Abstract
Objective: To identify the outcome of below knee bypass that focuses on the functional status and to investigate whether preoperative functional status can predict these outcomes.
Materials and Methods: One hundred and fifty one limbs in one hundred and thirty two patients that underwent below knee bypass between 2004 and 2008 were retrospectively reviewed. The patients were grouped as “ambulatory,” “non-ambulatory transfer” and “non-ambulatory bedridden,” according to their functional status. Clinical success was defined as the achievement of all of following end points; graft patency to wound healing, limb salvage for 1 year or until death, maintenance of ambulatory status for 1 year, and survival for 6 months. The effect of preoperative ambulatory status was analyzed.
Results: The overall primary and secondary graft patency, limb salvage and survival at 1 year were 76.3%, 81.8%, 89.1% and 84.1%, respectively. The overall success rate was 62.0%. Clinical success rates for the ambulatory and non-ambulatory groups were 75.6% and 34.9% (P = 0.0009, OR: 4.4; 95% CI: 1.8–10.6).
Conclusions: Bypass surgery is justified for maintaining the independent status of ambulatory patients. On the other hand, the high likelihood of poor outcomes for non-ambulatory patients must be considered before performing bypass surgery.
Keywords: below knee bypass, ambulatory status, clinical success rate, risk factors
Introduction
Due to an upward trend in the prevalence of risk factors for atherosclerosis, especially diabetes,1) the prevalence of peripheral arterial disease (PAD) is estimated to be increasing in Japan over the last decade. This has led to an increase in the number of patients undergoing bypass surgery and radiological intervention. Despite these therapies, the main outcomes, such as patency and limb salvage, remain as described by Rutherford in 1997.2)
Cardiovascular disease in patients with critical limb ischemia imposes obvious limitations on life expectancy. Thus, preserving functional status and minimizing complications after intervention for peripheral arterial occlusive disease are equally important to limb salvage and graft patency.
In this study, we examined the results of below-knee bypass based on various factors including ambulatory status and survival. And because we have focused on ambulatory status as one of the main outcome, this study also investigated whether preoperative ambulatory status affects the outcome of bypass surgery.
Materials and Methods
This study proceeded following the guidelines of the research ethics committee of our institution between January 2004 and December 2008. We obtained written, informed consent from patients with limb ischemia to perform below-knee bypasses. As a basic rule, we performed bypass surgery on all patients visiting our hospital with ischemic symptoms due to peripheral arterial disease. If bypass surgeries were possible to perform, we would offer bypass surgeries regardless of the patients’ mental status. We did not perform bypass surgery on patients who were regarded to be unable to tolerate the operation due to their medical comorbidities, had no recipient artery to perform a bypass, had infection or gangrene invading the site of anastomosis, had no vein usable as a graft, or refused to undergo the operation. Due to our policy, we did not perform any endovascular interventions on infrainguinal lesions.
The recorded preoperative characteristics were age, sex, hypertension, diabetes, renal failure, smoking status, serum albumin values, ejection fraction measured by transthoracic echocardiography as means of heart failure, sites of distal anastomosis and ambulatory status at 1 month before the onset of their ischemic symptoms. Patients were regarded as ambulatory if they could walk with or without a cane. As reported by Taylor, non-ambulatory patients were further classified as “non-ambulatory-transfer” if they could move into a wheelchair unassisted and the remaining patients were regarded as “non-ambulatory-bedridden.”3) For patients undergoing surgeries for bilateral limbs, data regarding the first surgery was used. When the surgery was performed simultaneously for both limbs, the more critical limb was analyzed.
A vein graft (reversed, non-reversed transposed or in-situ) was applied in all surgeries under total limb ischemia accomplished with a pneumatic tourniquet (non-dissection method).4–6) Postoperative computed tomography (CT) or angiography was performed 1–2 weeks after surgery, and a second operation was performed when necessary. The patients were asked to attend the hospital at 1- to 2-month intervals after discharge so that the status of the operated limb could be recorded. The patency of the graft was assessed by pulsation and Duplex sonography.
The results of the bypass surgery were analyzed using traditional graft patency, limb salvage, survival rate and the factors introduced by Taylor.3) A successful outcome was defined as the achievement of all of the following end points; graft patency to wound healing, limb salvage for 1 year or until death, maintenance of ambulatory status for 1 year and survival for 6 months. Transmetatarsal and toe amputations were regarded as limb salvage. Therefore, patients that were nonambulatory transfer preoperatively but nonambulatory bedridden postoperatively were regarded as a failure. Limb salvage was defined as the absence of lower limb shortening.
All data were analyzed using JMP 5.0 software (SAS Institute Inc.), and a P value of < 0.05 was considered significant in each analysis.
Results
Between January 2004 and December 2008, two hundred and two patients visited our hospital for critical limb ischemia. Below knee bypass was performed on 151 limbs in 132 patients, primary amputation was performed in 13 patients, and 57 patients were regarded as non-operable. As a result, the bypass surgery was performed in 65.3% of patients. Nineteen patients required bypass surgery for the contralateral limb simultaneously or later.
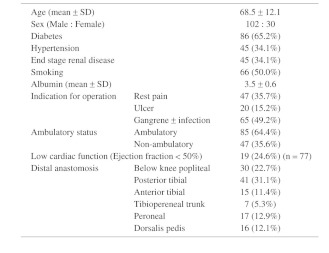
Of 132 patients, 85 (64.4%) were ambulatory, and 47 (35.6%) were non-ambulatory. Table 1 shows the baseline characteristics of the 132 patients. As in Table 1, all patients were operated for symptoms of critical limb ischemia, but 20 of the 85 ambulatory patients were severe claudicants one month before the operation. These claudicants had at least rest pain by the time of operation, which may seem a rapid change in ischemic condition. This was probably possible because we were able to perform most of the operation, especially patients whose symptoms changed rapidly, within one to two weeks after the first visit. The median follow up period was 14.5 months. The overall rates of primary and secondary graft patency, limb salvage and survival at 1 year were 76.8%, 81.1%, 89.2% and 83.8%, respectively. The overall clinical success rate was 62.3%.
Table 1. Baseline characteristics of 132 patients.
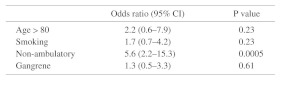
First, we performed univariate risk analysis on 132 patients regarding clinical success rate. As shown in Table 2, statistically significant factors were; age > 80, non-ambulatory status and gangrenous symptoms. Although not significant, smoking status tended to have some effect on clinical success rate. We then underwent multivariate analysis limited to these four factors. As in Table 3, the only significant factor was non-ambulatory status (P = 0.0005, OR: 5.6; 95% CI: 2.2–15.3).
Table 2. Univariate analysis for clinical success rate (n = 132).
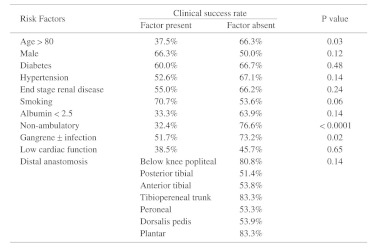
Table 3. Multivariate risk factor analysis for clinical success rate.
Discussion
Due to the increasing prevalence of risk factors for cardiovascular disease,1) it can be deduced that the prevalence of PAD is increasing in Japan, as in other countries. Infrainguinal bypass has been established as a treatment for PAD over the past few decades, and although the status of endovascular treatment has increased, bypass surgery remains the treatment of first choice for lesions below the knee.
The outcomes of lower extremity bypass surgery are traditionally assessed as graft patency, limb salvage and patient survival. Many factors including anatomical disease extent, clinical presentation, and resource availability can influence these outcomes.7) Despite the repeatedly documented ability of bypass surgery to achieve graft patency and limb salvage, legitimate concerns persist regarding the appropriate roles of these procedures.
One of the main concerns about bypass surgery is limited life expectancy, especially for patients with critical limb ischemia.8) Given the evident limitations on life expectancy imposed by critical limb ischemia,7) preserving functional status and minimizing complications after intervention for PAD are of equal importance to limb salvage and graft patency. Therefore, in addition to the traditional factors recommended by Rutherford,2) we used Taylor’s clinical success rate that included ambulatory status as a functional factor.3) Using these tools, we showed that the outcome after 1 year is worse in functionally dependent patients. The clinical success rate was considerably poorer in the non-ambulatory than ambulatory patients (32.4% vs. 76.6%). We are convinced that this is not due to technical problems because our overall success rate of 62.2% was comparable with that reported by Taylor (44.4%).3)
We were quite surprised that end-stage renal disease (ESRD) did not turn out to be a risk factor in our study. Due to the limited number of patients especially those with ESRD, this study can only say that the preoperative ambulatory status is more powerful risk factor compared with ESRD.
These findings indicate that ambulatory status is not only an outcome measure in bypass surgery, but also a preoperative risk factor that closely correlates with success rates. Crawford has also shown that preoperative functional status can predict perioperative outcomes (30-day morbidity and mortality) after infrainguinal bypass.9)
Abou-Zamzam has reported that 99% of survivors who lived independently before surgery continued to do so after surgery, whereas only 4% of survivors who did not live independently before the surgery achieved independence thereafter.10) Their study also concluded that preoperative non-ambulatory status and renal insufficiency or failure were independent predictors of death within 6 months. This report, together with our findings of better life expectancy for ambulatory patients (88.0% at 1 year) justifies performing bypass surgery on ambulatory patients to maintain their independence and ambulatory status.
On the other hand, these results also indicate a need for awareness of the poor outcomes of bypass surgery for non-ambulatory patients; however, this does not mean that primary amputation should be the first consideration for such patients. The potential effects of these strategies should be carefully compared before reaching a conclusion.
For example, the length of hospital stay and cost effectiveness should be considered. Chung found that wounds had not healed after 1 year in 25% of patients who had undergone infrainguinal bypass to treat critical limb ischemia.11) These patients might remain in hospital longer and thus miss the opportunity to be fitted with an appropriate prosthesis.
Primary amputation is by no means a safe remedy. Although not a randomized control trial, Sottiurai found that 30-day mortality rates of patients after femorodistal revascularization, below-knee amputations and above-knee (primary) amputations were 2.1%, 6.3% and 13.3%, respectively.12)
Lastly, primary amputation does not improve the outcomes of non-ambulatory patients. Taylor identified non-ambulatory status as a preoperative risk factor for an unsuccessful outcome after major lower limb amputation.13)
Conclusion
Due to relatively high success and survival rates, bypass surgery is justified for maintaining the independent status of ambulatory patients. On the other hand, for the non- ambulatory patients, in addition to the low probability of regaining ambulatory status, the high likelihood of poor general outcomes must be considered. Further studies should compare bypass surgery and primary amputation to determine a better strategy for treating PAD.
Reference
- 1.Kadota A, Miura K, Ueshima H. [Diabetes and cardiovascular disease in NIPPON DATA]. Nippon Rinsho 2010; 68: 847-52 [PubMed] [Google Scholar]
- 2.Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S.Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 1997; 26: 517-38 [DOI] [PubMed] [Google Scholar]
- 3.Taylor SM, Cull DL, Kalbaugh CA, Cass AL, Harmon SA, Langan EM., 3rdCritical analysis of clinical success after surgical bypass for lower-extremity ischemic tissue loss using a standardized definition combining multiple parameters: a new paradigm of outcomes assessment. J Am Coll Surg 2007; 204: 831-8 [DOI] [PubMed] [Google Scholar]
- 4.Bernhard VM, Boren CH, Towne JB. Pneumatic tourniquet as a substitute for vascular clamps in distal bypass surgery. Surgery 1980; 87: 709-13 [PubMed] [Google Scholar]
- 5.Sato O, Miyata T, Shindo S, Takayama Y, Tada Y. Nondissection method in distal arterial bypass surgery. Acta Chir Belg 1999; 99: 147-50 [PubMed] [Google Scholar]
- 6.Shindo S, Tada Y, Kamiya K, Suzuki O, Kobayashi M, Iyori K.Automatic sequential pneumatic tourniquet (pneumatic stocking) for distal bypass. J Vasc Surg 1995; 21: 869-70 [DOI] [PubMed] [Google Scholar]
- 7.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg 2007; 45Suppl S: S5-67 [DOI] [PubMed] [Google Scholar]
- 8.Criqui MH, Ninomiya JK, Wingard DL, Ji M, Fronek A. Progression of peripheral arterial disease predicts cardiovascular disease morbidity and mortality. J Am Coll Cardiol 2008; 52: 1736-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crawford RS, Cambria RP, Abularrage CJ, Conrad MF, Lancaster RT, Watkins MT.Preoperative functional status predicts perioperative outcomes after infrainguinal bypass surgery. J Vasc Surg 2010; 51: 351-9 [DOI] [PubMed] [Google Scholar]
- 10.Abou-Zamzam AM, Jr, Lee RW, Moneta GL, Taylor LM, Jr, Porter JM. Functional outcome after infrainguinal bypass for limb salvage. J Vasc Surg 1997; 25: 287-95 [DOI] [PubMed] [Google Scholar]
- 11.Chung J, Bartelson BB, Hiatt WR, Peyton BD, McLafferty RB, Hopley CW.Wound healing and functional outcomes after infrainguinal bypass with reversed saphenous vein for critical limb ischemia. J Vasc Surg 2006; 43: 1183-90 [DOI] [PubMed] [Google Scholar]
- 12.Sottiurai V, White JV. Extensive revascularization or primary amputation: which patients with critical limb ischemia should not be revascularized? Semin Vasc Surg 2007; 20: 68-72 [DOI] [PubMed] [Google Scholar]
- 13.Taylor SM, Kalbaugh CA, Blackhurst DW, Hamontree SE, Cull DL, Messich HS.Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg 2005; 42: 227-35 [DOI] [PubMed] [Google Scholar]


