Case Presentation
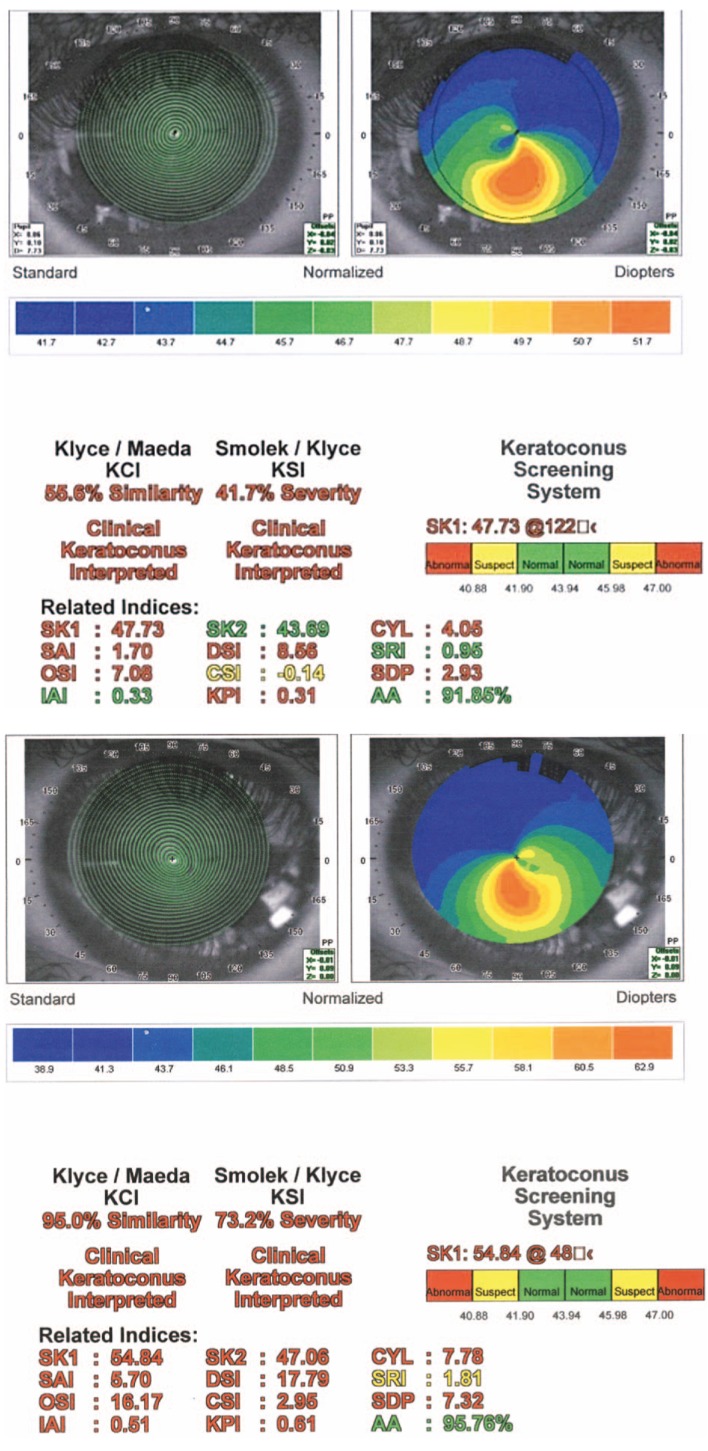
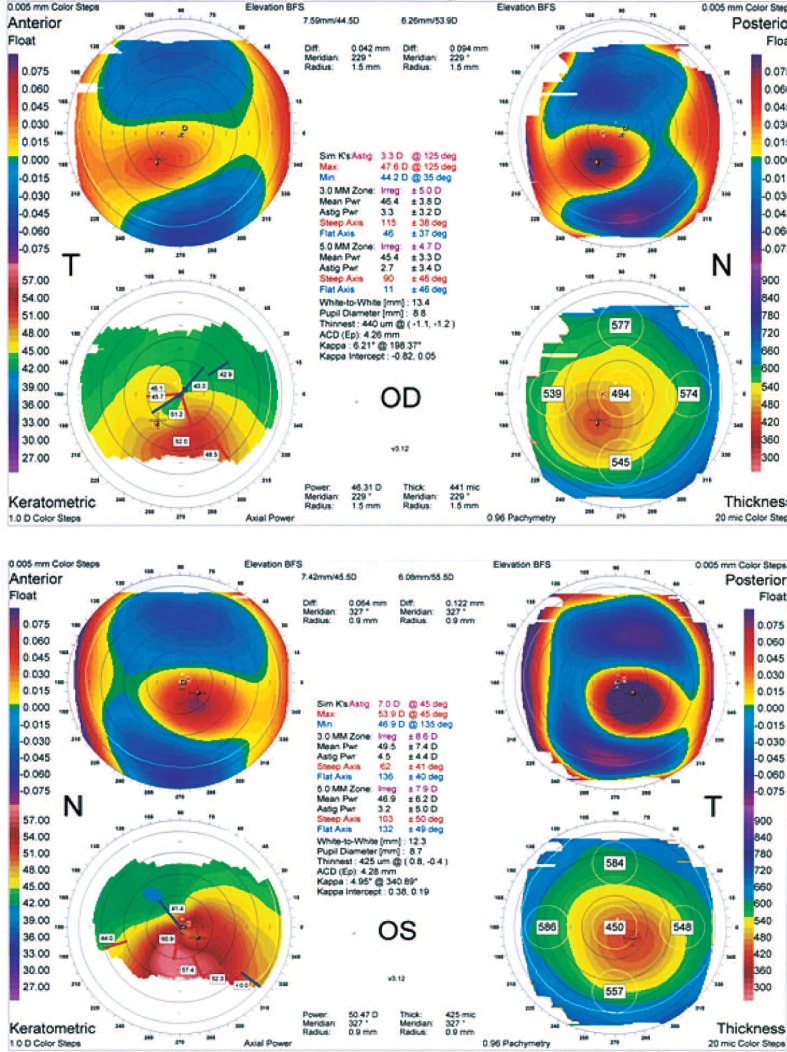
A 23-year-old lady was referred to the cornea clinic complaining of progressive visual loss from 8 years ago. Uncorrected visual acuity (UCVA) was 20/100 in her right eye and 20/600 in the left one. She was using rigid gas-permeable (RGP) contact lenses for 4 years and complained of contact lens intolerance especially in her left eye. On slit lamp examination, both corneas were clear but Vogts' striae and Fleischer rings were present in both eyes. Manifest refraction was -3.00-6.00×30 and -7.00-8.00×140 in the right and left eyes respectively with best spectacle corrected visual acuity (BSCVA) of 20/60 and 20/200; visual acuity with best-fitted contact lenses were 20/30 and 20/70 in the same order. Corneal topography and Orbscan maps are shown in Figures 1 and 2.
Herein we present the opinions of three corneal specialists in the management of keratoconus (KCN) in general, and this case in particular. The following matters will be specifically addressed:
What are the important points in the clinical history and diagnostic evaluation of patients with KCN?
What is the importance of subjective and manifest refraction, and uncorrected and corrected visual acuity?
Is the topographic pattern of the cornea important and does it affect your treatment plan, for example the type of intracorneal ring?
Is the topographic pattern of the cone and its location important?
What is your preferred plan for each eye?
What is your opinion about collagen cross linking (CCL) in this case; at which stage would you perform the procedure?
Do you recommend intracorneal ring segments (ICRS) for this patient? Which type of ring would you choose?
If you decide to implant ICRSs, which sites do you prefer for incision and implantation?
Do you consider corneal transplantation a viable option for this patient?
Kazem Amanzadeh, MD
Much like all eye diseases, when we deal with patients suspected of keratoconus, history is of particular importance; it helps both in the diagnosis and differential diagnosis. The age of onset of decreased visual acuity and wearing glasses are very important in this patient. If the patient had decreased visual acuity in childhood and had to use glasses, but was negligent or had a history of amblyopia therapy or strabismus surgery, one should consider other causes of decreased visual acuity such as amblyopia.
It is mandatory to perform the 8-part comprehensive eye examination and pay particular attention to the condition of the retina, optic nerve head and lens because this can help diagnose other causes of decreased vision.
Enquiries about eye problems which may accompany keratoconus such as allergic disorders, Leber’s congenital amaurosis or several corneal dystrophies and also long term history of RGP lens wear can also be helpful for diagnosis.
Questions about systemic problems, especially diseases that disrupt collagen metabolism such as Ehlers-Danlos and Marfan syndromes, and also mitral valve prolapse can be helpful.
Diagnosis is based on slit lamp examination and corneal topography (curvature and elevation based). Analysis by the ocular response analyzer (ORA), wavefront aberrometry, and Artemis images are also helpful in this regard.
Several factors should be considered in selection of an appropriate treatment plan, these include:
Age
Occupation
UCVA
BSCVA
BCVA with RGP lenses
Tolerance or intolerance to RGP (more or less than 8 hours of use per day)
-
Corneal topography
Kmax (less or more than 58 diopters)
Kmean (less or more than 55 diopters)
The location of the cone and its distance to the apex, and thinnest point from the center
Shape of the cone (symmetrical or asymmetrical with or without SRAX, pellucid like keratoconus)
Central corneal thickness (below or above 400 microns) and also corneal thickness in zones 5, 6, 7 mm
Patient’s desire to have better UCVA, and better BCVA with glasses and RGP lenses
Has the patient previously undergone surgery for keratoconus or not? If so, compare the results before and after surgery
Availability for regular follow-up, social and economic status of the patient, the extent of attention to the disease and its consequences
Regarding CCL, I perform the procedure for all patients under 25 years of age who have good vision with glasses (over 20/30) without proof of progression. But patients older than 25 years (up to 35) with similar conditions (vision over 20/30 with glasses) are monitored for 6 months and if any of the following items are observed, I perform CCL:
Increase in Kmax more than one diopter per year.
Corneal thinning (at the thinnest point) exceeding 30 microns per year
Increase in topographic astigmatism more than one diopter per year
Reduction in UCVA and BSCVA more than one line per year
In the following cases, CCL is not recommended for the patient:
Lack of adequate vision with glasses (less than 20/30)
Patient is a candidate for ICRS (CCL is done after the ring, as the effect of the corneal ring is decreased because of corneal stiffness after CCL)
Corneal thickness less than 400 micron (at the thinnest part)
Patient expectations for improvement after surgery
Kmax over 58 diopters
History of herpetic keratitis
Pregnancy
Active rheumatoid diseases (risk of melting) and also disorders affecting corneal epithelial healing
Candidates for ICRS implantation should have the following characteristics:
Vision with RGP more than 20/40 (functional visual acuity)
BSCVA better than 20/60
Kmean less than 55 diopters
Kmax below 60 diopters
Central corneal thickness of at least 400 microns
Transparent corneal center (4 mm over the pupil)
Inability to tolerate RGP lenses (less than 8-hour use per day) or tolerance to RGP but desire to achieve better spectacle corrected vision when not using lenses.
In subjects less than 20 years of age who are a future transplant candidate for advanced KCN and have severe decrease in visual acuity, ICRS may be combined with CCL implantation and surgery is postponed until the patient is older.
In this particular patient, her left eye has vision less than 20/40 with glasses and RGP lenses (functional VA), which means that corneal higher order aberrations (HOA) are significant and ICRS implantation will not be effective. Thus this eye is a candidate for corneal transplantation, preferably deep anterior lamellar keratoplasty (DALK) using the Big Bubble technique. If for any reason the patient does not wish to have corneal transplantation, other options such as CCL combined with ICRS may be offered, so that the patient can enjoy a more stable cornea until she is ready for transplantation.
In the right eye considering vision over 20/40 with RGP, the patient is a candidate for ICRS surgery. After surgery, the patient should be monitored for 6 months and if symptoms of progression are observed, she can undergo CCL. Both Intacs and Keraring are considered effective and safe for this case. A segment (0.45 mm) is placed in such a way that the cone and the thinnest part are bisected. For Keraring, one should always choose the incision on the steep meridian, and according to the spread of the steep point on both sides of the meridian, choose the type of the ring from nomograms A, B, or C. Since this patient’s vision with glasses is less than 20/40, the steep meridian should be identified by corneal topography.
Farid Karimian, MD
Based on the history and corneal topographic findings, this 23-year-old lady is a definite case of KCN. Age of onset together with visual acuity at the time of presentation indicate rapid progression. Topographic findings show a tear-drop appearance of the KCN cone. Considering keratometric values and according to Krumeich classification, the right and left eyes have mild and moderate KCN, respectively. When good to excellent best-corrected distance visual acuity (BCDVA) using RGP contact lenses is not achieved with this amount of keratometry and severity of KCN, other ocular pathologies should also be considered. The crystalline lens and retina should be carefully examined for other causes of reduced BCDVA. Amblyopia, which is a diagnosis of exclusion at this age, is very rare in eyes with KCN because progression of KCN is very rare in the first decade of life. To open the discussion, I assume no ocular pathology other than KCN is present in this young lady.
Treatment Plan
Due to the presence of Vogts’ striae and inferotemporal displacement of the cone in both eyes, a favorable result may not be achieved with ICRS. In my experience, Myoring (360 degree, round intracorneal ring) yields the best result in eyes with central cones accompanied by high amounts of myopia and astigmatism. Results of ICRS implantation, even in the best and most experienced hands, are not completely predictable. Considering the high cost of ICRS in our region, one has to discuss the somehow unpredictable results with the patient. I would prefer keratoplasty, preferably DALK, for the left eye which is more advanced and ICRS implantation, Keraring or Intacs, for the right eye provided that she accepts the terms and conditions.
Collagen Cross Linking (CCL)
Because of the progressive nature of KCN in this patient, I would suggest CCL after ICRS implantation in the right eye. It is better to have strong documentation, either by topographic findings or refractive data, before considering CCL. Based on the advanced nature of KCN together with low BCDVA in the left eye, CCL is not indicated in this eye and a more definitive plan (DALK) is preferable.
Type of ICRS
Due to the inferotemporal location of the cone on topography and the refractive error (low myopia, high astigmatism) in the right eye, segmental ICRSs have a better effect. Corneal thickness is another important factor. A minimum thickness of 350-400 µ is needed which is met in this case. Pupil diameter in both eyes is greater than 8.0 mm which is not rare in young patients. If pupil size is not due to the effect of mydriatic drops, it would constitute a relative contraindication for ICRS implantation. When pupil diameter is greater than 6.0 mm, it is better to recheck mesopic pupil size with the Colvard pupillometer to exclude the case.
Corneal topography, and the location and pattern of the cone, are also important for planning management. Central cones are better managed by round (360 or 355 degree) or 2 identical and symmetrical ring segments. If the cone and astigmatic pattern are asymmetrical, then asymmetric rings (both in length and thickness) should be used. Rings can be selected according to the proposed nomograms supplied by the manufacturers.
ICRS Position
The ring segment should usually be located over the steep meridian and the incision over the flat area. However, the location of the incision and position of ICRS is a matter of debate. Some authors place the incision on the flat meridian and others choose the steep meridian. Both groups have reported acceptable results and have their own preferences.
Keratoplasty Indication
Keratoplasty in the form of DALK is indicated in this young lady because she is in her active age and best corrected visual acuity (BCVA) with RGP is low (20/70) in her left eye. It is also important to make sure the patient has other qualifications for DALK including compliance and acceptance, a suitable job and finally postoperative availability for follow-up visits.
The Importance of Refraction
Considering the greater hyperopic shift with Myoring, it is more effective for eyes with high amounts of myopia and astigmatism. The magnitude of hyperopic shift in ICRS depends on segment length and thickness. Appropriate segment rings for the measured amount of myopia and astigmatism are suggested by the manufacturers.
Mehdi Khanlari, MD
Based on the provided data, the lady described herein is a case of moderate KCN in the right eye and severe KCN in the left one. Therefore, treatment should be directed not only to correction of vision, but also to halt progression of the ectatic process. As a non-surgical treatment it seems that spectacles are not a good option for this patient. Based on the level of BCDVA with RGP lenses (particularly 20/70 in her left eye), contact lenses may also not provide an acceptable outcome. Actually, low visual acuity in her left eye affects the success of any non-surgical or surgical treatment; however, CCL or ring surgery could be good modalities for the right eye. The left eye is a good candidate for penetrating or lamellar keratoplasty.
In the right eye, based on maximum K reading (52 D) and manifest refraction (-3.00-6.00×30), Intacs surgery using two asymmetric segments is a good choice; the thicker segment (450µ) should be inserted in the inferior tunnel and a thinner segment (350µ) should be placed in the superior tunnel, with incisions made on the 120º meridian. However, Pentacam may be more useful to locate the best site for the incisions. CCL for the right eye before or after ICRS implantation would be a very useful adjunct. In left eye, with K reading of 60 D and manifest refraction of -7.00 -8.00 ×140, Myoring (5-280 or 5-320) may be considered as an ICRS choice. However, as mentioned above and with a BCDVA of 20/70, good vision may not be easily possible.
I also strongly recommend contact lens re-fitting by another expert contact lens fitter. Because in the absence of any corneal scar, I expect better vision than that achieved in this case (especially in the left eye).
Topography has important roles in choosing the best treatment plan for ICRS implantation in a patient with keratoconus. It can be useful for selecting the incision site, segment thickness, and even the number of segments. Among different methods of corneal imaging (topography, Orbscan, Pentacam, etc.), my preferred method for selecting the incision and segment sites for ICRS surgery is the Pentacam.
It is noteworthy that in keratoconus patients, manifest refraction is not usually helpful and a meticulous subjective refraction by an expert has a more important role in planning treatment including incision site and ring type.
Figure 1.
Corneal topographic images of the right (upper image) and left (lower image) eyes of the patient.
Figure 2.
Orbscan images of the right and left eyes of the patient.
Footnotes
Conflicts of Interest
None.