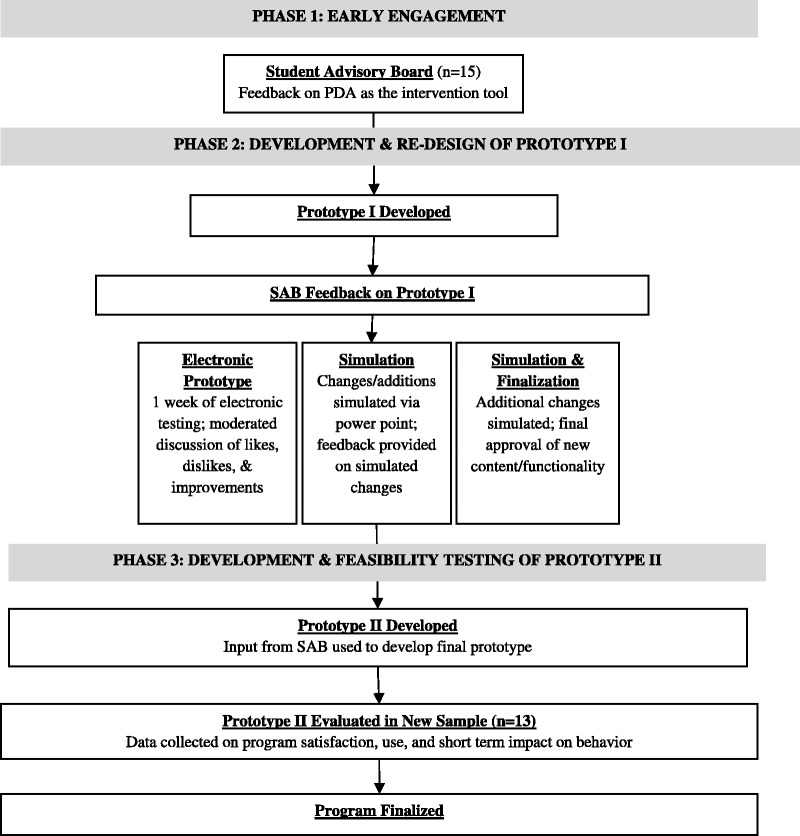
The process of developing the Growing Up Strong FV module is outlined in Figure 1. All study procedures were approved and monitored by the University of Kansas Medical Center Human Subjects Committee.
Fig. 1.
Flow diagram outlining the process of developing the growing up strong handheld computer program.
Phase 1: early engagement
Objective
PDAs were selected as the intervention tool given early input from the YWCA that the majority of girls in the target communities did not have access to cell phones or other mobile technologies (e.g. iPods). To gauge whether this technology would provide similar interest as other, more popular modalities, a Student Advisory Board (SAB) was assembled. The objective of this phase was to use the SAB to determine girls’ comfort with PDA technology and their interest in using this device for future health promotion programming. The SAB was established early in the development process so that they would guide development in all subsequent phases.
Methods
All girls (n = 25) participating in the YWCA summer camp program were invited to participate. Parental consent and child assent was obtained from 15 girls, who were provided with a Asus MyPal A626 with a 3.5 inch LCD, 240 × 320 resolution touch screen (http://www.asus.com/Mobile/MyPal_A626). Because the purpose of this phase of development was to determine girls comfort with PDA technology, devices maintained all the functions of the regular operating system—i.e. access to the music player, calendar, games, Microsoft Word and voice recorder—but did not include the Growing Up Strong program. The 15-member SAB carried their PDA for 2 weeks and at the conclusion of the 2 weeks, participated in a focus group regarding their experience with the technology.
Two focus groups with seven and eight girls each were held on two consecutive evenings. A clinical psychologist with previous training and experience in qualitative interviewing conducted the focus groups. The groups followed a semi-structured format, whereby a standard guide of open-ended questions was used to stimulate thought and discussion about participants experience with the PDA [48]. Specifically, participants’ were asked to describe what they did with the computer, their thoughts about the handheld computer (general and specifics likes/dislikes), access to other mobile technologies and preferred technology modality for future interventions. Groups took approximately 1 hour to complete. The focus groups were audiotaped, transcribed verbatim and then open coded by two independent raters for themes using a grounded theory approach [17]. The two raters then met to discuss the themes and reach consensus; all themes were identical across coders.
The height and weight of each participant was also taken. Height was measured without socks or shoes using a portable stadiometer and rounded to the nearest 0.1 inch. Weight was measured using the Tanita bioimpedance machine (TBF-310 and TBF-300; Tanita Corporation, Arlington Heights, IL). To account for clothing, participant’s weight was adjusted downward by 2 pounds and measured to the nearest 0.1 pound.
Results
Demographics
Girls ranged in age from 8 to 15 years (mean [standard deviation, SD] = 11.9 [2.0]). Eight (53.3%) were black, six (40.0%) were white and one (6.7%) was American Indian/Alaskan Native. Two (13.3%) were Hispanic/Latino. One-third (33.3%) were classified as obese (≥95th BMI percentile) by measured height and weight. Of the 15 girls, one had an MP3 player and four had an iPod and/or a cell phone. The remaining 10 girls reported no access to mobile technologies.
Qualitative feedback
Response to the PDA was overwhelmingly positive. During the moderated group discussion, members of the SAB stated that they thought the device was ‘neat’, ‘fun’, ‘cool’ and ‘easy to use’. They demonstrated their comfort with the technology by describing the diverse ways they used the PDA. SAB members reported that they loaded music on the PDA and listened to songs through the media player, added pictures, played games, beamed notes to each other, wrote poems and other documents using Microsoft Word Mobile and used the voice recording function. The majority (11/15) reported that a PDA was preferred over a cell phone or other mobile technology (e.g. iPod and Nintendo DS) for future health promotion programming.
Phase 2: development and rapid re-design of Prototype I
Development of Prototype I
Given the SABs comfort with PDAs, an initial Growing Up Strong prototype targeting FV intake was developed. Prototype I was grounded in the behavioral weight control principles of goal setting, self-monitoring, personalized feedback and positive reinforcement [23, 26] and capitalized on the potential of a PDA to prompt these behaviors in ‘real-time’. Prototype I had five primary components and functioned as follows (Table I).
Table I.
Growing Up Strong Prototype I and Prototype II program components
| Component | Prototype I | Prototype II |
|---|---|---|
| Education and feedback | - Initial setup provides education about serving sizes of FV | Same as Prototype I |
| - Assessment of FV intake | ||
| - Normative feedback compares current intake to national recommendations and peers | ||
| - Information on health benefits and importance of eating FV | ||
| Goal setting | - Education on goal setting | - Goal setting time parameters expanded to offer wider range of options |
| - Set two daily goals for adding: | ||
| • One serving of fruit to breakfast, lunch, afternoon snack or dinner | - Ability to select different goal times for weekdays and weekends | |
| • One serving of vegetable to breakfast, lunch, afternoon snack or dinner | ||
| - Input time parameters for meal/snack that was chosen (e.g. fruit to breakfast at 8:00 a.m.) | ||
| - Daily goals maintained for 1 week; option to select different goals at the end of 1 week | ||
| Morning general remindera | Not included in Prototype I | - Rings at pre-selected morning time to remind girls of their daily goals, including plan (i.e. tip or recipe) for meeting each goal |
| - Opportunity to select tip in ‘real time’ if one was not selected the night before | ||
| Daily goal remindersa | - Rings at pre-selected goal times to remind girls of chosen goals | Same as Prototype I |
| • ‘Your fruit goal for today is to add a serving of fruit to your breakfast’. | ||
| - Generic tips for meeting the goal included | ||
| • ‘For meeting your goal try to: slice an apple or banana a top it with peanut butter, make dried fruit your snack today … ’ | ||
| Assessment of goal completiona | - Rings 45 min after goal reminder and asks user to assess (yes/no) if they met their goals | Same as Prototype I |
| FV diary | Not included in Prototype I | - Prompts girls to enter all fruits and/or vegetables consumed during assessment of goal completion reminder prompts |
| - Keeps a running total of FV entered and provides feedback on consumption during nightly feedback and goal planning | ||
| Encouragement and problem solving | - Positive indication of goal achievement receives a screen with an encouraging messages | Same as Prototype I |
| • ‘Way to go! Keep up the good work’. | ||
| - Negative indication of goal achievement receives a series of barriers screens | ||
| • Participants select what got it their way from a predetermined list of barriers | ||
| • Each barrier linked to a series of screens that offer specific strategies and tips for that barrier | ||
| Nightly feedback and goal planninga | Not included in Prototype I | - Provides: |
| • Last chance for girls to enter any missed goals and/or missed FV in the food diary | ||
| • Feedback on progress toward goals, e.g. ‘Today you met your fruit goal but not your vegetable goal’. | ||
| • Feedback on daily FV consumption, e.g. ‘You reported eating FV 3 times today. Remember to eat 5 or more servings of FV a day for better health’. | ||
| • Goal planning exercise where girls they selected a tip or recipe for meeting their goals the next day | ||
| - Recipes integrated into the program | ||
| - Tips more kid-friendly and interactive | ||
| - Tips and recipes tailored to each goal, i.e. F or V, and each meal, i.e. breakfast, lunch, afternoon snack and dinner | ||
| Reward system | Not included in Prototype I | - Encourages continued use of the program by enabling girls to earn one song per day: |
| • Girls pre-selected songs | ||
| • Songs encrypted and loaded onto device | ||
| • Program prompted girls to ‘unlock’ one song of their choosing when they responded to 3 out of the 4 daily goal reminder and assessment of goal completion prompts | ||
| Health education | Not included in Prototype I | - Food diary, tips, recipes, barriers and background education/information continually available to girls at the click of a button. |
aRings up to three times over a 6-min period; times out if girl does not respond after the third try.
Education and feedback
Each user went through an initial setup of the program at which time she navigated through a series of screens that provided education about serving sizes of FV, assessment and feedback on her fruit and vegetable intake compared with national recommendations and girls her age, and information on the benefits of eating FV.
Goal setting
Next, she navigated through a series of screens that educated her on goal setting and then asked her to set two weekly goals: one to increase her fruit intake and one to increase her vegetable intake. These goals were linked to meal and snack times (e.g. breakfast and afternoon snack). For example, a girl could select adding a serving of fruit to her breakfast and a serving of vegetables to lunch as her weekly goal. The program also had her input time parameters for the meals chosen as her goal.
Goal reminders
Starting the next day and each subsequent day, the program sounded an audible alarm (like a ringtone) at the pre-selected times to remind her of the goal she had chosen. Accompanying the alarm were a series of screens that displayed generic tips for meeting the specific goal—e.g. ‘Just a reminder that your FRUIT goal for today is to add a serving of fruit to your snack. Try one of these tips for meeting your goal: slice an apple, pear, or banana and top it with peanut butter, have an apple with cheese slices, make dried fruit your snack today.’ The daily reminder alarm sounded up to three times over a 6-min period. Girls clicked through the series of screen and hit ‘done’ at the conclusion of the goal reminder and generic tips message. If no screens had been navigated through after the third try, the program timed out for that reminder.
Goal completion
Approximately 30 min after the goal reminder, a goal completion alarm sounded along with a series of screens that asked the user to assess (yes/no) if they met their goal. As with the daily goal reminders, goal completion reminders sounded up to three times over a 6-min period and timed out after the third try.
Encouragement and problem solving
Girls indicating they met their goal received a screen with an encouraging message—e.g. Way to go! Keep up the good work. Girls indicating they did not meet their goal navigated through a series of barriers screens. The barriers section asked girls to select, from a pre-determined list, what got in their way. Each barrier was linked to a unique series of screens that offered strategies for getting past that particular barrier.
Objective
With a fully functioning prototype developed, the next goal was to allow the SAB to experience the program and to get detailed feedback for improving acceptability, functionality and use.
Methods
A three-stage iterative process was used: First, the SAB was provided with the Growing Up Strong program on a PDA and asked to use the program for 1 week to monitor their FV intake. Whether girls responded to the two goal reminder and the two goal completion alarms was electronically time and date stamped, providing a preliminary estimate of program use. Acceptability was assessed through a moderated group discussion where girls provided feedback on their experience with the program. Second, additions and improvements suggested during the moderated group discussion were simulated through a ‘power point prototype’ and presented to the SAB in subsequent meetings. This simulation maximized efficiency and allowed the SAB to see screen shots of their ideas, approve the changes or provide suggestions for improvements. The simulation approach also provided researchers the opportunity to make sure that the SAB’s ideas were adequately understood and captured before substantial resources were dedicated to re-programming the Growing Up Strong program. Third, additional modifications were again simulated through a ‘power point prototype’. For example, girls suggested enhanced self-monitoring of their FV consumption during the first round of feedback. A FV diary component was simulated during the second round of feedback. Additional changes were suggested, and these changes were again simulated during the third round of feedback. No new changes were suggested during the third round of feedback, therefore this round served as the final beta test of all new content and functionality. This three-stage process took 3 months, beginning in October 2008 and ending in January 2009.
Results
Program use
Whether girls’ responded to the four daily alarms (i.e. two goal reminder and two goal completion) were extracted from time and date-stamped records on the PDA and reflected their mixed reviews of the initial prototype. They completed an average of 47.3% of the 28 prompts (4 prompts/day × 7 days), with use ranging from 20.7% to 72.4%.
Qualitative feedback
Girls liked many aspects of the program, including the goal setting (‘Setting goals helped me stay on track’) and reminder system (‘I liked that we had, um, things set up which reminded us to eat FV … instead of us reminding ourselves, it reminded us’), and they believed that the program had an impact on their behavior ( ‘ … sometimes I eat FV but that device really helped … I got my brother and sister and my mom and my dad eating more FV and they don’t even like ‘em’).
There were also many aspects of the program that girls thought could be improved. Most notably, they wanted more accountability in monitoring their FV consumption (‘I would like to be able to enter how many FV I eats each day and type in which one.’), help in meeting their daily goals (‘Planning ahead for the next day would be helpful’ ‘I eat breakfast at school. These tips don’t work at school’. ‘What about recipes? Those would be helpful.’) and flexibility in the times that the reminders sounded (‘My goal is fruit at breakfast. It goes off at 7:00. That is okay during the week but it is really early on the weekend.’). They also expressed a desire to be rewarded for using the program with songs and/or games that were accessible on their PDA (‘Could I get a song every time I use it? That would be cool. It would help me remember to use it more’).
Phase 3: development and feasibility testing of Prototype II
Development of Prototype II
Substantial revisions were made to the program based on the SAB’s feedback. The revised program retained the original components but included the following new components (Table I).
Morning general reminder
At the pre-selected morning time, the program sent an audible alarm that reminded girls of their two daily goals and the pre-selected plan (i.e. tip or recipe) for meeting each goal. If a tip/recipe was not selected the preceding night, girls were given the opportunity to select a tip for meeting each goal in ‘real time’.
FV diary
At each assessment of goal completion prompt, the program navigated through a series of screens that assisted girls in selecting the fruits and/or vegetables eaten that day. If girls missed the assessment of goal completion prompt, they could enter FV into the diary through the health education screens and/or at nightly feedback and goal planning (described later). The diary kept a running total of the FV entered and, each night, provided feedback on how their daily consumption compared with the national 5-a-Day for Better Health recommendations.
Nightly feedback and goal planning
At the pre-selected evening time, the program sent an audible alarm that prompted girls to navigate through a series of screens. The screens provided a last chance for girls to enter any missed goals and/or missed FV into their diary, feedback on progress toward their goals, e.g. ‘Today you met your fruit goal but not your vegetable goal’, feedback on daily FV consumption, e.g. ‘You ate fruit 3 times today. Remember to eat 5 or more servings of FV a day for better health’ and a goal planning exercise that assisted girls in selecting a tip or recipe for meeting each goal on the proceeding day. Tips and recipes were tailored to each goal, e.g. adding fruit to breakfast tips/recipes were different from adding vegetable to dinner tips/recipes, and included tips that were applicable to meals eaten at school and other away from home settings.
Reward system
A system for earning free music downloads was added to encourage girls’ continued use of the program. The music download system contained 50 songs, pre-selected by the girls that were encrypted and loaded onto the PDA. Girls earned one ‘point’ for responding to each of the two daily goal reminder and two daily assessment of goal completion prompts. Upon responding to three out of four of these daily reminders, the program prompted girls to ‘unlock’ one song of their choosing from the list of 50 encrypted songs. The song was instantly available and ready for play through the media player.
Health education
A health education component was added to the main menu screen. This feature displayed buttons for the food diary, tip/recipes, barriers and education/feedback screens (serving size, benefits and national recommendations for FV), making the information contained in these components of the program continually available to girls at the click of a button.
The functionality of key aspects of the program was also modified. Goal time parameters were expanded to account for the fact that meal times differed on weekdays and weekends. A popular song was used as the audible reminder in place of the standard PDA chime. This change served two functions: it had more appeal to the girls who thought the chime was ‘boring’ and it made the reminder 13 s versus 3 s, which increased the likelihood that girls would hear the reminders and respond. Finally, a graphic designer was hired to create a new look for the program that incorporated brighter colors and images that were more appealing to the girls.
Objective
The final step in the development of Growing Up Strong was to evaluate Prototype II in a new sample of girls. None of the girls from the SAB piloted Prototype II in Phase 3. The primary objective of this phase was to assess program use, acceptability and satisfaction. A secondary objective was to evaluate the impact of the program on FV intake and behavior change skills (e.g. self-monitoring, goal setting and goal planning).
Methods
All girls participating in a program run by a YWCA community partner in the same target communities (predominately low-income, racial/ethnic minorities) were invited to participate. Of 16 girls who expressed interest in participating, parental consent and child assent was obtained from 13 girls, who received Growing Up Strong Prototype II on a PDA (Asus MyPal A626) to monitor their FV intake for 2 weeks.
Program use was assessed at Week 2 through time- and date-stamped records of whether participants responded to the six daily alarms (i.e. two goal reminder, two goal completion, morning general and nightly feedback) that were stored on the PDA.
Acceptability and satisfaction with the overall program and with specific program components were assessed qualitatively through a moderated group discussion of girls’ experience with the program and quantitatively at Week 2 using a modified version of the Health Technology Questionnaire [49]. Responses to the Health Technology Questionnaire are on a 5-point Likert scale with higher scores indicating greater acceptability and satisfaction. There are no pre-existing cutoffs for these questions, and, in an effort to be as descriptive as possible, we chose to report the full range of values as opposed to assigning an arbitrary cutoff to indicate acceptability/satisfaction.
FV intake was measured at baseline and Week 2 using a two-item screener that assesses servings of fruit and servings of vegetables eaten in a typical day. The screener was developed for use in adolescents and has been found to be both reliable and valid, demonstrating adequate test-retest reliability (ICC = 0.68) and significant correlation with 3-day food record data (rs = 0.23, P < 0.01) [50].
Behavior change skills were assessed using the 15-item Fruit & Vegetable Change Strategies Questionnaire [51]. Items assess thoughts (‘I think about the benefits I will get from eating FV’) and activities (‘I set goals to eat at least five servings of FV a day’) commonly used when making a behavior change. The scale was developed for use in adolescents and has demonstrated high internal consistency (Cronbach’s α = 0.86–0.91) and test–retest reliability (ICC = 0.74–0.76) [51, 52].
Results
Girls (n = 13) ranged in age from 9 to 13 years (mean [SD] = 10.8 [1.5]). Twelve (92.3%) were black, and one (7.7%) was white. The majority (53.8%) were classified as overweight (23.0%; 85th to <95th BMI percentile) or obese (30.8%; ≥95th BMI percentile) according to measured height and weight.
Program use
Girls’ completed an average of 78.3% of the 84 prompts (6 prompts/day x 14 days), with use ranging from 43.3% to 97.6%. Evaluation of use by prompt type indicated high completion rates for all prompts. Specifically, girls completed 95.8% of the morning general reminders, 83.3% of the fruit goal reminders, 71.0% of the vegetable goal reminders, 95.8% of the fruit goal completion prompts, 95.8% of the vegetable goal completion prompts and 87.5% of the nightly feedback/goal-planning reminders. In addition, they used the FV diary 1.9 times per day (SD = 0.64) to enter an average of 5.4 (SD = 2.1) FV into their diary.
Program acceptability and satisfaction
Participants’ satisfaction with the overall program and ratings of specific components are listed in Table II. Girls were satisfied with the program (mean [SD] = 3.5 [1.3]) and found it helpful (mean [SD] = 4.1 [1.0]) and engaging (mean [SD] = 4.5 [0.80]). Individual components were also rated favorably, with girls feeling that the components were helpful (range = 3.5 [1.6]–3.8 [1.4]) and had an impact on their behavior (range = 3.5 [1.4]–4.1 [1.3]).
Table II.
Evaluation of the revised Growing Up Strong program (Prototype II) among a new sample of girls (n = 13)
| Acceptability and satisfaction | Mean (SD) | |||
|---|---|---|---|---|
| Overall ratings of the program | ||||
| Satisfaction (1 ‘Dissatisfied’ and 5 ‘Satisfied’) | 3.5 (1.3) | |||
| Helpfulness (1 ‘Not at all’ and 5 ‘Very’) | 4.1 (1.0) | |||
| Engaging (1 ‘Boring’ and 5 ‘Interesting’) | 4.5 (0.8) | |||
| User friendly (1 ‘Unfriendly’ and 5 ‘Friendly’) | 3.9 (1.1) | |||
| Repetitious (1 ‘Not at all’ and 5 ‘Very’) | 3.5 (1.3) | |||
| Ratings of specific program component (1 ‘Not at all’ and 5 ‘A lot’) | ||||
| FV feedback | ||||
| Helpful | 3.7 (1.1) | |||
| Impacted behavior | 3.9 (1.0) | |||
| Setting goals | ||||
| Helpful | 3.7 (1.4) | |||
| Impacted behavior | 4.1 (1.3) | |||
| Reminder system | ||||
| Helpful | 3.8 (1.4) | |||
| Impacted behavior | 3.9 (1.3) | |||
| Tips | ||||
| Helpful | 3.5 (1.6) | |||
| Impacted behavior | 3.5 (1.4) | |||
| FV intake and use of behavior change skills | ||||
|---|---|---|---|---|
| Pre-test, mean (SD) | Post-test, mean (SD) | Change, mean (SD) | P | |
| FV daily servings | 4.0 (2.3) | 5.6 (2.8) | 1.8 (2.6) | 0.03 |
| Number of behavior change skills used | 8.4 (4.3) | 10.7 (4.2) | 2.3 (3.9) | 0.05 |
During the qualitative interviews, girls reported what they liked about the program and what improvements they would suggest to make it more appealing to other girls their age. Girls liked the free music download system, food diary, nightly planning/feedback component, the wide selection of tips and recipes and the program reminders them to eat FV. They also stated that the screens and graphics were ‘cool’. One girl said, ‘I liked the music best and how I could earn more songs by just listening for it to ring’. Another said, ‘My favorite part about the Growing Up Strong program is it teaches you how to eat healthy and I know it sounds a little weird, but it actually kind of saves your life’. Another said, ‘I liked how you gave the recipes and how there was a wide variety and how you could choose between if you wanted a tip or a recipe … ’ Someone else said, ‘Entering your FV was motivating. I used the diary a lot. Our momma would be like “Did you put your vegetables in your food diary”’. Another girl said, ‘Um, I like how if you miss some screens you can go through them at the end of the day’. Girls had few suggestions for improving the program. The two suggestions noted were getting a song for responding to every prompt and being able to enter all their foods, not just FV, into the diary.
FV intake and use of behavior change skills
The impact of the program on FV consumption and use of behavior change skills is presented in Table II. Girls increased their FV consumption from 4.0 (2.3) daily servings at baseline to 5.6 (2.8) daily servings at Week 2 (P < 0.05). They used an average of 8.4 (4.3) behavioral skills to remind them to eat FV at baseline and 10.7 (4.2) behavioral skills at Week 2 (P = 0.05). Of the skills specifically targeted by Growing Up Strong, 62% reported setting a goal to eat 5 FV a day at baseline versus 77% at Week 2; 39% reported keeping track of how many FV they ate at baseline versus 69% at Week 2; 69% found a way to get around barriers to eating FV at baseline versus 77% at Week 2 and 39% made a plan to eat FV at baseline versus 54% at Week 2.
Discussion
The purpose of this study was to develop a handheld computer program grounded in behavior modification principles (goal setting, self-monitoring and cues to action) through an iterative process that involved girls throughout all phases of development. Our process was successful, resulting in a program that girls liked and used to make meaningful changes in their FV intake. Specifically, the three-stage approach greatly enhanced usability and appeal, with use jumping from 47% with Prototype I (pre-SAB feedback) to 78% with Prototype II (post-SAB feedback). Usage rates found in this study are higher than the 50% average use reported for similar programs in the literature [16–18, 22, 45–47]. Findings indicate the importance of engaging youth throughout all phases of program development and provide a platform for the development of future technology-based adolescent health promotion interventions.
Although it is not possible to pinpoint the specific device improvement that led to increased use, it is important to note that working with the SAB lead to substantial revisions in the Prototype I and II Growing Up Strong program. It was critical for the SAB to experience an early version of the program, which helped ground their feedback and provided them a clearer idea of how the program could function to make it more relevant to their lives. It was also critical for girls to see simulations by Microsoft Power Point of suggested modifications, which enabled them to experience their suggested changes in a timely fashion and resulted in a rapid re-design of the appearance and functionality of key components. Many of the changes suggested by the SAB, especially the free music download reward system and prompts that increased accountability (e.g. FV diary) and monitoring (e.g. the two added daily prompts), would not have been considered by the research team without this vital feedback. Seemingly small changes, like using a popular song as the reminder ring tone or providing a system for earning music, were important to the girls and likely helped to enhance use and appeal.
Findings also suggest that mobile technology designed with the early input of youth may be a promising way to improve adolescent health behaviors. Girls increased their use of crucial skills for successful behavior change, e.g. goal setting and goal planning [23, 26], and their FV consumption by 1.8 daily servings. Given that small to moderate (0.5–1.0 servings per day) increases in FV consumption have been associated with decreased risk of cardiovascular disease and some cancers [53–56], the increase seen in this study could represent a clinically meaningful finding if changes are sustained over time. These findings are particularly meaningful when considered within the context of our sample of low-income, predominately African American girls who have the highest risk for obesity but for whom few effective interventions currently exist [7].
Of note, although the PDAs used in this study are still available for purchase, the technology is outdated. However, the primary implications of this study are not in the technology modality but rather in what the technology does. Modern devices (e.g. Smartphones, iPad, Nook and iTouch) have exploded onto the marketplace and with them have come applications (apps) that third parties, including researchers, are able to create and distribute through online stores. There are currently over 500 000 apps available on iTunes and an estimated 7000 apps devoted to health-related topics [57–59]. A search of iTunes on 26 April 2012 for combined diet and fitness apps identified no apps available for download for children, 3 apps for teens and 29 apps for adults. Examination of these 32 apps found that six had a goal-setting component (e.g. setting a calorie, physical activity or weight loss goal) but did not facilitate other essential skills for behavior modification (e.g. reinforcement and problem solving). More importantly, all but one of the existing apps failed to capitalize on a cornerstone of behavior change—the ability of these technologies to provide periodic prompts and reminders that serve as cues to act. A systematic review of minimal contact interventions targeting weight loss, physical activity and/or diet found that of 19 studies that had used technology (i.e. reminder phone calls and text messages) to prompt action, 11 found periodic prompts to be beneficial to weight loss behaviors [60]. A recent study of smartphone applications for physical activity found that participants rated goal setting and problem solving as two of the most notably missing but needed features in existing smartphone apps [61]. Growing Up Strong is the first known program that is rooted in behavior change theory and takes full advantage of the potential of modern devices ‘to prompt the user’ to set goals, make a plan for meeting those goals, self-monitor and assess progress. Growing Up Strong could be easily adapted to other platforms (e.g. smartphone/tablet apps and iTouch) and provides some of the first evidence to support the potential effectiveness of emerging health programs that are being developed for these platforms. Our preliminary findings provide a template for developing apps that address dietary change and suggest that adolescent girls like and will use a device that prompts actions toward specified goals.
The limited access of our sample to cell phones is not unique and is likely driven by age. The mean age of our SAB was 11.9 years. Nationally, only 3% of children younger than 10 years, 6% of 10-year olds and 11% of 11-year olds have a cell phone, with the majority (46%) not receiving their first cell phone until the age of 12 or 13 years [8, 62]. These findings raise interesting questions about the use of non-cellular mobile technologies for engaging tweens, especially low-income tweens, in health promotion programs. Possibilities include the iTouch, which functions in many of the same ways as an iPhone but without calling/text messaging capabilities and with access to the internet only where WiFi is available. For our community, who was concerned about providing girls unsupervised access to the internet and the costs of a cellular phone plan, this device represents a viable option. For communities where cell phone access is not a concern, it is possible to set up some smartphones on a prepaid plan, which would eliminate costly monthly talk/data/text charges that range from $55 to $170/month. Research in this area is still expensive, however, and researchers wanting to work with tweens and those in low-income communities must consider the equipment costs (∼$200/device). In addition, this study found that free music downloads greatly enhanced use. Although a free music download system not be necessary, researchers choosing this option must consider the added cost of $99–$1.99/song.
Results should be interpreted with caution given the small sample size and the study being insufficiently powered to detect statistically significant effects. The free music download system may be cost-prohibitive outside of the research setting and limits wide-scale translation and use. Similarly, PDAs are an outdated technology; however, the functionality of Growing Up Strong and its application to other mobile platforms is highly relevant as discussed in detail earlier. Other limitations include the overall costs of work in this area, which may be especially cost prohibitive for those choosing to work with tweens who do not have access to cell phones or in low-income communities where access to mobile technologies may be less common. The program’s focus on FV only, short-term follow-up and use of a two-item screener to measure FV intake are other limitations that are currently being addressed in an ongoing pilot randomized control trial of the Growing Up Strong program. In the trial, 50 girls (25 per arm) are being randomized to receive three months of the Growing Up Strong PDA program addressing FV (1 month), sugar-sweetened beverages (1 month) and TV/screen time (1 month) or a paper manual control condition. The primary outcome is change in BMI post-treatment (Month 3). Secondary outcomes include change in FV and sugar-sweetened beverage consumption, objectively measured using standardized 24-hour dietary recall methods, and change in screen time, measured using a standardized questionnaire [63, 64]. Findings from the pilot randomized trial will provide a more definitive test of the feasibility (e.g. program use), acceptability (e.g. satisfaction) and effectiveness of mobile technologies for improving health behaviors among low-income, racial/ethnic minority girls.
Conclusions
Early engagement of youth in the development of Growing Up Strong allowed for rapid re-design that enhanced usability, appeal and resulted in program that had a meaningful impact on short term FV consumption. Although further work is needed to examine longer term use of Growing Up Strong and its impact on BMI and related health behaviors, preliminary findings suggest that mobile technologies designed with the early input of youth may be a promising way to improve the health behaviors of low-income, racial/ethnic minority girls at highest risk for obesity. Growing Up Strong is the first known program that is rooted in behavior change theory and takes full advantage of the potential of modern devices to prompt the user to set goals, make a plan for meeting those goals, self-monitor and assess progress. Our preliminary findings provide a template for developing smartphone apps that address dietary change and suggest that adolescent girls like and will use a device that prompts actions toward specified goals.
Funding
The Office of Research on Women’s Health at the National Institutes of Health (K12 HD052027); the National Heart Lung and Blood Institute at the National Institutes of Health (K23 HL090496).
Conflict of interest statement
None declared.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Whitlock EP, et al. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–44. doi: 10.1542/peds.2005-0242. [DOI] [PubMed] [Google Scholar]
- 3.Bergstrom A, et al. Overweight as an avoidable cause of cancer in Europe. Int J Cancer. 2001;91:421–30. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1053>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 4.Drewnowski A, et al. Poverty and childhood overweight in California Assembly districts. Health Place. 2009;15:631–5. doi: 10.1016/j.healthplace.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol. 2010;20:40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Skelton JA, et al. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–9. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freedman DS, et al. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity. 2006;14:301–8. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 8.Lenhart A. Teens, Smartphones, and Texting. Pew Internet & American Life Project 2012. Available at: http://www.pewinternet.org/Reports/2012/Teens-and-smartphones.aspx. Accessed: 25 July 2012.
- 9.Pew Research Center. Demographics of Teen Internet Users. 2011. Available at: http://www.pewinternet.org/Static-Pages/Trend-Data-(Teens)/Whos-Online.aspx. Accessed: 25 July 2012.
- 10.Nguyen B, Kornman KP, Baur LA. A review of electronic interventions for prevention and treatment of overweight and obesity in young people. Obes Rev. 2011;12:e298–314. doi: 10.1111/j.1467-789X.2010.00830.x. [DOI] [PubMed] [Google Scholar]
- 11.Goran MI, Reynolds K. Interactive multimedia for promoting physical activity (IMPACT) in children. Obes Res. 2005;13:762–71. doi: 10.1038/oby.2005.86. [DOI] [PubMed] [Google Scholar]
- 12.Jones M, et al. Randomized, controlled trial of an internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics. 2008;121:453–62. doi: 10.1542/peds.2007-1173. [DOI] [PubMed] [Google Scholar]
- 13.Doyle AC, et al. Reduction of overweight and eating disorder symptoms via the Internet in adolescents: a randomized controlled trial. J Adolesc Health. 2008;43:172–9. doi: 10.1016/j.jadohealth.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baranowski T, et al. The fun, food, and fitness project (FFFP): the Baylor GEMS pilot study. Ethn Dis. 2003;13:S30–9. [PubMed] [Google Scholar]
- 15.Frenn M, et al. Addressing health disparities in middle school students' nutrition and exercise. J Community Health Nurs. 2003;20:1–14. doi: 10.1207/S15327655JCHN2001_01. [DOI] [PubMed] [Google Scholar]
- 16.Haerens L, et al. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Educ Res. 2006;21:911–21. doi: 10.1093/her/cyl115. [DOI] [PubMed] [Google Scholar]
- 17.Haerens L, et al. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity. 2006;14:847–54. doi: 10.1038/oby.2006.98. [DOI] [PubMed] [Google Scholar]
- 18.Jago R, et al. Fit for Life Boy Scout badge: outcome evaluation of a troop and Internet intervention. Prev Med. 2006;42:181–7. doi: 10.1016/j.ypmed.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Long JD, Stevens KR. Using technology to promote self-efficacy for healthy eating in adolescents. J Nurs Scholarsh. 2004;36:134–9. doi: 10.1111/j.1547-5069.2004.04026.x. [DOI] [PubMed] [Google Scholar]
- 20.Marks JT, et al. A comparison of Web and print media for physical activity promotion among adolescent girls. J Adolesc Health. 2006;39:96–104. doi: 10.1016/j.jadohealth.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Russ C, et al. The effects of an innovative WWW-based health behavior program on the nutritional practices of tenth grade girls: preliminary report on the Eat4Life program. J Gend Cult Health. 1998;3:121–8. [Google Scholar]
- 22.Schiel R, et al. Long-term treatment of obese children and adolescents using a telemedicine support programme. J Telemed Telecare. 2008;14:13–6. doi: 10.1258/jtt.2007.070504. [DOI] [PubMed] [Google Scholar]
- 23.Cullen KW, Baranowski T, Smith SP. Using goal setting as a strategy for dietary behavior change. J Am Diet Assoc. 2001;101:562–6. doi: 10.1016/S0002-8223(01)00140-7. [DOI] [PubMed] [Google Scholar]
- 24.Hoelscher DM, et al. Designing effective nutrition interventions for adolescents. J Am Diet Assoc. 2002;102(Suppl. 3):S52–63. doi: 10.1016/s0002-8223(02)90422-0. [DOI] [PubMed] [Google Scholar]
- 25.Lytle L. Nutrition education for school-aged children. J Nutr Educ. 1995;27:298–311. [Google Scholar]
- 26.Foreyt JP, Poston WS, 2nd The role of the behavioral counselor in obesity treatment. J Am Diet Assoc. 1998;98:S27–30. doi: 10.1016/s0002-8223(98)00707-x. [DOI] [PubMed] [Google Scholar]
- 27.Foster GD, Makris AP, Bailer BA. Behavioral treatment of obesity. Am J Clin Nutr. 2005;82(Suppl. 1):230S–5S. doi: 10.1093/ajcn/82.1.230S. [DOI] [PubMed] [Google Scholar]
- 28.Koop A, Mosges R. The use of handheld computers in clinical trials. Control Clin Trials. 2002;23:469–80. doi: 10.1016/s0197-2456(02)00224-6. [DOI] [PubMed] [Google Scholar]
- 29.Glanz K, et al. Improving dietary self-monitoring and adherence with hand-held computers: a pilot study. Am J Health Promot. 2006;20:165–70. doi: 10.4278/0890-1171-20.3.165. [DOI] [PubMed] [Google Scholar]
- 30.King AC, et al. Promoting physical activity through hand-held computer technology. Am J Prev Med. 2008;34:138–42. doi: 10.1016/j.amepre.2007.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Atienza AA, et al. Using hand-held computer technologies to improve dietary intake. Am J Prev Med. 2008;34:514–8. doi: 10.1016/j.amepre.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 32.Patrick K, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res. 2009;11:e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woolford SJ, et al. OMG do not say LOL: obese adolescents' perspectives on the content of text messages to enhance weight loss efforts. Obesity (Silver Spring) 2011;19:2382–7. doi: 10.1038/oby.2011.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Woolford SJ, et al. Tailored mobile phone text messages as an adjunct to obesity treatment for adolescents. J Telemed Telecare. 2010;16:458–61. doi: 10.1258/jtt.2010.100207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shapiro JR, et al. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nutr Educ Behav. 2008;40:385–91. doi: 10.1016/j.jneb.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Birnbaum AS, et al. Are differences in exposure to a multicomponent school-based intervention associated with varying dietary outcomes in adolescents? Health Educ Behav. 2002;29:427–43. doi: 10.1177/109019810202900404. [DOI] [PubMed] [Google Scholar]
- 37.Huhman ME, et al. Evaluation of a national physical activity intervention for children: VERB campaign, 2002-2004. Am J Prev Med. 2007;32:38–43. doi: 10.1016/j.amepre.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 38.Resnicow K, et al. Results of go girls: a weight control program for overweight African-American adolescent females. Obes Res. 2005;13:1739–48. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 39.Resnicow K, et al. GO GIRLS!: results from a nutrition and physical activity program for low-income, overweight African American adolescent females. Health Educ Behav. 2000;27:616–31. doi: 10.1177/109019810002700507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson D, et al. Food, Fun and Fitness Internet program for girls: influencing log-on rate. Health Educ Res. 2007;23:228–37. doi: 10.1093/her/cym020. [DOI] [PubMed] [Google Scholar]
- 41.Thompson D, et al. Food, fun, and fitness internet program for girls: pilot evaluation of an e-Health youth obesity prevention program examining predictors of obesity. Prevent Med. 2008;47:494–7. doi: 10.1016/j.ypmed.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 42.Williamson DA, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity. 2006;14:1231–43. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 43.White MA, et al. Mediators of weight loss in a family-based intervention presented over the internet. Obes Res. 2004;12:1050–9. doi: 10.1038/oby.2004.132. [DOI] [PubMed] [Google Scholar]
- 44. Principles of Community Engagement Second Edition. Washington, DC: U.S. Government Printing Office, 2011. Available at: http://www.atsdr.cdc.gov/communityengagement/pdf/PCE_Report_508_FINAL.pdf. Accessed: 27 August 2012.
- 45.Pezzino G. Kansas County Health Rankings 2009. Topeka, KS: Kansas Health Institute; 2009. [Google Scholar]
- 46.Davis MM, et al. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl. 4):S229–53. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 47.Field AE, et al. Association between fruit and vegetable intake and change in body mass index among a large sample of children and adolescents in the United States. Int J Obes Relat Metab Disord. 2003;27:821–6. doi: 10.1038/sj.ijo.0802297. [DOI] [PubMed] [Google Scholar]
- 48.Bernard H. Research Methods in Anthropology: Qualitative and Quantitative Approaches. 3rd edn. Walnut Creek, CA: AltaMira Press; 2002. [Google Scholar]
- 49.Farzanfar R. Health e-Technologies Initiative—Building the Science of e-Health. Health technology questionnaire. Robert Wood Johnson Foundation, 2005. Available at: http://www.hetinitiative.org/grantee_instruments/BU%20Health%20Technologies%20Questionnaire%204.27.05.A.pdf. Accessed: 27 August 2012. [Google Scholar]
- 50.Prochaska JJ, Sallis JF. Reliability and validity of a fruit and vegetable screening measure for adolescents. J Adolesc Health. 2004;34:163–5. doi: 10.1016/j.jadohealth.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 51.Hagler AS, et al. Comparability and reliability of paper- and computer-based measures of psychosocial constructs for adolescent fruit and vegetable and dietary fat intake. J Am Diet Assoc. 2005;105:1758–64. doi: 10.1016/j.jada.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 52.Patrick K, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2001;155:940–6. doi: 10.1001/archpedi.155.8.940. [DOI] [PubMed] [Google Scholar]
- 53.Genkinger JM, et al. Fruit, vegetable, and antioxidant intake and all-cause, cancer, and cardiovascular disease mortality in a community-dwelling population in Washington County, Maryland. Am J Epidemiol. 2004;160:1223–33. doi: 10.1093/aje/kwh339. [DOI] [PubMed] [Google Scholar]
- 54.Hung HC, et al. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004;96:1577–84. doi: 10.1093/jnci/djh296. [DOI] [PubMed] [Google Scholar]
- 55.Joshipura KJ, et al. The effect of fruit and vegetable intake on risk for coronary heart disease. Ann Intern Med. 2001;134:1106–14. doi: 10.7326/0003-4819-134-12-200106190-00010. [DOI] [PubMed] [Google Scholar]
- 56.Liu S, et al. Fruit and vegetable intake and risk of cardiovascular disease: the Women's Health Study. Am J Clin Nutr. 2000;72:922–8. doi: 10.1093/ajcn/72.4.922. [DOI] [PubMed] [Google Scholar]
- 57.Boulos MN, et al. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online. 2011;10:24. doi: 10.1186/1475-925X-10-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Free C, et al. The effectiveness of M-health technologies for improving health and health services: a systematic review protocol. BMC Res Notes. 2010;3:250. doi: 10.1186/1756-0500-3-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kailas A, Chong CC, Watanabe F. From mobile phones to personal wellness dashboards. IEEE Pulse. 2010;1:57–63. doi: 10.1109/MPUL.2010.937244. [DOI] [PubMed] [Google Scholar]
- 60.Fry JP, Neff RA. Periodic prompts and reminders in health promotion and health behavior interventions: systematic review. J Med Internet Res. 2009;11:e16. doi: 10.2196/jmir.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rabin C, Bock B. Desired features of smartphone applications promoting physical activity. Telemed J E Health. 2011;17:801–3. doi: 10.1089/tmj.2011.0055. [DOI] [PubMed] [Google Scholar]
- 62.Lenhart A, et al. Teens and Mobile Phones: Text Messaging Explodes as Teens Embrace It as a Centerpiece of Their Communication Strategies with Friends. Pew Internet & American Life Project 2010. Available at: http://pewinternet.org/Reports/2010/Teens-and-Mobile-Phones.aspx. Accessed: 28 August 2012.
- 63.Robinson TN. Reducing children's television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–7. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 64.Schmitz KH, et al. Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. J Sch Health. 2004;74:370–7. doi: 10.1111/j.1746-1561.2004.tb06632.x. [DOI] [PubMed] [Google Scholar]