Abstract
Introduction
The incidence of contrast-induced nephropathy (CIN) ranges between 10% and 50% among high-risk patients. Whether medications that affect rennin-angiotensin-aldosterone system (RAAS) have any impact on the development of CIN remains uncertain.
Materials and Methods
We performed a retrospective study of patients with CKD stages 3 and 4 who were either on or off RAAS blockade therapy at the time of coronary angiography. Development of CIN was defined by a 25% increase of serum creatinine from baseline or an increase in serum creatinine by 0.5 mg/dL from baseline. Serum creatinine values were recorded before contrast exposure and for 5 days after coronary angiography.
Results
A total of 178 patients with CKD who had coronary angiography during the study period were included, of whom 62 (35%) were on ACE inhibitors, 12 (7%) were on ARBs, and 1 (1%) was on combination of ACE inhibitors and ARBs. The estimated glomerular filtration rate was 44.0 ± 11.5 mL/min. The odds ratio of acute kidney failure on day 5 was 0.73 (95% confidence interval, 0.31 to 1.69) for the ACE inhibitors and 0.46 (95% confidence interval, 0.06 to 3.70) for ARBs. Multivariable analysis revealed the findings to be independent of demographic variables, comorbidities, type of contrast medium, and the prophylactic strategies.
Conclusions
Patients on RAAS blockade therapy before contrast exposure did not have an increased incidence of CIN. There was also no increased incidence of CIN with ACE inhibitors or ARBs in the subgroups at higher risk, such as those with diabetes mellitus.
Keywords: contrast media, cariac angiography, angiotensin-converting enzyme inhibitors, chronic kidney disease, acute kidney injury
INTRODUCTION
Contrast-induced nephropathy (CIN) is considered the 3rd leading cause of iatrogenic acute kidney injury in high-risk patients undergoing radiographic procedures.1 It is associated with substantial in-hospital morbidity and mortality and usually develops within 48 hours of contrast administration.2 Contrast-induced nephropathy is diagnosed by an elevation of serum creatinine by a proportionate 25% to 50% rise from the baseline and in the absence of other explanations.3 Other criteria used to define CIN are based on creatinine clearance, glomerular filtration rate (GFR), and a fixed rise in serum creatinine of approximately 0.5 mg/dL to 1 mg/dL above baseline.4–7 The precise mechanism by which contrast agents cause kidney failure is not fully understood. The postulated pathogeneses of CIN include direct tubular injury, tubular obstruction and dysfunction and renal vasomotor constriction, resulting in medullary hypoxemia. The reported incidence of CIN has varied widely in the medical literature. Numerous studies have reported an estimated incidence of CIN, ranging from as low as 2% to as high as 50%.4–7 This variation is generally based on the presence or absence of risk factors for development of CIN. Some identified risk factors include preexisting chronic kidney disease (CKD), diabetic nephropathy, true or relative hypovolemia, percutaneous coronary interventions, concomitant nephrotoxic exposure, and osmolality, volume and tonicity of radiocontrast media.8–13 A study by Pakfetrat and colleagues using multiple logistic regression analysis showed diabetes mellitus to be the strongest predictor for at risk of contrast-related acute kidney injury, followed by hypercholesterolemia, and an estimated glomerular filtration rate lower than 90 mL/min/1.73 m2.14
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) have been associated with a decline in GFR, primarily mediated through the reduced effects of angiotensin II-induced increase in resistance at the efferent (postglomerular) arteriole. By blocking the response of angiotensin II, the efferent arteriole relaxes, which lowers intraglomerular pressure and reduces the GFR.15 This reduction in GFR can be severe in certain patients such as those with bilateral renal artery stenosis, heart failure, diabetes, vascular disease or CKD. A significant drop in GFR can also occur in those who already have reduced intrarenal perfusion pressure such as acute volume loss. This retrospective study aims to investigate the possible impact of use of the rennin-angiotensin-aldosterone system (RAAS) medications (ACE inhibitors and ARBs) on the incidence of CIN in patients with mild-to-moderate CKD who received coronary angiography.
MATERIALS AND METHODS
Study Protocol
The protocol was reviewed and approved by the Institutional Review Board. For this retrospective cross-sectional study, data was obtained by medical chart review. Inclusion criteria were as follows: age greater than 18, contrast medium exposure during a coronary angiography, CKD stages 3 or 4 (estimated GFR between 15 mL/min to 59 mL/min) as determined by the Modification of Diet in Renal Disease (MDRD) equation, a baseline creatinine on the day of contrast exposure and for 5 days following contrast administration. Data from patients on any form of renal replacement therapy were excluded from the study. Information regarding diabetes mellitus, congestive heart failure, peripheral vascular disease, prophylactic medications received, dose and type of intravenous contrast medium, acute myocardial infarction, unstable angina, hypotension (systolic blood pressure < 80 mm Hg), and body mass index was gathered. Serum creatinine values were recorded before contrast exposure and for 5 days after coronary angiography. All creatinine values were measured at one central laboratory by dry slide rate enzymatic methodology. The primary endpoint was development of CIN, which was defined by 25% increase of serum creatinine from baseline or an increase in serum creatinine by 0.5 mg/dL from baseline.
Statistical Analysis
For the calculation of the sample size, we assumed an incidence of CIN of 20% in the control group and 40% in the group on RAAS blockade. The inclusion of 39 patients in the RAAS group allowed for a two-sided significance level of 5% and 80% power, assuming a normal distribution. The odds ratio of acute kidney failure (AKF) and associated 95% confidence intervals (CIs) were calculated for the ACE inhibitor and ARB groups. Multivariable analysis was performed to determine any significant covariates that could affect the incidence of CIN in these groups. The variable included in the multivariable model consisted of age, ethnicity, comorbidities, type and volume of contrast medium, and prophylactic strategies.
RESULTS
Between January 1, 2007 and December 31, 2008, a total of 398 patients with CKD Stage 3 or 4 underwent coronary angiography. Of these, 220 were excluded due to lack of sufficient follow-up data, resulting in inclusion of 178, of whom 35% were on ACE inhibitors and 7% were on ARBs. Review of the electronic medical records confirmed the diagnosis of CIN by the definition noted above. Characteristics of the patients at baseline are shown in Table 1. The mean age was 71.3 ± 10.7 years and the mean estimated GFR was 44 ± 11.5 mL/min. There were no significant differences in the baseline characteristics of groups on RAAS blockade agents and the control group (Table 2).
Table 1.
Characteristics of Patients Included in the Study*
| Characteristic | Number (%) |
|---|---|
| Female | 68 (38) |
| Caucasian | 166 (93) |
| Comorbidities | |
| Diabetes mellitus | 108 (61) |
| Hypertension | 112 (62) |
| Coronary artery disease | 118 (66) |
| Contrast medium | |
| Iohexol | 112 (63) |
| Iodixinol | 63 (35) |
| Combination | 4 (2) |
| RAAS blockade agent | |
| ACE inhibitor | 62 (35) |
| ARB | 11 (7) |
| Combination | 1 (1) |
| Prophylactic strategies | |
| Bicarbonate | 5 (3) |
| Normal saline | 144 (81) |
| N-acteylcysteine | 51 (29) |
RAAS indicates rennin-angiotensin-aldosterone system; ACE, angiotensin-converting enzyme; and ARB, angiotensin receptor blocker.
Table 2.
Baseline Characteristics of the Renin-Angiotensin-Aldosterone (RAAS) Blockade and the Control Groups
| Characteristic | RAAS Group | Control Group | P |
|---|---|---|---|
| Age, y | 70.2 ± 11.0 | 72.1 ± 10.5 | .13 |
|
| |||
| Female | 25 (33.8) | 43 (41.4) | .39 |
|
| |||
| Caucasian | 68 (91.9) | 98 (94.2) | .76 |
|
| |||
| Comorbidities | |||
| Diabetes mellitus | 40 (54.1) | 68 (65.4) | .17 |
|
| |||
| Hypertension | 44 (59.5) | 68 (65.4) | .52 |
|
| |||
| Coronary artery disease | 52 (70.3) | 66 (63.5) | .43 |
|
| |||
| Contrast medium | |||
| Iohexol | 50 (67.6) | 62 (59.6) | .36 |
|
| |||
| Iodixinol | 21 (28.4) | 42 (40.4) | .14 |
|
| |||
| Combination | 2 (2.7) | 2 (1.9) | .87 |
|
| |||
| Volume of contrast medium, mL | 139 ± 78 | 128 ± 77 | .07 |
|
| |||
| Prophylactic strategies | |||
| Bicarbonate | 2 (2.7) | 3 (2.9) | .70 |
|
| |||
| Normal saline | 60 (81.1) | 84 (80.8) | .89 |
|
| |||
| N-acteylcysteine | 16 (21.6) | 35 (33.7) | .11 |
|
| |||
| Volume of normal saline, mL | 531 ± 543 | 524 ± 553 | .94 |
On day 2, 13% of patients had experienced AKF. The peak incidence of acute kidney failure was on day 3 at 19%. Figure 1 illustrates the percentage of patients with AKF relative to days after contrast exposure. The odds ratio of ARF on day 5 was 0.73 (95% CI, 0.31 to 1.69) for ACE inhibitors (Figure 2) and 0.46 (95% CI, 0.06 to 3.70) for ARBs (Figure 3). Multivariable analysis revealed the findings to be independent of demographic variables, comorbidities, type of contrast medium, and the prophylactic strategies utilized.
Figure 1.
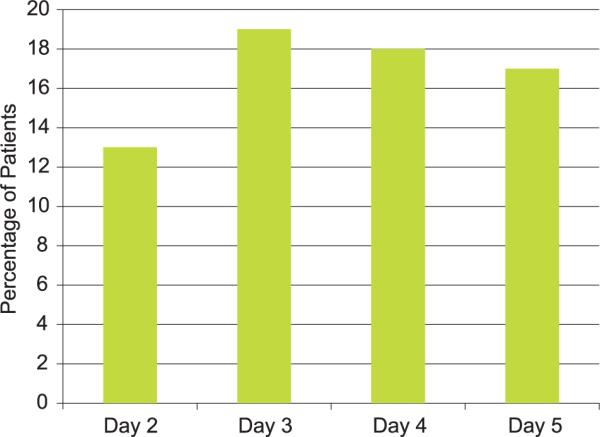
Percentage of patients with acute kidney failure relative to days after contrast exposure.
Figure 2.
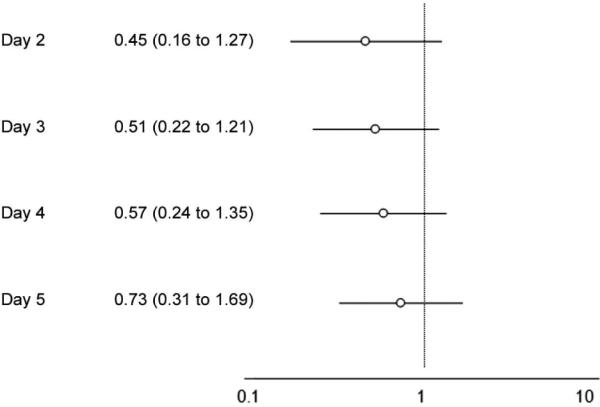
Odds ratios of acute kidney failure in patients on angiotensin-converting enzyme inhibitors (95% confidence interval) relative to days after contrast exposure.
Figure 3.
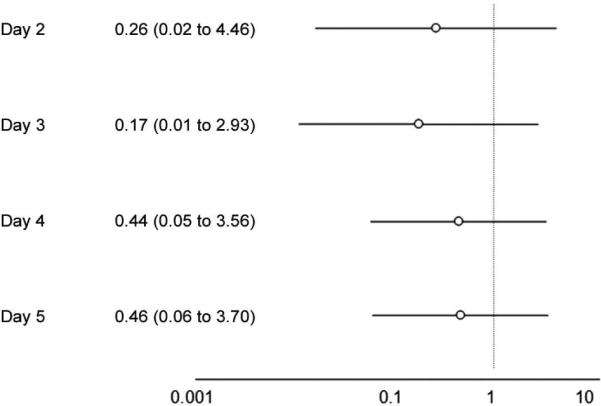
Odds ratios of acute kidney failure in patients on angiotensin receptor blockers (95% confidence interval) relative to days after contrast exposure.
DISCUSSION
We performed a retrospective study of patients with CKD Stage 3 or 4 who were on or off RAAS blockade at the time of coronary angiography. A total of 178 patients were included in the study, of whom 35% were on ACE inhibitors and 7% were on ARBs. The results showed a trend towards a protective effect with RAAS blockade, however, the results did not achieve statistical significance. Multivariable analysis revealed the findings to be independent of demographic variables, comorbidities, type of contrast medium, and the prophylactic strategies utilized.
The incidence of CIN varies widely between 10% to 50% among patients, depending on the presence of risk factors such as CKD, the definition of CIN, the amount and type of the contrast medium administered, and the exact radiologic procedure. Overall, the rate of AKF requiring dialysis from CIN appears to be low. In a retrospective study of 58 000 coronary procedures, only 10 and 49 patients required dialysis within one week and one month after contrast administration, respectively.16
Several risk factors for the development of CIN have been established. Studies have shown that underlying renal insufficiency (serum creatinine greater than 1.5 mg/dL or estimated GFR less than 60 mL/min/1.73 m2 by the MDRD), diabetic nephropathy with renal insufficiency, heart failure, hypovolemia or states of reduced perfusion, percutaneous coronary intervention, and high total doses of the contrast medium all predispose the patient to development of CIN.2,17,18 A few scoring systems including well-established risk factors for CIN have been developed to estimate the individual risk of CIN and dialysis, the most familiar of which has been developed by Mehran and coworkers.7
Whether certain medications, specifically RAAS blockade agents, are risk factors for development of CIN remains controversial. A randomized prospective study was published by Gupta and colleagues over a decade ago, in which patients undergoing coronary angiography were randomized to receive captopril or placebo. Renal scintigraphy scans were used to measure GFR and it was concluded that patients who had received captopril had a mean increase in the GFR of 13 mL/min compared to placebo.19 Other investigators have reported conflicting findings. In a recent study, Kiski and colleagues performed a retrospective analysis of patients who participated in a single-center prospective study to compare different prophylactic strategies for CIN prevention. The impact of RAAS blockade on the frequency of CIN was assessed. Patients treated with RAAS blockade before exposure to contrast media developed significantly more CIN episodes within 72 hours (11.9% versus 4.2%, P = .006). Using multivariable analysis, RAAS blockade was found to be an independent predictor of CIN (odds ratio, 3.082; 95% CI, 1.23 to 7.70, P =.02).20
The limitations of this study include the single-center nature and the retrospective design. In addition, baseline creatinine was noted on the day of contrast administration; however, not all patients had serum creatinine values documented months prior to determine true baseline. Lastly, only patients who had remained in the hospital and had creatinine values 5 days after contrast exposure were included in this analysis. Thus, the results may not be generalizable to stable outpatients undergoing coronary angiography.
CONCLUSIONS
This retrospective study demonstrates that patients on ACE inhibitor or ARB while undergoing cardiac catheterization are not at a higher risk of developing CIN. Prospective randomized trials are needed to help determine the effect of RAAS blockade on CIN.
Acknowledgments
Dr Nasrollah Ghahramani is supported by Award Number K23DK084300 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
CONFLICT OF INTEREST The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
REFERENCES
- 1.Tublin ME, Murphy ME, Tessler FN. Current concepts in contrast media-induced nephropathy. AJR Am J Roentgenol. 1998;171:933–9. doi: 10.2214/ajr.171.4.9762972. [DOI] [PubMed] [Google Scholar]
- 2.Parfrey PS, Griffiths SM, Barrett BJ, et al. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med. 1989;320:143–9. doi: 10.1056/NEJM198901193200303. [DOI] [PubMed] [Google Scholar]
- 3.Katzberg RW. Urography into the 21st century: new contrast media, renal handling, imaging characteristics, and nephrotoxicity. Radiology. 1997;204:297–312. doi: 10.1148/radiology.204.2.9240511. [DOI] [PubMed] [Google Scholar]
- 4.Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005;95:13–9. doi: 10.1016/j.amjcard.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 5.From AM, Bartholmai BJ, Williams AW, Cha SS, McDonald FS. Mortality associated with nephropathy after radiographic contrast exposure. Mayo Clin Proc. 2008;83:1095–100. doi: 10.4065/83.10.1095. [DOI] [PubMed] [Google Scholar]
- 6.Levy EM, Viscoli CM, Horwitz RI. The effect of acute renal failure on mortality. A cohort analysis. JAMA. 1996;275:1489–94. [PubMed] [Google Scholar]
- 7.Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393–9. doi: 10.1016/j.jacc.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 8.Agmon Y, Peleg H, Greenfeld Z, Rosen S, Brezis M. Nitric oxide and prostanoids protect the renal outer medulla from radiocontrast toxicity in the rat. J Clin Invest. 1994;94:1069–75. doi: 10.1172/JCI117421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cantley LG, Spokes K, Clark B, McMahon EG, Carter J, Epstein FH. Role of endothelin and prostaglandins in radiocontrast-induced renal artery constriction. Kidney Int. 1993;44:1217–23. doi: 10.1038/ki.1993.371. [DOI] [PubMed] [Google Scholar]
- 10.Mathew R, Haque K, Woothipoom W. Acute renal failure induced by contrast medium: steps towards prevention. BMJ. 2006;333:539–40. doi: 10.1136/bmj.38943.401852.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pflueger A, Larson TS, Nath KA, King BF, Gross JM, Knox FG. Role of adenosine in contrast media-induced acute renal failure in diabetes mellitus. Mayo Clin Proc. 2000;75:1275–83. doi: 10.4065/75.12.1275. [DOI] [PubMed] [Google Scholar]
- 12.Russo D, Minutolo R, Cianciaruso B, Memoli B, Conte G, De Nicola L. Early effects of contrast media on renal hemodynamics and tubular function in chronic renal failure. J Am Soc Nephrol. 1995;6:1451–8. doi: 10.1681/ASN.V651451. [DOI] [PubMed] [Google Scholar]
- 13.Weisberg LS, Kurnik PB, Kurnik BR. Radiocontrast-induced nephropathy in humans: role of renal vasoconstriction. Kidney Int. 1992;41:1408–15. doi: 10.1038/ki.1992.206. [DOI] [PubMed] [Google Scholar]
- 14.Pakfetrat M, Nikoo MH, Malekmakan L, et al. Risk Factors for contrast-related acute kidney injury according to risk, injury, failure, loss, and end-stage criteria in patients with coronary interventions. Iran J Kidney Dis. 2010;4:116–22. [PubMed] [Google Scholar]
- 15.Rose BD, Post TW. Clinical physiology of acid-base and electrolyte disorders. 5th ed. McGraw-Hill, Medical Pub. Division; New York: 2001. [Google Scholar]
- 16.Liss P, Persson PB, Hansell P, Lagerqvist B. Renal failure in 57 925 patients undergoing coronary procedures using iso-osmolar or low-osmolar contrast media. Kidney Int. 2006;70:1811–7. doi: 10.1038/sj.ki.5001887. [DOI] [PubMed] [Google Scholar]
- 17.Cigarroa RG, Lange RA, Williams RH, Hillis LD. Dosing of contrast material to prevent contrast nephropathy in patients with renal disease. Am J Med. 1989;86:649–52. doi: 10.1016/0002-9343(89)90437-3. [DOI] [PubMed] [Google Scholar]
- 18.McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368–75. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 19.Gupta RK, Kapoor A, Tewari S, Sinha N, Sharma RK. Captopril for prevention of contrast-induced nephropathy in diabetic patients: a randomised study. Indian Heart J. 1999;51:521–6. [PubMed] [Google Scholar]
- 20.Kiski D, Stepper W, Brand E, Breithardt G, Reinecke H. Impact of renin-angiotensin-aldosterone blockade by angiotensin-converting enzyme inhibitors or AT-1 blockers on frequency of contrast medium-induced nephropathy: a post-hoc analysis from the Dialysis-versus-Diuresis (DVD) trial. Nephrol Dial Transplant. 2010;25:759–64. doi: 10.1093/ndt/gfp582. [DOI] [PubMed] [Google Scholar]


