Abstract
Objectives. We tested the hypothesis that neighborhood-level social capital and individual-level neighborhood attachment are positively associated with adult dental care use.
Methods. We analyzed data from the 2000–2001 Los Angeles Family and Neighborhood Survey that were linked to US Census Bureau data from 2000 (n = 1800 adults aged 18–64 years across 65 neighborhoods). We used 2-level hierarchical logistic regression models to estimate the odds of dental use associated with each of 4 forms of social capital and neighborhood attachment.
Results. After adjusting for confounders, the odds of dental use were significantly associated with only 1 form of social capital: social support (adjusted odds ratio [AOR] = 0.85; 95% confidence interval [CI] = 0.72, 0.99). Individual-level neighborhood attachment was positively associated with dental care use (AOR = 1.05; 95% CI = 1.01, 1.10).
Conclusions. Contrary to our hypothesis, adults in neighborhoods with higher levels of social capital, particularly social support, were significantly less likely to use dental care. Future research should identify the oral health–related attitudes, beliefs, norms, and practices in neighborhoods and other behavioral and cultural factors that moderate and mediate the relationship between social capital and dental care use.
Oral health is an indicator of general health and social justice.1,2 Common dental diseases such as tooth decay and gum disease are linked to chronic health conditions, including cardiovascular disease, stroke, diabetes, obesity, and kidney disease.3–7 When left untreated, dental diseases can lead to difficulties chewing food, pain, systemic infections, hospitalization, and, in rare cases, death. Less visible are the social consequences of poor oral health, such as lost work hours,8 functional limitations,9,10 and poor quality of life.11
A comprehensive strategy for optimal oral health involves exposure to topical fluorides (e.g., in optimally fluoridated water, toothpaste), limited fermentable carbohydrate intake, tobacco use prevention, and regular dental visits.12 Professional dental care is particularly important because dentists have opportunities to assess a patient’s risk level for oral health problems, provide diagnostic and preventive care as well as needed restorative care, deliver patient-centered anticipatory guidance, and screen for systemic health conditions.13–16 However, not all individuals in the United States have equal access to dental care.17
Most dental utilization studies focus on children younger than 18 years and seniors aged 65 years and older, even though data from the National Health and Nutrition Examination Survey indicate a decline in dental care use for US adults aged 18 to 64 years.18 Between 1988 and 1994 and 1999 and 2004, there were significant drops in the proportions of adults who had an annual dental visit for those aged 20 to 34 years (from 63.5% to 54.6%) and those aged 35 to 49 years (from 69.0% to 62.5%).18 The factors related to these declines are unknown.
The 2008 World Health Organization report Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health calls for policies and interventions targeting the social determinants of health to reduce and eliminate health disparities.19 Social determinants of health are the structural and environmental conditions that shape human welfare and well-being,20 with health inequalities attributed to unequal distribution of and access to power, money, and resources.21 Although social factors contribute to disparities in dental care use,22 relevant studies focus mostly on individual-level determinants.23–37 There has been less emphasis on the area-level social determinants of adult dental care use.
Social capital is an important health determinant38–41 and is defined as the material, affective, and informational resources inherent in social networks. Most health research has focused on social capital in neighborhoods. Neighborhood-based social capital can be operationalized into 4 forms: (1) social support (provisions that help residents cope with everyday challenges), (2) social leverage (sharing information on health- and non–health-related issues), (3) informal social control (maintenance of safety and norms), and (4) neighborhood organization participation (organized efforts that address community quality of life and personal well-being).42 Social capital has direct and interactive associations with a range of positive and negative health-related outcomes.43,44 In some cases, these resources may not help individuals pursue a desirable health outcome or may inhibit an individual’s efforts through negative influences in the community.45
Although investigators have examined social capital and access to health care services,46 fewer oral health–related studies have focused on social capital. In 2 multilevel studies of elderly persons in Japan, number of teeth was positively associated with higher levels of neighborhood friendship networks47 and a higher prevalence of neighborhood peer group activities.48 Neighborhood social capital also moderated the relationship between income inequality and self-reported oral health but not the number of teeth present among the Japanese elderly.49 A study of Japanese students aged 18 to 19 years found that poor self-reported oral health was associated with lower levels of neighborhood trust and with higher levels of neighborhood informal social control.50 Among Brazilians aged 14 to 15 years, a 5-dimension measure showed that social capital (social trust, social control, empowerment, neighborhood security, and political efficacy) was inversely associated with odds of dental injury.51
Although social capital was not the primary focus, there are 2 relevant US publications. The first reported positive associations between neighborhood social capital and self-reported oral health for children younger than 18 years.52 In the second, neighborhood social capital was identified as a potential source of oral health disparities between Black children and White children aged 3 to 17 years (measured as having a dental problem and poor self-reported oral health) but not for disparities in preventive dental care use.53 Collectively, these studies suggest that neighborhood social capital is an important determinant of oral health.54–56 However, they have 2 main limitations: (1) none of the operationalizations of social capital considered the extent of neighborhood social ties, the resources linked to these ties, or unequal access to resources42; and (2) none focused on dental care use for adults aged 18 to 64 years, a US population subgroup that has exhibited declines in dental care use.18
We addressed previous limitations by adopting a multilevel conceptual model of social capital42,43,45 to examine how neighborhood social capital is associated with dental care use for US adults (Figure 1). We operationalized neighborhood-level social capital as the 4 forms identified earlier (social support, social leverage, informal social control, and neighborhood organization participation). Individual-level neighborhood attachment is the extent to which an individual knows and socializes with neighbors42–44; this moderates the effects of social capital.57 On the basis of this model, we tested 3 hypotheses: (1) higher levels of each form of neighborhood social capital are associated with greater odds of dental use, (2) neighborhood attachment is associated with greater odds of dental care use, and (3) there are interactions between social capital and neighborhood attachment. This study represents an important first step in understanding the social determinants of an important oral health behavior. Our long-term goal is to develop and test neighborhood-based interventions and policies aimed at improving the oral health of individuals at greatest risk for disparities in dental care use.
FIGURE 1—
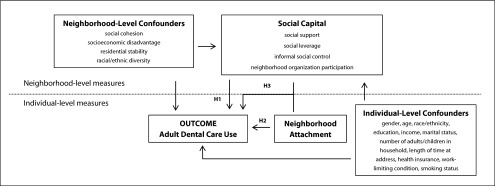
Conceptual model and proposed study hypotheses tested using data from the Los Angeles Family and Neighborhood Survey, 2000–2001.
Note. H1 = hypothesis 1 (there is a direct relationship between the 4 social capital forms and adult dental care use); H2 = hypothesis 2 (there is a direct relationship between neighborhood attachment and adult dental care use); H3 = hypothesis 3 (in modeling adult dental care use, there is an interaction between the four forms of social capital and neighborhood attachment).
METHODS
We analyzed data from wave 1 of the 2000–2001 Los Angeles Family and Neighborhood Survey (L.A.FANS) linked to tract-level data from the 2000 US Census Bureau. L.A.FANS is representative of all neighborhoods and households in Los Angeles County, California, and oversamples low-income neighborhoods and families with children.58 The data set included 2620 individuals in 65 census tracts. We focused our analyses on 1800 adults aged 18 to 64 years who (1) had complete data on the model variables and (2) had lived in their current residence at least 12 months, to ensure adequate exposure to the neighborhood environment.
Variables
Variable selection was guided by a 2-level conceptual model in which we hypothesized neighborhood-level social capital to influence individual-level health behaviors and outcomes.42 We classified model variables as neighborhood- or individual-level variables. We assessed all neighborhood-level variables at the census tract level, which L.A.FANS used for delineating neighborhood boundaries and sampling respondents. Although there are limitations associated with defining census tracts as neighborhoods (e.g., tracts may not represent the units in which neighborhood social capital aggregates),59 census tracts are the closest of any commonly available spatial entity to approximate neighborhoods.60
Main predictor variables.
There were 2 main predictors: neighborhood-level social capital and individual-level neighborhood attachment. There were 4 forms of neighborhood social capital, defined as the resources inherent in neighborhood social networks: social support, social leverage, informal social control, and neighborhood organization participation (Figure 1). We created neighborhood-level social capital scores using empirical Bayes residuals derived from multilevel regression models—a common approach in neighborhood social capital research.43,61,62 This method produces a neighborhood-specific score for each form of social capital that is (1) a deviation from the neighborhood-level grand mean score for that measure and (2) adjusted for sociodemographic and—for informal social control, which we measured with multiple items—item response characteristics of respondents. We z-scored all 4 measures. We measured neighborhood attachment, defined as the degree to which an individual socializes with neighbors and is integrated into neighborhood-based networks, using 4 items and summed it into a single measure (Cronbach α = 0.65; Figure 1).
Outcome variable.
We measured self-reported dental care use, the outcome variable, from a single item asking individuals whether they had visited a dentist for any reason in the past 12 months. Previous studies have demonstrated the validity of this measure.63,64
Neighborhood-level variables.
We modeled 4 variables as neighborhood-level confounders: social cohesion, socioeconomic disadvantage, residential stability, and racial/ethnic diversity. Each is associated with neighborhood social capital43 and dental care use.22,23,35,37 We measured social cohesion, defined as the pattern of interactions between residents and the values linked to these interactions,65 with 4 items using the empirical Bayes residual methods (Figure 1). We used tract-level US census data to generate the remaining neighborhood-level variables.
We measured socioeconomic disadvantage with 5 indicators: income inequality, mean family income, percentage foreign born, percentage female-headed households, and percentage living below the poverty level. We measured income inequality using the Gini coefficient (range = 0–1), with higher values indicating greater degree of income inequality. We created a composite score by z-scoring each item (Cronbach α = 0.89) and computing the mean of the 5 items. We measured residential stability by the percentage of residents who lived in the same tract 5 years earlier. We computed racial/ethnic diversity from the relative proportion of each of 4 racial/ethnic groups (White, Black, Asian/Pacific Islander, and Hispanic) in each census tract, using an entropy score Iceland66 detailed and computed as
where πri refers to the proportion of a particular racial/ethnic group in tract i. We standardized all neighborhood-level variables (mean = 0; SD = 1).
Individual-level variables.
Our models included sociodemographic and health-related variables that we also modeled as confounders (Figure 1). Sociodemographic variables included gender, age, race/ethnicity, education, annual family income, marital status, number of adults and children living in the household, and years at present address. To measure income, we used the L.A.FANS income file, which accounts for incomplete and missing data through multistep imputation procedures.58 There were 3 health status variables: health insurance status, work-limiting health condition, and daily smoking status. Originally, we included employment status in our models, but we found that it did not significantly affect our findings. Because employment is a construct captured by income and education (both of which we included), we excluded it from our final models.
Data Analysis
We generated descriptive statistics, ran bivariate correlations between neighborhood-level variables, and constructed 2-level hierarchical binary logistic regression models (α = 0.05) to estimate adjusted odds ratios (AORs) and corresponding 95% confidence intervals (CIs). These models specified parameters as fixed effects and the intercept to have a between-neighborhood random effect. We analyzed data using Stata version 10.0 (StataCorp LP, College Station, TX).
After running a baseline model that included only the neighborhood- and individual-level confounders, we tested our first and second hypotheses by adding to the baseline model the 4 forms of social capital and neighborhood attachment. We tested our third hypothesis by introducing 4 separate interaction terms—one for each social capital form and neighborhood attachment.
RESULTS
About 53.0% of adults reported using dental care in the previous 12 months (Table 1). The mean age of adults was 37.9 years, and 41.9% were male. More than 55.0% of adults in the study were Hispanic, 26.0% were White, and 9.6% were Black. One in 3 adults did not complete high school. More than 54.0% were married. Nearly one third did not have health insurance, and 11.7% had a work-limiting health condition.
TABLE 1—
Descriptive Statistics: Los Angeles Family and Neighborhood Survey, 2000–2001
| Variable | % or Mean (SD) | Range |
| Self-reported dental care use in past 12 moa | 52.5 | … |
| Male gender | 41.9 | … |
| Age, y | 37.9 (10.9) | 18–64 |
| Race/ethnicity | ||
| White | 26.0 | … |
| Black | 9.6 | … |
| Hispanic | 55.3 | … |
| Other | 9.1 | … |
| Education | ||
| < high school | 32.9 | … |
| Completed high school or GED | 20.7 | … |
| Vocational training | 3.8 | … |
| Some college | 22.2 | … |
| Bachelor’s degree | 11.8 | … |
| Graduate school | 8.6 | … |
| Annual family income (quartiles), $ | ||
| Q1: 0–15 724 | 25.0 | … |
| Q2: 15 725–30 801 | 25.0 | … |
| Q3: 30 802–60 900 | 25.0 | … |
| Q4: 60 901–1 303 000 | 25.0 | … |
| Currently married | 54.3 | … |
| No. adults in household | 2.4 (1.2) | 1–11 |
| No. children in household | 1.8 (1.4) | 0–10 |
| Length of time at present address, y | 7.3 (7.1) | 1.0–51.1 |
| Health status | ||
| Currently does not have health insurance | 30.2 | … |
| Has a work-limiting health condition | 11.7 | … |
| Smokes daily | 14.5 | … |
Note. GED = general equivalency diploma. The sample size was n = 1800.
Outcome variable.
Bivariate Correlations
Three forms of social capital (social support, social leverage, and informal social control) were positively and significantly correlated with one another (0.28–0.58) but not with the fourth form of social capital (neighborhood organization participation; Table 2). The largest correlation was between social cohesion and informal social control (0.88). Sensitivity and diagnostic analyses indicated that these correlations were not problematic in terms of multicollinearity.
TABLE 2—
Bivariate Correlations for Neighborhood-Level Variables: Los Angeles Family and Neighborhood Survey, 2000–2001
| Correlations |
||||||||
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| 1. Social support | 1.00 | |||||||
| 2. Social leverage | 0.45** | 1.00 | ||||||
| 3. Informal social control | 0.58** | 0.28* | 1.00 | |||||
| 4. Neighborhood organization participation | 0.23 | 0.02 | 0.24 | 1.00* | ||||
| 5. Social cohesion | 0.48** | 0.19 | 0.88** | 0.19* | 1.00** | |||
| 6. Socioeconomic disadvantage | −0.31* | −0.04 | −0.76** | −0.17 | −0.75** | 1.00 | ||
| 7. Residential stability | 0.37** | 0.03 | 0.36** | −0.01* | 0.35** | −0.45** | 1.00 | |
| 8. Racial/ethnic diversity | 0.15 | −0.08 | 0.34** | 0.02 | 0.26* | −0.26* | −0.17 | 1.00 |
Note. The study included 65 neighborhoods.
*P ≤ .05; **P ≤ .01.
Regression Models
Social support was the only form of social capital significantly associated with dental use (Table 3). For each SD increase in neighborhood social support, the odds of dental use decreased by 15% (AOR = 0.85; 95% CI = 0.72, 0.99). Individual-level neighborhood attachment was positively associated with greater odds of dental use (AOR = 1.05). None of the 4 social capital and neighborhood attachment interaction terms was statistically significant (data not shown).
TABLE 3—
Adjusted Odds Ratios for Self-Reported Dental Care Use in the Past 12 Months: Los Angeles Family and Neighborhood Survey, 2000–2001
| Variable | AOR (95% CI) |
| Main neighborhood-level predictor: social capital | |
| Social support | 0.85* (0.72, 0.99) |
| Social leverage | 1.08 (0.94, 1.23) |
| Informal social control | 0.93 (0.69, 1.24) |
| Neighborhood organization participation | 0.98 (0.87, 1.10) |
| Main individual-level predictor: neighborhood attachment | 1.05* (1.01, 1.10) |
DISCUSSION
We adopted a previously developed model of neighborhood social capital and health to test the hypotheses that adult dental care use is positively associated with (1) neighborhood-level social capital and (2) individual-level neighborhood attachment and that there would be interactions between (1) and (2). On the basis of L.A.FANS and the US Census Bureau data, we found that only 1 form of neighborhood social capital (i.e., social support) was significantly associated with adult dental care use but not in the hypothesized direction. Conversely, higher levels of social capital were associated with significantly lower odds of self-reported dental care. In addition, higher levels of neighborhood attachment were associated with greater odds of dental use. We found no evidence of interactions between social capital and neighborhood attachment. Collectively, these findings indicate that neighborhood social capital (particularly social support) is an important factor associated with adult dental utilization but that higher levels of social support are associated with decreased odds of dental care use.
Direct comparisons with other studies are limited because of heterogeneity in study populations and social capital operationalizations. A previous publication reported a negative relationship between neighborhood social capital and self-reported oral health among students in Japan,50 which is consistent with our main finding that neighborhood social support was associated with lower odds of dental use and other studies linking social capital with negative health outcomes.67 Two additional studies—both using L.A.FANS data—reported associations between higher neighborhood social support and several outcomes: lower odds of having a regular source of primary care and receipt of a medical check-up68 and higher odds of smoking and binge drinking.62
A possible explanation for our finding is that neighborhood-level behavioral factors relevant in oral health such as shared attitudes and norms may be moderators of dental care use. Previous work suggests that behavioral and cultural factors such as attitudes, knowledge, norms, and perceived control are related to health care use.69 Residents with similar norms may help create a supportive environment with high levels of neighborhood-level social support, but these individuals may share low self-efficacy regarding their ability to find a dentist or may undervalue professional dental care because of low health literacy. Thus, improving neighborhood-level social support without addressing relevant oral health–related attitudes, knowledge, and norms could lead to the unintended consequences. Individual-level behavioral and cultural factors could also mediate the relationship between neighborhood-level social capital and individual-level oral health, as has been demonstrated with self-reported health status.70 Future work should identify the individual-level oral health–specific behavioral and cultural factors that may be as important as neighborhood-level social factors in moderating or mediating desired oral health behaviors.
The other 3 forms of social capital in our model (informal social control, neighborhood organization participation, and social leverage) failed to reach statistical significance. There are 2 potential explanations. The first is that the social capital measures were not specific to dental care. For instance, our measure of social leverage did not indicate whether employment-related advice from neighbors leads to job opportunities that provide dental insurance. Future work should include oral health–specific measures of each form of social capital. The second is the ethnic composition of our study population, which was 55% Hispanic. A recent publication reported that individual-level social capital (measured as trust and volunteerism) was not associated with perceived access to health care services for Mexican American women,71 whereas another household study with an ethnically diverse population found a positive relationship between social capital and access to health care services.72 Studies should investigate how neighborhood-level social capital may lead to differential health behaviors and outcomes for ethnic/racial minorities, which has implications for developing targeted interventions on the basis of the composition of the target communities.
Neighborhood attachment, an individual-level measure of the extent to which residents have access to neighborhood-based resources,42 was associated with greater odds of dental use, which is consistent with findings from non–oral health studies.73,74 Although we did not evaluate mechanisms, 1 possibility is increased familiarity with the environment,75 which could lead to improved knowledge about the location and availability of community dentists and dental care facilities. Another possible mechanism is that having friends in the neighborhood gives individuals access to transportation as well as personal referrals to dentists. In the context of our finding that the 4 forms of neighborhood social capital were negatively associated or not associated with dental care use, our finding on neighborhood attachment highlights the difference between of personal ties located in neighborhoods that benefit specific individuals and broader neighborhood-based ties that potentially benefit everyone in the community. These seemingly contradictory findings are consistent with previous work that distinguishes benefits arising from personal versus communal ties in neighborhoods.76 Future studies should examine the particular mechanisms underlying neighborhood attachment that lead to increased odds of dental care use.
The interaction between the 4 social capital forms and neighborhood attachment failed to reach statistical significance in our models. In other words, the association between social capital (social support) and dental use is observed across all adult residents who live in a particular neighborhood regardless of one’s degree of neighborhood attachment. Previous studies have found significant cross-level interactions between these 2 factors on health outcomes such as self-rated health and smoking.43,62 One explanation for our findings is that other social and behavioral characteristics of the neighborhood relevant to oral health may be more important correlates of dental use than is attachment. Another explanation is that greater attachment to neighbors may not link an individual to the neighborhood social capital forms as measured in this study. Rather, social capital may be shared only among certain neighbors (e.g., only among neighbors who are close friends). Future research should include a wider range of measures of neighborhood and non–neighbor-based social ties and social capital.
Broadly, our work has implications for future research as well as the development of oral health interventions and policies. In terms of research, our findings indicate the need to account for upstream area-based resources (e.g., neighborhood social capital) as well as access to these resources (e.g., neighborhood attachment) to fully understand how social factors influence dental care use.77 There is also a need to develop and test oral health behavior– and dental disease–relevant measures of social capital that can be used to generate the knowledge needed to develop neighborhood-level oral health interventions. For instance, 1 aspect of social support relevant to oral health is food choice and eating patterns, which are thought to be transmitted across social networks.78 Furthermore, oral health interventions and policies may need to be tailored to communities on the basis of the availability of social resources and conditions, which is supported by previous research external to dentistry.45,79 Our findings challenge the traditional approach that targets health interventions at resource-poor environments without considering social context.
Limitations
L.A.FANS is one of the best US data sets for studying issues related to neighborhood social capital. However, there are 6 main study limitations. First, we analyzed cross-sectional data, which limits our ability to make causal inferences. Second, there is the potential for neighborhood selection bias (i.e., people chose where to live on the basis of neighborhood attributes). Third, there are limitations with our social capital and neighborhood attachment measures. We operationalized the 3 forms of social capital—social support, social leverage, and neighborhood organization participation—with only 1 item each, and our attachment measure was unable to capture potential resources in networks outside the neighborhood.
Fourth, our analysis is derived from data from an urban county in California. Although census tracts enclose small geographic areas that are likely to be representative of actual urban neighborhoods, it is unclear whether our findings are generalizable to rural communities. Fifth, it was unknown if the type of dental care utilized represented primary, secondary, or tertiary preventive care. In the future, dental utilization measures should be more specific. Sixth, the study was limited to evaluating the role of neighborhood-based resources. However, resources beyond the neighborhood setting (e.g., dental office location, transportation, flexible work schedules) that were not included in our study may also influence dental care use. Despite these limitations, this is the first study to our knowledge from the United States to test a series of theory-driven hypotheses related to neighborhood social capital and adults’ dental care use.
Conclusions
Oral health is inextricably linked to systemic health outcomes and quality of life, but large proportions of US adults do not utilize dental care. This has motivated efforts to identify the upstream social determinants of dental care use. We found that 1 form of neighborhood social capital—social support—was associated with decreased odds of dental care use among adults aged 18 to 64 years, but the mechanisms underlying this relationship are unknown. Furthermore, increased levels of neighborhood attachment were associated with increased odds of dental care use.
Dental visits alone are not likely to solve oral health disparities, but they do play an important role in helping patients maintain good oral health. Nearly 50% of adults in our study did not utilize dental care, which calls for additional research to understand the behavioral and cultural mechanisms by which neighborhood social capital and other social factors are related to dental care use. Once the neighborhood-based determinants and mechanisms associated with dental care use are identified, multilevel place-based clinical interventions and policies can be generated that seek to reduce disparities in dental care use among vulnerable adults.
Acknowledgments
This study was funded by the National Institute of Dental and Craniofacial Research and the National Institutes of Health Career Development (award K08DE020856 to D. L. C.) and the Michael Smith Foundation for Health Research and Canadian Institutes of Health Research (to R. M. C.). The Los Angeles Family and Neighborhood Survey is funded by the US National Institute of Child Health and Human Development to RAND in Santa Monica, CA (grant R01HD35944).
Portions of this study were presented at the Academy Health Annual Research Meeting in Seattle, WA, June 2011.
Human Participant Protection
The University of British Columbia’s behavioral research ethics board approved the study.
References
- 1.US Department of Health and Human Services Oral Health in America: A Report of the Surgeon General. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000 [Google Scholar]
- 2.Treadwell HM, Northridge ME. Oral health is the measure of a just society. J Health Care Poor Underserved. 2007;18(1):12–20 [DOI] [PubMed] [Google Scholar]
- 3.Ylöstalo PV, Järvelin MR, Laitinen Jet al. Gingivitis, dental caries and tooth loss: risk factors for cardiovascular diseases or indicators of elevated health risks. J Clin Periodontol. 2006;33(2):92–101 [DOI] [PubMed] [Google Scholar]
- 4.Fisher MA, Taylor GW. A prediction model for chronic kidney disease includes periodontal disease. J Periodontol. 2009;80(1):16–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griffin SO, Barker LK, Griffin PMet al. Oral health needs among adults in the United States with chronic diseases. J Am Dent Assoc. 2009;140(10):1266–1274 [DOI] [PubMed] [Google Scholar]
- 6.Desvarieux M, Demmer RT, Jacobs DR, Jret al. Periodontal bacteria and hypertension: the oral infections and vascular disease epidemiology study (INVEST). J Hypertens. 2010;28(7):1413–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ioannidou E, Hall Y, Swede Het al. Periodontitis associated with chronic kidney disease among Mexican Americans. J Public Health Dent. July 6, 2012; Epub ahead of print [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. Am J Public Health. 1992;82(12):1663–1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Locker D, Quiñonez C. Functional and psychosocial impacts of oral disorders in Canadian adults: a national population survey. J Can Dent Assoc. 2009;75(7):521. [PubMed] [Google Scholar]
- 10.Sanders AE, Slade GD, Lim Set al. Impact of oral disease on quality of life in the US and Australian populations. Community Dent Oral Epidemiol. 2009;37(2):171–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hollister MC, Weintraub JA. The association of oral status with systemic health, quality of life, and economic productivity. J Dent Educ. 1993;57(12):901–912 [PubMed] [Google Scholar]
- 12.Gooch BF, Malvitz DM, Griffin SOet al. Promoting the oral health of older adults through the chronic disease model: CDC’s perspective on what we still need to know. J Dent Educ. 2005;69(9):1058–1063 [PubMed] [Google Scholar]
- 13.Crall JJ. Rethinking prevention. Pediatr Dent. 2006;28(2):96–101 [PubMed] [Google Scholar]
- 14.Watson JM, Logan HL, Tomar SLet al. Factors associated with early-stage diagnosis of oral and pharyngeal cancer. Community Dent Oral Epidemiol. 2009;37(4):333–341 [DOI] [PubMed] [Google Scholar]
- 15.Strauss SM, Russell S, Wheeler Aet al. The dental office visit as a potential opportunity for diabetes screening: an analysis using NHANES 2003–2004 data. J Public Health Dent. 2010;70(2):156–162 [DOI] [PubMed] [Google Scholar]
- 16.Viswanathan K, Muzzin K, Pickett FAet al. Monitoring pediatric blood pressure at dental appointments. J Dent Child (Chic). 2010;77(3):140–145 [PubMed] [Google Scholar]
- 17.Institute of Medicine; National Research Council Improving Access to Oral Health Care for Vulnerable and Underserved Populations. Washington, DC: National Academies Press; 2011 [Google Scholar]
- 18.Dye BA, Tan S, Smith Vet al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat 11. 2007;248:1–92 [PubMed] [Google Scholar]
- 19.Commission on Social Determinants of Health Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. Geneva: World Health Organization; 2008 [Google Scholar]
- 20.Marmot M, Wilkinson R, eds. Social Determinants of Health. 2nd ed. Oxford: Oxford University Press; 2006 [Google Scholar]
- 21.Friel S, Marmot MG. Action on the social determinants of health and health inequities goes global. Annu Rev Public Health. 2011;32:225–236 [DOI] [PubMed] [Google Scholar]
- 22.Patrick DL, Lee RS, Nucci Met al. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6(suppl 1):S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doty HE, Weech-Maldonado R. Racial/ethnic disparities in adult preventive dental care use. J Health Care Poor Underserved. 2003;14(4):516–534 [DOI] [PubMed] [Google Scholar]
- 24.Okunseri C, Bajorunaite R, Matthew Ret al. Racial and ethnic variation in the provision of dental procedures. J Public Health Dent. 2007;67(1):20–27 [DOI] [PubMed] [Google Scholar]
- 25.Dismuke CE, Egede LE. Association of serious psychological distress with health services expenditures and utilization in a national sample of US adults. Gen Hosp Psychiatry. 2011;33(4):311–317 [DOI] [PubMed] [Google Scholar]
- 26.Milgrom P, Weinstein P. Dental fears in general practice: new guidelines for assessment and treatment. Int Dent J. 1993;43(3 suppl 1):288–293 [PubMed] [Google Scholar]
- 27.Riley JL, 3rd, Gilbert GH, Heft MW. Dental attitudes: proximal basis for oral health disparities in adults. Community Dent Oral Epidemiol. 2006;34(4):289–298 [DOI] [PubMed] [Google Scholar]
- 28.Drilea SK, Reid BC, Li CHet al. Dental visits among smoking and nonsmoking US adults in 2000. Am J Health Behav. 2005;29(5):462–471 [DOI] [PubMed] [Google Scholar]
- 29.Vargas CM, Manski RJ. Dental expenditures and source of payment by race/ethnicity and other sociodemographic characteristics. J Public Health Dent. 1999;59(1):33–38 [DOI] [PubMed] [Google Scholar]
- 30.Green BL, Person S, Crowther Met al. Demographic and geographic variations of oral health among African Americans based on NHANES III. Community Dent Health. 2003;20(2):117–122 [PubMed] [Google Scholar]
- 31.Patel N, Bae S, Singh KP. Association between utilization of preventive services and health insurance status: findings from the 2008 Behavioral Risk Factor Surveillance System. Ethn Dis. 2010;20(2):142–147 [PubMed] [Google Scholar]
- 32.Vargas CM, Dye BA, Hayes KL. Oral health status of rural adults in the United States. J Am Dent Assoc. 2002;133(12):1672–1681 [DOI] [PubMed] [Google Scholar]
- 33.Mullins CD, Cohen LA, Magder LSet al. Medicaid coverage and utilization of adult dental services. J Health Care Poor Underserved. 2004;15(4):672–687 [DOI] [PubMed] [Google Scholar]
- 34.Schrimshaw EW, Siegel K, Wolfson NHet al. Insurance-related barriers to accessing dental care among African American adults with oral health symptoms in Harlem, New York City. Am J Public Health. 2011;101(8):1420–1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hjern A, Grindefjord M, Sundberg Het al. Social inequality in oral health and use of dental care in Sweden. Community Dent Oral Epidemiol. 2001;29(3):167–174 [DOI] [PubMed] [Google Scholar]
- 36.Gomes A, Lunet N, Santos ACet al. Social, demographic, clinical and lifestyle determinants of dental care visits in an urban sample of Portuguese adults. Oral Health Prev Dent. 2008;6(1):3–11 [PubMed] [Google Scholar]
- 37.Pavi E, Karampli E, Zavras Det al. Social determinants of dental health services utilisation of Greek adults. Community Dent Health. 2010;27(3):145–150 [PubMed] [Google Scholar]
- 38.Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: a contextual analysis. Am J Public Health. 1999;89(8):1187–1193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kawachi I, Subramanian SV, Kim D, eds. Social Capital and Health. New York: Springer; 2008 [Google Scholar]
- 40.Schultz J, O’Brien AM, Tadesse B. Social capital and self-rated health: results from the US 2006 social capital survey of one community. Soc Sci Med. 2008;67(4):606–617 [DOI] [PubMed] [Google Scholar]
- 41.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398 [DOI] [PubMed] [Google Scholar]
- 42.Carpiano RM. Toward a neighborhood resource-based theory of social capital for health: can Bourdieu and sociology help? Soc Sci Med. 2006;62(1):165–175 [DOI] [PubMed] [Google Scholar]
- 43.Carpiano RM. Actual or potential neighborhood resources and access to them: testing hypotheses of social capital for the health of female caregivers. Soc Sci Med. 2008;67(4):568–582 [DOI] [PubMed] [Google Scholar]
- 44.Carpiano RM, Kimbro RT. Neighborhood social capital, parenting strain, and personal mastery among female primary caregivers of children. J Health Soc Behav. 2012;53(2):232–247 [DOI] [PubMed] [Google Scholar]
- 45.Cené CW, Akers AY, Lloyd SWet al. Understanding social capital and HIV risk in rural African American communities. J Gen Intern Med. 2011;26(7):737–744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Derose KP, Varda DM. Social capital and health care access: a systematic review. Med Care Res Rev. 2009;66(3):272–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Aida J, Kuriyama S, Ohmori-Matsuda Ket al. The association between neighborhood social capital and self-reported dentate status in elderly Japanese—the Ohsaki Cohort 2006 Study. Community Dent Oral Epidemiol. 2011;39(3):239–249 [DOI] [PubMed] [Google Scholar]
- 48.Aida J, Hanibuchi T, Nakade Met al. The different effects of vertical social capital and horizontal social capital on dental status: a multilevel analysis. Soc Sci Med. 2009;69(4):512–518 [DOI] [PubMed] [Google Scholar]
- 49.Aida J, Kondo K, Kondo Net al. Income inequality, social capital and self-rated health and dental status in older Japanese. Soc Sci Med. 2011;73(10):1561–1568 [DOI] [PubMed] [Google Scholar]
- 50.Furuta M, Ekuni D, Takao Set al. Social capital and self-rated oral health among young people. Community Dent Oral Epidemiol. 2012;40(2):97–104 [DOI] [PubMed] [Google Scholar]
- 51.Pattussi MP, Hardy R, Sheiham A. Neighborhood social capital and dental injuries in Brazilian adolescents. Am J Public Health. 2006;96(8):1462–1468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bramlett MD, Soobader MJ, Fisher-Owens SAet al. Assessing a multilevel model of young children’s oral health with national survey data. Community Dent Oral Epidemiol. 2010;38(4):287–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guarnizo-Herreño CC, Wehby GL. Explaining racial/ethnic disparities in children’s dental health: a decomposition analysis. Am J Public Health. 2012;102(5):859–866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Watt RG. Emerging theories into the social determinants of health: implications for oral health promotion. Community Dent Oral Epidemiol. 2002;30(4):241–247 [DOI] [PubMed] [Google Scholar]
- 55.Newton JT, Bower EJ. The social determinants of oral health: new approaches to conceptualizing and researching complex causal networks. Community Dent Oral Epidemiol. 2005;33(1):25–34 [DOI] [PubMed] [Google Scholar]
- 56.Marmot M, Bell R. Social determinants and dental health. Adv Dent Res. 2011;23(2):201–206 [DOI] [PubMed] [Google Scholar]
- 57.Bourdieu P. The forms of capital. In: Richardson JG, ed. Handbook of Theory and Research for the Sociology of Education. New York: Greenwood; 1986 [Google Scholar]
- 58. RAND. The Los Angeles Families and Neighborhoods Study. Available at: http://www.lasurvey.rand.org. Accessed August 8, 2012.
- 59.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jargowsky PA. Poverty and Place: Ghettos, Barrios, and the American City. New York: Russell Sage Foundation; 1997 [Google Scholar]
- 61.Browning CR, Cagney KA. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. J Health Soc Behav. 2002;43(4):383–399 [PubMed] [Google Scholar]
- 62.Carpiano RM. Neighborhood social capital and adult health: an empirical test of a Bourdieu-based model. Health Place. 2007;13(3):639–655 [DOI] [PubMed] [Google Scholar]
- 63.Gilbert GH, Rose JS, Shelton BJ. A prospective study of the validity of data on self-reported dental visits. Community Dent Oral Epidemiol. 2002;30(5):352–362 [DOI] [PubMed] [Google Scholar]
- 64.Bhandari A, Wagner T. Self-reported utilization of health care services: improving measurement and accuracy. Med Care Res Rev. 2006;63(2):217–235 [DOI] [PubMed] [Google Scholar]
- 65.Putnam RD. The prosperous community: social capital and public life. Am Prospect. 1993;13:35–42 [Google Scholar]
- 66.Iceland J. The Multigroup Entropy Index. Available at: http://www.census.gov/hhes/www/housing/resseg/multigroup_entropy.pdf. Accessed May 10, 2012.
- 67.Moore S, Daniel M, Gauvin Let al. Not all social capital is good capital. Health Place. 2009;15(4):1071–1077 [DOI] [PubMed] [Google Scholar]
- 68.Prentice JC. Neighborhood effects on primary care access in Los Angeles. Soc Sci Med. 2006;62(5):1291–1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bradley EH, McGraw SA, Curry Let al. Expanding the Andersen model: the role of psychosocial factors in long-term care use. Health Serv Res. 2002;37(5):1221–1242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mohnen SM, Völker B, Flap Het al. Health-related behavior as a mechanism behind the relationship between neighborhood social capital and individual health—a multilevel analysis. BMC Public Health. 2012;12:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Valencia-Garcia D, Simoni JM, Alegría Met al. Social capital, acculturation, mental health, and perceived access to services among Mexican American women. J Consult Clin Psychol. 2012;80(2):177–185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hendryx MS, Ahern MM, Lovrich NPet al. Access to health care and community social capital. Health Serv Res. 2002;37(1):87–103 [PubMed] [Google Scholar]
- 73.Barrow S, Harrison RA. Unsung heroes who put their lives at risk? Informal caring, health and neighbourhood attachment. J Public Health (Oxf). 2005;27(3):292–297 [DOI] [PubMed] [Google Scholar]
- 74.Lenzi M, Vieno A, Perkins DDet al. Perceived neighborhood social resources as determinants of prosocial behavior in early adolescence. Am J Community Psychol. 2012;50(1–2):37–49 [DOI] [PubMed] [Google Scholar]
- 75.Bolan M. The mobility experience and neighborhood attachment. Demography. 1997;34(2):225–237 [PubMed] [Google Scholar]
- 76.Dominguez S, Watkins C. Creating networks for survival and mobility: examining social capital amongst low-income African-American and Latin-American mothers. Soc Probl. 2003;50(1):111–135 [Google Scholar]
- 77.Watt RG. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol. 2007;35(1):1–11 [DOI] [PubMed] [Google Scholar]
- 78.Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101(11):2170–2177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Blickem C, Bower P, Protheroe Jet al. The role of information in supporting self-care in vascular conditions: a conceptual and empirical review. Health Soc Care Community. 2011;19(5):449–459 [DOI] [PubMed] [Google Scholar]


