Abstract
Objective
Recent randomised clinical trials among stable HIV sero-discordant couples (SDCs) in sub-Saharan Africa (SSA) have reported that about 20–30% of new HIV infections are acquired from external sexual partners, rather than transmitted from the infected to the uninfected partner within the couple. The aim of this study is to examine whether, and to what extent, these findings are generalisable to SDCs in the wider population in SSA.
Methods
A mathematical model was constructed to calculate the fraction of new HIV-1 infections among SDCs that are due to sources external to the couple. The model was parameterised using empirical and population-based data for 20 countries in SSA. Uncertainty and sensitivity analyses were also conducted.
Results
The contribution of external infections among SDCs was generally modest, but it varied widely across SSA. In low HIV prevalence countries (≤3.0%), it ranged from 0.6–2.9%. In intermediate prevalence countries (3.0–18.0%), it ranged from 4.9–11.7%. In Swaziland and Lesotho, the world's most-intense epidemics, sizable levels of 27.9% and 27.3% were found, respectively.
Conclusions
In most countries in SSA, nearly all HIV acquisitions by the uninfected partners in SDCs appear to be due to transmissions from the HIV infected partners in the SDCs. The contribution of externally acquired infections varies with HIV population prevalence, but rarely exceeds 10% in the majority of countries. Only in hyperendemic HIV epidemics the contribution of external infections is substantial and may reach the levels reported in recent randomised clinical trials involving SDCs.
Keywords: Africa, Epidemiology (General), HIV
Introduction
Recent randomised controlled clinical trials (RCTs) among stable HIV sero-discordant couples (SDCs) have reported that about 20–30% of new HIV infections among these SDCs were acquired from external sexual partners, rather than transmitted from the infected to the uninfected partner within the couple.1 2 In these trials, viral linkages between study-partner pairs were established through phylogenetic analyses and gene sequencing for the C2-V3-C3 regions of the env gene1 or the HIV-1 pol gene.2 The probability of linkage was determined either through measuring the pairwise nucleotide distances between the sequences,1 or by using Bayes’ theorem to compare the genetic similarity of HIV-1 from partner pairs with the genetic similarity of HIV-1 from local control subjects.2
The conditions under which these trials were conducted, with sero-status disclosure and counselling, pose a question about the generalisability of the trials’ findings to other SDCs within the wider population. This issue has recently received much attention in light of the debate about the contribution of HIV sero-conversions among SDCs to the HIV epidemic in sub-Saharan Africa (SSA).3–5 Against this background, we constructed a mathematical model parameterised by state of the art empirical data to calculate the population-level fraction of new HIV-1 infections among SDCs that are due to sources external to the couple in 20 countries in SSA.
Methods
Model structure
The annual risk of HIV transmission from the infected to the uninfected partner within an SDC (φ) is determined by HIV transmission probability per coital act (p), the number of coital acts per year (n), the fraction of coital acts protected by condom use (fcondom), the efficacy of condom use in preventing HIV transmission per sexual act (Econdom), and whether the susceptible partner in the couple is a circumcised male. In a couple where the male is not circumcised, φ is given by:
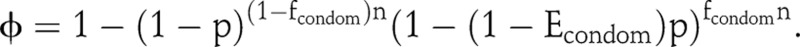
The average φ in the population is determined as a weighted average of the annual risk of HIV transmission among SDCs with and without male circumcision (see supplementary online appendix (SOA)).
Let λ be the annual risk of the HIV sero-negative individual in an SDC to acquire the infection from a source external to the couple. We assume that the annual risk of any susceptible individual in the population to acquire the infection, that is, the hazard rate of infection or incidence rate, is approximately equal among those individuals in stable couples versus those not in stable couples, and is also approximately equal among those in HIV concordant negative couples versus those in SDCs. Accordingly, λ can be approximated by HIV population-level incidence rate. While the strict validity of this assumption is not known, existing empirical data discussed below suggests its plausibility. Moreover, potential violations of this assumption are more likely than not to affirm our conclusion regarding the contribution of external infections. Further considerations regarding this assumption and its variations are in the Discussion section.
Based on this assumption and using competing hazards, that is, comparing the likelihood of acquiring the HIV infection from an external source to the likelihood of acquiring the infection from the infected partner in an SDC, the fraction of new HIV-1 infections among SDCs that are due to sources external to the couple (fext) is given by fext = λ/(λ+φ). Further mathematical derivations can be found in SOA.
Model parameterisation
We used the most recent Demographic and Health Survey (DHS) databases for 20 countries in SSA6 to calculate the country-specific: HIV prevalence (P), fraction of HIV-infected females among the SDCs (findex), fraction of circumcised males in SDCs with HIV-infected females (fmc), and condom use at last sexual act among stable couples (fcondom) (see table S1 in SOA). HIV population-level incidence rate was obtained from the Joint United Nations Programme on HIV/AIDS SPECTRUM model predictions for each country for the specific year of the DHS survey (Gouws E, Joint United Nations Programme on HIV/AIDS (UNAIDS). Personal Communication. 2011).7 For countries where SPECTRUM model predictions are not available, or where the bounds of the 95% CI are not precisely specified, estimates for HIV incidence rate were derived using the DHS country-specific HIV-1 prevalence (SOA). We calculated p as the average from the Rakai Study8 and the Partners in Prevention Study (Hughes JP. Personal communication. 2010),1 9 and derived n from the Rakai Study8 as data on frequency of coital acts were not available in the DHS databases from which we derived these measures. We opted to use n in the Rakai Study because this choice implies values for φ that are consistent with the existing empirical measures, and in fact are at the mid-range of these estimates.8–10 Further discussion of the model parameters can be found in SOA.
Uncertainty and sensitivity analyses
An uncertainty analysis was conducted to generate country-specific likelihood distributions for fext using Monte Carlo sampling from the uncertainty ranges of p, n, country-specific λ, country-specific findex, country-specific fmc, country-specific fcondom, Econdom, and the efficacy of male circumcision in preventing HIV acquisition among susceptible males (Emc). The distributions were used to calculate the country-specific means and 95% CIs of fext across SSA. Further description of the uncertainty analysis can be found in SOA.
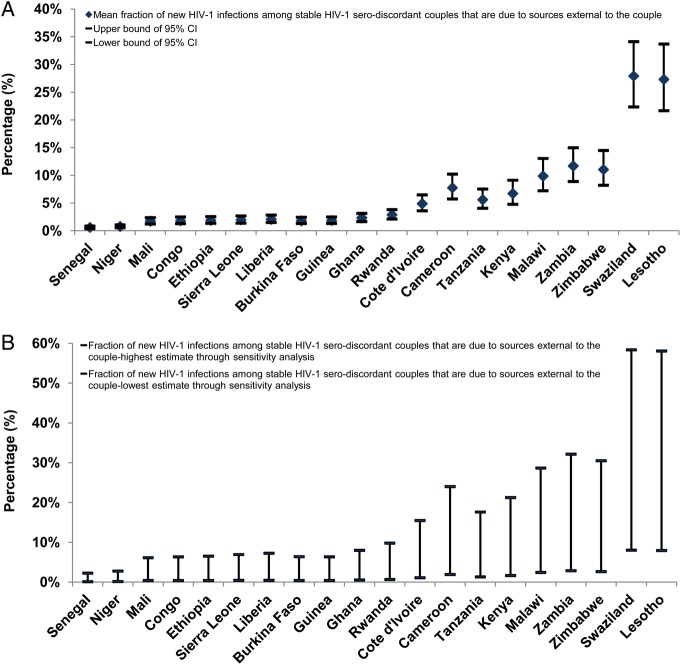
To explore the impact of alternative assumptions to our model assumptions, we conducted a sensitivity analysis for fext by varying φ and λ over a range starting from half to twice the values for these measures (figure 1B). We also conducted an additional sensitivity analysis where we examined the variation of fext across a spectrum of values for λ and φ (section IV and figure S1 of SOA).
Figure 1.
Fraction of new HIV-1 infections among stable HIV-1 sero-discordant couples that are due to sources external to the couple (fext) across sub-Saharan Africa (SSA). (A) Country-specific means and 95% CIs for fext across 20 countries in SSA. (B) Country-specific ranges for fext using a sensitivity analysis on our model assumptions. Countries are shown in order of increasing HIV-1 prevalence. This figure is only reproduced in colour in the online version.
Results
Figure 1A and online supplementary table S1 show the estimates for the country-specific fext. In low HIV prevalence countries (≤3.0%), fext had a range of 0.6–2.9%. In intermediate prevalence countries (3.0–18.0%), the range was 4.9–11.7%. In Swaziland and Lesotho, the world's most-intense epidemics, high levels of 27.9% and 27.3% were found, respectively. The uncertainty analysis showed narrow CIs particularly in low to intermediate HIV prevalence countries (figure 1A). The sensitivity analyses showed that overall fext is unlikely to exceed 30% even with extreme variations in our model assumptions, and that for most countries fext is no more than just few percentage points (figure 1B and figure S1 of SOA).
Discussion
In most countries in SSA, nearly all new HIV acquisitions by the uninfected partners in SDCs appear to be due to transmissions from the HIV infected partners in the SDCs. The contribution of external infections to SDCs is minimal and substantially lower than what has been observed recently in RCTs involving SDCs.1 2
However, the risk of HIV acquisition from external partners varies across SSA, and depends strongly on HIV prevalence in the population (figure 1). While less than 3% of HIV infections are from external partners in low prevalence countries, as much as 12% of infections are externally acquired in intermediate prevalence countries. Moreover, in the high-prevalence countries of Swaziland and Lesotho, the contribution of external partnerships reaches sizable levels, comparable to those measured in the RCTs.1 2 These findings were found robust to the limitations in our knowledge of some of the model parameters as the uncertainty analysis in figure 1A demonstrates.
We have tested our model by applying it to a specific site with robust empirical data: Rakai, Uganda. Our estimate for fext in Rakai agreed nicely with the data from the Rakai Study. In this setting, HIV population-level incidence rate (λ) was reported to be 1.5 per 100 person-years,11 and the annual risk of HIV transmission within an SDC (φ) to be 9.2 per 100 person-years.12 Accordingly using our model, the contribution of external infections to HIV incidence among SDCs is estimated at 14%. Phylogenetic analysis was performed in the Rakai Study, by sequencing the gag (p24) and gp41 regions, to establish the level of HIV viral linkage within the couples, and accordingly estimate fext.13 It was found that 86% of HIV transmissions were strongly or moderately linked.13 This suggests that fext is of the order of 15%, a value that is, in close agreement with our estimate.
The strong dependence of fext on HIV prevalence is easily understood considering that λ depends on the likelihood of forming a partnership with an HIV infected individual, and that the probability of selecting at random an HIV infected individual in a given population, that is, HIV population prevalence, varies widely across SSA. Indeed, it is 50 times higher in Lesotho, with an HIV prevalence of 23.0%, compared to Senegal, with an HIV prevalence of only 0.5%.
Although φ and λ vary across the countries, these variations had minimal impact on our conclusion that fext is overall small except in countries at high HIV prevalence (see eg, online supplementary figure S1). It bears notice that our country-specific estimates for φ are consistent with available empirical measures and are at the mid-range of the reported values.8–10
Our findings suggest that the values found recently in RCTs1 2 are not representative of the population-based fext in the majority of countries. Sero-status disclosure, intensive counselling, and access to prevention methods may explain the larger fext in RCTs. For instance, sero-disclosure in the Partners in Prevention RCT resulted in a reduction in sexual activity within the SDC and an increased engagement of the uninfected partners in external partnerships.14 This is affirmed by the low HIV incidence rate among SDCs that has been reported in these RCTs (∼2 per 100 person-years),1 2 which is much smaller than that observed in observational studies (∼10 per 100 person-years).8 10 These considerations indicate that the large values of fext reported in these RCTs are on the extreme end of the actual values for fext in the wider population across SSA.
The essential assumption in our methodology is that the risk of infection from external sources does not vary substantially based on the individual's marital status, or engagement in a concordant negative couple versus an SDC. The validity of this assumption is not known, but empirical data from the Rakai Study suggests its plausibility. In Rakai, the risk of HIV acquisition per person was 0.5% (95% CI 0.3% to 0.8%) in round I prior to antiretroviral therapy availability among persons in concordant negative couples, versus 0.7% (95% CI 0.4% to 1.0%) among unmarried persons (over about 14 months of follow-up). These estimates were calculated from the data in Gray et al.5 In round II post antiretroviral therapy availability, it was 0.7% (95% CI 0.5% to 0.9%) versus 1.1% (95% CI 0.8% to 1.4%) (over about 18 months of follow-up). These values suggest that the risk of external infection among persons in stable couples is comparable, though possibly somewhat lower, than those among unmarried persons. If married persons engage in less extra-marital sex than unmarried persons, this would further lower our fext estimates.
On the other hand, it is reasonable to assume that HIV sero-status disclosure can increase the risk of external infection among SDCs in comparison to concordant negative stable couples.14 However, the low levels of condom use at last sex reported by the couples in the DHS databases (table S1 of SOA) suggest that sero-disclosure is rather limited in the wider population in SSA. Hence, the actual current levels of sero-disclosure in SSA are not likely to affect our conclusion.
The risk of acquiring HIV from external sources may vary by age, since HIV incidence rate is strongly dependent on age, and thus may affect our estimates for fext. We examined the age distribution of SDCs across the SSA countries included in our analysis. The mean age of females in SDCs was found overall to be in the range of 25–35 years with an average over countries of 30.5 years. As for males, it was overall in the range of 35–45 years with an average over countries of 38.7 years. These results were invariable regardless of whether the index partner was a female or a male. By comparing these age distributions to empirical measures of HIV incidence-rate age distribution across different settings in SSA,15 16 we found that HIV incidence rate among these SDCs age groups to be substantially lower than that in the younger age groups and comparable to the overall HIV incidence rate. Indeed, close to half of all HIV infections in SSA are among those younger than 25 years of age, and females acquire HIV at an earlier age group than males.15–17 These considerations suggest that it is unlikely that the variability in the age distribution of HIV incidence rate will noticeably affect our analysis.
A fraction of HIV population-level incidence rate arises from the incidence of HIV among SDCs. Eliminating this contribution from HIV population incidence rate would further reduce the likelihood of acquiring HIV from external sources among SDCs and hence lower our estimates for fext. This further suggests that our estimates for fext are more likely to overestimate rather than underestimate the actual contribution of external infections among SDCs.
On balance, the discussion above suggests the overall validity of our assumptions. Moreover, even considerable deviations to these assumptions are not likely to affect our conclusion of modest role for external infections as shown in the sensitivity analyses (figure 1B and online supplementary figure S1).
To sum up, fext varies substantially across SSA, but is generally below 10% in most countries. Only in hyperendemic HIV epidemics the contribution of external infections is sizable and may reach up to 30%. The vast majority of HIV acquisitions among SDCs are transmissions from the infected to the susceptible partner. These findings however should not be over-interpreted to believe that HIV incidence within SDCs dominates HIV incidence in the population.
Key messages.
Nearly all of HIV incidence among stable HIV-1 sero-discordant couples (SDCs) in most countries in sub-Saharan Africa (SSA) appears to be attributed to HIV transmission from the infected to the uninfected partner in the couple.
The fraction of externally acquired HIV infections among stable HIV-1 SDCs strongly depends on HIV prevalence in the population and varies across SSA.
Only in hyperendemic HIV epidemics, the contribution of external infections among stable HIV-1 SDCs is sizable and may reach up to 30%.
Supplementary Material
Acknowledgments
HC and LJA are grateful for the Qatar National Research Fund for primarily supporting this work (NPRP 08-068-3-024).
Footnotes
Contributors: HC managed the DHS databases, conducted the bulk of the statistical and mathematical modelling analyses, and wrote the first draft of the paper. LJA conceived and designed the study and led the analyses and drafting of the article.
Funding: The Qatar National Research Fund (NPRP 08-068-3-024) and the Biostatistics, Epidemiology, and Biomathematics Research Core at the Weill Cornell Medical College—Qatar. Additional support from the National Institutes of Health (R01 AI083034).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Open Access: This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
References
- 1.Celum C, Wald A, Lingappa JR, et al. Acyclovir and transmission of HIV-1 from persons infected with HIV-1 and HSV-2. N Engl J Med 2010;362:427–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med (Multicenter Study Randomized Controlled Trial Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't) 2011;365:493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shelton JD. A tale of two-component generalised HIV epidemics. Lancet 2010;375:964–6 [DOI] [PubMed] [Google Scholar]
- 4.Dunkle K, Stephenson R, Karita E, et al. New heterosexually transmitted HIV infections in married or cohabiting couples in urban Zambia and Rwanda: an analysis of survey and clinical data. Lancet 2008;371:2183–91 [DOI] [PubMed] [Google Scholar]
- 5.Gray R, Ssempiija V, Shelton J, et al. The contribution of HIV-discordant relationships to new HIV infections in Rakai, Uganda. AIDS 2011;25:863–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demographic and health surveys Calverton: ICF Macro; (cited 19 May 2010); http://www.measuredhs.com/
- 7.UNAIDS HIV estimates with uncertainty bounds 1990–2009. 2010. (cited September 2011); http://www.unaids.org/en/dataanalysis/epidemiology/
- 8.Wawer MJ, Gray RH, Sewankambo NK, et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis 2005;191:1403–9 [DOI] [PubMed] [Google Scholar]
- 9.Hughes JP, Baeten JM, Lingappa JR, et al. Determinants of per-Coital-Act HIV-1 infectivity among African HIV-1-Serodiscordant couples. J Infect Dis 2012;205:358–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guthrie BL, De Bruyn G, Farquhar C. HIV-1-discordant couples in sub-Saharan Africa: explanations and implications for high rates of discordancy. Current HIV Research (Article) 2007;5:416–29 [DOI] [PubMed] [Google Scholar]
- 11.Wawer MJ, Sewankambo NK, Serwadda D, et al. Control of sexually transmitted diseases for AIDS prevention in Uganda: a randomised community trial. Rakai project study group. Lancet 1999;353:525–35 [DOI] [PubMed] [Google Scholar]
- 12.Reynolds SJ, Makumbi F, Nakigozi G, et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS (Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural). 2011;25:473–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollingsworth TD, Laeyendecker O, Shirreff G, et al. HIV-1 transmitting couples have similar viral load set-points in Rakai, Uganda. PLoS pathogens (Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.) 2010;6:e1000876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ndase P, Celum C, Thomas K, et al. Outside sexual partnerships and risk of HIV acquisition for HIV uninfected partners in African HIV serodiscordant partnerships. J Acquir Immune Defic Syndr (Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't). 2012;59:65–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hallett TB, Zaba B, Todd J, et al. Estimating incidence from prevalence in generalised HIV epidemics: methods and validation. PLoS Med. (Research Support, Non-U.S. Gov't Validation Studies). 2008;5:e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gouws E, Williams BG, Sheppard HW, et al. High incidence of HIV-1 in South Africa using a standardized algorithm for recent HIV seroconversion. J Acquir Immune Defic Syndr (Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.). 2002;29:531–5 [DOI] [PubMed] [Google Scholar]
- 17.Monasch R, Mahy M. Young people: the centre of the HIV epidemic. World Health Organ Tech Rep Ser 2006;938:15–41 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.