Abstract
We report a case of a life-threatening massive hemothorax caused by iatrogenic injury of the right subclavian artery. The patient was successfully treated with placement of a covered stent. During the procedure, occlusion balloon catheters rapidly controlled the massive bleeding.
Keywords: hemorrhage, minimally invasive therapy, subclavian artery injury
Introduction
Although accidental arterial puncture may follow 1 out of 20 central venous catheterization attempts,1) this complication is often recognized before the catheter is introduced into the blood vessel due to pulsatile backflow of oxygenated blood. Some patients experience massive bleeding from the insertion and immediate removal of a thin catheter into an artery. It was reported that the risk for serious complications after catheter removal increases with increases in the diameter of the catheter and length of time since catheter insertion.2) Thus, in cases when the diameter of the access route is large, complications caused by accidental arterial catheterization are sometimes serious.
Recently, we encountered a case of a life-threatening hemorrhage caused by inadvertent placement of a large vascular access catheter that damaged the right subclavian artery. For this case, we were successful in placing the covered stent on the area of injury, first by decreasing the blood flow with a balloon catheter.
Case Report
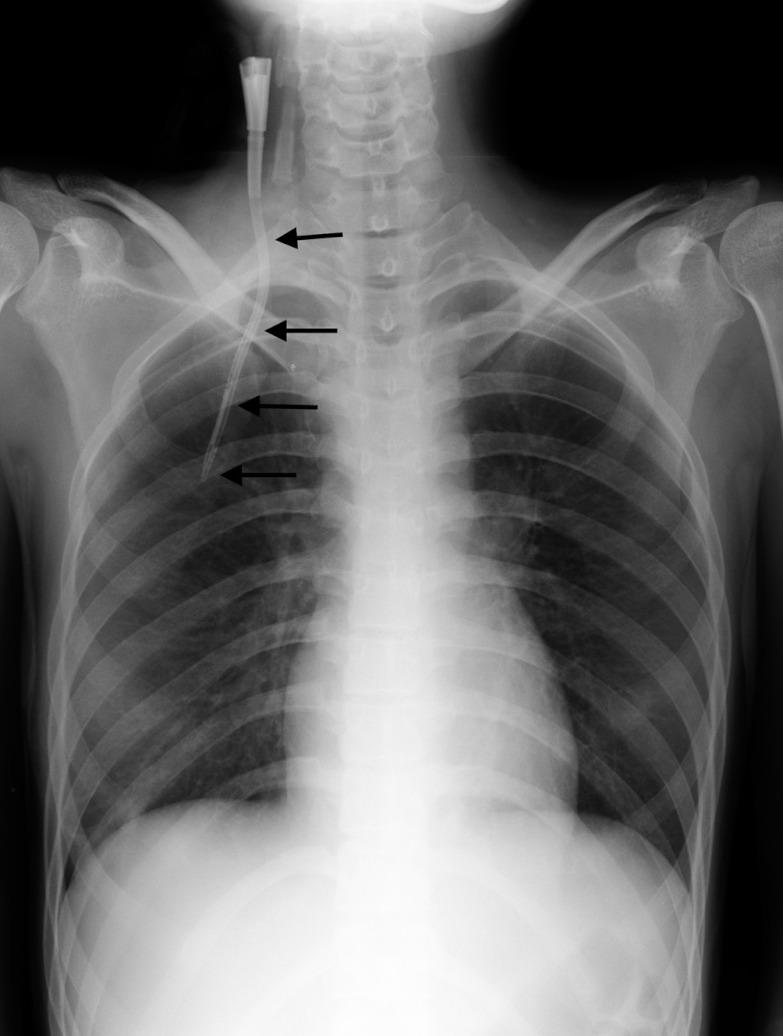
A 23-year-old woman with systemic lupus erythematosus and severe liver dysfunction had a bedside plasma exchange, by the insertion of an 11-F double lumen Shaldon catheter into the right jugular vein. The chest roentgenogram taken just after the catheter implantation led us to suspect misplacement of the catheter (Fig. 1). Enhanced chest computed tomography (CT) showed a right pneumohemothorax with the catheter running outside of the right jugular vein, close to the right subclavian artery with its tip located in the right pleural cavity. Before the procedure, the patient’s hemoglobin had been 10.3 g/dl, but just after the enhanced CT, it had decreased to 7.8 g/dl. At that time, the blood pressure was 112/75 mmHg and the heart rate was 58 beats/min. After the patient had given written informed consent, we began endovascular treatment with local anesthesia to stop the bleeding.
Fig. 1.
Chest roentgenogram of misplaced Shaldon catheter (arrows) after catheter implantation.
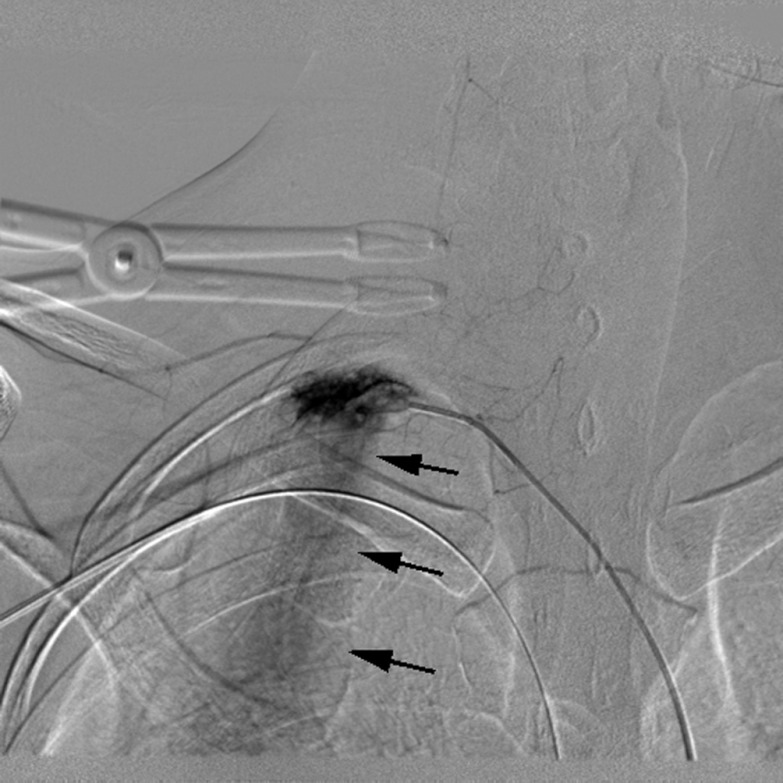
First, we inserted a 4-F catheter from the left femoral artery to the right subclavian artery. Since the right subclavian arteriogram showed no extravasations, we slowly withdrew the Shaldon catheter. Then, the blood pressure rapidly decreased to 82/21 mmHg, and the heart rate was 120 beats/min. The patient had temporary loss of consciousness. Then we took a right subclavian arteriograph, which revealed rapid and continuous extravasations from the right subclavian artery (Fig. 2). Second, after inflating the 5-F balloon catheter (9 mm diameter) at the point to decrease the bleeding, we removed the 4-F catheter. We then advanced a guide wire to the right brachial artery through the 5-F balloon catheter. Third, we advanced an 18-gauge intravenous catheter (Surflo; Terumo, Tokyo, Japan) at the guide wire and advanced the 5-F sheath introducer into the right brachial artery. Then, we advanced a 5-F balloon catheter (11 mm diameter) from the right brachial artery to the bleeding point and inflated the 5-F balloon to decrease the bleeding after withdrawal of the 5-F balloon catheter (Fig. 3). Fourth, we exchanged the left femoral artery sheath with a 9-F sheath introducer and a self-expandable metallic covered stent (8 mm diameter) and then inserted a 5-cm long stent (Niti-S ComVi stent; Taewoong Medical, Gimpo, Korea). Before deployment, the stent was advanced to the point where the brachial balloonwould be positioned. The brachial balloon catheter was deflated and pulled back to the distal part of the right subclavian artery. In the next instant, we placed the covered stent in the right subclavian artery to cover the bleeding point. After the stent placement, the hemorrhage was no longer visible in the right subclavian arteriography (Fig. 4). The stent successfully closed the source of bleeding of the right vertebral artery; however, the left vertebral arteriogram clearly showed centripetal flow in the entire right vertebral artery. After stent placement, we drained 2 liters of bloody pleural fluid with a chest tube. The entire procedure took approximately 3 hours.
Fig. 2.
Right subclavian arteriography of rapid and continuous extravasations from the right subclavian artery (arrows) after withdrawal of Shaldon catheter.
Fig. 3.
Right subclavian arteriography of inflated balloon catheter (arrow) advancing from the brachial artery with no extravasations.
Fig. 4.
Right subclavian arteriography of the stent (arrows) stopping the extravasations.
The anemia resolved after stent placement and infusion of 1300 mL of red blood cell concentrate. Plasma exchange was performed after re-insertion of the Shaldon catheter. Discharge of bloody pleural fluid from the chest tube immediately decreased and finally disappeared. The chest tube was removed 9 days after stent placement. Therapies for systemic lupus erythematosus were resumed. More than 5 months after stent placement, the patient did not experience any hemorrhaging from the right subclavian artery, and covering the origin of the right vertebral artery did not cause any neurological symptoms.
Discussion
There is widespread use of a central venous catheter to provide venous access for nutritional support or management of peri-operative fluids. Central venous access procedures are associated with inadvertent arterial puncture in up to 5% of cases.1) Because this complication is often recognized before the insertion of the catheter into the blood vessel, inadvertent arterial catheterization is much less common.
Treatment strategies after inadvertent arterial catheterization include local compression, open surgical treatment with direct arterial repair and percutaneous endovascular treatment.2) When hemostasis is not obtained by local compression,2, 3) surgical treatment or percutaneous endovascular treatment should be chosen.2, 3) Surgical treatment is usually safe; however, it can add significant morbidity as patients undergoing placement of a central venous catheter are often seriously ill and open repair can be complex, requiring general anesthesia and perhaps sternotomy.2) On the other hand, less invasive percutaneous endovascular treatment of the inadvertent catheterization of the carotid or subclavian artery can be performed while the patient is under local anesthesia. In such percutaneous endovascular treatments, there are two options: use of a percutaneous closure device or a stent graft.2–5)
In this study, while the patient was under local anesthesia, we successfully deployed a 5-cm Niti-S ComVi stent to stop a massive hemorrhage caused by inadvertent catheterization of a wide vascular access (11-F) to the subclavian artery. This stent is a self-expandable Nitinol covered by a 4-cm-long membrane of polytetrafluoroethylene, 0.5 cm uncovered at each end. For stoppage of massive bleeding, it is extremely useful to place the balloon catheter close to the bleeding area during withdrawal of the inadvertently placed catheter and until insertion of the stent. Even when an evident extravasation is not viewable in scans, the inadvertently placed catheter may be compressing the area and stopping the bleeding6, 7); thus, the catheter should not be withdrawn until preparations are ready for carrying out the procedure in the angiography room. Above all, we recommend ultrasonographic- and fluoroscopic-guidance in the angiography room for the safe insertion of a vascular access catheter, especially for those with large diameters. Insertion at the bedside should be avoided.
References
- 1.Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med 2006; 21: 40-6 [DOI] [PubMed] [Google Scholar]
- 2.Pikwer A, Acosta S, Kolbel T, Malina M, Sonesson B, Akeson J. Management if inadvertent arterial catheterization associated with central venous access procedures. Eur J Vasc Endovasc Surg 2009; 38: 707-14 [DOI] [PubMed] [Google Scholar]
- 3.Cayne NS, Berland TL, Rockman CB, Manadonado TS, Adelman MA, Jacobowitz GR.Experience and technique for the endovascular management of iatrogenic subclavian injury. Ann Vasc Surg 2010; 24: 44-7 [DOI] [PubMed] [Google Scholar]
- 4.Shetty SV, Kwolek CJ, Garasic JM. Percutaneous closure after inadvertent subclavian artery cannulation. Catheter Cardiovasc Interv 2007; 69: 1050-2 [DOI] [PubMed] [Google Scholar]
- 5.Midorikawa H, Kannno M, Ishikawa K, Takano T, Ono T, Morishima S. Endovascular repair of a Kommerell’s diverticulum and aneurismal right-sided aortic arch: a case report. Ann Vasc Dis 2009; 2: 54-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cil BE, Canyigit M, Penyircioglu B, Harizolan T, Carkaci S, Cekirge S.Subcutaneous venous port implantation in adult patients: a single center experience. Diagn Interv Radiol 2006; 12: 93-8 [PubMed] [Google Scholar]
- 7.Dede D, Akmangit I, Yildirim ZN, Sanverdi E, Sayin B. Ultrasonography and fluoroscopy-guided insertion of chest ports. Eur J Surg Oncol 2008; 34: 1340-3 [DOI] [PubMed] [Google Scholar]