Abstract
Early efforts to use point-of-care clinical decision support (CDS) were limited to the use of prompts and reminders, which improved test ordering but not intermediate outcomes of care such as glucose, blood pressure, or lipid levels. More sophisticated diabetes CDS tools are now available that use electronic medical record data to provide patient-specific advice on medication use based on previous treatment, distance from goal, and other clinical data. These tools have shown modest but significant improvement in glucose and blood pressure control. Promising next-generation developments will include prioritizing clinical actions that have maximum benefit to a given patient at the point of care and developing effective methods to communicate CDS information to patients to better incorporate patient preferences in care decisions.
Keywords: health informatics, electronic health records, chronic disease care, diabetes, hypertension, heart disease, cardiovascular risk
Introduction
The quality of outpatient diabetes care has improved remarkably since the Diabetes Control and Complications Trial1 and the United Kingdom Prospective Diabetes Study2,3 were published in the 1990s. Moreover, there is abundant evidence that quality-of-care improvements have accelerated markedly in the last 10 years. In 2002, less than 5% of adults with diabetes were simultaneously at recommended levels of glycated hemoglobin (HbA1c), low-density lipoprotein (LDL) cholesterol, and blood pressure (BP). In 2012, the proportion of patients simultaneously reaching recommended goals is over 50% in many delivery systems, and the proportion reaching A1c <8%, systolic BP <140 mm Hg, and LDL <100 mg/dL or on statin treatment is approaching 80% in many systems, including the Veterans Administration health system.4–6 These gains are reflected in reduced microvascular complications (www.cdc.gov/diabetes). Despite these improvements, the current quality of outpatient diabetes care, whether delivered by subspecialist diabetologists or primary care providers, is far from that recommended in current evidence-based guidelines such as those issued by the American Diabetes Association or the Institute for Clinical Systems Improvement.7,8
Many strategies have been used to improve diabetes care in the last decade, including public reporting of quality measures, paying providers more money for meeting predetermined quality thresholds, expanding the roles of nurses and pharmacists in diabetes care, and working to improve the conceptual model and effectiveness of diabetes patient education. The use of multiple interventions to improve the quality of diabetes care is generally a more effective strategy than the use of single isolated interventions.9 As we look forward to the coming decade, it is likely that an increasingly important component of diabetes quality improvement efforts—especially in outpatient settings—will be innovative applications of sophisticated clinical information systems. This is especially true of electronic medical records (EMR), whose dissemination and use is encouraged and even mandated by federal health agencies such as the Center for Medicaid and Medicare Services (CMS).10–12 In this article, we review what we have learned thus far about outpatient EMR-based diabetes clinical decision support (CDS) and current systems that have been shown to improve important aspects of care. Finally, we speculate about how this rapidly changing field of research and experimentation will evolve in the next 5 to 10 years.
Limitations of Early Diabetes CDS systems
EMR-based CDS is an exciting idea that has been around for a long time. Two Institute of Medicine reports in the early 1990s championed the potential of EMR systems to improve quality of care, and expectations were high.13,14 However, the expense of implementing such systems, the initial lack of availability of reliable commercially available systems, and the cost of training providers to use them slowed dissemination in primary care settings.
First-generation diabetes CDS in outpatient settings focused on prompts and reminders. Some of these CDS tools were applied to identify patients with diabetes or to identify those in need of specific tests (e.g., HbA1c test, microalbuminuria screening test, retinal exam). Other CDS tools identified patients who had elevated BP or HbA1c values at clinic visits. The timing and format of these prompts and reminders was variable. Presenting providers with multiple prompts and reminders was a potential obstacle to their use. Nevertheless, investigators at many centers worked assiduously to refine and improve CDS technologies. At Regenstrief Institute in Indiana, early efforts to provide CDS for chronic conditions such as hypertension, asthma, and congestive heart failure were tested, but the overall results indicated lack of major improvements in care that could be directly attributed to the EMR-based CDS technology.15–17
Early efforts to implement diabetes-specific outpatient CDS included those by Meigs et al18 at Massachusetts General Hospital outpatient clinics and Montori et al19 at Mayo Clinic outpatient clinics. In both these CDS systems, rates of testing for HbA1c and lipids increased, but few significant improvements in control of glucose, BP, or LDL were noted. In effect, the CDS technology sometimes increased the costs of care (and improved what some call the “process” of care) without improving important intermediate outcomes of care that are direct predictors of major microvascular and macrovascular complications.
Why did these early efforts fail to fully achieve the desired results? Careful perusal of the data suggests that one major reason for failure was that the primary care providers did not look at the CDS information in many cases. Reasons for lower than desirable use rates were that care processes were not established to ensure that the CDS was presented at an optimal time during patient encounters (e.g., before the visit agenda, before major decisions had already been made), that the CDS was not considered sophisticated or valuable enough to the provider, or that there was not enough time to use the CDS during a visit.
Qualitative work with primary care providers suggests that EMR systems slow their workflow, and providers are often somewhat resistant to new work processes that require multiple additional “clicks” on the keyboard or mouse during an already complex clinical encounter. In effect, providers are reluctant to open tools that take time to use. Moreover, they intensely resent “forced” CDS20 that interrupts their interaction with the EMR and requires action to clear the screen.
Second-Generation EMR-Based Diabetes CDS Strategies
To be effective in primary care, point-of-care CDS for diabetes must reduce the duration of the encounter, reduce the number of clicks required (relative to a visit without a CDS system), and recognize that competing demands and clinical priorities make it impractical to address diabetes care at all such visits from the point of view of clinic workload and patient flow.21,22
How then can diabetes CDS be designed so that primary care providers are eager to use it? An intriguing study by Koopman et al21 indicated that an EMR system that was programmed to consolidate all the information needed to manage diabetes care in adult patients on one screen at the click of one button saved providers more than 40 clicks and almost 4 minutes per visit—if the purpose of the visit was diabetes care or care related to key components of diabetes care (e.g., BP, lipid management).
In response to these observations and early failures, several teams of investigators have developed second-generation diabetes CDS systems. These systems provide much more detailed CDS than earlier prompts and reminders, and the CDS is much more personalized to an individual patient. Rather than simply presenting a prompt or reminder, second-generation CDS tools typically present a single-screen information display before or early in the visit that captures and presents key data needed to manage multiple aspects of diabetes care (e.g., glucose, BP, lipids, smoking, aspirin use, and obesity). Second-generation CDS uses EMR-embedded clinical algorithms that automatically collect and input patient-specific demographic, pharmacy, laboratory, comorbidity, and allergy data. The clinical algorithms then output personalized suggestions on which treatment moves might improve any clinical domain (e.g., BP, glucose) that is not at the suggested clinical goal.
Next-Generation Diabetes CDS Systems
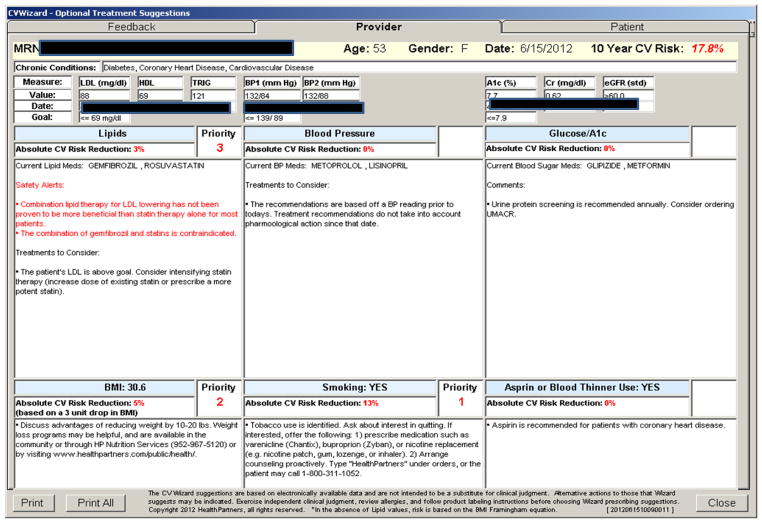
An example of a next-generation diabetes CDS system is shown in Figure 1. This CDS tool, called “CV Wizard” was developed at HealthPartners in Minnesota and is based on prior work that documented the ability of a diabetes-specific version of this CDS system to improve glucose control and some aspects of BP control.23 CV Wizard does the following tasks at the click of one button: (a) gathers clinical information, (b) identifies specific available treatment options based on previous treatment, allergies to medications, distance from goal, comorbidities, and factors (e.g., renal function, heart function) that constrain therapeutic choices, (c) prioritizes a set of clinical domains (e.g., glucose, BP, lipids) according to which domain, if addressed at the current visit, will maximally reduce the patient’s risk of major cardiovascular (CV) complications in the next 10 years, and (d) identifies existing “risky prescribing events” and suggests alternative treatments congruent with the patients previous treatment, distance from goal, allergies, renal function, and cardiac function.
Figure 1.
Screen shot of CDS Interface for Providers. Interface ranks 6 clinical domains based on clinical benefit to the patients, measured by magnitude of cardiovascular risk reduction.
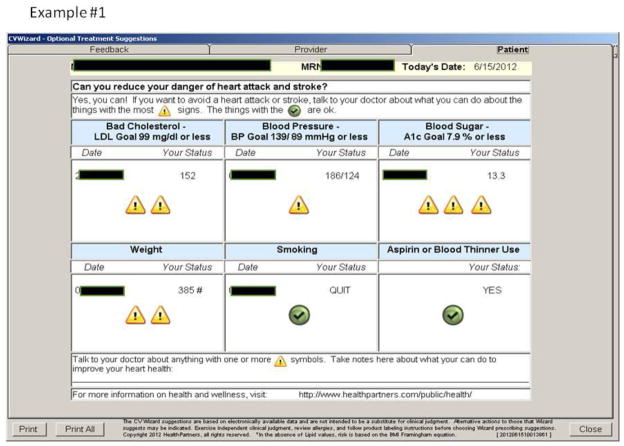
An additional feature of the CV Wizard is that it outputs CDS information both to the primary care provider and to the patient (Figure 2). While the format for providing information to the primary care provider has been in use for more than 4 years and is known to be effective from both results of clinical trials23 and primary care provider feedback, the “patient interface” for CDS information is new and relatively unproven in terms of effectiveness.
Figure 2.
Screen shot of CDS Interface for Patients. Interface ranks 6 clinical domains based on clinical benefit to the patients, measured by magnitude of cardiovascular risk reduction.
So far, most patients and providers like it because the use of symbols rather than numbers makes the main messages about priorities easy to understand. However, some patients may find the presentation of information using symbols rather than numbers too simplistic. There is a clear need to communicate CDS information to patients in a way that is intelligible, actionable, accurate, and unbiased. However much more work is needed to develop optimal communication strategies, and the communication strategies themselves may need to be customized for various types of patients.
Regional and Networked Clinical Decision Support
Another major unresolved challenge and opportunity that is now fully upon us is the need to develop diabetes CDS systems that can be used across multiple care systems. Developing outpatient diabetes clinical care algorithms that are widely used by primary care physicians in multiple care systems (e.g., medical groups, health care organizations) would have many advantages in terms of improved diabetes care, especially the impetus to continuously update the CDS based on new evidence and guidelines. However, many challenges must be surmounted before we can achieve this worthy goal. First, because of disparate EHR systems of different medical groups, there are the technical challenges of communicating data to and from a central service where the treatment and prioritization algorithms reside. This technical challenge may be solved by applying a common digital interface tool (HL7) and related communications strategies that have been mandated by CMS and others for wide use in the next couple of years.10–12
Other challenges to regional, networked CDS include clinical controversy or disagreement about how the results of recent clinical trials such as ACCORD and ADVANCE should be translated into practice and variation in “evidence-based” guideline recommendations emanating from various professional organizations.24,25 The Institute of Medicine recently issued a report titled Clinical Practice Guidelines We Can Trust, which identifies serious potential conflicts of interest when guideline-issuing organizations derive millions of dollars in revenue from drug and device manufacturers each year.26. Such organizations and the potential specialty bias of experts they select to compose clinical guideline groups may favor more aggressive and expensive care strategies that are not necessarily beneficial for many patients and may be harmful for some.27
A great deal of research is currently focused on how to increase the effectiveness of point-of-care outpatient diabetes CDS, and some second-generation CDS systems have recently reported improved glucose and BP control in randomized studies (see reference list).23 However, the observed benefits were relatively modest, and work continues to develop more effective and intuitive CDS systems that save providers time and increase quality of care. A second frontier in diabetes CDS is the development of patient interfaces (via EMR, Web, smart phone, or other communication channels) able to convey accurate information that patients can understand and use to make more informed treatment choices. Balanced presentation of long-term risks and benefits of various pharmatherapeutic or lifestyle treatment choices is an important area of ongoing inquiry.
Development of maximally effective diabetes CDS strategies may be more likely to emerge from front-line providers and patients than from research teams in industry or academia. Providers and patients should identify novel insights that can make care more patient-centered and communicate those insights and ideas to innovators in care systems who can translate such ideas into systems that may improve diabetes care. When we are all active participants in this process, we will begin to move towards a truly “learning” health care system that is increasingly patient-centered.
Future Perspective: Where Will We Be in 10 Years?
Where will diabetes outpatient CDS be 10 years from now? In an ideal world, we will have (a) solved the communications problems across disparate EMR systems, (b) developed increased consensus on at least a minimal standard of care for key clinical goals, (c) found ways to adequately personalize specific care recommendations that include both lifestyle and pharmacologic treatments, (d) developed and validated transparent clinical algorithms and risk equations that operate within CDS systems to prioritize open clinical options based on absolute patient benefit, and (e) developed effective ways to communicate such information to patients in a personalized way so that it can be clearly grasped and lead to clinical actions freely chosen by an informed, proactive patient.
Will such efforts be rewarded with better quality of care, and will patients reap significant benefits in terms of fewer major microvascular and macrovascular complications and longer quality-adjusted life spans? This is the common hope of providers and patients, but we providers often overestimate the benefits of intensive diabetes care. Recent data suggest that the benefits of very good glucose control vary widely depending on the age of the patient at diabetes diagnosis, with the greatest benefit in younger patients, and decreased benefits in patients who develop diabetes after age 65.28,29 Similarly, the benefits of treatment of type 2 diabetes using Roux-en-Y bariatric surgery, vary greatly by the age at surgery (greater benefit at age 40 than age 60 years) as well as by baseline BMI (greater benefit at BMI in the 35–50 range than when BMI > 60).30 As more precise data about benefits and risks of alternative treatment choices become available, the use of prioritized CDS and effective patient-centered communication tools may be an important way to support informed patient decision-making.
In summary, point-of-care clinical decision support has demonstrated potential to improve glucose and BP control in adults with diabetes, but available tools need further development to increase their effectiveness. As more precise data about the long-term benefits and risk of various diabetes treatment strategies becomes available, and as genetic markers for risk of complications and treatment response to specific drugs become more widely available in the next 5 to 10 years, a point-of-care, algorithm-based CDS system will become an indispensible tool for delivering diabetes care that is both patient-centered and maximally effective.
Executive summary.
In the next decade it is likely that an increasingly important component of diabetes quality improvement efforts—especially in outpatient settings—will be innovative applications of sophisticated clinical information systems. This is especially true of EMRs.
First-generation CDS technology (prompts and reminders) sometimes increase the costs of care (and improved what some call the “process” of care) without improving important intermediate outcomes of care that are direct predictors of major microvascular and macrovascular complications.
Second-generation CDS systems provide much more detailed CDS than the earlier prompts and reminders, and the CDS is much more personalized to an individual patient.
Next-generation CDS systems will need to feature effective ways to communicate information about risks and benefits of alternative treatments to patients in a way that is intelligible, actionable, accurate, and balanced.
A major unresolved challenge and opportunity that is now fully upon us is the need to develop diabetes CDS systems that can be used across multiple care systems.
Providers and patients should identify novel insights based on personal experience and communicate those insights and ideas to innovators in care systems who can translate such ideas into patient-centered CDS systems that may improve diabetes care.
Footnotes
Disclosure
Conflicts of interest: P.J. O’Connor: has an NHLBI grant pending; has received honoraria from Peking University, the Montana Diabetes Program, and PCORIJ; has a patent pending on diabetes decision support but no anticipation of money paid;. Desai: none; J. Butler: none; E. Kharbanda: none; J.M. Sperl-Hillen: is a nonpaid Board member of SimCare Health; has received grant support from Merck & Co. and Pfizer; has received honoraria for the BMJ Guideline, and ADA Editor for Diabetes Spectrum; is listed inventor on a patent for simulation-based provider education; has received payment for development of educational presentations including service on speakers’ bureaus for travel expenses to speak at diabetes conference for Medical College of Wisconsin; and travel expenses were covered for speaking engagements and abstract/oral presentations.
References
- 1.DCCT. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993 Sep 30;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 2.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998 Sep 12;352(9131):837–853. [PubMed] [Google Scholar]
- 3.UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998 Sep 12;352(9131):854–865. [PubMed] [Google Scholar]
- 4.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004 Jan 21;291(3):335–342. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 5.Kerr EA, Lucatorto MA, Holleman R, Hogan MM, Klamerus ML, Hofer TP. Monitoring performance for blood pressure management among patients with diabetes mellitus: too much of a good thing? Arch Intern Med. 2012 Jun 25;172(12):938–945. doi: 10.1001/archinternmed.2012.2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MNCM. [Accessed 9/4/2012];Minnesota Community Measurement. 2011 http://www.mncm.org/site/?page=about.
- 7.ADA. Standards of Medical Care in Diabetes. Diabetes Care. 2012;35(S1) [Google Scholar]
- 8.ICSI. Health Care Guideline: Diagnosis and Management of Type 2 Diabetes Mellitus in Adults. Minneapolis, MN: Institute for Clinical Systems Improvement; 2010. [Google Scholar]
- 9.Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001 Oct;24(10):1821–1833. doi: 10.2337/diacare.24.10.1821. [DOI] [PubMed] [Google Scholar]
- 10.Blumenthal D. Launching HITECH. N Engl J Med. 2010 Feb 4;362(5):382–385. doi: 10.1056/NEJMp0912825. [DOI] [PubMed] [Google Scholar]
- 11.CMMS. Centers for Medicare and Medicaid Services. Federal Register. Washington, DC: Department of Health and Human Services; 2010. Medicare and Medicaid Programs; Electronic Health Record Incentive Program; Final Rule; pp. 44314–44588. [Google Scholar]
- 12.HEALTLH I. Transforming Health Care: The Role of Health IT. 2012. Bipartisan Policy Center Task Force on Delivery System Reform and Health IT. [Google Scholar]
- 13.Institute of Medicine. The computer-based patient record. An essential technology for health care. Washington DC: National Academy Press; 1991. [Google Scholar]
- 14.Institute of Medicine. From development to use. Washington DC: National Academy Press; 1992. Guidelines for clinical practice. [Google Scholar]
- 15.Tierney WM, Overhage JM, Murray MD, et al. Effects of computerized guidelines for managing heart disease in primary care. J Gen Intern Med. 2003 Dec;18(12):967–976. doi: 10.1111/j.1525-1497.2003.30635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray MD, Harris LE, Overhage JM, et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial. Pharmacotherapy. 2004 Mar;24(3):324–337. doi: 10.1592/phco.24.4.324.33173. [DOI] [PubMed] [Google Scholar]
- 17.Tierney WM, Overhage JM, Murray MD, et al. Can computer-generated evidence-based care suggestions enhance evidence-based management of asthma and chronic obstructive pulmonary disease? A randomized, controlled trial. Health Serv Res. 2005 Apr;40(2):477–498. doi: 10.1111/j.1475-6773.2005.00368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meigs JB, Cagliero E, Dubey A, et al. A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project. Diabetes Care. 2003 Mar;26(3):750–757. doi: 10.2337/diacare.26.3.750. [DOI] [PubMed] [Google Scholar]
- 19.Montori VM, Dinneen SF, Gorman CA, et al. The impact of planned care and a diabetes electronic management system on community-based diabetes care: the Mayo Health System Diabetes Translation Project. Diabetes Care. 2002 Nov;25(11):1952–1957. doi: 10.2337/diacare.25.11.1952. [DOI] [PubMed] [Google Scholar]
- 20.Bates DW, Kuperman GJ, Wang S, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003 Nov-Dec;10(6):523–530. doi: 10.1197/jamia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koopman RJ, Kochendorfer KM, Moore JL, et al. A diabetes dashboard and physician efficiency and accuracy in accessing data needed for high-quality diabetes care. Ann Fam Med. 2011 Sep-Oct;9(5):398–405. doi: 10.1370/afm.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barnes CS, Ziemer DC, Miller CD, et al. Little time for diabetes management in the primary care setting. Diabetes Educ. 2004 Jan-Feb;30(1):126–135. doi: 10.1177/014572170403000120. [DOI] [PubMed] [Google Scholar]
- 23•.O’Connor PJ, Sperl-Hillen JM, Rush WA, et al. Impact of Electronic Health Record Clinical Decision Support on Diabetes Care: A Randomized Trial. Ann Fam Med. 2011 Jan 1;9(1):12–21. doi: 10.1370/afm.1196. This randomized trial showed that point-of-care diabetes clinical decision support was able to modestly but signficantly improve glucose control and some aspects of BP control in adults with diabetes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2560–2572. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 26.IOM. Institute of Medicine: Guidelines we can Trust. 2012 http://iom.edu/Reports/2011/Clinical-Practice-Guidelines-We-Can-Trust.aspx.
- 27.Kung J, Miller R, Mackowiak P. Failure of Clinical Practice Guidelines to Meet Institute of Medicine Standards: Two More Decades of Little, If Any, Progress. Arch Intern Med. 2012 doi: 10.1001/2013.jamainternmed.56. (published online October 22, 2012) [DOI] [PubMed] [Google Scholar]
- 28.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-Year Follow-up of Intensive Glucose Control in Type 2 Diabetes. N Engl J Med. 2008 Sep 10;359:1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 29.CDC Diabetes Cost-effectiveness Group. Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. The CDC Diabetes Cost-effectiveness Group. JAMA. 2002 May 15;287(19):2542–2551. doi: 10.1001/jama.287.19.2542. [DOI] [PubMed] [Google Scholar]
- 30.O’Connor P, Arterburn DE, Bogart A, et al. Impact of Bariatric Surgery on Long-Term Remission and Relapse of Type 2 Diabetes Mellitus: A Multi-Site Study. Diabetes. 2011;60(Suppl 1):A327. [Google Scholar]