Abstract
Objective: A less invasive method to assess internal thoracic artery (ITA) graft function after coronary artery bypass grafting (CABG) is desired. This study reports the novel method to estimate ITA graft function using CT angiography.
Materials and Methods: Fifty ITA grafts were assessed. Hounsfield Unit transition of each graft on the same cross section was detected during the Test Bolus Injection, which led to the making of a time density curve (TDC), for each ITA. Variables from the TDC were compared statistically with data obtained from Pulse Doppler Echo (PDE), the best indicator of graft function, of ITA grafts.
Results: The ascending slope of the TDC was significantly associated with the following PDE data: Velocity time integral (VTI), VTI × Heart Rate (HR) and Mean Flow of ITA graft. A multivariate analysis showed an especially strong relationship with the ascending slope of the TDC and VTI × HR (R2 = 0.588).
Conclusion: The ascending slope of the TDC means the concentration transition of contrast media, which may be affected by the blood stream in the ITA graft. This study suggests the possibility of the ability to assess ITA graft function by CT angiography.
Keywords: ita graft function, coronary artery bypass grafting, time density curve, ct angiography
Introduction
Postoperative assessment of internal thoracic artery (ITA) grafts after coronary artery bypass grafting (CABG) is important because it assesses the cardiac risk of the patient who undergoes surgery or provides feedback to surgeons.
Since graft angiography using the catheter technique implies the possibility of brain infarction or other thrombotic complications,1) CT angiography is considered a safe and useful examination to assess ITA grafts due to its image construction potentials.2–4) However, CT angiography is not a measurer of ITA graft function since it shows only a static image.
Pulse Doppler Echo (PDE) is reported to be a useful examination for the assessment of ITA graft function, in many articles.5–7) However, it is hard to obtain structural information of ITA grafts using PDE. If there is a method to assess ITA graft function by CT angiography, structural and functional information of ITA grafts can be obtained safely at the same time, which may be an ideal examination. This study reports the novel method to estimate ITA graft function using CT angiography.
Materials and Methods
50 ITA grafts including 32 left and 18 right ITAs were assessed in our institutions. ITA grafts were assessed in all cases using CT angiography and PDE after CABG. The time of examination after CABG range from 2 weeks to 30 months.
64-channel multidetector row helical CT scanner (Lightspeed VCD; GE Healthcare, USA) was used in all cases. During the CT examination, Hounsfield Unit (HU) transition of each graft on the same cross section was detected after the Test Bolus Injection (TBI), which led to the making of a time density curve (TDC) for each ITA graft. A TBI was carried out under certain conditions: 2-sec injection time, 30-mgI/kg contrast media use, and cross section filming every 2 seconds at the level of pulmonary artery bifurcation. The region of interest (ROI) was unified to 0.6 mm2 for the detection of the HU of each ITA. Patients, whose heart rate were over than 70 beats per minute, were administrated an intravenous β-blocker or calcium channel blocker to maintain the heart rate under 70 beats per minute during the CT examination to obtain more accurate CT images.
The PDE for the examination of ITA graft function was done in all patients, as well, by the supra-clavicular approach. Echocardiography for the assessment of general cardiac function was performed, as well. The left ventricular ejection fraction (LVEF) ranged between 55% and 80% in the study subjects. for minimization of the influence of cardiac function against ITA graft function, patients with an LVEF fewer than 50% or severe valvular heart disease were excluded from this study.
The TDC and PDE variables of each ITA graft were compared statistically to assess if some TDC variables had the potential to assume an ITA graft function similar to those of PDE.
Since study data were obtained from a routine postoperative CT angiography or PDE examination after CABG in our institutions, individuals were not identified in this study. Informed consent from all patients was obtained for the use of contrast media only.
Statistical Analysis
The statistical analysis was performed using SPSS 11.0 software (SPSS Inc., Chicago, IL, USA). A p value less than 0.05 was considered significant for all of the following statistical tests.
All data are presented as means ± standard deviation. For univariate analysis, correlation analysis was used, and for multivariate analysis, multiple regression analysis was used to identify the relationship with each variable.
Results
All ITA grafts were harvested by a full skeletonization technique in which a harmonic scalpel was used. All ITA grafts were grafted on left coronary artery area (left anterior descending area, 35 cases; left circumflex area, 15 cases). All ITA grafts were patent with no obvious stenosis at the time of examination, which was proven by CT angiography.
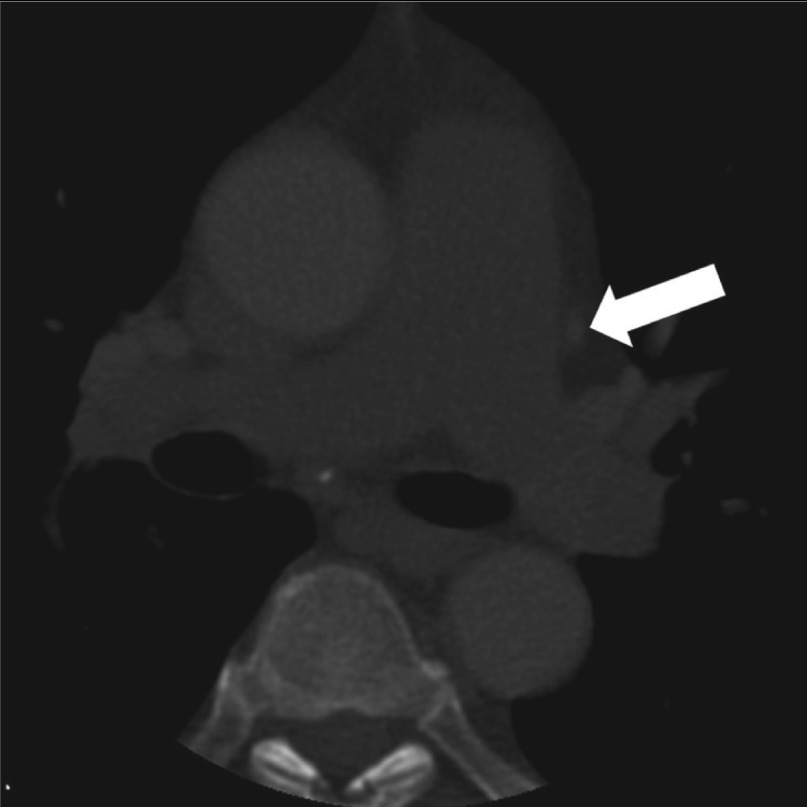
The variables obtained from the TDC (ascending slope, descending slope, peak value and ITA area of the cross section) and PDE (mean flow, maximum flow, minimum flow, velocity time integral (VTI), VTI × Heart Rate (HR), diastolic VTI, diastolic fraction (DF) and ITA area) are shown in Table 1. Figure 1 shows the cross section image where the ITA HU transition data was obtained, and Fig. 2 shows a representative TDC for the ITA.

Fig. 1.
The cross section image where the ITA HU transition data was obtained. White Arrow shows the ITA graft section. ITA: internal thoracic artery; HU: Hounsfield unit
Fig. 2.
The representative Time Density Curve of ITA graft. ITA: internal thoracic artery
The correlation analysis was performed, and it showed a significant correlation between ascending slope of the TDC and PDE variables (mean flow, maximum flow, VTI, VTIxHR, diastolic VTI) as shown in Table 2. Among them, an especially remarkable correlation was seen between ascending slope of the TDC and VTI×HR (R = 0.740), VTI (R = 0.706) and Mean Flow (R = 0.661). Table 3 shows the multivariate analysis of these variables, and it suggests a strong relationship of these variables as well, especially between the ascending slope of the TDC and VTI × HR (R2 = 0.588). Figure 3 shows the scatter plot of ascending slope of the TDC and VTIxHR that presents a linear correlation (y = 64x+327, R2 = 0.588) with each other.


Fig. 3.
The scatter plot of ascending slope of TDC and VTI×HR, which shows the linear relationship (y = 64x+327, R2 = 0.588) between ascending slope of TDC and VTIxHR. TDC: time density curve; VTI: velocity thoracic integral; HR: heart rate
Discussion
CT angiography gives a lot of structural information of ITA grafts.2–4) If ITA graft function is detectable using CT angiography, structural and functional information can be obtained safely at the same time, which is an ideal method of assessing ITA grafts. Although CT angiography is a safer method than graft angiography using a catheter, it is difficult to administer to patients with a chronic kidney disease because of the adverse effect of contrast media upon the kidney.8,9) Since, in our daily practice, as in this study, we avoid using contrast media in patients with diabetes mellitus, who has congestive heart failure and estimated glomerular filtration rate <60 mL/min/1.72m2, which is thought to be a risk factor of contrast media inducing acute kidney injury.10,11)
Many reports suggest the usefulness and feasibility of PDE in assessing ITA graft function.5–7) Those many reports recommended adopting mean flow, diastolic flow, VTI or DF of ITA graft to assess its function, which we adopted in this study, as well. In this study, the heart rate of subjects during the PDE examination ranged from 52 to 97 beats per minute, not only for VTI, which represented only one cardiac cycle, but also for VTI × HR, which was closer to the cardiac output and seemed to be a meaningful variable of PDE. Negative issues of PDE include the difficulty of the method itself, which means that it cannot be done easily for all cases and by all physicians or engineers, and earning less information of ITA graft structure including the anastomosis site.
According to the results of this study, ascending slope of the TDC was strongly correlated with the graft function data obtained from PDE. Ascending slope of the TDC means the concentration transition of contrast media, which may be affected by the blood stream in the ITA graft. Thus, this study results may suggest the possibility of CT angiography in assessing blood flow, in other words, graft function, of ITA graft after CABG. However, ITA grafts with significant stenosis were excluded, not assessed, in this study, further investigation is needed to assess ITA grafts with significant stenosis using this method.
There are some factors affecting the TDC: patient factors and non-patient factors, which cannot be ignored.12–15) Patient factors include body weight, heart rate, cardiac function and valvular heart disease. Non-patient factors include injection time of contrast media and injection quantity of iodine. Other factors may exist, as well. In this study, to minimize the influence of those known factors, we adjusted non-patient factors by adopting the constant injection time and body weight adjusted injection quantity of contrast media. Patients with a severe valvular heart disease or moderately decreased cardiac systolic function (LVEF <50%) were excluded from this study for minimizing the influence of patient factors. Thus, since this study was not adopted for all patients, we need a further investigation to expand the adaptation of this novel method.
Conclusion
Although there are some limitations, this study suggests the possibility of assessing ITA graft function by CT angiography. A further investigation, including an incomplete ITA graft, is needed.
Disclosure Statement
The authors declare that they have no conflicts of interest associated with this study.
References
- Hamon M, Baron JC, Viader F, et al. Periprocedural stroke and cardiac catheterization. Circulation 2008; 118: 678-83 [DOI] [PubMed] [Google Scholar]
- Ropers D, Pohle FK, Kuettner A, et al. Diagnostic accuracy of noninvasive coronary angiography in patients after bypass surgery using 64-slice spiral computed tomography with 330-ms gantry rotation. Circulation 2006; 114: 2334-41, quiz 2334 [DOI] [PubMed] [Google Scholar]
- Laynez-Carnicero A, Estornell-Erill J, Trigo-Bautista A, et al. Non-invasive assessment of coronary artery bypass grafts and native coronary arteries using 64-slice computed tomography: comparison with invasive coronary angiography. Rev Esp Cardiol 2010; 63: 161-9 [DOI] [PubMed] [Google Scholar]
- Feuchtner GM, Schachner T, Bonatti J, et al. Diagnostic performance of 64-slice computed tomography in evaluation of coronary artery bypass grafts. AJR Am J Roentgenol 2007; 189: 574-80 [DOI] [PubMed] [Google Scholar]
- Jones CM, Athanasiou T, Tekkis PP, et al. Does Doppler echography have a diagnostic role in patency assessment of internal thoracic artery grafts? Eur J Cardiothorac Surg 2005; 28: 692-700 [DOI] [PubMed] [Google Scholar]
- Chirillo F, Bruni A, Balestra G, et al. Assessment of internal mammary artery and saphenous vein graft patency and flow reserve using transthoracic Doppler echocardiography. Heart 2001. 86(4): 424-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Murgatroyd F, Widenka K, et al. Role of transcutaneous ultrasound in evaluation of graft patency following minimally invasive coronary surgery. Eur J Cardiothorac Surg. 1998; 14: S88-92 [DOI] [PubMed] [Google Scholar]
- Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis 2002; 39: 930-6 [DOI] [PubMed] [Google Scholar]
- Kagan A, Sheikh-Hamad D. Contrast-induced kidney injury: focus on modifiable risk factors and prophylactic strategies. Clin Cardiol 2010; 33: 62-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol 2004; 44: 1393-9 [DOI] [PubMed] [Google Scholar]
- Brown JR, DeVries JT, Piper WD, et al. Serious renal dysfunction after percutaneous coronary interventions can be predicted. Am Heart J 2008; 155: 260-6 [DOI] [PubMed] [Google Scholar]
- Terasawa K, Hatcho A. Contrast enhancement technique in brain 3D-CTA studies: optimizing the amount of contrast medium according to scan time based on TDC. Nihon Hoshasen Gijutsu Gakkai Zasshi 2008; 64: 681-9 [DOI] [PubMed] [Google Scholar]
- Bae KT, Heiken JP, Brink JA. Aortic and hepatic peak enhancement at CT: effect of contrast medium injection rate –pharmacokinetic analysis and experimental porcine model. Radiology 1998; 206: 455-64 [DOI] [PubMed] [Google Scholar]
- Bae KT, Heiken JP, Brink JA. Aortic and hepatic contrast medium enhancement at CT. Part II. Effect of reduced cardiac output in a porcine model. Radiology 1998; 207: 657-62 [DOI] [PubMed] [Google Scholar]
- Ichikawa T, Erturk SM, Araki T. Multiphasic contrast-enhanced multidetector-row CT of liver: contrast-enhancement theory and practical scan protocol with a combination of fixed injection duration and patients' body-weight-tailored dose of contrast material. Eur J Radiol 2006; 58: 165-76 [DOI] [PubMed] [Google Scholar]