Abstract
Purpose
To report the recurrence of keratoconus 49 months after deep anterior lamellar keratoplasty (DALK).
Case Report
A 21-year-old man with history of bilateral keratoconus who had undergone DALK in his right eye, presented with gradual visual loss 49 months after corneal transplantation. Slit lamp biomicroscopy revealed graft ectasia together with Vogt’s striae in the posterior stroma and corneal topography demonstrated inferior steepening. With a diagnosis of recurrent keratoconus in the graft, the patient underwent penetrating keratoplasty (PK) and histopathological examination confirmed the diagnosis of keratoconus in the graft.
Conclusion
Similar to PK, keratoconus can recur in the transplanted cornea after DALK. However, the time interval from transplantation to recurrence seems to be much shorter in DALK grafts.
Keywords: Keratoconus, Deep Anterior Lamellar Keratoplasty, Recurrent Keratoconus
INTRODUCTION
Keratoconus is a non-inflammatory ectatic corneal degeneration.1 Penetrating keratoplasty (PK) is a well established surgical intervention when other modalities such as contact lens wear, corneal collagen cross-linking, or intrastromal corneal rings fail to provide acceptable visual acuity in keratoconic eyes. However, PK breaches the anatomical integrity and disturbs the immunological status of the eye; these can lead to visual loss due to trauma or graft rejection. To reduce such risks, deep anterior lamellar keratoplasty (DALK) has gained popularity; this procedure leaves the recipient Descemet’s membrane (DM) and endothelium in place and therefore better preserves globe integrity against blunt trauma and eliminates the risk of endothelial graft rejection.2
In spite of these advantages, there are still several aspects of DALK grafts to be elucidated. For example we previously reported acute hydrops in a transplanted cornea after DALK using the big-bubble technique.3 It may be possible that retention of abnormal DM and posterior stroma encourages the progression of degenerative changes leading to recurrence of keratoconus after DALK. Although, recurrent keratoconus has also been reported following PK, this seems to be a rare complication which occurs no earlier than 2 decades after surgery.4-8 Herein, we present the second case of recurrent keratoconus relatively short after DALK.
Case report
A 21-year-old man with advanced keratoconus of the right eye underwent DALK in March 2006. He had no history of allergic diseases such as vernal keratoconjunctivitis and atopy, or any previous ocular/systemic disorders and surgeries. DALK using Anwar’s big-bubble technique was attempted but failed to yield a bare DM, therefore layer-by-layer manual dissection employing a crescent blade (Alcon Laboratories, Fort Worth, TX, USA) was performed to remove as much corneal stroma as possible. An 0.25 mm-oversized corneal graft (8.50 mm) was harvested from a male donor aged 20 years. Death-to-preservation time was less than 30 hours while preservation-to-transplantation time was 72 hours. After DM and endothelium removal, the donor cornea was secured to the recipient bed with 8 separate 10-0 nylon sutures accompanied by a single running 10-0 nylon suture (Sharpoint, Angiotech, Vancouver, BC, Canada).
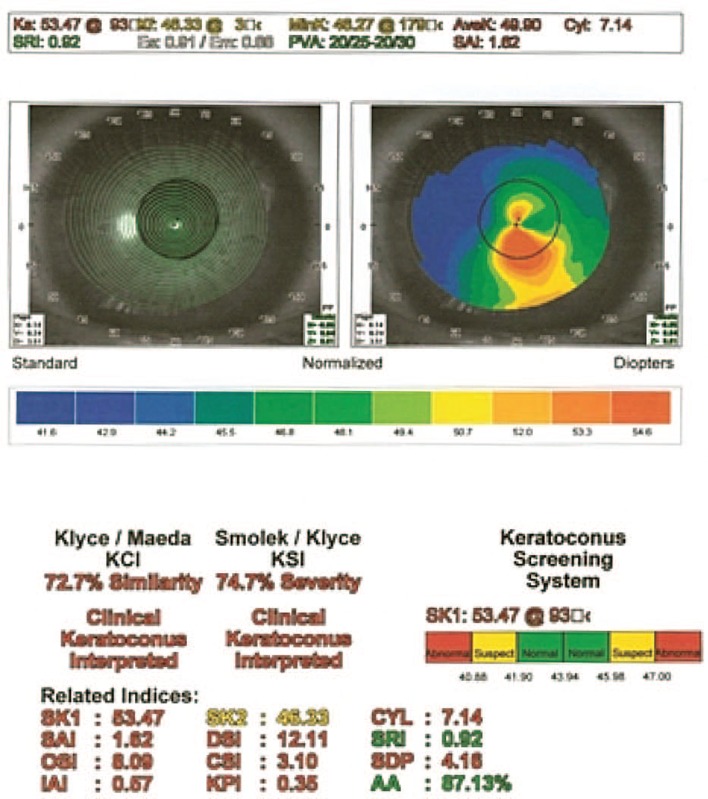
The postoperative course was uneventful and selective removal of the separate sutures was started after 6 months, and completed by month 12 with removal of the running suture. Thereafter, manifest refractive error dramatically changed from +2.5-1.0×180 at month 14, to -2.75-6.0×180 at month 49 (at the last visit prior to regrafting) which provided best-corrected visual acuity of 20/80. Meanwhile, slit lamp examination revealed a centrally bulging graft with Vogt’s striae in the posterior stroma and an intact donor-recipient interface (Fig. 1). Additionally, there was a scissor reflex on retinoscopy and inferior steepening of the graft on corneal topography (Fig. 2). With a diagnosis of recurrence of keratoconus in the graft, the patient underwent PK in March 2011; the full thickness of the corneal disc containing donor epithelium and stroma together with recipient DM and endothelium were submitted in 10% formalin for histopathological evaluation.
Figure 1.
Slit lamp photograph of the right corneal graft at month 49. Thinning and steepening of the graft and Vogt’s striae in the posterior stroma are evident.
Figure 2.
Corneal topography demonstrates inferior steepening of the graft.
The eye that received the mate tissue belonged to a young girl with congenital glaucoma who underwent PK for corneal opacity. This graft had rapidly failed and was replaced with another graft after 1 month.
Histopathological examination
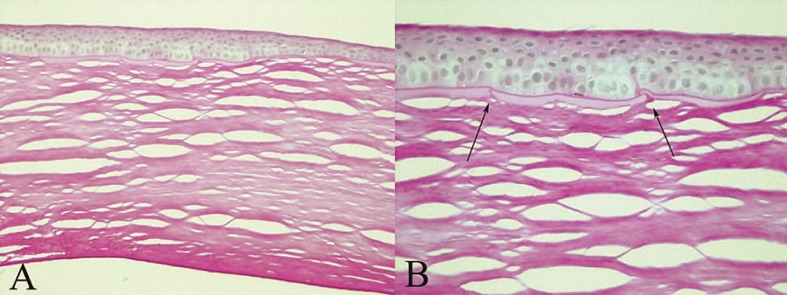
After bisecting the corneal disc into two halves, the specimens were processed and paraffin-embedded; thin 5-micron sections were prepared and stained with hematoxylin and eosin (H&E), and periodic acid-Schiff (PAS) for observation under light microscopy (Olympus BX43, Tokyo, Japan). Microscopic examination revealed focal thickening and irregularity of the corneal epithelium overlying breaks in Bowman’s layer in the mid-peripheral region. The graft stroma demonstrated thinning (340 microns) but no scar was present in the region of the ectasia. The donor-recipient interface was smooth and regular with very thin residual recipient stroma measuring 5 to 20 microns. The recipient DM and endothelium were unremarkable (Fig. 3).
Figure 3.
Histopathology of the graft at the site of ectasia. A, Note focal thickening and irregularity of the epithelium overlying breaks in Bowman’s layer and stromal thinning; the residual recipient stroma, Descemet’s membrane and endothelium are unremarkable (hematoxylin and eosin, ×200); B, Higher magnification of breaks (arrows) in Bowman’s layer (periodic acid-Schiff, ×400).
DISCUSSION
DALK may circumvent certain complications inherent to PK such as endothelial graft rejection and provide superior globe integrity.2 However, more experience is required to demonstrate whether or not DALK is superior to PK in all aspects. For example, recurrent ectasia in penetrating grafts which develops after 2 decades has been previously reported as a rare occurrence.9-11 The current case constitutes the second report of recurrent keratoconus after DALK, and was diagnosed clinically and confirmed by topography and histopathology 49 months following grafting. Histopathological features of the donor tissue were compatible with typical features previously defined for keratoconus.12 In a previous report we described a keratoconic eye which had undergone Anwar’s big-bubble DALK experiencing a rapid increase in keratometric astigmatism over a 52-month period leading to acute hydrops.3 These two eyes, out of 126 eyes undergoing DALK for keratoconus between January 2003 and December 2007, provide a recurrence rate of 1.6% over a mean follow-up period of 61 months.2 These findings are in contrast to PK in which the recurrence of keratoconus usually occurs after 2 decades.9-11
Several mechanisms have been proposed to explain recurrent keratoconus after PK. One speculative mechanism is failure to completely excise the cone which may lead to progression of keratoconus in the host tissue with possible involvement of the donor.13,14 This appears as progressive thinning of the host cornea, usually inferiorly, with secondary astigmatism. However, this theory is not applicable to our case as the recipient trephine size (8.25 mm) was large enough to include the entire ectatic area. Another postulated mechanism is the use of a donor with undiagnosed keratoconus; this is an uncertain assumption as the mate cornea was rapidly replaced without histopathological examination and therefore there was no chance to detect the possible development of keratoconus in this cornea.
Recurrence of keratoconus in a donor cornea has already been described9-11 and may well be manifestation of the same mechanisms that caused ectasia of the host cornea in the first place. This could be due to degradative enzymes liberated by abnormal host epithelium or infiltration of the graft by abnormal host keratocytes that produce abnormal collagen.15,16 This speculation is supported by histopathological characteristics such as abnormal epithelium and fragmented Bowman’s layer observed in donor grafts several years after PK.9,10,17
In contrast to PK, keratoconus recurred a few years after DALK. Such earlier recurrence can be attributed to several differences pertaining to the DALK surgical technique. First, retained keratocytes in the stromal bed may invade and replace donor tissue leading to recurrent keratoconus much earlier than what is expected in PK. We previously reported that even after successful big-bubble formation, some posterior stroma containing abnormal keratocytes remains in place.18 Second, removal of DM from the donor cornea, a common practice in DALK, can theoretically weaken donor tissue. Although our comparison of graft biomechanical properties between bare-DM DALK and PK in keratoconic eyes failed to demonstrate a significant difference,19 DM removal may actually yield donor tissue with less strength resulting in earlier manifestation of ectasia when keratoconus recurs in the DALK graft.
In summary, this case report indicates that recurrence of keratoconus is a possibility after DALK and appears to occur much earlier as compared to PK. The retention of abnormal keratocytes which can invade donor corneas and removal of DM which can render a weakened graft are among possible explanations for the recurrence of keratoconus after DALK.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Feizi S, Javadi MA, Jamali H, Mirbabaee F. Deep anterior lamellar keratoplasty in patients with keratoconus: big-bubble technique. Cornea. 2010;29:177–182. doi: 10.1097/ICO.0b013e3181af25b7. [DOI] [PubMed] [Google Scholar]
- 3.Javadi MA, Feizi S, Kanavi MR, Faramarzi A, Hashemian J, Mirbabaee F. Acute hydrops after deep anterior lamellar keratoplasty in a patient with keratoconus. Cornea. 2011;30:591–594. doi: 10.1097/ICO.0b013e3181d92866. [DOI] [PubMed] [Google Scholar]
- 4.Aldave AJ, Mabon M, Hollander DA, McLeod SD, Spencer WH, Abbott RL. Spontaneous corneal hydrops and perforation in keratoconus and pellucid marginal degeneration. Cornea. 2003;22:169–174. doi: 10.1097/00003226-200303000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Tuft SJ, Gregory WM, Buckley RJ. Acute corneal hydrops in keratoconus. Ophthalmology. 1994;101:1738–1744. doi: 10.1016/s0161-6420(94)31110-9. [DOI] [PubMed] [Google Scholar]
- 6.Grewal S, Laibson PR, Cohen EJ, Rapuano CJ. Acute hydrops in the corneal ectasias: associated factors and outcomes. Trans Am Ophthalmol Soc. 1999;97:187–198. [PMC free article] [PubMed] [Google Scholar]
- 7.Ezra DG, Mehta JS, Allan BD. Late corneal hydrops after penetrating keratoplasty for keratoconus. Cornea. 2007;26:639–640. doi: 10.1097/ICO.0b013e3180415d6b. [DOI] [PubMed] [Google Scholar]
- 8.Wickremasinghe SS, Smith GT, Pullum KW, Buckley RJ. Acute hydrops in keratoconus masquerading as acute corneal transplant rejection. Cornea. 2006;25:739–741. doi: 10.1097/01.ico.0000208824.55485.6a. [DOI] [PubMed] [Google Scholar]
- 9.Abelson MB, Collin HB, Gillette TE, Dohlman CH. Recurrent keratoconus after keratoplasty. Am J Ophthalmol. 1980;90:672–676. doi: 10.1016/s0002-9394(14)75135-9. [DOI] [PubMed] [Google Scholar]
- 10.Kremer I, Eagle RC, Rapuano CJ, Laibson PR. Histologic evidence of recurrent keratoconus seven years after keratoplasty. Am J Ophthalmol. 1995;119:511–512. doi: 10.1016/s0002-9394(14)71239-5. [DOI] [PubMed] [Google Scholar]
- 11.Pramanik S, Musch DC, Sutphin JE, Farjo AA. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology. 2006;113:1633–1638. doi: 10.1016/j.ophtha.2006.02.058. [DOI] [PubMed] [Google Scholar]
- 12.Scroggs MW, Proia AD. Histopathological variation in keratoconus. Cornea. 1992;11:553–559. doi: 10.1097/00003226-199211000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Ilari L, Daya SM. Corneal wedge resection to treat progressive keratoconus in the host cornea after penetrating keratoplasty. J Cataract Refract Surg. 2003;29:395–401. doi: 10.1016/s0886-3350(02)01487-6. [DOI] [PubMed] [Google Scholar]
- 14.Bechrakis N, Blom ML, Stark WJ, Green WR. Recurrent keratoconus. Cornea. 1994;13:73–77. doi: 10.1097/00003226-199401000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Teng CC. Electrone microscope study of the pathology of keratoconus: I. Am J Ophthalmol. 1963;55:18–47. doi: 10.1016/0002-9394(63)91645-3. [DOI] [PubMed] [Google Scholar]
- 16.Cannon DJ, Foster CS. Collagen crosslinking in keratoconus. Invest Ophthalmol Vis Sci. 1978;17:63–65. [PubMed] [Google Scholar]
- 17.Bourges JL, Savoldelli M, Dighiero P, Assouline M, Pouliquen Y, BenEzra D, et al. Recurrence of keratoconus characteristics: a clinical and histologic follow-up analysis of donor grafts. Ophthalmology. 2003;110:1920–1925. doi: 10.1016/S0161-6420(03)00617-1. [DOI] [PubMed] [Google Scholar]
- 18.Jafarinasab MR, Rahmati-Kamel M, Kanavi MR, Feizi S. Dissection plane in deep anterior lamellar keratoplasty using the big-bubble technique. Cornea. 2010;29:388–391. doi: 10.1097/ICO.0b013e3181ba7016. [DOI] [PubMed] [Google Scholar]
- 19.Jafarinasab MR, Feizi S, Javadi MA, Hashemloo A. Graft biomechanical properties after penetrating keratoplasty versus deep anterior lamellar keratoplasty. Curr Eye Res. 2011;36:417–421. doi: 10.3109/02713683.2011.556303. [DOI] [PubMed] [Google Scholar]