Abstract
A secondary analysis of 1999–2002 Nebraska case-control data was conducted to assess the risk of non-Hodgkin lymphoma (NHL) associated with exposure to nitrate- and atrazine-contaminated drinking water. Water chemistry data were collected and weighted by well contribution and proximity of residence to water supply, followed by logistic regression to determine odds ratios (OR) and 95% confidence intervals (CI). We found no association between NHL risk and exposure to drinking water containing atrazine or nitrate alone. Risk associated with the interaction of nitrate and atrazine in drinking water was elevated (OR, 2.5; CI, 1.0–6.2). Risk of indolent B-cell lymphoma was higher than risk of aggressive B-cell lymphoma (indolent: OR, 3.5; CI, 1.0–11.6 vs. aggressive: OR, 1.9; CI, 0.6–5.58). This increased risk may be due to in vivo formation and subsequent metabolism of N-nitrosoatrazine. A larger study is warranted to confirm our findings.
Keywords: NHL, atrazine, nitrate, nitrosamines, drinking water
Introduction
In recent years, the incidence of non-Hodgkin lymphoma (NHL) has increased more rapidly in rural areas than in urban areas and has been consistently higher in Nebraska than the United States as a whole.1,2 In 2008, the Centers for Disease Control reported NHL incidence in Nebraska’s 93 counties ranged from 17/100,000 to 32/100,000 people.2 Agricultural practices,3–5 ingestion of nitrate-contaminated drinking water,6–10 and pesticide exposure11–14 have all been linked to an increased incidence of NHL.
Substantial nitrate and atrazine contamination of groundwater has occurred in Nebraska, mainly attributed to application of atrazine and nitrogen-based fertilizers, and exacerbated by irrigation.15–17 Ground-water provides more than 85% of Nebraska’s drinking water and median nitrate-N concentrations in Nebraska groundwater rose an average of 0.16 mg/L/year from 1978 to 1998.16 Atrazine (6-chloro-N-ethyl-N′-(1-methylethyl)-1,3,5-triazine-2,3-diamine) is a triazine herbicide widely used since its introduction in the 1960s, with peak application rates during the 1980s.18,19 Atrazine is one of the most prevalent corn herbicides and is the most common pesticide detected in US waters.20,21 A 1997 study reported co-occurrence of high nitrate-N concentrations in 70 drinking water wells testing positive for atrazine.22
Exposure to drinking water contaminated with both nitrate and atrazine may increase the risk of developing NHL due to in vivo nitrosamine formation.23–25 Many nitrosamines are known carcinogens26 and some are on the Environmental Protection Agency’s Unregulated Contaminant Monitoring Rule 2 list, raising concerns that nitrosamines may be related to drinking water toxicity. During digestion nitrate is reduced to nitrite and many secondary amines are nitrosated in the presence of nitrite under acidic conditions that are similar to those of the human stomach.27–30 Atrazine is a secondary amine that nitrosates to form N-nitrosoatrazine (NNAT), which has been shown to significantly increase chromosomal abnormalities in lymphocytes in vitro at low concentrations.31
A positive association between atrazine in drinking water and stomach cancer and a negative association between stomach cancer and nitrate in drinking water has been reported in an ecological study conducted in Canada. An evaluation of the interaction was not reported in that study.32 An association between nitrate in drinking water and an increased risk of NHL in Nebraska men and women has been reported,7 but there was no association with risk of any cancer, NHL, leukemia, melanoma or cancers of the colon, breast, lung, pancreas or kidney in Iowa women,10 or in case control studies conducted in Iowa and Minnesota.8,9 These discrepancies may be due to differences in study design, methodology used to determine exposure, analytical techniques, confounding due to other drinking water contaminants, or uncontrolled confounding due to other causes. To our knowledge, these studies did not control for exposure to atrazine, which may be a confounder in the Nebraska study, thereby showing a positive association between nitrate and NHL risk.
The methodologies used to determine exposure differ among studies and exposure data may be unreliable, leading to misclassification of exposure. Like many cancers, NHL has a long latency period and assessing risk associated with environmental exposures using historical data is difficult at best. Many study participants consume water from a complex public water supply (PWS) infrastructure. Based on the pathways of nitrosamine formation, metabolism and subsequent carcinogenicity, we hypothesized that exposure to both atrazine and nitrate would increase risk of NHL. The associations between risk factors and NHL histological subtypes are reportedly stronger than associations between the same risk factors and NHL in aggregate.33 Therefore we further hypothesized that differences would be observed based on NHL subtype (aggressive B-cell, indolent B-cell, and T-cell). The aims of our analysis were to: (1) estimate each subject’s exposure to the contaminants of concern from municipal wells that directly contribute to a subject’s exposure to atrazine and nitrate from his/her drinking water supply; (2) evaluate the association between NHL and drinking water contaminated with atrazine and/or nitrate; and (3) assess the association of exposure to nitrate- and/or atrazine-contaminated drinking water by NHL subtype.
Methods
Study population
The sample of participants for this analysis was selected from a population-based sample of 389 NHL cases and 535 controls recruited between January of 1999 and December of 2002.34 Participants included males and females of white, black, Hispanic, Asian, and Native American origin, aged 21 to 75, and residing in Nebraska. Cases were identified using a rapid-reporting system through the Nebraska Lymphoma Registry and Tissue Bank and were eligible for the study if they met the following criteria: (1) diagnosed with NHL; (2) resided in one of 66 counties in eastern Nebraska at the time of diagnosis; (3) between 20 and 75 years of age; (4) alive at the time of initial contact; (5) had histologic and microscopic confirmation of the diagnosis; (6) had no history of other cancer or HIV infection; and (7) mentally competent to participate. Of 949 cases identified, 529 met eligibility requirements and were administered a telephone interview (for the non-dietary part of the questionnaire) and mailed a questionnaire (for collection of dietary information). Three hundred eighty-nine subjects were enrolled in the study (73.4% participation rate). Outright refusals by subjects and physicians accounted for 21% and the remaining 5.5% could not be contacted. All tumor cases were classified according to the NHL classification system of the World Health Organization.35
Eligible controls were identified by two-stage random-digit dialing by the Iowa State University Center for Survey Statistics and Methodology. Controls without a history of HIV infection and cancer were randomly selected from the same geographical area as cases with frequency matching by age (five-year age groups) and sex using a 1.5 to 1 matching ratio. Controls also needed to meet the following eligibility criteria: (1) a resident in one of 66 counties in eastern Nebraska; (2) alive at the time of initial contact; and (3) mentally competent to give informed consent. Of 697 eligible controls, 535 participated in the study (76.8% participation rate). The main reasons for non-participation were subject refusal (n = 116), concern regarding blood collection (n = 10), subject could not be contacted (n = 28), or illness (n = 8).34
After obtaining informed consent, 924 Nebraska residents aged 21 to 75 were interviewed by telephone. Information on basic demographics, tobacco use, and family history of cancer was obtained, as well as additional information about city and state of residence between 1970 and the interview date, the number of years lived at each residence, and past sources of drinking water.34,36
Exact addresses were collected for the most recent residence whereas previous residences included only city and state. It was imperative for identifying the associated water source(s) that the exact location of all residences be known. A subgroup of participants from the original study was included in the analysis. This subgroup included those subjects who reported one residence between 1978 and recruitment. Tumor classes were categorized as aggressive B-cell lymphoma, indolent B-cell lymphoma, or T-cell lymphoma. The protocol for use of human subjects in this research was approved by the Institutional Review Board at the University of Nebraska Medical Center (IRB# 318-05-EP).
Water data: assessment and variables
For each PWS represented in this study, the manager was contacted to confirm that the address of interest was connected to the PWS during the time period of interest. Fifty-nine participants listing private well as their water supply were excluded for lack of well water quality data. Private wells are not subject to mandatory testing under the Safe Drinking Water Act (SDWA). One hundred and forty cases and 192 controls were eligible to participate in this study, representing 98 PWSs.
Archived records of nitrate and pesticide concentrations were obtained from the Nebraska Department of Health and Human Services and PWS managers. Data extracted and transcribed for 1967 through 1998 included the date the well went into service, annual well production during the time period of interest, contaminant concentrations, and geographical location of residence respective to the well(s) or storage reservoir of interest. Not all wells contribute an equal amount of water to the PWS. Pumping volumes for PWS wells are calculated and reported annually. From these data, we calculated yearly exposure concentrations for each contaminant per study subject. For each subject, total annual production of each well contributing to the subject’s residence was multiplied by the average contaminant concentration for that well, then weighted based on the percentage of that well’s contribution relative to the total contribution of all wells pumping into the distribution system, for the residence of interest. These annual exposure concentrations were then averaged to give a final exposure concentration of each contaminant per participant.36 For those listing purified or bottled water as their water supply, concentrations were entered as 0, as were PWS values reported as “no detect” or “< MDL” (less than method detection limit). All nitrate and pesticide analyses were performed at the State of Nebraska’s Department of Public Health Environmental Laboratory in Lincoln. The analytical method used for the majority of pesticide analyses was USEPA 525 (GC-MS) and nitrate-N was analyzed using automated cadmium reduction. MDLs are determined on an annual basis. Reporting limits are determined from method detection limits and are 3 to 5 times greater than the MDL. We elected not to use censored data because reporting limits varied slightly from year to year. Therefore the use of 0 for non-detects simplified the methodology.
Atrazine and nitrate-N were the primary contaminants of interest but we also obtained information on methoxychlor, 2,4-D, simazine, and alachlor in order to eliminate confounding due to exposure to other pesticides in drinking water. Nitrate-N and pesticide concentrations were recorded together with month and year of the test result, well number, and well usage for the time period of interest. PWSs are required to monitor based on contaminant concentration but at a minimum the PWS must test annually for nitrate-N. The maximum contaminant level (MCL) for nitrate-N is 10 mg/L and has been an enforceable standard since 1992, when the Phase II rule was implemented by the EPA. If the concentration is greater than 5 mg/L, the PWS must increase the monitoring to quarterly intervals. The reporting limit for nitrate-N is 0.05 mg/L. Regulation of atrazine in drinking water began in 1992 following the 1986 amendment to the SDWA addressing synthetic organic compounds. The MCL for atrazine is 3 μg/L and monitoring must be performed every three years and increased to annually if atrazine is detected at or above the 0.08 μg/L reporting limit. Based on groundwater monitoring reports and research conducted in Nebraska evaluating atrazine application and irrigation trends, an assumption was made that the period of greatest exposure would occur during the latency period for NHL, believed to be 10–20 years before contracting the disease.15,36,37 If this assumption results in misclassification, it would likely underestimate exposure and bias the study toward the null hypothesis that there is no association between NHL risk and exposure to nitrate and atrazine in drinking water.
To estimate “lifetime exposure dose” for each subject, data generated from a 1989 report was used to estimate total tap water intake based on age and gender.38 The average yearly contaminant exposure for each participant was then multiplied by their total tap water intake and the yearly exposures summed for a lifetime dose.
Outcome and covariates
The primary outcomes of interest were all NHL cases and three subtypes of NHL: aggressive B-cell (mantle cell, diffuse large cell, Burkett, other B-cell, other), indolent B-cell (chronic lymphocytic/small lymphocytic, marginal zone, follicular), and T-cell (peripheral T-cell, other T-cell). Covariates assessed included adult body mass index (BMI), years of education, gender, ethnicity (white, Hispanic, black, Asian, Indian), family history of cancer (none, cancer other than NHL, cancer of unknown type, hematopoietic other than NHL, NHL), age, marital status (married, single, separated, divorced, widowed), smoking history (never, ever), and water supply (private well, community system, bottled water, other). Six participants in the subgroup and 43 participants in the original study group reported their drinking water source as “other”, which we were able to classify as PWS or bottled water. Agrichemical covariates assessed were methoxychlor, 2,4-D, simazine, alachlor, nitrate-N, and atrazine. The agrichemicals were evaluated initially as individual compounds and then as mixtures.
Statistical analysis
Analyses were conducted using SPSS (Statistical Package for Social Sciences version 17.0, IBM, Chicago, IL). Because we were analyzing a subset of the original sample, we examined whether restricting the analysis to those with only one residence might have selected for those at greater risk of NHL.
Descriptive statistics were used to summarize participant characteristics. Covariates and exposures to nitrate, atrazine, methoxychlor, 2,4-D, simazine and alachlor in cases and controls were compared using the odds ratio (OR) and 95% confidence intervals (CI) from univariate logistic regression models. Multivariable logistic regression was conducted; covariates identified in the univariate analysis and shown to be associated with case-control status and associated with the contaminant of interest were used to adjust the logistic regression model. For pesticides, exposed was defined as the pesticide ever being detected in the drinking water supply at a concentration above the method detection limit. The United States Geographical Survey classified 2 mg/L as being the background concentration for nitrate-N in groundwater in the USA.39 Thus, in this study, participants were dichotomized as either exposed to ≤2 mg nitrate-N/L or >2 mg/L. Multivariable models were then reduced using manual backward regression. To test whether the interaction of atrazine and nitrate in drinking water may be associated with increased risk of NHL, we calculated the effects of atrazine, nitrate, and the interaction of atrazine and nitrate using multivariable logistic regression. Adjusted ORs and CIs were calculated maintaining only those confounders and interaction terms with a two-sided P-value ≤ 0.05.
Results
Subgroup cases and controls tend to be older than original study participants (Table 1). The distribution of gender, race, and marital status was similar between the subgroup and the original study group, as was the distribution of smokers and nonsmokers, family history of cancer, BMI, and water supply. Participants in the original study group were slightly more educated than the subgroup. Both groups had a similar distribution of NHL type among cases; 47% of the original study group and 49% of the subgroup were diagnosed with diffuse large cell (aggressive B-cell). Of the original group, 48% were diagnosed with follicular lymphoma (indolent B-cell), as were 46% of the subgroup. T-cell lymphoma represents 5% of cancers in both the original study and the subgroup. There was no association between the number of residences and disease status, water supply, gender, race or marital status.
Table 1.
|
Original study population
|
Subgroup study population
|
|||
|---|---|---|---|---|
| Controls (n = 535) (58%) | Cases (n = 387) (42%) | Controls (n = 192) (58%) | Cases (n = 140) (42%) | |
| Age (years) | 59 (48–68) | 61 (54–76) | 65 (55–70) | 65 (56–72) |
| Median (IQR)‡ | ||||
| n (%) | n (%) | n (%) | n (%) | |
|
|
||||
| Education | ||||
| ≤ 12 | 241 (45) | 164 (43) | 95 (49) | 69 (50) |
| 13–15 | 141 (26) | 122 (32) | 49 (26) | 37 (27) |
| 16+ | 153 (29) | 97 (25) | 49 (25) | 32 (23) |
| Water supply | ||||
| Private | 71 (13) | 75 (20) | 0 (0) | 0 (0) |
| Community | 417 (78) | 284 (74) | 181 (94) | 134 (96) |
| Bottled | 16 (3) | 11 (3) | 7 (4) | 4 (3) |
| Other | 30 (6) | 13 (3) | 4 (2) | 2 (2) |
| Gender | ||||
| Males | 281 (52) | 214 (55) | 94 (49) | 70 (50) |
| Females | 254 (48) | 173 (45) | 98 (51) | 70 (50) |
| Race | ||||
| White | 512 (96) | 370 (96) | 188 (98) | 131 (94) |
| Hispanic | 3 (<1) | 6 (2) | 0 (0) | 2 (1) |
| Black | 11 (2) | 7 (2) | 4 (2) | 4 (3) |
| Asian | 4 (<1) | 3 (<1) | 0 (0) | 2 (1) |
| Indian | 5 (<1) | 1 (<1) | 0 (0) | 1 (<1) |
| Marital status | ||||
| Married | 362 (68) | 294 (76) | 125 (65) | 100 (71) |
| Single | 59 (11) | 23 (6) | 21 (11) | 7 (5) |
| Separated | 3 (<1) | 2 (<1) | 2 (1) | 0 (0) |
| Divorced | 51 (10) | 33 (8) | 16 (8) | 9 (6) |
| Widowed | 60 (11) | 34 (9) | 28 (15) | 24 (17) |
| Smoking status | ||||
| Ever | 219 (49) | 156 (47) | 72 (44) | 55 (48) |
| Never | 226 (51) | 173 (53) | 92 (56) | 60 (52) |
| Family history | ||||
| None | 260 (49) | 173 (45) | 60 (43) | 90 (47) |
| Other | 224 (42) | 161 (42) | 61 (44) | 84 (44) |
| Unknown | 8 (1) | 7 (2) | 1 (<1) | 3 (2) |
| Hematopoietic (not NHL) | 20 (4) | 24 (6) | 9 (7) | 9 (5) |
| NHL | 21 (4) | 19 (5) | 7 (5) | 5 (2) |
| BMI | ||||
| < 24 | 133 (25) | 85 (22) | 47 (25) | 31 (23) |
| 24.1–27 | 142 (27) | 95 (25) | 43 (23) | 36 (26) |
| 27.1–30 | 121 (23) | 78 (21) | 50 (26) | 23 (17) |
| > 30 | 134 (25) | 120 (32) | 50 (26) | 46 (34) |
| NHL type | ||||
| Aggressive B-cell | 181 (47) | 68 (49) | ||
| Indolent B-cell | 187 (48) | 64 (46) | ||
| T-cell | 19 (5) | 8 (5) | ||
Notes:
Those who reported living at one residence between 1978 and recruitment;
percentages may not always total 100% due to missing data;
Interquartile range.
The subgroup included 78 controls and 101 cases reporting a family history of cancer. In the univariate analysis, family history of cancer was not associated with increased risk of developing NHL and risk of NHL was not associated with BMI, smoking history, or education. There was no association between NHL risk and nitrate or atrazine, as well as no increased risk of developing NHL associated with methoxychlor, 2,4-D, simazine, or alachlor exposure (Table 2).
Table 2.
Univariate risk of NHL associated with BMI, smoking, education, family history of cancer, and drinking water contaminants.
| Controls (n ==192)* | Cases (n ==140)† | OR 95% CI | |
|---|---|---|---|
| BMI | 190 | 136 | 1.0 referent |
| 1.0 (1.0–1.1) | |||
| Smoking | 163 | 116 | |
| No | 92 | 60 | 1.0 referent |
| Yes | 71 | 56 | 1.2 (0.8–2.0) |
| Education | 190 | 136 | |
| ≤12 | 95 | 69 | 1.0 referent |
| 13–15 | 49 | 37 | 1.0 (0.6–1.8) |
| ≥16 | 49 | 32 | 1.1 (0.6–2.1) |
| Family history of cancer | 190 | 136 | |
| None | 90 (47%) | 61 (44%) | 1.0 referent |
| Other cancer | 83 (43%) | 61 (44%) | 0.5 (0.2–1.7) |
| Unknown cancer | 2 (2%) | 1 (<1%) | 0.5 (0.2–1.7) |
| Heme, not NHL | 9 (5%) | 9 (6%) | 0.2 (0.0–3.0) |
| NHL | 5 (5%) | 7 (5%) | 0.7 (0.2–1.0) |
| Contaminants | |||
| Nitrate | |||
| Nitrate (≤2 mg) | 135 (70%) | 102 (73%) | 1.0 referent |
| (>2 mg/L) | 57 (30%) | 38 (27%) | 0.9 (0.5–1.4) |
| Atrazine | |||
| Never | 93 (48%) | 58 (41%) | 1.0 referent |
| Ever | 97 (51%) | 80 (57%) | 1.2 (0.8–1.7) |
| Methoxychlor | 189 | 137 | |
| Never | 142 (75%) | 104 (76%) | 1.0 referent |
| Ever | 47 (25%) | 33 (24%) | 1.0 (0.7–1.3) |
| 2,4-D | 169 | 138 | |
| Never | 93 (55%) | 76 (55%) | 1.0 referent |
| Ever | 76 (45%) | 62 (45%) | 1.1 (0.9–1.8) |
| Simazine | 190 | 138 | |
| Never | 162 (85%) | 122 (88%) | 1.0 referent |
| Ever | 28 (15%) | 16 (12%) | 0.8 (0.4–1.5) |
| Alachlor | 189 | 138 | |
| Never | 161 (85%) | 120 (87%) | 1.0 referent |
| Ever | 28 (15%) | 18 (13%) | 0.9 (0.5–1.6) |
Notes:
Controls may not sum to 192 due to missing data;
cases may not sum to 140 due to missing data.
Thirty-six percent of Nebraska’s population resides in the state’s two major cities, Lincoln and Omaha; in this analysis 51% (n = 163) of participants listed Omaha or Lincoln as their city of residence. We excluded participants from Lincoln and Omaha and repeated the analysis to ensure that our results were not biased toward residences in these cities. NHL risk associated with nitrate exposure was unchanged. The same sample showed risk of NHL in those exposed to atrazine as slightly elevated (OR, 1.3; CI, 0.9–1.9) but not significantly (P = 0.20).
Multivariable logistic regression showed the relationship between the log odds and atrazine increased by 0.916 (SE = 0.48) when nitrate-N exposure was greater than 2 mg/L as opposed to nitrate-N exposure of 2 mg/L or less. After transforming into odds, our statistical model resulted in the odds of developing NHL being 2.9 times greater when subjects were exposed to both nitrate- and atrazine-contaminated drinking water (OR, 2.9; CI, 1.1–7.4) (P = 0.025) as opposed to when only atrazine or nitrate was present. After adjusting for age (by adding age as an additional continuous independent variable in the model), the risk of developing NHL remained elevated (OR, 2.5; CI, 1.0–6.2) (P = 0.047) (Table 3).
Table 3.
Age adjusted odds ratios (ORs) and 95% confidence intervals (CI) from univariate and multivariable main effects and interaction models of nitrate, atrazine, and the interaction of nitrate and atrazine in assessing risk for NHL in Nebraska.
| No. of controls* | No. of cases† | Univariate OR (95% CI) | Multivariable OR (95% CI) | |
|---|---|---|---|---|
| Nitrate | 192 | 140 | ||
| Never | 135 | 102 | 1.0* | 1.0 referent |
| Ever | 57 | 38 | 0.9 (0.5–1.4) | 0.6 (0.3–1.1) |
| Atrazine | 190 | 138 | ||
| Never | 93 | 58 | 1.0* | 1.0 referent |
| Ever | 97 | 80 | 1.2 (0.8–1.7) | 1.0 (0.7–1.4) |
| Atrazine + nitrate | 190 | 138 | ||
| Never | 174 | 120 | ||
| Ever | ||||
| NHL in aggregate | 16 | 18 | 2.5 (1.0–6.2) | |
| Indolent B-cell NHL | 16 | 7 | 3.5 (1.0–11.6) | |
| Aggressive B-cell NHL | 16 | 11 | 1.9 (0.6–5.6) |
Notes:
Controls may not sum to 192 due to missing data;
cases may not sum to 140 due to missing data.
We investigated the association of nitrate and atrazine with risk of NHL by subtypes. After adjusting for age, the risk of indolent B-cell lymphoma (n = 64) was significantly greater (OR, 3.5; CI, 1.0–11.6) (P = 0.04) for those exposed to drinking water containing both nitrate and atrazine than those not exposed. There was also an elevated, but non-significant risk (OR, 1.9; CI, 0.6–5.6, P = 0.26), for aggressive B-cell lymphoma (n = 68). Analysis by subtype strongly suggests that those exposed to nitrate- and atrazine-contaminated drinking water may be at greater risk for indolent B-cell lymphoma than aggressive B-cell lymphoma. The number of T-cell lymphoma cases was small (n = 8) and therefore not included in this analysis.
Approximately 30% of controls and 27% of cases were exposed to average nitrate-N concentrations greater than the background level of 2 mg/L while still not showing an association with increased risk of NHL in the univariate analysis. Similarly, no associated risk of NHL was found when cutoff values were lowered to 1 mg/L or 0 mg/L modeled as binary variables. Atrazine exposure occurred in 51% of controls and 57% of cases but there was no NHL risk associated with drinking water contaminated with atrazine. There was no difference in mean nitrate exposure or mean atrazine exposure over time between cases and controls. When mean nitrate and mean atrazine exposures were multiplied, the resulting median exposure was eight times greater for cases than controls (0.42 for cases and 0.05 for controls respectively).
Discussion
For many years, the risk of developing NHL has been postulated to be associated with exposure to nitrate-contaminated drinking water and to pesticides such as the commonly used herbicide atrazine; however, studies have been inconsistent in confirming these associations.6,7,11 To our knowledge, this is the first case-control study to examine the risk of NHL associated with exposure to both nitrate and atrazine in drinking water. No association between NHL risk and drinking water containing nitrate or atrazine alone was observed; however our analysis suggests increased NHL risk for subjects exposed to drinking water containing both nitrate and atrazine. We hypothesize that endogenous formation and subsequent metabolism of N-nitrosoatrazine is responsible for carcinogenesis. The atrazine molecule has two secondary amine moieties and can form mono-N-nitrosoatrazine or di-N-nitrosoatrazine. We synthesized mono-NNAT according to the method of Mirvish et al40 and found it very stable when stored at 0 °C in an amber vial. We also found that NNAT formed readily in aqueous solution at a pH between 2 and 4, comparable to that of the human stomach, and in soil at pH ≤ 5.41 Di-nitrosated atrazine is much less stable and readily decomposes to mono-NNAT.42 Both nitrosamines may be forming during digestion and di-NNAT could be more toxic than mono-NNAT. No di-NNAT was detected in the soil and water experiments.
Many nitrosamines have been reported as carcinogenic in animal models.26,43–45 Studies have shown that nitrosamines act differently depending on chemical structure and physicochemical properties, and that metabolism can vary among nitrosamines.46,47 Meisner et al31 reported significant increases in chromosome breakage in human lymphocytes exposed to 0.1 μg NNAT/L, a 1,000 to 10,000-fold smaller concentration than nitrate, nitrite, and/or atrazine producing comparable damage.31 Contamination of groundwater with atrazine and nitrate can be chronic and nitrosamines are reportedly more effective in tumor induction when administered chronically than as a single large dose.43 The specific mechanism of action for NNAT is not known, but the mechanism most frequently attributed to N-nitrosamine carcinogenicity requires metabolic activation by a cytochrome P450 enzyme, most commonly CYP450 2E1. In this reaction, an intermediate radical is generated and subsequently hydroxylated at the α-carbon to produce a hydroxynitrosamine. The hydroxynitrosamine is unstable and decomposes to an alkyldiazonium ion, which is an aggressive alkylating agent.27,29 Alkyldiazonium ions can alkylate DNA bases, especially at N-7 and O-6 of guanine and O-4 of thymine. Cancer initiation is thought to occur when the O-6-alkylguanine pairs with thymine rather than cytosine, producing G:C-A:T mutations.27,44,48 Although the topic is controversial, researchers have concluded that neither nitrate nor atrazine are mutagenic or carcinogenic49–54 and the results of our exploratory study are consistent with those reports.
For nitrosation to occur, the concentration of available nitrite must be at least four times that of the nitrosatable compound.40 In the present study, subjects exposed to both nitrate and atrazine were exposed to nitrate at a concentration nearly 1000 times greater than atrazine. Approximately 5% of ingested nitrate is converted to nitrite in saliva.27 Simultaneous exposure to 1 mg of nitrate and 1 μg of atrazine in 1 L of drinking water would yield a nitrite concentration 50 times greater than atrazine, which is more than adequate for nitrosation.
When conducting epidemiology studies assessing disease risk due to drinking water exposure, the contribution of water supply infrastructure must be considered to limit misclassification. The 1996 study7 evaluating NHL risk associated with exposure to nitrate in drinking water included all well and distribution data which could have led to exposure misclassification, producing a false positive finding (type I error). Many PWS wells are routinely sampled but do not provide drinking water and are not decommissioned and remain available for fire protection, irrigation and for uses other than human consumption. Data from these wells are entered into the Nebraska Health and Human Services drinking water database as an active well. Unless a well is formally decommissioned and capped, quarterly monitoring is required under the SDWA. These wells may have higher nitrate concentrations or detectable levels of atrazine, biasing results away from the null hypothesis of no association between exposure to nitrate and atrazine in drinking water and the risk of developing NHL. To reduce misclassification we investigated the PWS infrastructure and only included wells contributing to a subject’s residence. Furthermore, sampling from the distribution system occurs at random locations within the PWS and contaminant concentrations can differ depending on where the sample was obtained. Since 1993, sampling must be performed where the water enters the distribution system. This point of entry (POE) may be a treatment plant, reservoir, or well. Data in the current study were from samples obtained at the POE and water source inclusion/exclusion criteria were based on contribution to the location of interest. Finally, more water quality data have been compiled since the last Nebraska study, resulting in a more exact assessment of individual-specific drinking water exposures. Although the exclusion of participants not living at the same residence for the entire time period of interest reduced sample size, it more importantly eliminated exposure misclassification due to differences in drinking water quality between residence locations and exposure duration.
Consideration should be given to the limitations of the study. Transcription of large amounts of water data is not likely to be error-free but misclassification due to transcription errors should be minimal. Secondly, most environmental epidemiological datasets have missing exposure data for many participants. In this study, missing water data were generally due to data being destroyed (PWSs are required to maintain water quality records for only 10 years), frequency of monitoring (which depends on previous concentrations as monitoring of nitrate-N is required only yearly if the concentration is less than or equal to 5 mg/L and pesticide monitoring is required only every three years if no detection), and when the PWS implemented the SDWA (after passage of the SDWA, PWSs were allowed a few years for compliance). We generally assume that missing data alters the results of the analysis and makes findings less meaningful. In this analysis, results were unchanged using a first-observation-carried-forward or a last-observation-carried-backward method of imputation. Third, pesticide exposure history and occupational history, neither of which was available for this secondary analysis, could be confounding the results. The original study found that farmers using insecticides had a weak elevated risk of NHL (OR = 1.2; CI = 0.9–1.6) as did farmers who used herbicides (OR = 1.1; CI = 0.8–1.5), compared with non-farmers. Family history of hematopoietic cancer among first-degree relatives was significantly associated with increased risk of NHL (OR = 1.5; CI = 1.0–2.5) in the original study but not in this study. When the highest quartile of intake was compared with the lowest, the original study reported an increased risk of NHL associated with total fat (OR = 1.6; CI = 0.8–3.0). No apparent association between NHL and cigarette smoking was found.34
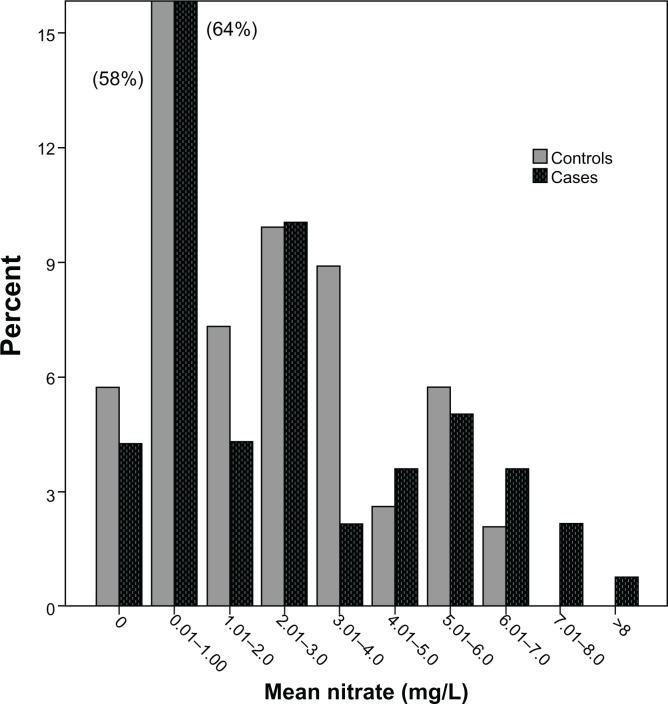
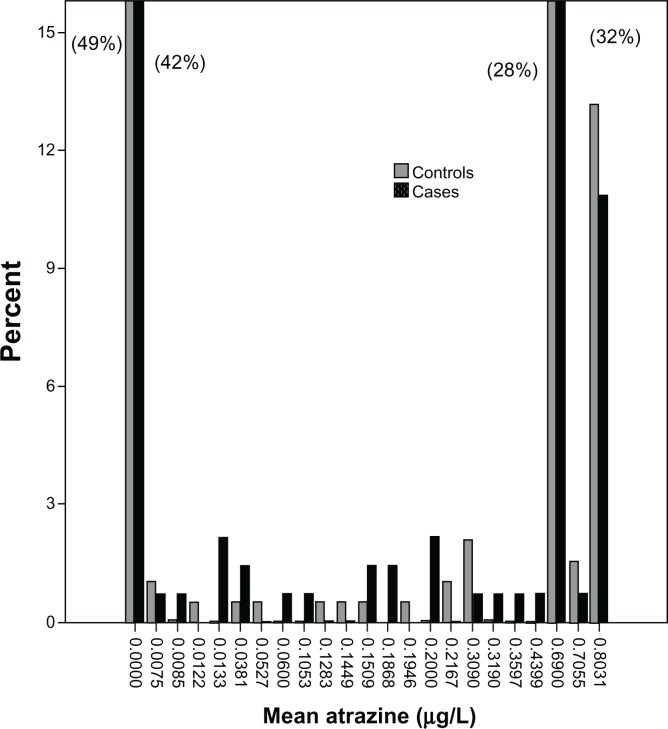
Furthermore, farmers may live in areas where water has higher nitrate and atrazine concentrations and may, because of their occupation, also have other modes of pesticide exposures. Alternatively, one could assume that most farmers live in rural areas and use private wells. This study included only subjects who used public water systems and lived at one residence during the latency period (1978–1998). It is expected, however, that small town residents would have increased exposure from application due to their residence being closer to farm fields. Excluding the two largest cities represented in this study (Lincoln and Omaha) produced no change in our results. Water quality may be a surrogate for some other factor in the environment such as exposure to farm animals,55 another drinking water contaminant such as arsenic, uranium or another agrichemical, or exposure to nitrosamines produced from drinking water disinfection treatments.56 The data were not sufficient to evaluate NHL risk associated with alachlor combined with nitrate (3 cases, 3 controls) or simazine combined with nitrate (1 case, 3 controls). Finally, because an association was observed only after dichotomizing the nitrate and atrazine data, it is possible that the positive finding is due to chance. The nitrate-N data have a positively skewed distribution and mean exposure concentrations range from 0.00 mg/L to 8.08 mg/L with a median concentration of 0.94 mg/L (Fig. 1). The atrazine data have a bimodal distribution and are zero-inflated, with mean exposure concentrations ranging from 0.00 μg/L to 0.80 μg/L and a median exposure concentration of 0.08 μg/L (Fig. 2). The second highest quartile of atrazine exposure showed an association between exposure and risk of NHL (OR, 4.8; CI, 1.2–19.9; P = 0.03; n = 56 cases and 64 controls) but the association was less strong for the highest atrazine exposure quartile and NHL risk (OR, 3.3; CI, 1.0–11.1; P = 0.06; n = 16 cases and 28 controls). To evaluate the quantitative dose-response relationship regarding the interaction of atrazine and nitrate, we fit the logistic regression and found that the relationship between log odds and atrazine increased as nitrate dose increased, although not significantly (P = 0.168).
Figure 1.
Mean nitrate exposure for cases and controls.
Figure 2.
Mean atrazine exposure for cases and controls.
Confounding due to the t(14;18) translocation typically seen in NHL patients with indolent B-cell lymphoma could be a limiting factor.57 A study evaluating the occurrence of t(14;18) in cases versus controls and exposure to nitrate and atrazine in drinking water would be informative. An additional limitation is subject-specific water consumption information. We could only estimate tap water intake based on a 1989 report in which the investigators evaluated total water and tap water intake in the United States by age and gender.38 Incorporating these data into the analysis did not elicit a discrepancy with our original findings.
With just over 8% of controls exposed to nitrate and atrazine, this study has a post-hoc power of 79% to detect a true difference in risk of NHL in aggregate and 97% power to detect a difference in risk of indolent B-cell NHL between subjects exposed and subjects not exposed to nitrate and atrazine in drinking water. We recognize that dichotomization is less efficient for statistical analysis and decreases power; however, the finding of an increased risk of NHL in association with exposure to nitrate and atrazine in drinking water warrants reporting and should be confirmed in a larger study. This could be accomplished with a historical cohort study. Using water quality data from several agricultural regions, subjects would be stratified according to the occurrence of nitrate, atrazine, and the combination of nitrate and atrazine. Then incidence of NHL would be compared between the groups: high nitrate:low nitrate; nitrate + atrazine:nitrate; nitrate + atrazine:atrazine; atrazine:no atrazine. Alternatively, a case control study could be repeated with a larger number of participants to increase the power of the findings. A crucial element to epidemiology studies that evaluate cancer risk in association with environmental exposures such as drinking water contaminants is the longevity at a residence. Most cancers have latency periods of 10–20 years. Therefore, to eliminate exposure misclassification, an investigator must be able to estimate exposure retrospectively over a long time period. Finally, the best possible study would be a prospective cohort study. Subjects would be enrolled and their drinking water sampled annually for 20 years. Statistical analysis would then be conducted to evaluate if those exposed to nitrate, atrazine, or nitrate and atrazine together were more likely to develop NHL than those not exposed, controlling for other known risk factors and confounders. A cohort study would offer subject-specific water data to determine exposure rather than estimating exposure, as is the protocol for retrospective studies. Analysis could also be performed for drinking water contaminants not regulated under the SDWA, such as deethylatrazine and deisopropylatrazine, two degradation products of atrazine which are also nitrosatable. Although prospective cohort studies elicit the most reliable information, these studies are very expensive and time-consuming. Confirmation of our results in a larger study would increase our confidence in generalizing the results to people chronically exposed to these two drinking water contaminants.
Conclusion
Our findings illustrate the potential significance of evaluating mixtures of compounds for toxicity. To our knowledge, this study is the first to evaluate NHL risk associated with exposure to both nitrate- and atrazine-contaminated drinking water. Our findings suggest that exposure to drinking water containing nitrate is associated with a nearly three-fold increase in risk for developing NHL if atrazine is also present in the drinking water. The mechanism by which nitrosamines form and are metabolized makes it biologically plausible that simultaneous exposure to nitrate and atrazine in drinking water may increase the risk of developing NHL. Atrazine is a relatively persistent groundwater contaminant and has been detected for the past 40 years.13,37,58 Groundwater monitoring studies and exposure data suggest that simultaneous exposure to nitrate and atrazine is probably not an acute event but rather one that can occur over decades, depending on residential longevity. Two atrazine degradation products (deethylatrazine and deisopropylatrazine) are also nitrosatable and relatively persistent in groundwater; however, they were not evaluated in this study and are not routinely monitored. Deethylatrazine, the most important degradate, could easily be quantified using EPA method 525; however, quantification of deisopropylatrazine would be difficult without employing isotope dilution. If concentrations of these degradation products are included, total atrazine residues in groundwater may be two to five times that of atrazine alone.15,59 To our knowledge, studies evaluating the toxicity of nitrosated atrazine degradation products have not been conducted.
Future studies addressing nitrate in drinking water as a risk factor for NHL should evaluate both concurrent exposure to atrazine and NHL subtype. When exposed to a mixture of contaminants in drinking water, there is potential for in vivo formation of a more toxic compound. This is of particular concern when biological plausibility exists, as in the case of exposure to nitrate and secondary amines, many of which will nitrosate under conditions similar to that of the human stomach and form cancer-causing nitrosamines. The importance of evaluating mixtures when assessing risk has been underscored by the EPA, National Research Council, and the US Geological Survey.60,61
Acknowledgments
This research was made possible by the subjects participating in the original study. We thank Brian Chiu at the University of Chicago for providing the case control data and the public water supply managers for their assistance in collecting and analyzing the water data. Many thanks to Debbi-Barnes Josiah (Nebraska Department of Health and Human Services) for her review and constructive comments in the preparation of this manuscript.
Footnotes
Author Contributions
Conceived and designed the experiments: MGR, JLM, CLB, PJS, RFS. Analyzed the data: MGR, JLM, CLB, AK, JMV, KME, RFS. Wrote the first draft of the manuscript: MGR. Contributed to the writing of the manuscript: MGR, JLM, CLB, PJS, AK, JMV, KME, RFS. Agree with manuscript results and conclusions: MGR, JLM, CLB, PJS, AK, JMV, KME, RFS. Jointly developed the structure and arguments for the paper: MGR, JLM, CLB, PJS, JMV, KME, RFS. Made critical revisions and approved final version: MGR, JLM, CLB, PJS, AK, JMV, KME, RFS. All authors reviewed and approved of the final manuscript.
Funding
Partial support for this project was provided by the Center for Environmental Toxicology, University of Nebraska Medical Center, Omaha, Nebraska.
Competing Interests
JMV’s institution has received grants or has grants pending from Celgene, GSK and Genentech. Other authors disclose no competing interests.
Disclosures and Ethics
As a requirement of publication author(s) have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
Farming practices and the use of fertilizers and pesticides in the past 50 to 60 years have led to public concern that drinking water contaminated with agrichemicals may increase risk of developing cancer. This report presents the findings of a hypothesis-generating study conducted to assess the risk of non-Hodgkin lymphoma after simultaneous exposure to two agrichemicals found in some drinking waters.
References
- 1.Devesa SS, Fears T. Non-Hodgkin’s lymphoma time trends: United States and international data. Cancer Res. 1992;52(Suppl):5432S–40. [PubMed] [Google Scholar]
- 2.Department of Health and Human Services, Centers for Disease Control and Prevention United States Cancer Statistics (USCS). 1999–2008 Cancer Incidence and Mortality Data. Available at: http://www.cdc.gov/cancer/npcr/uscs.
- 3.Cantor KP, Blair A, Everett G, et al. Pesticides and other agricultural risk factors for non-Hodgkin’s lymphoma among men in Iowa and Minnesota. Cancer Res. 1992;H52:2447–55. [PubMed] [Google Scholar]
- 4.Schroeder JC, Olshan AF, Baric R, et al. Agricultural risk factors for t(14;18) subtypes of non-Hodgkin’s lymphoma. Epidemiology. 2001;12(6):701–9. doi: 10.1097/00001648-200111000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Richardson DB, Terschuren C, Hoffman W. Occupational risk factors for non-Hodgkin’s lymphoma: A population based case-control study in Northern Germany. Am J Indust Med. 2008;51:258–68. doi: 10.1002/ajim.20552. [DOI] [PubMed] [Google Scholar]
- 6.Weisenburger DD. Environmental epidemiology of non-Hodgkin’s lymphoma in eastern Nebraska. Am J Indust Med. 1990;18:303–5. doi: 10.1002/ajim.4700180310. [DOI] [PubMed] [Google Scholar]
- 7.Ward MH, Mark SD, Cantor KP, Weisenburger DD. Drinking water nitrate and the risk of non-Hodgkin’s lymphoma. Epidemiology. 1996;7:465–70. [PubMed] [Google Scholar]
- 8.Ward MH, Cerhan JR, Colt JS, Hartge P. Risk of non-Hodgkin lymphoma and nitrate and nitrite from drinking water and diet. Epidemiology. 2006;17:375–82. doi: 10.1097/01.ede.0000219675.79395.9f. [DOI] [PubMed] [Google Scholar]
- 9.Freedman DM, Cantor KP, Ward MH, Helzlsouer KJ. A case-control study of nitrate in drinking water and non-Hodgkin’s lymphoma in Minnesota. Arch Env Health. 2000;55:326–9. doi: 10.1080/00039890009604024. [DOI] [PubMed] [Google Scholar]
- 10.Weyer PH, Cerhan JR, Kross BC, et al. Municipal drinking water nitrate level and cancer risk in older women: the Iowa women’s health study. Epidemiology. 2001;11:161–9. doi: 10.1097/00001648-200105000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Zahm SH, Weisenburger DD, Cantor KP, Holmes FF, Blair A. Role of the herbicide atrazine in the development of non-Hodgkin’s lymphoma. Scand J Work Env Health. 1993;48:108–14. doi: 10.5271/sjweh.1499. [DOI] [PubMed] [Google Scholar]
- 12.De Roos AJ, Hartge P, Lubin JH, et al. Integrative assessment of multiple pesticides as risk factors for non-Hodgkin’s lymphoma among men. Occ Env Med. 2003 Sep;60(9):E11. doi: 10.1136/oem.60.9.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fritschi L, Benke G, Hughes AM, et al. Occupational exposure to pesticides and risk of non-Hodgkin’s lymphoma. Am J Epidemiology. 2005;162:849–57. doi: 10.1093/aje/kwi292. [DOI] [PubMed] [Google Scholar]
- 14.Orsi L, Delabre L, Monneraeu A, et al. Occupational exposure to pesticides and lymphoid neoplasms among men: results of a French case-control study. Occ Env Med. 2009;66:291–8. doi: 10.1136/oem.2008.040972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spalding RF, Exner ME, Snow DD, Cassada DA, Burbach ME, Monson SJ. Herbicides in ground water beneath Nebraska’s Management Systems Evaluation Area. J Env Qual. 2003;32:92–9. doi: 10.2134/jeq2003.9200. [DOI] [PubMed] [Google Scholar]
- 16.Nebraska Department of Environmental Quality Nebraska Groundwater Quality Monitoring Report. 2005–2007. Available at: http://www.deq.state.ne.us.
- 17.Exner ME, Perea-Estrada H, Spalding RF. Long-term response of ground-water nitrate concentrations to management regulations in Nebraska’s central Platte valley. Sci World J. 2010;10:286–97. doi: 10.1100/tsw.2010.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Department of Agriculture National Agrigulture Statistics Service Farm and Ranch Irrigation Survey. 2003. Volume 3, special studies. Available at: http://www.nass.usda.gov/census.
- 19.Johnson BB, Kamble ST. Pesticide Use on Major Crops in Nebraska-1982. Lincoln: Department of Agricultural Economics, University of Nebraska; 1984. [Google Scholar]
- 20.Sass JB, Colangelo JD. European Union bans atrazine, while the United States Negotiates continued use. Int J Occup Environ Health. 2006;12:260–7. doi: 10.1179/oeh.2006.12.3.260. [DOI] [PubMed] [Google Scholar]
- 21.Gillom RJ, Barbash JE, Crawford CG, et al. The Quality of Our Nation’s Waters—Pesticides in the Nation’s Streams and Ground Water. Reston, VA: Circular 1291, US Geological Survey; 2006. 1992–2001. [Google Scholar]
- 22.Gosselin D, Headrick CJ, Tremblay V, Chen X, Summerside S. Domestic well water quality in rural Nebraska: focus on nitrate-nitrogen, pesticides, and coliform bacteria. Ground Water Monitoring and Remediation. 1997;17(2):77–87. [Google Scholar]
- 23.Ward MH, deKok TM, Levallois P, et al. Workgroup report: Drinking-water nitrate and health-recent findings and research needs. Env Health Persp. 2005;113:1607–14. doi: 10.1289/ehp.8043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cova D, Nebuloni C, Arnoldi A, Bassoli A, Trevisan M, Del Re AAM. N-nitrosation of triazines in human gastric juice. J Ag Food Chem. 1996;44:2852–5. [Google Scholar]
- 25.Krull IS, Mills K, Hoffman G, Fine DH. The analysis of N-nitrosoatrazine and N-nitrosocarbaryl in whole mice. J Anal Toxicol. 1980;4:260–2. doi: 10.1093/jat/4.5.260. [DOI] [PubMed] [Google Scholar]
- 26.Pruessmann R, Stewart BW. N-nitroso carcinogens. In: Searle CE, editor. Chemical Carcinogens. Washington, DC: American Chemical Society; 1984. pp. 643–868. [Google Scholar]
- 27.Mirvish SS. Formation of N-nitroso compounds: chemistry, kinetics and in vivo occurrence. Tox and Appl Pharm. 1975;31:325–51. doi: 10.1016/0041-008x(75)90255-0. [DOI] [PubMed] [Google Scholar]
- 28.Wolfe NL, Zepp RG, Gordon JA, Fincher RC. N-nitrosamine formation from atrazine. Bull Env Con and Tox. 1976;15:342–7. doi: 10.1007/BF01812647. [DOI] [PubMed] [Google Scholar]
- 29.Loeppky RN. Nitrosamine and N-nitroso compount chemistry and biochemistry: Advances and perspectives. In: Loeppsky RN, Michejda CJ, editors. Nitrosamines and Related N-Nitroso Compounds. Washington, DC: American Chemical Society; 1994. [Google Scholar]
- 30.Brambilla G, Mattioli F, Martelli A. Genotoxic and carcinogenic effects of antipsychotics and antidepressants. Toxicology. 2009;261:77–88. doi: 10.1016/j.tox.2009.04.056. [DOI] [PubMed] [Google Scholar]
- 31.Meisner LF, Roloff BD, Belluck DA. In vitro effects of N-nitrosoatrazine on chromosome breakage. Arch Env Con and Tox. 1993;24:108–12. doi: 10.1007/BF01061097. [DOI] [PubMed] [Google Scholar]
- 32.Van Leeuwen JA, Waltner-Toews D, Abernathy T, Smit B, Shoukri M. Assocations between stomach cancer incidence and drinking water contamination with atrazine and nitrate in Ontario (Canada) agroecosystems, 1987–1991. Int J Epidemiol. 1999;28(5):836–40. doi: 10.1093/ije/28.5.836. [DOI] [PubMed] [Google Scholar]
- 33.Vose JM, Chiu BCH, Cheson BD, Dancey J, Wright J. Update on epidemiology and therapeutics for non-Hodgkin’s lymphoma. Hematology. 2002:241–62. doi: 10.1182/asheducation-2002.1.241. [DOI] [PubMed] [Google Scholar]
- 34.Chiu BC, Kolar C, Gapstur SM, Lawson TA, Anderson JR, Weisenburger DD. Association of NAT and GST polymorphisms with non-Hodgkin lymphoma: a population-based case-control study. Br J Haem. 2005;128:610–5. doi: 10.1111/j.1365-2141.2004.05358.x. [DOI] [PubMed] [Google Scholar]
- 35.Mauch PM, Armitage JO, Coiffier B, Dalla-Favera R, Harris NL. Non-Hodgkin’s Lymphomas. Philadelphia, PA: Lippincott Williams and Wilkins; 2004. [Google Scholar]
- 36.Rhoades MG. Risk of non-Hodgkin Lymphoma and Drinking Water in Nebraska:Atrazine and Nitrate. Omaha, NE: University of Nebraska Medical Center; 2010. [Google Scholar]
- 37.Spalding RF, Junk GA, Richard JJ. Water: Pesticides in ground water beneath irrigated farmland in Nebraska Aug 1978. Pestici Moni J. 1980;14:70–3. [PubMed] [Google Scholar]
- 38.National Cancer Institute. Ershow AG, Cantor KP. Total Water and Tapwaer Intake in the United States: Population Based Estimates of Quantities and Sources. May, 1989. Report prepared under NCI order #263-MD-810264. [PubMed]
- 39.Nolan BT, Stoner JD. Nutrients in groundwaters of the conterminous United States, 1992–1995. Env Sci Technol. 2000;34:1156–65. [Google Scholar]
- 40.Mirvish SS, Gannett P, Babcook DM, Williamson D, Chen SC, Weisenburger DD. N-Nitrosoatrazine: Synthesis, kinetics of formation and nuclear magnetic resonance spectra and other properties. J Agric Food Chem. 1991;39:1205–10. [Google Scholar]
- 41.Wei HR, Rhoades MG, Shea PJ. Formation, Adsorption, and Stability of N-Nitrosoatrazine in Water and Soil. In: Roberts-Kirchohoff ES, Murray MN, Garshott DM, Benvenuto MA, editors. It’s All in the Water: Studies of Materials and Conditions in Fresh and Salt Water Bodies. Washington, DC: American Chemical Society; 2011. pp. 3–19. [Google Scholar]
- 42.Kearney PC, Olifer JE, Helling CS, Isensee AR, Kontson A. Distribution, movement, persistence and metabolism of N-nitrosoatrazine in soils and a model aquatic ecosystem. J Agric Food Chem. 1977;25(5):1177–81. doi: 10.1021/jf60213a015. [DOI] [PubMed] [Google Scholar]
- 43.Lijinsky W. How nitrosamines cause cancer. New Sci. 1977;73(1036):216–7. [Google Scholar]
- 44.Mirvish SS. Role of N-nitroso compounds (NOC) and N-nitrosation in etiology of gastric, esophageal, nasopharyngeal and bladder cancer and contribution to cancer of known exposures to NOC. Cancer Lett. 1995;93:17–48. doi: 10.1016/0304-3835(95)03786-V. [DOI] [PubMed] [Google Scholar]
- 45.Lijinsky W. The significance of N-nitroso compounds as environmental carcinogens. J Env Sci and Health Part C Env Carc Rev. 1986:1–45. [Google Scholar]
- 46.Graves RJ, Swann PF. Clearance of N-nitrosodimethylamine and N-nitrosodiethylamine by the perfused rat liver. Relationship to the Km and Vmax for nitrosamine metabolism. Biochem Pharm. 1993;45:983–9. doi: 10.1016/0006-2952(93)90240-w. [DOI] [PubMed] [Google Scholar]
- 47.Eisenbrand G, Janzowski C. Potential mechanism of action of nitrosamines with hydroxyl, oxo or carboxy groups. In: Michejda CJ, Loeppky RN, editors. Nitrosamines and Related N-nitroso Compounds. American Chemical Society; 1994. pp. 179–94. [Google Scholar]
- 48.Liteplo RG, Meek ME, Windle W. United Nations Environment Programme, International Labour Organization, and the World Health Organization. N-nitrosodimethylamine Concise International chemical Assessment Document 38. Available at: http://www.inchem.org/documents/cicads/cicads/cicad38.htm.
- 49.World Health Organization WHO Food Additives Series: 50. Nitrate (and Potential Endogenous Formation of N-Nitroso Compounds) Available at: http://www.inchem.org/documents/jecfa/jecmono/v50je06.htm.
- 50.World Health Organization . WHO/HSE/WSH/10.01/11 Atrazine and its Metabolism in Drinking Water. Background Document for Development of WHO Guidelines for Drinking-Water Quality. World Health Organization; 2010. http://www.who.int/water_sanitation_health/dwq/chemicals/dwq_background_20100701_en.pdf. [Google Scholar]
- 51.Gammon DW, Aldous CN, Wesley CC, Sanborn JR, Pfeifer KF. A risk assessment of atrazine use in California: Human health and ecological aspects. Pest Manag Sci. 2005;61:331–55. doi: 10.1002/ps.1000. [DOI] [PubMed] [Google Scholar]
- 52.Lubow J, Howd R. Should atrazine and related chlorotriazines be considered carcinogenic for human health risk assessment? J Environ Sci Health: Environ Carcinog Ecotoxicol Rev. 2011;29(2):99–144. doi: 10.1080/10590501.2011.577681. [DOI] [PubMed] [Google Scholar]
- 53.Freeman LEB, Rusiecki JA, Hoppin JA, et al. Atrazine and cancer incidence among pesticide applicators in the agricultural health study (1994–2007) Environ Health Perspect. 2011;119(9):1253–9. doi: 10.1289/ehp.1103561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simpkins JW, Swenberg JA, Weiss N, et al. Atrazine and breast cancer: A framework assessment of the toxicological and epidemiological evidence. Tox Sci. 2011;123(2):441–59. doi: 10.1093/toxsci/kfr176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tranah GJ, Bracci PM, Holly EA. Domestic and farm animal exposures and risk of non-Hodgkin’s lymphoma in a population based study in the San Francisco Bay area. Cancer Epidemiol, Biomarkers and Prev. 2008;7(9):2382–7. doi: 10.1158/1055-9965.EPI-08-0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhao Y, Boyd JM, Woodbeck M, et al. Formation of N-nitrosamines from eleven disinfection treatments of seven different surface waters. Env Sci Technol. 2008;42:4857–62. doi: 10.1021/es7031423. [DOI] [PubMed] [Google Scholar]
- 57.Chiu BC, Dave BJ, Ward MH, et al. Dietary factors and risk of t(14;18)-defined subgroups of NHL. Cancer Causes and Control. 2008;19:859–67. doi: 10.1007/s10552-008-9148-3. [DOI] [PubMed] [Google Scholar]
- 58.Van Maanen JMS, De Vaan MAJ, Veldstra AWF, Hendrix WPAM. Pesticides and nitrate in groundwater and rainwater in the province of Limburg in The Netherlands. Env Monit Assess. 2001;72:95–114. doi: 10.1023/a:1011963922054. [DOI] [PubMed] [Google Scholar]
- 59.Ribaudo MO, Bousahaer A. Atrazine: Environmental Characteristics and Economics of Management. 1994. Economic Research Services. Economic Report No. 699; Available at: http://usda.mannlib.cornell.edu/usda/nass/general/aer/aer699.pdf.
- 60.Toccalino PL, Norman JE, Scott JC. Chemical mixtures in untreated water from public-supply wells in the US-Occurrence, composition, and potential toxicity. Sci Total Env. 2012;431:262–70. doi: 10.1016/j.scitotenv.2012.05.044. [DOI] [PubMed] [Google Scholar]
- 61.Committee on Improving Risk Analysis Approaches Used by the US EPA, National Research Council . Science and Decisions: Advancing Risk Assessment. Washington, DC: National Acadamies Press; 2009. [Google Scholar]