Abstract
Primary infections of the aorta and infected aortic aneurysms are rare and are life threatening. Most of them are due to bacterial infection occurring in an atheromatous plaque or a pre existing aneurysm during bacteremia. Rarely spread from a contiguous septic process may be the cause. The reported hospital mortality ranges from 16–44%. Gram positive bacteria are still the most common causative organisms. More recently, Gram negative bacilli are seen increasingly responsible. The mortality rate is higher for the Gram negative infection since they most often cause supra renal aneurysms and are more prone for rupture. Best results are achieved by appropriate antibiotics and aggressive surgical treatment. Excision of the infected aneurysm sac as well as surrounding tissue and in situ reconstruction of aorta is the preferred treatment. Pedicled omental cover also helps to reduce infection. Long term antibiotic is needed to prevent reinfection. Mortality is high for those who undergo emergency operation, with advanced age and for nonsalmonella infection.
Keywords: aorta, aortitis, pseudo aneurysm, mycotic aneurysm
In 1885 Osler described in detail about the infected aneurysms and coined the term Mycotic aneurysm. Most of the early reports of infected aneurysms were due to infective endocarditis due to streptococcal infection. Later association with other septic foci such as osteomyelitis causing arterial infection was noticed. With the advent of antibiotics, the incidence of infective endocarditis and aortic infection declined. Recent years have seen an increase in the incidence of aortic infections due to increased use of immunosuppression, arteriography, intra-arterial invasive procedures and drug addiction.
Based on the clinical findings and etiology primary arterial infections have been classified into 4 types1) to which a fifth type can be added.
Mycotic aneurysm—due to septic emboli (embolomycotic). Usually from endocarditis.
Microbial arteritis—Bacteremia causes infection in an atheromatous plaque leading to destruction of the wall and aneurysm formation. This is most common in the aorta.
Infection of a pre existing aneurysm.
Post traumatic false aneurysm such as following penetrating injury, invasive intra-arterial cannulation or drug abuse.
Aortic infection from a contiguous organ with sepsis—from psoas abscess or osteomyelitis of vertebra or diaphragmatic abscess.
There are several theories to explain the pathology of aortic infection. Infected microemboli may lodge in the vasa vasorum causing occlusion and damage to the aortic wall which leads to degeneration and aneurysm formation. Emboli can also lodge in the irregular intima or the thrombus in the aneurysm during bacteremia. Aortic wall infection can occur due to direct inoculation into the arterial wall.
Aortic infection is known to occur after arteriography due to contamination. In the earliar days, majority of the aortic infections and infective aneurysms were caused by infective endocarditis due to streptococcal infection. Even now, majority of them are caused by Gram positive cocci mostly Staphylococci. Gram negative bacilli are rarer causes and Salmonella and Pseudomonas are the most commonly found bacteria. An analysis of all types of infected aneurysms revealed Gram positive bacteria in 41%, Salmonella in 15%, Pseudomonas in 3%, various other Gram negative bacteria in 13%, anerobic organism in 2% and fungal infection in 1%. Culture was negative in 25% of patients.2) Culture negativity may be because of antibiotic usage as well as failure to do routine anerobic culture. Routine cultures from the aortic wall during surgery have yielded positive cultures in 15%. Gram positive organism was seen in 81% and Gram negative in 19%.3) Tubercular aneurysms are extremely rare and less than 15 cases have been reported.4) They are usually due to direct extension to the vessel wall from a contiguous tuberculous focus in the lymphnode or vertebra. Hematogenous spread has also been suggested. Usually mycobacterium can be isolated from the abscess. If the Biopsy is typical, patient should be treated for tuberculosis even if Mycobacterium is not isolated. Fungal infection is known to occur in patients who are receiving immunosuppression. Most studies have shown that infection due to Gram negative organism is associated with higher incidence of suprarenal aneurysm, rupture and higher morbidity and mortality. Many of these patients are immunologically compromised and have severe atherosclerosis. Most patients with infection of a pre existing aneurysm tend to be in the infrarenal location since that is the more common site for the aneurysm. But infection of an atheromatous aorta leading to aneurysm formation is more often in the suprarenal location and hence is more difficult to manage.
Usually these patients present with high fever and abdominal or back pain. Palpable pulsatile tender mass, leucocytosis and positive blood culture are the classical signs. In some patients, palpable mass may not be there and even blood culture may be negative. Forty percent of the infected AAAs may not be palpable and may go unrecognized until rupture.1) After an analysis of infected aortoiliac aneurysms, Reddy et al. 1991 reported positive blood cultures in 69% and positive aneurysm wall cultures in 92% of patients.5) Hence a very high index of suspicion is needed to diagnose this condition. Unexplained fever in any patient over the age of 50 with atherosclerosis and with history of intravenous or intra-arterial cannulation should raise the suspicion of aortic infection.
Aortic aneurysms associated with vertebral body erosion and aneurysms devoid of calcification should raise the suspicion of infected etiology. Ultrasonography and arteriography of the aorta can only detect the aneurysm but cannot detect infection. The features suggestive of infective etiology are saccular aneurysm in an otherwise normal looking aorta and multilobulated aneurysm. CT or MR aortogram are more useful in identifying infection. Presence of peri aortic inflammation, nodes and abscess formation are diagnostic of infection (Fig. 1 and 2). Labelled white cell scanning has been used but has not been very accurate.
Fig. 1.
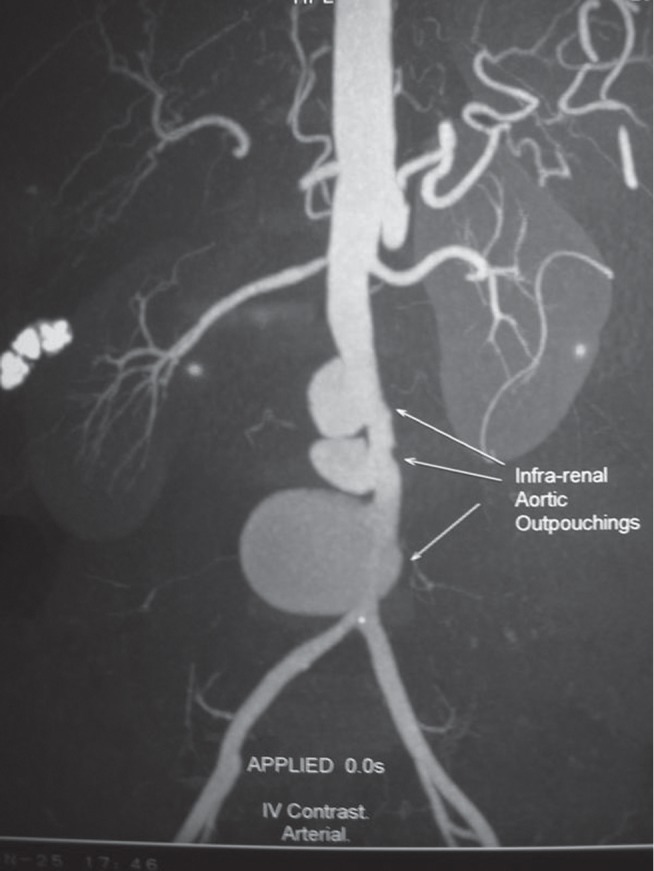
CT Aortogram showing multiple saccular out pouching-suggestive of infective etiology.
Fig. 2.
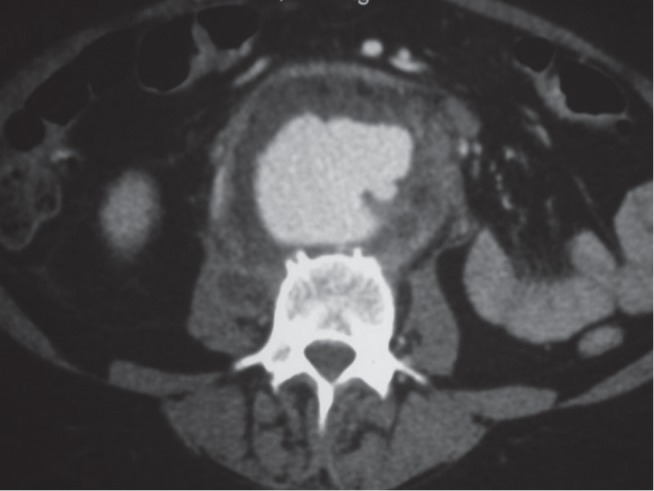
CT image of the same patient showing aortic aneurysm with evidence of periaortic Inflammation, abscess and absence of calcification. There is an abscess within the right Psoas muscle.
Treatment of an infected aorta is challenging. As soon as infected aorta is suspected, blood cultures for aerobic and anaerobic bacteriae and fungus should be sent and broad spectrum antibiotic therapy should be started. There is still controversy as to the timing of operation for these patients. If the fever subsides and the leukocyte count declines, antibiotic therapy can be continued for 4–6 weeks and then elective surgery may be performed. Early surgery is advised for those with uncontrolled infection, persistent fever, septic shock or evidence of threatened rupture in the form of severe pain, shock or enlarging pseudoaneurysm.6) It is better to be aggressive and perform early surgery to avoid rupture once the infection is under control. Very rarely medical therapy alone is successful. Hsu et al. analysed the results after medical treatment for infected aortic aneurysm and found that aneurysm related mortality was 82% for non Salmonella infection and 36% for Salmonella infection. They recommend surgery for all non Salmonella infection and medical treatment for high risk patients with Salmonella infection. They advice intravenous ceftrioxone for 6 weeks followed by life long oral ciprofloxacin for those with Salmonella infection.7)
Surgery includes resection of the aneurysm and debridement of all the surrounding infected tissue. Aneurysm wall should be sent for Gram stain and all cultures. Aortic reconstruction can be done in situ or extra anatomic through uninfected tissue planes. Traditionally infected infra renal aneurysms have been managed with ligation of the aorta and axillo bifemoral graft. However this procedure has the potential problems of graft patency of the extra anatomic bypass and aortic stump rupture caused by residual tissue infection. Alternatively in situ reconstruction with antibiotic bonded graft (rifampicin or silver) has shown good results8) (Fig. 3 and 4). Hsu et al. reported graft infection in only one out of 19 patients after in situ repair.6) Autogenous femoral vein grafts have also been used for in situ reconstruction with good results. But it is a major operation and has significant morbidity. Arterial homografts have also been tried for in situ reconstruction. But the results have been poor because of degeneration, aneurysm formation and thrombosis. When the aneurysm involves the renal or suprarenal segment, the infected segment of the aorta should be excised and ligated. Reconstruction is done by doing proximal anastomosis to uninvolved aorta. The visceral arteries are reconstructed by reimplantation or with separate grafts for them. It is tempting to do a patch aortoplasty for small saccular aneurysm. But the chance of reinfection of the patch is very high. It is better to resect that segment of the aorta and reconstruct. Omentopexy to cover the graft and the aneurysm bed after excising the infected sac and surrounding tissue has been found to be useful to reduce the risk of reinfection.9) Result of surgery largely depends on the virulence of the organism and the severity and extent of the aortic infection. For tubercular infections of the aorta, good debridement and in situ reconstruction have been successful provided adequate anti tubercular treatment has been given for a period of six to nine months.4)
Fig. 3.

Operative photo showing the infected sac and the posterior rupture of the same patient.
Fig. 4.
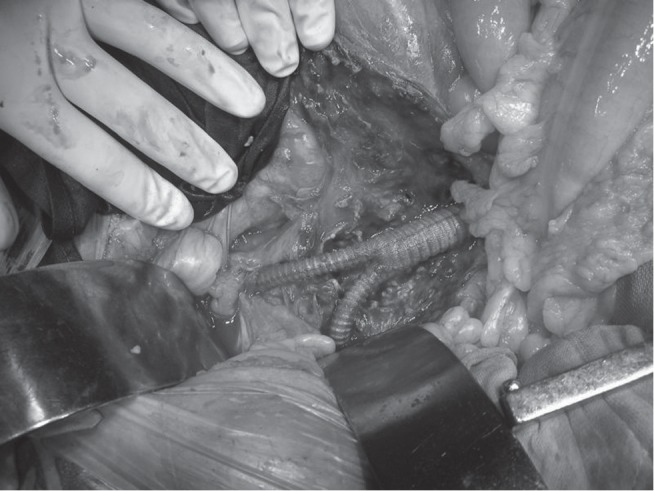
In situ Aortic reconstruction after complete excision of the infected tissue with silver impregnated coated Dacron graft. The graft was also wrapped with pedicled omentum.
Some have advocated use of drains and irrigation with antibiotic solution to prevent reinfection. Appropriate antibiotic should be continued in the postoperative period. Duration of antibiotic therapy is controversial. Most would agree that intravenous antibiotic should be given for 6–8 weeks and then oral antibiotic for another 6 months. Some have advised even longer duration of treatment.
The results after treatment of infected aortic aneurysms have improved over the years due to early diagnosis, improved surgical techniques and advanced microbial therapy. A review of six large series of infected aortoiliac aneurysms comprising of 149 patients reported a mortality of 23%.1) Hsu et al. reported no mortality when surgery was done electively and 36% mortality when done as an emergency. Non Salmonella infection, advanced age and nonoperative treatment were the other determinants of mortality.6) Oderich and colleagues have reported postoperative survival of 82% at one year after aggressive treatment.10)
References
- Reddy DJ, Weaver MR. Chap 108: Infected aneurysms. Rutherford Vascular Surgery, Elsevier Saunders, Philadelphia: 6th edition2006; 1581–96 [Google Scholar]
- Brown SL, Busutill RW, Baker JD, Machleder HI, Moore WS, Barker WF. Bacteriologic and surgical determinants of survival in patients with mycotic aneurysms. J Vasc Surg. 1984; 1: 541. [PubMed] [Google Scholar]
- Ernst CB, Campbell HC, Jr, Daugherty ME, Sachatello CR, Griffen WO., Jr Incidence and significance of intra-operative bacterial cultures during abdominal aortic aneurysmectomy. Ann Surg. 1997; 185: 626–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canaud L, Marzelle J, Bassinet L, Carrié AS, Desgranges P, Becquemin JP. Tuberculous aneurysms of the abdominal aorta. J Vasc Surg. 2008; 48: 1012–6 [DOI] [PubMed] [Google Scholar]
- Reddy DJ, Shepard AD, Evans JR, Wright DJ, Smith RF, Ernst CB. Management of infected aortoiliac aneurysms. Arch Surg. 1991; 126: 873–8 [DOI] [PubMed] [Google Scholar]
- Hsu RB, Tsay YG, Wang SS, Chu SH. Surgical treatment for primary infected aneurysm of the descending thoracic aorta, abdominal aorta, and iliac arteries. J Vasc Surg. 2002; 36: 746–50 [DOI] [PubMed] [Google Scholar]
- Hsu RB, Chang CI, Wu IH, Lin FY. Selective medical treatment of infected aneurysm of the aorta in high risk patients. J Vasc Surg. 2009; 49: 66–70 [DOI] [PubMed] [Google Scholar]
- Hayes PD, Nasim A, London NJ, Sayers RD, Barrie WW, Bell PR, et al. In situ replacement of infected aortic grafts with rifampicin bonded prostheses: The Leicester experience (1992-98). J Vasc Surg. 1999; 30: 92–8 [DOI] [PubMed] [Google Scholar]
- Fichelle JM, Tabet G, Cormier P, Farkas JC, Laurian C, Gigou F, et al. Infected infrarenal aortic aneurysms. When is in situ reconstruction safe? J Vasc Surg. 1993; 17: 635–45 [DOI] [PubMed] [Google Scholar]
- Oderich GS, Panneton JM, Bower TC, Cherry KJ, Jr, Rowland CM, Noel AA, et al. Infected aortic aneurysm: Aggressive presentation, complicated early outcome but durable results. J Vasc Surg. 2001; 34: 900. [DOI] [PubMed] [Google Scholar]


