Abstract
Objectives
The purposes of this study were to analyze data from the longitudinal Medical Expenditures Panel Survey (MEPS) to evaluate the impact of an aging population on secular trends in back pain and chronicity and to provide estimates of treatment costs for patients who used only ambulatory services.
Methods
Using the MEPS 2-year longitudinal data for years 2000 to 2007, we analyzed data from all adult respondents. Of the total number of MEPS respondent records analyzed (N = 71 838), we identified 12 104 respondents with back pain and further categorized 3842 as chronic cases and 8262 as nonchronic cases.
Results
Secular trends from the MEPS data indicate that the prevalence of back pain has increased by 29%, whereas chronic back pain increased by 64%. The average age among all adults with back pain increased from 45.9 to 48.2 years; the average age among adults with chronic back pain increased from 48.5 to 52.2 years. Inflation-adjusted (to 2010 dollars) biennial expenditures on ambulatory services for chronic back pain increased by 129% over the same period, from $15.6 billion in 2000 to 2001 to $35.7 billion in 2006 to 2007.
Conclusion
The prevalence of back pain, especially chronic back pain, is increasing. To the extent that the growth in chronic back pain is caused, in part, by an aging population, the growth will likely continue or accelerate. With relatively high cost per adult with chronic back pain, total expenditures associated with back pain will correspondingly accelerate under existing treatment patterns. This carries implications for prioritizing health policy, clinical practice, and research efforts to improve care outcomes, costs, and cost-effectiveness and for health workforce planning.
Key Indexing Terms: Back pain, Costs and cost analysis, Aging, Spine, Economics, Chronic disease
The “Baby Boomer Generation” is a demographic bulge in the US population considered by the US Census Bureau to encompass those individuals born during the demographic birth boom between 1946 and 1964 (Fig 1).1 A “pig in a python” metaphor aptly describes the effect of this birth cohort on society,2 as entire social infrastructures have adapted over time, first expanding and then contracting to meet the changing needs of the boomers. For example, municipal school systems were first overbuilt and then later dismantled or repurposed, to accommodate the boomers as they passed through the educational system. With boomers now approaching retirement age, the US health care system must prepare for the coming shockwave of their increasing health care needs, which will likely include a greater and more costly burden of musculoskeletal conditions such as back pain.
Fig 1.
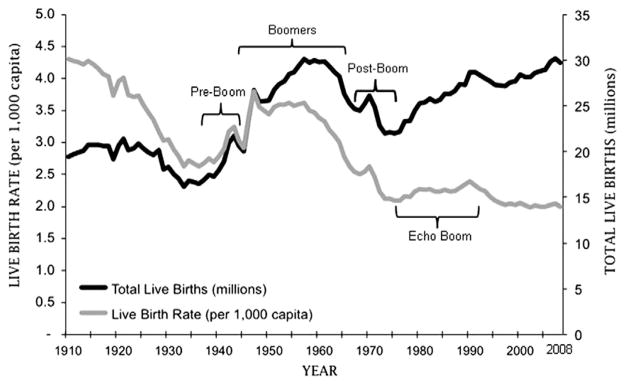
Long-term US live birth trends from 1910 to 2008. Live birth trends in 1910 to 1959 are based on adjusted values for underregistration, whereas 1960 to 2008 trends are based on US registered live births. Source of data: Population Profile of the United States.1
In the general population, back pain is extremely common and associated with considerable costs.3–5 Back pain is the second most common reason adults consult a primary care provider (second only to upper respiratory infections), 6,7 and in recent years, the prevalence and expenditures on conditions related to the spine in the United States have significantly increased.4,8 A 2006 study found an epidemic rise in the prevalence of nonspecific low back pain among Medicare beneficiaries and dramatic increases in charges.5 It has been estimated that 75% of direct health services expenditures for back pain can be attributed to only 25% of the back pain population,9 which includes many who have chronic back pain.
It is unclear to what extent the aging of the population accounts for the increased prevalence of back pain generally or chronic back pain in particular. The potential impact of aging boomers on the prevalence and chronicity of back pain threatens to strain the US health care system. It is important for policymakers, payers, and other stakeholders to understand the effects of the growing back pain population and its impending demands.
Therefore, the purpose of this study was to analyze data from the longitudinal Medical Expenditures Panel Survey (MEPS) to evaluate the impact of an aging population, in particular the aging of boomers, on secular trends in back pain. This study provides a model of the impacts of aging on back pain and chronicity and provides estimates of treatment costs for patients who used only ambulatory services.
Methods
Data Source and Sampling
The Palmer College institutional review board authorized an exemption from review for this study because it used publicly available and de-identified data from the MEPS. The MEPS is a nationally representative survey of the noninstitutionalized US population, conducted annually by the Agency for Healthcare Research and Quality. Information is gathered on health care use, expenditures, and health behaviors. The MEPS 2-year longitudinal study design resurveys respondents during each of 5 separate interview rounds throughout the 2 years. We analyzed data from all adult (18 years or older at entry into longitudinal panel) respondents to all 5 rounds of the MEPS Longitudinal Survey, for MEPS panels 5 through 11, which spanned years 2000 to 2007. The total number of respondent records analyzed was 71 838 (Table 1).
Table 1.
National estimates of US adults with back pain, 2000 to 2007
| MEPS 2-y longitudinal survey years | Total, mean, or % (SE)
|
||||||
|---|---|---|---|---|---|---|---|
| 2000–2001 | 2001–2002 | 2002–2003 | 2003–2004 | 2004–2005 | 2005–2006 | 2006–2007 | |
| MEPS panel no. a | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| Total no. of sample b | 6797 | 13 827 | 10 081 | 10 344 | 10 219 | 9964 | 10 606 |
| Projected national estimates | |||||||
| All adults, millions | 195.3 (16.8) | 199.5 (10.3) | 201.7 (10.3) | 203.5 (10.9) | 204.8 (7.0) | 208.2 (7.5) | 209.7 (5.7) |
| Percent of MEPS panel according to birth category | |||||||
| Born before 1935 (elders) | 15.2% (0.7) | 14.0% (0.5) | 13.2% (0.5) | 12.1% (0.5) | 11.3% (0.5) | 10.3% (0.4) | 9.7% (0.4) |
| Born 1935–1944 (preboomers) | 13.0% (0.6) | 13.1% (0.4) | 12.6% (0.5) | 12.4% (0.4) | 12.1% (0.5) | 11.9% (0.5) | 11.5% (0.4) |
| Born 1945–1964 (boomers) | 39.8% (0.8) | 38.9% (0.6) | 38.3% (0.7) | 38.1% (0.7) | 38.0% (0.7) | 37.0% (0.7) | 36.5% (0.6) |
| Born 1965–1975 (postboomers) | 21.2% (0.8) | 21.1% (0.5) | 21.4% (0.6) | 20.9% (0.6) | 20.4% (0.6) | 20.6% (0.6) | 20.2% (0.5) |
| Born after 1975 (younger adults) | 10.8% (0.4) | 12.9% (0.4) | 14.5% (0.5) | 16.5% (0.5) | 18.2% (0.5) | 20.2% (0.6) | 22.2% (0.7) |
| Adults with any reported back pain c | |||||||
| Total adults, millions | 30.2 (2.9) | 33.8 (2.0) | 35.4 (2.1) | 35.8 (2.1) | 38.7 (1.7) | 38.5 (1.7) | 38.9 (1.3) |
| Percent of all adults | 15.4% (0.6) | 17.0% (0.4) | 17.5% (0.5) | 17.6% (0.5) | 18.9% (0.6) | 18.5% (0.5) | 18.6% (0.5) |
| Mean age (y) | 45.9 (0.6) | 46.6 (0.4) | 46.9 (0.5) | 47.5 (0.5) | 47.4 (0.5) | 48.1 (0.5) | 48.2 (0.5) |
| Adults with chronic back pain d | |||||||
| Total adults, millions | 7.8 (0.9) | 9.2 (0.7) | 10.5 (0.8) | 10.7 (0.7) | 12.8 (0.8) | 11.8 (0.7) | 12.8 (0.7) |
| Percent of all adults | 4.0% (0.3) | 4.6% (0.2) | 5.2% (0.3) | 5.3% (0.3) | 6.3% (0.4) | 5.7% (0.3) | 6.1% (0.3) |
| Mean age (y) | 48.5 (1.0) | 51.6 (0.7) | 52.1 (0.8) | 51.6 (0.7) | 50.5 (0.8) | 52.4 (0.8) | 52.2 (0.7) |
Medical Expenditure Panel Survey respondents are resurveyed for each of 5 separate rounds throughout the 2-year longitudinal panel survey. Each round recall period ranges from 4 to 6 months, and respondents report their experiences for the entire time frame of each round.
Adults (age ≥18 years at entry into 2-year longitudinal survey) who were in scope with valid data during “all 5 rounds” of the 5-round data collection.
Medical Expenditure Panel Survey respondents with any reported back pain during any round of longitudinal panel survey.
Medical Expenditure Panel Survey respondents with reported back pain in 3 or more rounds of longitudinal survey.
Identification of Back Pain
Using the MEPS 2-year longitudinal data, we identified respondents with back pain reported in any interview round.10 In response to prompts from MEPS field interviewers, MEPS respondents describe their health problems in a narrative form, and the narratives from the MEPS field interviews are then interpreted and assigned by trained expert MEPS coders into condition diagnostic codes according to the International Classification of Diseases, Ninth Revision (ICD-9) and a Clinical Classification Category (CCC code). From the MEPS Medical Conditions data file, we identified MEPS respondents with the CCC back pain code “205” and/or with ICD-9 codes “846” or “847.” (CCC code “205” encompasses 66 ICD codes for back conditions such as spondylosis and intervertebral disc disorders but does not include ICD codes “846” and “847” for sacroiliac and back sprain/strain, which are categorized as sprain/strain under CCC code “232.”) Pooled across MEPS panels 5 through 11, we identified 12 104 adults with back pain.
Back Pain Chronicity
During the course of the MEPS 2-year longitudinal survey, respondents are resurveyed during 5 interview rounds, approximately every 4 to 6 months. During each round interview, MEPS respondents are asked to recall their experiences during the entire preceding round period. For each MEPS round, MEPS respondents are queried as to whether they were “bothered” by back pain, or had a back pain disability day (missed work or school, or a day in bed, due to back pain), or used any health services for back pain during that round. For each MEPS respondent, we classified each of the 5 MEPS round periods as either “back pain active” or “back pain inactive.” Details of the complex validated methodology used to identify the round-by-round experience of MEPS respondents with back pain have been described previously.10
For this population-based study, we identified as chronic those respondents with “active” back pain reported in 3 or more MEPS longitudinal survey rounds. The MEPS respondents who reported back pain in only 1 or 2 rounds (ie, having ≥3 “inactive” rounds without back pain) were termed nonchronic, which likely include those with acute, subacute, or sporadic episodes of back pain. Among 12 104 respondents with back pain, we categorized 3842 as chronic cases and 8262 as nonchronic cases.
Use and Costs of Services for Back Pain
For each back pain case, we identified 2-year (all 5 rounds) ambulatory service use for back pain, from 4MEPS use events data files: office-based visits, outpatient visits, emergency department visits, and prescription medication purchases. Of our total 12 104 respondents with back pain, 9792 (81%) used any health care services for their back pain and 9431 (78%) used only ambulatory, that is, services provided during visits to outpatient or office-based or emergency department settings, including all purchased medicines that were prescribed in those ambulatory encounters.
We elected to focus our cost analysis on the patients who reported using only ambulatory services during the time frame of our study. Of the 9792 MEPS respondents who used any health services to manage their back pain, most (n = 9431; 96%–97%) received only ambulatory care. The very small proportion of inpatient users in our study constitutes a distinct group that warrants separate analyses.
To adjust for the effects of inflation, expenditures on ambulatory services were converted to 2010 dollars. With inpatient care and its relatively high inflation rate excluded from our analysis, we used the professional services category of the medical care component of the Consumer Price Index for all Urban Consumers for our adjustment. Professional services increased at a compound annual rate of 3.2% between 2000 and 2010 compared with a 4.1% rate for medical care overall.
Analysis
We used SPSS version 19.0 (SPSS, Chicago, IL) to apply complex survey design methods to generate national estimates. Complex survey design methods account for the respondent’s probability of selection and sampling design methodology.
In addition to estimating back pain prevalence and chronicity among the entire adult US population, we wanted to visualize the prevalence of chronic back pain and related use of various cohorts of interest as they aged their way through the health care system. Therefore, we defined 5 distinct population-based cohorts with back pain, categorized according to year of birth: the cohorts of elders (born before 1935), preboomers (born 1935–1944), boomers (born 1945–1964), postboomers (born 1965–1975), and younger adults (born after 1975) (Table 1).
We also tested whether back pain chronicity predicts use of back pain services and tested this for the entire population and for each birth cohort.
Results
Over the period examined in this study, the total number of adults with any back pain increased by 29% (from 30.2 million in 2000–2001 to 38.9 million adults in 2006–2007), whereas the total number of adults with chronic back pain increased by 64% (from 7.8 million in 2000–2001 to 12.8 million in 2006–2007) (Table 1 and Fig 2). Over the entire 7-year period, chronic back pain accounted for more than half of the overall increase in back pain prevalence.
Fig 2.
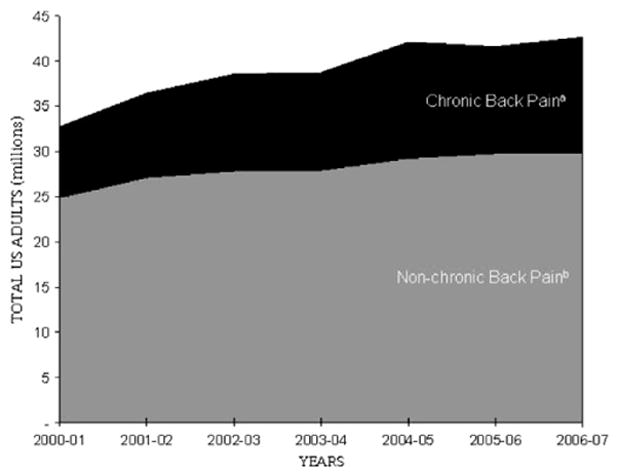
Estimated total US adults with back pain.a, Chronic back pain defined as back pain reported for 3 or more MEPS rounds during 2-year longitudinal panel survey.b, Nonchronic back pain defined as back pain reported for 1 or 2 MEPS rounds.
The mean (SD) age among all adults with back pain increased from 2000 to 2007, from 45.9 (0.6) years to 48.2 (0.5) years (Table 1). The mean (SD) age among adults with chronic back pain increased from 48.5 (1.0) years in 2000–2001 to 52.2 (0.7) years in 2006–2007.
A picture of “creeping chronicity” becomes readily apparent by mapping secular trends that demonstrate the progression of chronic back pain among aging adults with back pain (Fig 3). Most noticeably, upward of 25% of older adults with back pain (elders, preboomers, and boomers age categories) already have chronic back pain as they enter retirement age. Noteworthy also, up to 40% of back pain may eventually become chronic among oldest elders. For the 2 younger cohorts born after 1964 (postboomers and younger adults), the prevalence of chronic back pain was lower overall.
Fig 3.
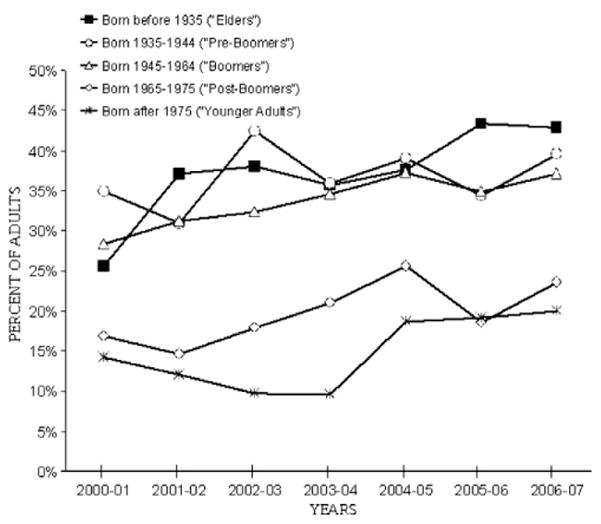
Among US adults with back pain, percentage with chronic back pain according to birth year category. Chronic back pain defined as back pain reported for 3 or more MEPS rounds during 2-year longitudinal panel survey.
Use of health care services for back pain is significantly related to back pain chronicity. Overall, 94% of patients with chronic back pain use services, whereas 75% of those with nonchronic back pain use services (odds ratio, 4.7; 95% confidence interval, 4.0–5.6). This association was significant for each of our age groups, although use of services for both chronic and nonchronic back pain did increase with age. Among our youngest cohort of younger adults, 90% of patients with chronic back pain and 71% of those with nonchronic back pain used services; among our oldest group of elder adults, 97% of patients with chronic back pain and 81% of those with nonchronic back pain used services.
Biennial expenditures (2010 dollars) for ambulatory care of back pain for those who did not receive inpatient care (96%–97% across the panels) are shown in Table 2. The number of adults in this category increased from 23.5 million in 2000 to 2001 to 30.3 million in 2006 to 2007, as a result of a growing adult population and a growing share of the adult population. With rising mean cost per patient (from $1146 to $1742), estimated biennial national expenditures increased from $26.9 billion in 2000 to 2001 to $52.8 billion in 2006 to 2007 (2010 dollars).
Table 2.
Biennial national expenditures ($2010) on ambulatory services for back pain among US adults, 2000 to 2007
| MEPS 2-year longitudinal survey years | Total, mean, median, or % (SE)
|
||||||
|---|---|---|---|---|---|---|---|
| 2000–2001 | 2001–2002 | 2002–2003 | 2003–2004 | 2004–2005 | 2005–2006 | 2006–2007 | |
| MEPS panel no.a | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| Projected national estimates | |||||||
| All adults, millionsb | 195.3 (16.8) | 199.5 (10.3) | 201.7 (10.3) | 203.5 (10.9) | 204.8 (7.0) | 208.2 (7.5) | 209.7 (5.7) |
| Adults with back pain who received care, millions | 24.4 (2.4) | 27.4 (1.6) | 29.2 (1.8) | 29.7 (1.8) | 31.4 (1.4) | 31.2 (1.4) | 31.6 (1.1) |
| Percentage of all adults | 12.5 (0.5) | 13.7 (0.4) | 14.5 (0.4) | 14.6 (0.4) | 15.3 (0.5) | 15.0 (0.5) | 15.1 (0.4) |
| Adults with back pain—no inpatient care, millions | 23.5 (2.3) | 26.5 (1.5) | 28.0 (1.7) | 28.6 (1.8) | 30.6 (1.4) | 30.3 (1.4) | 30.3 (1.1) |
| Percentage of all adults | 12.0 (0.5) | 13.3 (0.4) | 13.9 (0.4) | 14.1 (0.4) | 14.9 (0.5) | 14.6 (0.4) | 14.5 (0.4) |
| Percentage of those who received care | 96.1 (0.7) | 96.6 (0.5) | 95.9 (0.6) | 96.5 (0.5) | 97.3 (0.5) | 97.1 (0.4) | 96.0 (0.6) |
| Mean expenditure per adult with back pain ($) | 1146 (79) | 1358 (66) | 1392 (83) | 1477 (91) | 1715 (110) | 1520 (100) | 1742 (130) |
| Median expenditure per adult with back pain ($) | 406 | 431 | 438 | 478 | 550 | 531 | 499 |
| Adults with chronicc back pain, millions | 7.0 (0.8) | 8.0 (0.6) | 9.3 (0.7) | 9.4 (0.7) | 11.6 (0.7) | 10.4 (0.6) | 11.3 (0.6) |
| Percentage of all adults | 4.0 (0.3) | 4.6 (0.2) | 5.2 (0.3) | 5.3 (0.3) | 6.3 (0.4) | 5.7 (0.3) | 6.1 (0.3) |
| Mean expenditure per adult with chronic back pain ($) | 2235 (188) | 2622 (170) | 2701 (213) | 2790 (195) | 3161 (241) | 2789 (236) | 3152 (313) |
| Median expenditure per adult with chronic back pain ($) | 1121 | 1285 | 1242 | 1327 | 1535 | 1293 | 1149 |
| Total expenditures on chronic back pain, $ billions | 15.6 (1.5) | 21.0 (1.6) | 25.1 (2.5) | 26.3 (2.2) | 36.5 (3.2) | 28.9 (2.7) | 35.7 (3.6) |
| Adults with nonchronicc back pain, millions | 16.5 (1.8) | 18.5 (1.1) | 18.7 (1.2) | 19.2 (1.3) | 19.0 (0.9) | 19.9 (1.0) | 19.0 (0.8) |
| Percentage of all adults | 11.4 (0.5) | 12.3 (0.4) | 12.3 (0.4) | 12.3 (0.4) | 12.7 (0.4) | 12.9 (0.4) | 12.5 (0.4) |
| Mean expenditure per adult with nonchronic back pain ($) | 684 (62) | 810 (50) | 741 (56) | 832 (67) | 836 (47) | 861 (74) | 903 (59) |
| Median expenditure per adult with nonchronic back pain ($) | 237 | 263 | 273 | 281 | 301 | 278 | 273 |
| Total expenditures on nonchronic back pain, $ billions | 11.3 (1.5) | 15.0 (1.0) | 13.8 (1.3) | 16.0 (1.4) | 15.9 (1.0) | 17.2 (1.7) | 17.2 (1.3) |
| Total biennial expenditures on back pain, $ billions | 26.9 (2.4) | 36.0 (2.2) | 39.0 (2.8) | 42.3 (2.9) | 52.4 (3.7) | 46.1 (3.5) | 52.8 (4.2) |
Medical Expenditure Panel Survey respondents are resurveyed for each of 5 separate rounds throughout the 2-year longitudinal panel survey. Each round recall period ranges from 4 to 6 months, and respondents report their experiences for the entire time frame of each round.
Data reported for adults (age ≥18 years at entry into 2-year longitudinal survey) who were inscope with valid data during all 5 rounds of the 5-round data collection.
Chronic defined as MEPS respondents with reported back pain in 3 or more rounds of longitudinal survey; nonchronic defined as MEPS respondents with reported back pain in only 1 or 2 rounds.
Separate analyses of the chronic and nonchronic categories reveal dramatic effects of the growing chronicity described earlier. Not only has the chronic population increased much more rapidly than the nonchronic population, but the mean biennial cost per patient with chronic back pain is substantially higher (eg, $3152 for chronic vs $903 for nonchronic in 2006–2007). Thus, the estimated national biennial costs for patients with chronic back pain are substantially higher than costs for patients with nonchronic back pain, despite the latter being the larger population. In 2006 to 2007, the national costs for patients with chronic back pain were $35.7 billion compared with $17.2 billion for patients with nonchronic back pain (Fig 4).
Fig 4.
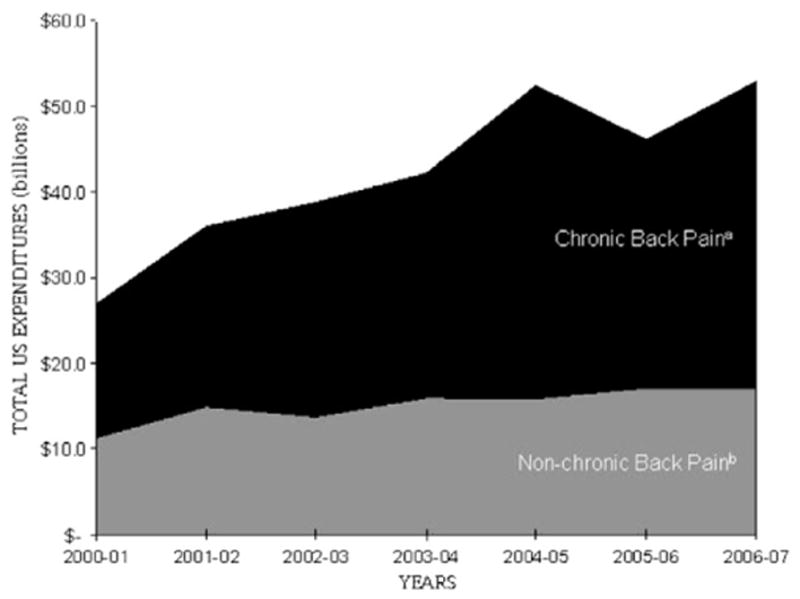
Estimated total US inflation-adjusted expenditures ($2010) on back pain.a, Chronic back pain defined as back pain reported for 3 or more MEPS rounds during 2-year longitudinal panel survey.b, Nonchronic back pain defined as back pain reported for 1 or 2 MEPS rounds.
The distribution of expenditures on health care, in general, is highly skewed, and our estimates are consistent with this pattern. For both patients with chronic and patients with nonchronic back pain, mean costs (eg, $3152 and $903, respectively, for years 2006–2007) are substantially higher than median costs ($1149 and $273, respectively). Table 3 contains additional information on the 2006 to 2007 expenditure distributions for both patients with chronic and patients with nonchronic back pain, as well as for several age groups among the former.
Table 3.
Biennial expenditures ($2010) on ambulatory services for back pain in 2006 to 2007 (MEPS panel 11), by birth category
| Total or percent (SE)
|
||||
|---|---|---|---|---|
| Population, millions (SE) | Expenditure range ($) for decile group | Expenditures, $ millions (SE) | Percent of expenditures | |
| All adults with nonchronic back pain a | 19.0 (0.7) | 17 168 (1.3) | 100.0 | |
| Top decile | 2101–18 195 | 9788 (949) | 57.0 | |
| Next decile | 1047–2100 | 3060 (187) | 17.8 | |
| Next 30% | 273–1046 | 3322 (215) | 19.4 | |
| Lowest 50% | 0–272 | 997 (55) | 5.8 | |
| All adults with chronic back pain b | 11.3 (0.5) | 35 675 (3.6) | 100.0 | |
| Top decile | 6501–67 238 | 20 146 (3092) | 56.5 | |
| Next decile | 3421–6500 | 5641 (421) | 15.8 | |
| Next 30% | 1149–3420 | 7080 (574) | 19.8 | |
| Lowest 50% | 0–1148 | 2807 (238) | 7.9 | |
| According to birth category | ||||
| Chronic preboomers (1935–1944) b | 1.8 (0.2) | 5794 (774) | 100.0 | |
| Top decile | 6676–21 402 | 3072 (786) | 53.0 | |
| Next decile | 4001–6675 | 1116 (120) | 19.3 | |
| Next 30% | 1271–4000 | 1175 (149) | 20.3 | |
| Lowest 50% | 0–1270 | 432 (1) | 7.5 | |
| Chronic boomers (1945–1964) b | 5.3 (0.4) | 18 188 (2681) | 100.0 | |
| Top decile | 7201–67 238 | 10 412 (2691) | 57.2 | |
| Next decile | 3601–7200 | 2914 (546) | 16.0 | |
| Next 30% | 1171–3600 | 3484 (137) | 19.2 | |
| Lowest 50% | 0–1170 | 1378 (61) | 7.6 | |
| Chronic postboomers (1965–1975) b | 1.5 (0.2) | 4788 (210) | 100.0 | |
| Top decile | 6301–45 220 | 2850 (138) | 59.5 | |
| Next decile | 3401–6300 | 502 (94) | 10.5 | |
| Next 30% | 1276–3400 | 1022 (59) | 21.3 | |
| Lowest 50% | 0–1275 | 415 (29) | 8.7 | |
Nonchronic back pain defined as back pain reported for 1 or 2 MEPS rounds.
Chronic back pain defined as back pain reported for 3 or more MEPS rounds during the 2-year longitudinal panel survey.
The top decile among users with chronic back pain accounts for 57% of costs, and the top quintile accounts for 72%. The corresponding values for the nonchronic population are similar, 57% and 75%, respectively. Table 3 also shows the corresponding values for the 3 dominant birth cohorts: boomers (who account for 51% of total chronic costs), preboomers (the second highest spending group with 16% of total chronic costs), and postboomers (who will begin entering retirement [age 65 years] in the year 2030 and who already account for 13% of the cost).
Discussion
Our study found that overall, the prevalence of back pain has increased by nearly 30% in recent years, of which the proportion of adults with chronic back pain has increased significantly. Our results corroborate previous reports that demonstrated the increasing prevalence of back pain4,8 and increasing chronicity of back pain.11 We estimate that the total number of adults in the United States with chronic back pain increased by 64%, with a mean rate of increase of 8.3% per year. If the current rate of growth continues, we estimate that there will be nearly 22 million US adults with chronic back pain by 2020. When we examined back pain among adults by birth year category, we found that these increases are largely driven by our aging population. Boomers represent only the peak of a surge of higher birth rates that began around 1935 and tapered off around 1970. Considering the potential effect of other trends such as the “Echo Boom” (Fig 1) and increasing life expectancy, it is likely that the prevalence of chronic back pain may rise even higher.
Our study indicates that both age and chronicity help to explain and predict the use of health services for back pain. The relationship between aging and the prevalence of back pain is not well understood.12 The belief that back pain prevalence tends to decrease after age 55 years was dispelled, in part, by a 2006 systematic review that found a preponderance of evidence for increased prevalence of severe back pain with increasing age.13 Our findings suggest that age is associated not only with back pain severity but also with back pain chronicity.
Back pain in the United States is a costly burden: from 1997 to 2005, the inflation-adjusted expenditures on health services for spine problems increased by 65%.4 Cost estimates found in the literature vary, but the general consensus is that approximately $90 billion is spent on back pain diagnosis and management and $10 to $20 billion is attributed to consequent economic losses in productivity.3,4 Chronic back pain accounts for most expenditures on health services for back pain.14
Our work confirms and extends these findings. In particular, our study is the first one to develop longitudinal national expenditure estimates among the 96% to 97% (Table 2) of patients who use only ambulatory care for back pain. For this group, total biennial expenditures in inflation-adjusted dollars nearly doubled to $52.8 billion in 2006 to 2007 from $26.9 billion in 2000 to 2001. Nearly 68% of the total expenditures in 2006 to 2007 were associated with chronic back pain, although those with chronic back pain represented just 33% of the entire adult population with back pain. Among adults with chronic back pain, just 10% accounted for 57% of the total expenditures on ambulatory services.
Implications
Although this study shows that the prevalence of back pain is increasing, the rapid increase in the prevalence of chronic back pain is of the greatest concern. To the extent that this growth in chronic back pain is due partly to an aging population, the growth will likely continue to accelerate. With relatively high cost per adult with chronic back pain, total expenditures associated with back pain will correspondingly accelerate under existing treatment patterns. This carries implications for prioritizing health policy, practice, and research efforts to improve care outcomes, costs, and cost-effectiveness and for health workforce planning.
Patient-Centered Outcomes and the Chronic Care Model
Recognizing that a “curative” acute care model fails to serve the needs of many patients with back pain who will never fully recover, a chronic care model for management of back pain would emphasize better coordination of care that focuses on prevention, education, self-care, and functional improvement.15 Based on the chronic care model, Dobscha et al 16 tested a collaborative care intervention for patients with musculoskeletal pain (back, neck, arthritic, or joint pain) in a Department of Veterans Affairs primary care setting. 16 The multidisciplinary approach resulted in significant improvements in pain disability and pain intensity, as well as improvement in depression severity among the patients with depression. Similarly, Townsend et al17 found that even patients on chronic opioid therapy for longstanding chronic back, neck, or other pain (averaging 9 years in duration) can experience significant and sustained improvement in pain severity and functioning by participating in a multidisciplinary rehabilitation program that incorporates opioid withdrawal.17
Such recent reports lend further support to recommendations that multidisciplinary approaches offer particular benefits in the physical and mental health of chronic back patients, such as improved functioning, quality of life, medication use, pain and pain behavior, or quality of sleep.18 Current clinical guidelines for management of low back pain issued jointly by the American College of Physicians and the American Pain Society recommend numerous therapeutic approaches including spinal manipulation, exercise therapy, acupuncture, massage therapy, yoga, cognitive-behavioral therapy, and progressive relaxation. 19 Overall care coordination across disciplines could be improved though collaborative development of multidisciplinary guidelines to identify and encourage best practices in current chronic pain management and by supporting further efforts to discern best options for delivering therapeutically efficacious and cost-effective care to specific subgroups of patients. 20
Costs and Cost-Effectiveness
Inflation-adjusted biennial expenditures on ambulatory services for chronic back pain increased by 129% over the study period, from $15.6 billion in 2000 to 2001 to $35.7 billion in 2006 to 2007. The increasing chronicity that we have identified suggests that this figure will continue to grow rapidly under current practice standards. Our data also indicate that the top quintile of patients account for more than 70% of expenditures.
Given that a relatively small group of patients with chronic back pain account for the overwhelming share of expenditures, future research efforts need to identify and target these high-cost drivers to determine which interventions, including collaborative multidisciplinary programs, may prove most cost-effective for which subgroups of these patients.
Initial evaluations of multidisciplinary pain programs suggested the potential for considerable cost reductions. Gatchel and Okifuji20 estimated a lifetime savings of more than $400 000 per patient with chronic back pain relative to conventional treatment. However, their 68% annual savings rate was based on cost values derived from a small sample of patients treated at a single pain center in the 1980s.21 A recent review of the cost-effectiveness literature provides a more realistic assessment of the cost implications of back pain treatments endorsed by the American College of Surgeons and American Pain Society.22 With other well-defined inclusion criteria, the review process produced only 15 cost-effectiveness studies of therapeutic approaches such as interdisciplinary rehabilitation, exercise, spinal manipulation, or cognitive-behavioral therapy.
These 15 studies indicated the cost-effectiveness of various treatment options, as well as coordinated provision of multidisciplinary care for chronic back pain, using the UK’s National Institute for Health and Clinical Excellence criterion of £20 000 to £30 000 (about $32 000–$48 000 at March 2012 exchange rates) per quality-adjusted life-year. However, the estimates vary widely across studies, and several went well beyond the National Institute for Health and Clinical Excellence threshold.
It is also important to recognize that although the potential exists for cost savings, wider adoption of more effective collaborative interventions may not necessarily reduce total national costs. When new treatments dominate existing treatments, by providing better outcomes at lower cost, the cost per patient will diminish, but total costs may increase or decrease depending on the number of previously untreated (or minimally treated) patients who are given the new therapy. When the new approach improves outcomes at an increased cost per patient, total costs will increase.
An evaluation of a collaborative model for veterans with chronic neuromusculoskeletal pain, treated at 5 clinics associated with a Veterans Affairs medical center, provides a recent example. It reported an average of 16 additional pain disability–free days (PDFDs) over a 12-month follow-up period, at an adjusted incremental cost of $354 per PDFD. 23 The collaborative approach provided more PDFDs than usual care, but at a substantially higher cost. Thus, wider adoption of this approach would raise total costs. To keep total costs in check, further research is needed to identify subgroups of patients for whom the collaborative approach is more cost-effective, as well as to track cost implications of better coordinated care for chronic back pain over the longer time frame.
The effect of an aging population on both the prevalence and the chronicity of back pain will likely strain an already stretched health care system. Comprehensive, early intervention programs are initially expensive. With most nonelderly US population insured through managed care organizations, high disenrollment rates among managed care organizations can deter significant upfront investments even when these investments are highly cost-effective over the long run.24 Thus, health care policymakers, payers, and other stakeholders need to develop innovative strategies for managing the growing needs of the population with chronic back pain.
There is increasing recognition that the United States needs to bend the cost curve without sacrificing high quality health care and that the historic rates of expenditure increases are unsustainable, especially for the Medicare and Medicaid populations. The logical strategy is to identify and hone in on the delivery of high-value care.25 There is reasonable evidence that some interventions for chronic back pain improve patient outcomes relative to traditional care and that meaningful improvements in care coordination will prove to be cost-effective. Such a concerted effort may lead to cost reductions, measured over the longer term if not in the near term, for some patient subgroups, even as their outcomes improve. Even if cost reductions are not realized, there will be societal gains through the improved resource allocation associated with wider adoption of cost-effective treatments.
Workforce Planning
Even as demand for back pain care is growing, the availability of primary care medical physicians (often the first line in back pain care) varies widely across the United States,26 with 65 million US residents living in primary care shortage areas.27 Meeting the growing demand for back pain care will require involvement of the full spectrum of the health care workforce to strengthen capacity for both primary and specialty care, as noted by the Council on Graduate Medical Education and the Institute of Medicine. The Council on Graduate Medical Education recommends increasing the numbers of nonphysician providers practicing in coordinated, integrated practice in primary care teams,28 and the Institute of Medicine recommends establishing a multidisciplinary National Geriatric Service Core to provide for the growing demand for comprehensive primary and specialty care of older adults.29
Limitations
Our study only investigated back pain trends among noninstitutionalized US adults 18 years or older. Trends may differ among children or among those in the military, and although we found a high rate of chronic back pain among the noninstitutionalized elderly population, we do not know how this compares with elderly residents of nursing homes. Also, because MEPS data on health care use and expenditures are derived from interviews, self-reporting errors may occur. However, MEPS attempts to reduce self-reporting error by verifying response data with the respondent’s health care providers and insurers.
We observed what appeared to be an anomaly in our MEPS back pain data, most evident in the irregularity of back pain expenditures trended across MEPS panels 9 and 10 (see Table 2 and Fig 4). However, MEPS documentation cautions that the inherent skewness of the underlying expenditure distributions can produce substantial year-to-year variations in means and totals, especially for smaller population subgroups, and MEPS recommends that a more complete picture of trends is better projected over longer periods rather than short periods from 1 year to the next.30
Our study indicates that a relatively small group of patients with chronic back pain account for the overwhelming share of expenditures. Therefore, future research should be directed at identifying high-cost drivers and the factors associated with their higher costs. Further research should also be directed toward discerning best options for delivering therapeutically efficacious and cost-effective care, toward better identifying subgroups of patients for whom the collaborative approach may be more cost-effective in both the short term and the longer term and improving care coordination across providers and settings.31,32
Conclusion
The prevalence of back pain is increasing, with chronic back pain showing the most rapid increase. An aging population likely contributes to the growing prevalence of chronic back pain, and increasing demand for back pain services will necessitate appropriate health workforce planning. Given that existing treatment patterns also contribute to driving concomitant growth in expenditures associated with back pain, priority should be given efforts to improve outcomes and the cost-effectiveness of care.
Practical Applications.
Trends show that the prevalence of back pain has increased by 29% and chronic back pain has increased 64%.
The average age among all adults with back pain increased from 45.9 to 48.2 years.
Inflation-adjusted ($2010) biennial expenditures on ambulatory services for chronic back pain increased by 129%, from $15.6 billion in 2000 to 2001 to $35.7 billion in 2006 to 2007.
Acknowledgments
Funding Sources
Monica Smith was supported in this work by National Institutes of Health (NIH) grant number 5K01AT002391. Matthew Davis was supported by NIH grant number 5K01AT006162. James Whedon was supported by NIH grant number 5K01AT005092. The contents of this manuscript are solely the responsibility of the author(s) and do not necessarily represent the official views of the National Center for Complementary and Alternative Medicine or the NIH.
Footnotes
Potential Conflicts of Interest
Miron Stano contributed expertise in health economics and econometrics to this research involving analyses of MEPS data. As an economist, Dr Stano has served as an expert witness in antitrust cases within the health care sector. Dr Stano reports no conflict between his service as an expert witness and his work on this research of MEPS data.
References
- 1.Population Profile of the United States. U.S. Department of Commerce; 2010. [Accessed January 25, 2011.]. Available at: http://www.census.gov/population/www/pop-profile/natproj.html. [Google Scholar]
- 2.Jones L. Great Expectations: America and the Baby Boom Generation. New York: Coward, McCann and Geoghegan; 1980. [Google Scholar]
- 3.Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299:656–64. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 5.Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med. 2006;7:143–50. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 6.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 7.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine. 1995;20:11–9. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Martin BI, Turner JA, Mirza SK, et al. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997–2006. Spine. 2009;34:2077–84. doi: 10.1097/BRS.0b013e3181b1fad1. [DOI] [PubMed] [Google Scholar]
- 9.Luo X, Pietrobon R, Sun SX, et al. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2004;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 10.Smith M. Identifying episodes of back pain using Medical Expenditures Panel Survey data: patient experience, use of services, and chronicity. J Manipulative Physiol Ther. 2010;33:562–75. doi: 10.1016/j.jmpt.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med. 2009;169:251–8. doi: 10.1001/archinternmed.2008.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24:1813–9. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 13.Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing. 2006;35:229–34. doi: 10.1093/ageing/afj055. [DOI] [PubMed] [Google Scholar]
- 14.Becker A, Held H, Redaelli M, et al. Low back pain in primary care. Spine. 2010;35:1714–20. doi: 10.1097/brs.0b013e3181cd656f. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22:62–8. doi: 10.3122/jabfm.2009.01.080102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dobscha SK, Corson K, Perrin NA, et al. Collaborative care for chronic pain: a cluster randomized trial. JAMA. 2009;301:1242–52. doi: 10.1001/jama.2009.377. [DOI] [PubMed] [Google Scholar]
- 17.Townsend CO, Kerkvliet JL, Bruce BK, et al. A longitudinal study of the efficacy of a comprehensive pain rehabilitation program with opioid withdrawal: comparison of treatment outcomes based on opioid use status at admission. Pain. 2008;140:177–89. doi: 10.1016/j.pain.2008.08.005. http://dx.doi.org/10.1016/j.pain.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 18.Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology. 2008;47:670–8. doi: 10.1093/rheumatology/ken021. http://dx.doi.org/10.1093/rheumatology/ken021. [DOI] [PubMed] [Google Scholar]
- 19.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 20.Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain. 2006;7:779–93. doi: 10.1016/j.jpain.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Simmons JW, Avant WS, Demski J, Parisher D. Determining successful pain clinic treatment through validation of cost effectiveness. Spine. 1988;13:342–4. doi: 10.1097/00007632-198803000-00020. [DOI] [PubMed] [Google Scholar]
- 22.Lin C-WC, Haas M, Maher CG, Machado LAC, van Tulder MW. Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J. 2011;20:1024–38. doi: 10.1007/s00586-010-1676-3. http://dx.doi.org/10.1007/s00586-010-1676-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dickinson KC, Sharma R, Duckart JP, et al. VA healthcare costs of a collaborative intervention for chronic pain in primary care. Med Care. 2010;48:38–44. doi: 10.1097/MLR.0b013e3181bd49e2. [DOI] [PubMed] [Google Scholar]
- 24.Goodman AC, Stano M. HMOs and health expenditures: a local public goods perspective. Public Finance Rev. 2000;28:247–69. [Google Scholar]
- 25.Owens DK, Qaseem A, Chou R, et al. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011;154:174–80. doi: 10.7326/0003-4819-154-3-201102010-00007. [DOI] [PubMed] [Google Scholar]
- 26.Chang CH, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. 2011;305:2096–104. doi: 10.1001/jama.2011.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood) 2010;29:799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 28.Council on Graduate Medical Education. 20th Report: Advancing Primary Care. 2010 Dec; Available at: http://www.aafp.org/online/etc/medialib/aafp_org/documents/press/2011-match-media-kit/cogme-advancing-primary-care.Par.0001.File.tmp/COGME-20threport-2011-Exec-Summ.pdf.
- 29.Rowe J. Statement before the Special Committee on Aging. U. S. Senate: Institute of Medicine; 2008. [Google Scholar]
- 30.MEPS documentation HC-085A: 2004 Prescribed Medicines. Agency for Healthcare Research and Quality; Oct, 2006. Available at: http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h85a/h85adoc.pdf. [Google Scholar]
- 31.Weigel PA, Hockenberry JM, Bentler SE, Kaskie B, Wolinsky FD. Chiropractic episodes and the co-occurrence of chiropractic and health services use among older Medicare beneficiaries. J Manipulative Physiol Ther. 2012;35:168–75. doi: 10.1016/j.jmpt.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith M. Usual source of care for adults with and without back pain: Medical Expenditures Panel Survey data pooled for years 2000 to 2006. J Manipulative Physiol Ther. 2011;34:356–61. doi: 10.1016/j.jmpt.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


