Abstract
Objective
To provide family physicians with a structured approach to patients presenting with memory difficulties.
Sources of information
The approach is based on an accredited memory clinic training program developed by the Centre for Family Medicine Memory Clinic in partnership with the Ontario College of Family Physicians.
Main message
Use of a structured clinical reasoning approach can assist physicians in achieving an accurate diagnosis in patients presenting with memory difficulties. Delirium, depression, and reversible causes need to be excluded, followed by differentiation among normal cognitive aging, mild cognitive impairment, and dementia. Obtaining collateral history and accurate functional assessment are critical. Common forms of dementia can be clinically differentiated by the order in which symptoms appear and by how cognitive deficits evolve over time. Typically, early signs of Alzheimer dementia involve impairment in episodic memory, whereas dementia involving predominantly vascular causes might present with early loss of executive function and relatively preserved episodic memory. Frontotemporal dementia and Lewy body spectrum disorders might have early loss of executive function and visuospatial function, as well as characteristic clinical features.
Conclusion
A clinical reasoning approach can help physicians achieve early, accurate diagnoses that can guide appropriate management and improve care for patients with memory difficulties.
While current Canadian consensus guidelines suggest that most patients with dementia can be adequately assessed and managed by their primary care physicians,1 the issues for patients with memory difficulties are complex and are often challenging to address in family practice. Indeed, for primary care physicians, studies have demonstrated that complexity of care and diagnostic uncertainty remain considerable barriers to the early diagnosis and management of dementia.2–5 Currently, most people living in the community with dementia remain undiagnosed and untreated,6–8 yet early detection offers important benefits.9 These include the option of early initiation of appropriate medications1,10 and access to supports,11–13 the opportunity for patients to maximally participate in future care planning,14,15 and possible net fiscal benefits.16
Achieving an early, accurate diagnosis is therefore an important first step in helping to guide appropriate further management for these patients. Medical education literature suggests that use of a clinically relevant framework or scaffolding can help in assessing patients with complex problems,17,18 and applying a structured clinical reasoning approach might help family physicians to simplify the process of assessing patients who present with memory difficulties.
Case description
Mrs S. is a 73-year-old patient presenting with memory difficulties. Her medical history includes atrial fibrillation, transient ischemic attack 5 years ago, diabetes, hypertension, hyperlipidemia, osteoarthritis, urinary incontinence, and depression first noted 3 years ago. Her current medications include 20 mg of citalopram once daily; 1 mg of lorazepam at bedtime as needed; 2 mg of warfarin once daily; 2 tablets of a combination of 300 mg acetaminophen and 30 mg of codeine, 3 times daily; 5 mg of bisoprolol once daily; 25 mg of hydrochlorothiazide once daily; 10 mg of atorvastatin once daily; 0.125 mg of digoxin once daily; 5 mg of ramipril once daily; 5 mg of glyburide twice daily; and 2 mg of tolterodine twice daily. She is a retired bookkeeper and has 3 children. She is accompanied by her husband and daughter.
During the past 2 years, family members have noticed increasingly frequent missed bill payments and medication errors. Mrs S. now has difficulty with meal preparation and can no longer manage chores. She repeats questions and gets lost in familiar environments. Her daughter is concerned about Mrs S.’s ability to drive.
Sources of information
The approach described below is based on a Mainpro-C accredited memory clinic training program19 developed by the Centre for Family Medicine (CFFM) Memory Clinic20 with the support of the Ontario College of Family Physicians.
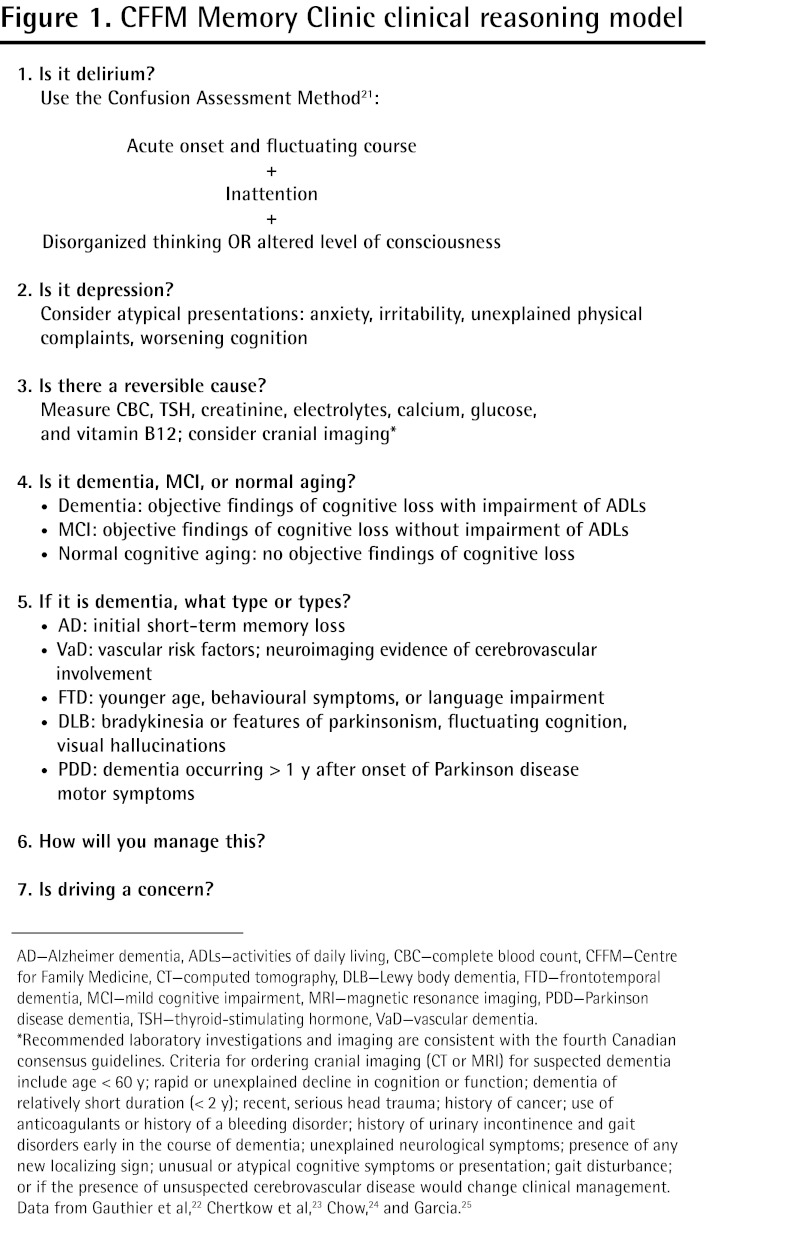
Clinical reasoning approach (Figure 1).21–25
Figure 1.
CFFM Memory Clinic clinical reasoning model
AD—Alzheimer dementia, ADLs—activities of daily living, CBC—complete blood count, CFFM—Centre for Family Medicine, CT—computed tomography, DLB—Lewy body dementia, FTD—frontotemporal dementia, MCI—mild cognitive impairment, MRI—magnetic resonance imaging, PDD—Parkinson disease dementia, TSH—thyroid-stimulating hormone, VaD—vascular dementia.
*Recommended laboratory investigations and imaging are consistent with the fourth Canadian consensus guidelines. Criteria for ordering cranial imaging (CT or MRI) for suspected dementia include age < 60 y; rapid or unexplained decline in cognition or function; dementia of relatively short duration (< 2 y); recent, serious head trauma; history of cancer; use of anticoagulants or history of a bleeding disorder; history of urinary incontinence and gait disorders early in the course of dementia; unexplained neurological symptoms; presence of any new localizing sign; unusual or atypical cognitive symptoms or presentation; gait disturbance; or if the presence of unsuspected cerebrovascular disease would change clinical management.
Data from Gauthier et al,22 Chertkow et al,23 Chow,24 and Garcia.25
When an elderly person presents with memory difficulties, the first step is to rule out delirium—a common, potentially fatal condition26 that is often missed.27 The Confusion Assessment Method is a validated, easy-to-use screening tool with high sensitivity and specificity for detection of delirium (Table 1).21
Table 1.
The Confusion Assessment Method diagnostic algorithm: The diagnosis of delirium requires a present or abnormal rating for criteria 1 and 2 plus either 3 or 4.
| CRITERIA | DESCRIPTION |
|---|---|
| 1. Acute onset and fluctuating course | Is there evidence of an acute change in the patient’s mental status? Did this behaviour fluctuate during the past day—ie, come and go or increase and decrease in severity? (Usually requires information from family members or caregivers) |
| 2. Inattention | Does the patient have difficulty focusing?—eg, are they easily distracted or do they have difficulty keeping track of what is being said? (Inattention can be detected by the digit span test or asking for the days of the week to be recited backward) |
| 3. Disorganized thinking | Is the patient’s speech disorganized or incoherent, such as rambling or irrelevant conversation, unclear or illogical flow of ideas, or unpredictable switching between subjects? (Disorganized thinking and sleepiness can also be detected during conversation with the patient) |
| 4. Altered level of consciousness | Overall, would you rate this patient’s level of consciousness as alert (normal), vigilant (hyperalert), lethargic (drowsy, easily aroused), stupor (difficult to arouse), or coma (cannot be roused)? (All ratings except alert are scored as abnormal) |
Data from Inouye et al.21
Those with suspected delirium require a thorough history and physical examination to identify underlying causes. Common precipitants include medications (particularly highly anticholinergic drugs, benzodiazepines, and narcotic analgesics), metabolic imbalance, infection, and occult organ failure such as myocardial infarction or respiratory failure.28,29
The second step is to rule out depression, which might mimic or coexist with dementia. In elderly persons, depression can present atypically with unexplainable physical symptoms, social withdrawal, anxiety, or memory difficulties. In patients with dementia, depression might present as cognitive deterioration, apathy, irritability, or lack of interest in previously enjoyed activities. The Geriatric Depression Scale30 or SIG E CAPS mnemonic list of symptoms31 can be used to screen for depression in elderly persons with normal cognitive functioning or mild to moderate cognitive loss. The Cornell Scale for Depression in Dementia is the most validated screen for depression in patients with moderate to severe dementia30,32,33 but it might be less practical for use in busy family practice. If depression is suspected, a trial of therapy with antidepressant medication with low anticholinergic load and few drug interactions (eg, citalopram) might be warranted, with reassessment of cognitive functioning after the depression is adequately treated. Of note, patients experiencing a first episode of depression after age 60 often go on to develop dementia.34
It is important to exclude reversible causes,23–25 as outlined in Figure 1.21–25 If none is identified, the next step is to determine whether the patient’s memory difficulties represent “normal” cognitive aging, mild cognitive impairment (MCI), or dementia. These represent a continuum of cognitive states in the elderly. Normal aging is characterized by patients’ subjective complaints of memory loss but no substantially abnormal findings on cognitive testing.35 Slower processing speed and naming difficulties particularly with proper nouns can be common manifestations of normal cognitive aging,36 but, typically, forgotten memories are recalled with cues. Mild cognitive impairment refers to the symptomatic predementia stage and has a prevalence of 16.8% in those 65 years of age and older37 and a lifetime conversion rate to dementia of 60% to 80%.38,39 In MCI, there are subjective complaints of memory loss and objective evidence of impairment on cognitive testing, but no substantial decline in functional abilities.39,40 Validated tools such as the Montreal Cognitive Assessment (MoCA) can be used to screen for impairment in various domains of cognitive functioning. Compared with the Mini-Mental State Examination (MMSE), the MoCA is a more sensitive screening tool for the milder stages of cognitive impairment commonly seen in ambulatory care.41 The MoCA is validated for use in various medical conditions, in many different languages, and in several international settings; currently, the Canadian Stroke Consortium and the US National Institutes of Health recommended that the MoCA be used for cognitive assessment.
Functional impairment is determined by the patient’s decline in ability to perform 1 or more activities of daily living, which can be assessed with the CFFM Memory Clinic Brain Map, available from CFPlus.*
If a decline in functional abilities is identified and there is evidence of considerable impairment in at least 1 domain on cognitive testing, then a diagnosis of dementia can be considered. The Diagnostic and Statistical Manual of Mental Disorders, 4th edition, criteria for dementia include memory loss, decline in at least 1 other cognitive domain (aphasia, apraxia, agnosia, or executive function), and substantial functional, social, or occupational impairment with decline from the previous level of functioning.42 Revisions are proposed for the fifth edition, in which dementia criteria will be redefined.43 The prevalence of dementia in Canadians older than 60 years of age is estimated to be 7%.44 Common types of dementia include Alzheimer disease, vascular dementia, and mixed dementia (Alzheimer plus vascular pathology); in community-based studies, mixed dementia seems to be most common.45 Less frequently encountered dementia types include Lewy body spectrum disorders (Lewy body dementia and Parkinson disease dementia) and frontotemporal dementia. It is important to diagnose the type of dementia involved, if possible, because treatment and prognosis for patients can differ depending on the underlying cause. The differentiation between the various types of dementia remains a clinical exercise based on the order in which symptoms appeared and the evolution of specific cognitive deficits over time.46
Clinical features of common types of dementia
Typical Alzheimer disease is characterized by early episodic memory loss (deficits in recall of recently learned information, often referred to as short-term memory loss), followed by later involvement of executive dysfunction and visuospatial impairment as the pathology spreads from the medial temporal lobe and hippocampus to other areas of the brain.47,48 Much less commonly, Alzheimer disease can present atypically with prominent and early behavioural problems, executive dysfunction, or other focal cortical syndromes.48 On cognitive testing, patients with Alzheimer disease usually demonstrate deficits in episodic memory early in the disease, with impaired 3-word delayed recall on the MMSE or 5-word delayed recall on the MoCA.
Currently there is a lack of consensus about the diagnostic criteria for vascular and mixed dementias.45,46,49,50 These conditions might represent a continuous spectrum of conditions with relatively pure vascular-type dementia on one end, relatively pure Alzheimer disease on the other end, and a combination of pathologies (mixed dementia) representing the largest group in between.51
At present, vascular dementia remains a clinical-radiologic diagnosis: in addition to vascular risk factors, there must be neuroimaging evidence of cerebrovascular involvement. Typically, there is early loss of executive function46 owing to vascular disease affecting primarily the frontal lobes and their subcortical connections. Executive function refers to cognitive processes that are responsible for planning, initiating, sequencing, and monitoring complex goal-directed behaviours.52 Examples of findings suggestive of executive dysfunction include abnormalities in the Trail Making Test Part B53 (which tests attention switching between letters and numbers), phonemic verbal fluency54 (eg, f words on the MoCA), or the Luria Fist-Edge-Palm test.55
Mixed dementia remains an enigma with no currently accepted, validated clinical guidelines for diagnosis.45,50 Patients with mixed dementia will have features of both Alzheimer disease and vascular dementia. They will have vascular risk factors but neuroimaging evidence of cerebrovascular infarcts might or might not be present.
Frontotemporal dementias typically present in the middle years of life with early progressive changes in behaviour, personality, or language functioning. Behavioural changes include loss of social skills, emotional blunting, loss of insight, and lack of concern.56,57 Patients presenting with language forms of frontotemporal dementia might have word-finding difficulties and speech that is nonfluent (sparse, agrammatic, containing primarily nouns, with frequent word-finding pauses54) or fluent but with impaired comprehension.58 On cognitive testing, there is often early loss of executive function with relative preservation of memory and visuospatial skills.56
Lewy body spectrum disorders represent a continuum of diseases associated with Lewy body pathology and include Parkinson disease dementia and Lewy body dementia. These conditions share common clinical features of bradykinesia and other symptoms of parkinsonism, fluctuating alertness and cognition, and often the presence of well-formed visual hallucinations.59 Although it is an arbitrary distinction, Parkinson disease dementia and Lewy body dementia have been differentiated by the “1-year rule”: Parkinson disease dementia is suspected if onset of dementia occurs after a year or more of parkinsonism; in Lewy body dementia, dementia onset is before or within a year of the development of parkinsonism symptoms.60 Often, findings on cognitive testing demonstrate early loss of executive and visuospatial function with relative sparing of memory and language functions until the later stages of illness.46,61
Screening tests for visuospatial function (constructional praxis) can include pen-and-paper reproduction of intersecting pentagons on the MMSE or the 3-dimensional cube on the MoCA. Clock drawing tests assess both visuospatial and executive functioning.62 Visuospatial tasks rely primarily on parietal lobe functioning but also involve frontal and occipital lobes.54
Steps 5 and 6 of the CFFM Memory Clinic clinical reasoning model address management and driving issues that have been well documented elsewhere.1,63–65 Molnar et al provide a practical approach to assessing fitness to drive in dementia.53
Brain map
Common types of dementia can be clinically differentiated by the order in which symptoms and signs appear over time. This requires careful history taking with corroborated information from family members, as well as supporting evidence on cognitive testing and targeted physical examination for focal neurologic deficits or features of parkinsonism. Areas of deficits on cognitive test performance can help to identify the parts of the brain affected by the pathologic process, thus providing important clues to the type of dementia involved. To facilitate localization of these deficits, we have developed a CFFM Memory Clinic Brain Map* to assist the busy primary care physician in mapping elements of cognitive screening tests that can help identify the type of dementia involved. This approach to education is consistent with the theory of cognitive apprenticeship,17,18 in which the Brain Map, along with the clinical reasoning model, serves as a scaffold to guide thinking processes as physicians become more skilled in assessing patients with memory problems
Case resolution
On cognitive testing, Mrs S.’s MoCA score is 14 out of 30, with 0 out of 5 for delayed recall, impairment on the Trail Making Test and cube drawing, and verbal fluency of just 5 f words. Performance on the clock drawing test is grossly impaired, as is performance on the Trail Making Test Part B, which has numerous errors and requires 5 minutes to complete. She is unable to perform the Luria Fist-Edge-Palm test. She does not appear depressed. A cranial computed tomography scan reveals moderate periventricular microangiopathic changes.
Working through the CFFM clinical reasoning model, Mrs S. does not meet the criteria for delirium based on the Confusion Assessment Method; however, her cognition might be adversely affected by lorazepam, codeine, and tolterodine (which has high anticholinergic load), and these drugs should be discontinued and her cognitive functioning reassessed. Her depression is appropriately treated with citalopram. If, after medication adjustment, her cognitive deficits persist, she might have dementia, as shown by impairment in activities of daily living and objective findings of deficits on cognitive testing in episodic memory (delayed recall), executive functioning (trails testing, verbal fluency, Luria test), and visuospatial functioning (clock and cube drawing).
The likely diagnosis is mixed dementia, given features of both Alzheimer disease (predominance of episodic memory loss) and vascular dementia (transient ischemic attack and vascular risk factors.) Appropriate management can be initiated, and fitness to drive must be assessed.
Conclusion
A 7-step clinical reasoning approach and the use of a Brain Map can assist primary care physicians in assessing patients presenting with memory difficulties. After excluding delirium, depression, and reversible causes, a distinction must be made between normal cognitive aging, MCI, and dementia. Common forms of dementia can often be clinically differentiated by the order in which cognitive deficits appear and by how symptoms evolve over time. Office-based cognitive testing can supplement patient history in sorting out the common types of dementia likely to be seen in primary care. This clinical reasoning approach might help primary care physicians achieve early, accurate diagnosis that can guide appropriate management and improve care for patients with dementia.
KEY POINTS
Diagnostic uncertainty and the complexity of the care required for patients with dementia remain considerable barriers to the early diagnosis and management of dementia in primary care. Early, accurate diagnosis is an important first step in helping to guide appropriate management for such patients. The authors present a 7-step clinical reasoning model to help physicians assess patients presenting with memory difficulties. Office-based cognitive testing can supplement patient history in sorting out the common types of dementia likely to be seen in primary care.
Footnotes
This article has been peer reviewed.
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de mars 2013 à la page e129.
The Centre for Family Medicine Memory Clinic Brain Map is available at www.cfp.ca. Go to the full text of the article online, then click on CFPlus in the top right-hand side of the page.
Contributors
All authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Hogan DB, Bailey P, Carswell A, Clarke B, Cohen C, Forbes D, et al. Management of mild to moderate Alzheimer’s disease and dementia. Alzheimers Dement. 2007;3(4):355–84. doi: 10.1016/j.jalz.2007.07.006. Epub 2007 Sep 17. [DOI] [PubMed] [Google Scholar]
- 2.Hinton L, Franz CE, Reddy G, Flores Y, Kravitz RL, Barker JC. Practice constraints, behavioral problems, and dementia care: primary care physicians’ perspectives. J Gen Intern Med. 2007;22(11):1487–92. doi: 10.1007/s11606-007-0317-y. Epub 2007 Sep 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pimlott NJ, Persaud M, Drummond N, Cohen CA, Silvius JL, Seigel K, et al. Family physicians and dementia in Canada. Part 2. Understanding the challenges of dementia care. Can Fam Physician. 2009;55:508-9.e1–7. Available from: www.cfp.ca/content/55/5/508.full.pdf+html. Accessed 2013 Jan 23. [PMC free article] [PubMed] [Google Scholar]
- 4.Foster NL. Barriers to treatment: the unique challenges for physicians providing dementia care. J Geriatr Psychiatry Neurol. 2001;14(4):188–98. doi: 10.1177/089198870101400404. [DOI] [PubMed] [Google Scholar]
- 5.Koch T, Iliffe S, EVIDEM-ED Project Rapid appraisal of barriers to the diagnosis and management of patients with dementia in primary care: a systematic review. BMC Fam Pract. 2010;11:52. doi: 10.1186/1471-2296-11-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sternberg SA, Wolfson C, Baumgarten M. Undetected dementia in community-dwelling older people: the Canadian Study of Health and Aging. J Am Geriatr Soc. 2000;48(11):1430–4. doi: 10.1111/j.1532-5415.2000.tb02633.x. [DOI] [PubMed] [Google Scholar]
- 7.Feldman HH, Jacova C, Robillard A, Garcia A, Chow T, Borrie M, et al. Diagnosis and treatment of dementia. 2. Diagnosis. CMAJ. 2008;178(7):825–36. doi: 10.1503/cmaj.070798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valcour VG, Masaki KH, Curb D, Blanchette PL. The detection of dementia in the primary care setting. Arch Intern Med. 2000;160(19):2964–8. doi: 10.1001/archinte.160.19.2964. [DOI] [PubMed] [Google Scholar]
- 9.Moise P, Schwarzinger M, Um MY, Dementia Experts’ Group . Dementia care in 9 OECD countries: a comparative analysis. Paris, Fr: Organization for Economic Co-operation and Development; 2004. Report No.: 13. Available from: www.oecd-ilibrary.org/social-issues-migration-health/dementia-care-in-9-oecd-countries_485700737071. Accessed 2011 Nov 22. [Google Scholar]
- 10.Gauthier SG. Alzheimer’s disease: the benefits of early treatment. Eur J Neurol. 2005;12(Suppl 3):11–6. doi: 10.1111/j.1468-1331.2005.01322.x. [DOI] [PubMed] [Google Scholar]
- 11.Brodaty H, Green A, Koschera A. Meta-analysis of psychosocial interventions for caregivers of people with dementia. J Am Geriatr Soc. 2003;51(5):657–64. doi: 10.1034/j.1600-0579.2003.00210.x. [DOI] [PubMed] [Google Scholar]
- 12.Weber SR, Pirraglia PA, Kunik ME. Use of services by community-dwelling patients with dementia: a systematic review. Am J Alzheimers Dis Other Demen. 2011;26(3):195–204. doi: 10.1177/1533317510392564. Epub 2011 Jan 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mittelman MS, Ferris SH, Shulman E, Steinberg G, Levin B. A family intervention to delay nursing home placement. JAMA. 1996;276(21):1725–31. [PubMed] [Google Scholar]
- 14.Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care. Alzheimer Dis Assoc Disord. 2009;23(4):306–14. doi: 10.1097/WAD.0b013e3181a6bebc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erde EL, Nadal EC, Scholl TO. On truth telling and the diagnosis of Alzheimer’s disease. J Fam Pract. 1988;26(4):401–6. [PubMed] [Google Scholar]
- 16.Weimer DL, Sager MA. Early identification and treatment of Alzheimer’s disease: social and fiscal outcomes. Alzheimers Dement. 2009;5(3):215–26. doi: 10.1016/j.jalz.2009.01.028. Epub 2009 Apr 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Facione NC, Facione PA. Critical thinking and clinical reasoning in the health sciences: a teaching anthology. Millbrae, CA: Insight Assessment, The California Academic Press; 2008. Critical thinking and clinical judgment; pp. 1–13. [Google Scholar]
- 18.Ambrose SA, Bridges MW, DiPietro M, Lovett MC, Norman MK. How learning works: 7 research-based principles for smart teaching. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 19.Lee L, Kasperski J, Weston WW. Building capacity for dementia care: a training program to develop primary care memory clinics. Can Fam Physician. 2011;57:e249–52. Available from: www.cfp.ca/content/57/7/e249.full.pdf+html. Accessed 2013 Jan 29. [PMC free article] [PubMed] [Google Scholar]
- 20.Lee L, Hillier LM, Stolee P, Heckman G, Gagnon M, McAiney CA, et al. Enhancing dementia care: a primary care based memory clinic. J Am Geriatr Soc. 2010;58(11):2197–204. doi: 10.1111/j.1532-5415.2010.03130.x. [DOI] [PubMed] [Google Scholar]
- 21.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 22.Gauthier S, Patterson C, Chertkow H, Gordon M, Herrmann N, Rockwood K, et al. Recommendations of the 4th Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD4) Can Geriatr J. 2012;15(4):120–6. doi: 10.5770/cgj.15.49. Epub 2012 Dec 4. Available from: www.cgjonline.ca/index.php/cgj/article/view/49/96. Accessed 2013 Feb 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chertkow H, Bergman H, Schipper HM, Gauthier S, Bouchard R, Fontaine S, et al. Assessment of suspected dementia. Can J Neurol Sci. 2001;28(Suppl 1):S28–41. doi: 10.1017/s0317167100001189. [DOI] [PubMed] [Google Scholar]
- 24.Chow T. Structural neuroimaging in the diagnosis of dementia. Alzheimers Dement. 2007;3(4):333–5. doi: 10.1016/j.jalz.2007.07.016. Epub 2007 Sep 10. [DOI] [PubMed] [Google Scholar]
- 25.Garcia A. Cobalamin and homocysteine in older adults: do we need to test for serum levels in the work-up of dementia? Alzheimers Dement. 2007;3(4):318–24. doi: 10.1016/j.jalz.2007.07.003. Epub 2007 Sep 19. [DOI] [PubMed] [Google Scholar]
- 26.Siddiqi N, House AO, Homes JD. Occurrence and outcomes of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350–64. doi: 10.1093/ageing/afl005. Epub 2006 Apr 28. [DOI] [PubMed] [Google Scholar]
- 27.Saxena S, Lawley D. Delirium in the elderly: a clinical review. Postgrad Med J. 2009;85(1006):405–13. doi: 10.1136/pgmj.2008.072025. [DOI] [PubMed] [Google Scholar]
- 28.Young J, Inouye SK. Delirium in older people. BMJ. 2007;334(7598):842–6. doi: 10.1136/bmj.39169.706574.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chew ML, Mulsant BH, Pollock BG, Lehman ME, Greenspan A, Mahmoud RA, et al. Anticholinergic activity of 107 medications commonly used by older adults. J Am Geriatr Soc. 2008;56(7):1333–41. doi: 10.1111/j.1532-5415.2008.01737.x. [DOI] [PubMed] [Google Scholar]
- 30.Watson LC, Pignone MP. Screening accuracy for late-life depression in primary care: a systematic review. J Fam Pract. 2003;52(12):956–64. [PubMed] [Google Scholar]
- 31.Jenike MA. Assessment and treatment of affective illness in the elderly. J Geriatr Psychiatry Neurol. 1988;1(2):89–107. doi: 10.1177/089198878800100206. [DOI] [PubMed] [Google Scholar]
- 32.Wancata J, Alexandrowicz R, Marquet B, Weiss M, Friedrich F. The criterion validity of the Geriatric Depression Scale: a systematic review. Acta Psychiatr Scand. 2006;114(6):398–410. doi: 10.1111/j.1600-0447.2006.00888.x. [DOI] [PubMed] [Google Scholar]
- 33.Kørner A, Lauritzen L, Abelskov K, Gulmann N, Brodersen AM, Wedervang-Jensen T, et al. The Geriatric Depression Scale and the Cornell Scale for Depression in Dementia. A validity study. Nord J Psychiatry. 2006;60(5):360–4. doi: 10.1080/08039480600937066. [DOI] [PubMed] [Google Scholar]
- 34.Alexopoulos GS, Meyers BS, Young RC, Mattis S, Kakuma T. The course of geriatric depression with “reversible dementia”: a controlled study. Am J Psychiatry. 1993;150(11):1693–9. doi: 10.1176/ajp.150.11.1693. [DOI] [PubMed] [Google Scholar]
- 35.Petersen RC, Smith GE, Waring SC, Ivnik RJ, Kokmen E, Tangelos EG. Aging, memory, and mild cognitive impairment. Int Psychogeriatr. 1997;9(Suppl 1):65–9. doi: 10.1017/s1041610297004717. [DOI] [PubMed] [Google Scholar]
- 36.Budson AE. Understanding memory dysfunction. Neurologist. 2009;15(2):71–9. doi: 10.1097/NRL.0b013e318188040d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Graham JE, Rockwood K, Beattie BL, Eastwood R, Gauthier S, Tuokko H, et al. Prevalence and severity of cognitive impairment with and without dementia in an elderly population. Lancet. 1997;349(9068):1793–6. doi: 10.1016/S0140-6736(97)01007-6. [DOI] [PubMed] [Google Scholar]
- 38.Busse A, Angermeyer MC, Riedel-Heller SG. Progression of mild cognitive impairment to dementia: a challenge to current thinking. Br J Psychiatry. 2006;189:399–404. doi: 10.1192/bjp.bp.105.014779. [DOI] [PubMed] [Google Scholar]
- 39.Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256(3):183–94. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 40.Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging and Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9. doi: 10.1016/j.jalz.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 42.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Publishing, Inc; 2000. text revision. [Google Scholar]
- 43.American Psychiatric Association . DSM-5 development. S 24 major neurocognitive disorder. Arlington, VA: American Psychiatric Association; 2012. Available from: www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=419. Accessed 2011 Nov 22. [Google Scholar]
- 44.Alzheimer’s Society of Canada . Rising tide: the impact of dementia on Canadian society. Toronto, ON: Alzheimer’s Society of Canada; 2010. [Google Scholar]
- 45.Nadeau Y, Black SE. Mixed dementia: the most common cause of dementia? Can J Diagn. 2010;27(4):35–44. [Google Scholar]
- 46.Robillard A. Clinical diagnosis of dementia. Alzheimers Dement. 2007;3(4):292–8. doi: 10.1016/j.jalz.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 47.McKhann GM, Knopman DS, Chertkow H, Hyman BD, Jack CR, Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup. Alzheimers Dement. 2011;7(3):263–9. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alladi S, Xuereb J, Bak T, Nestor P, Knibb J, Patterson K, et al. Focal cortical presentations of Alzheimer’s disease. Brain. 2007;130(Pt 10):2636–45. doi: 10.1093/brain/awm213. [DOI] [PubMed] [Google Scholar]
- 49.Moorhouse P, Rockwood K. Vascular cognitive impairment: current concepts and clinical developments. Lancet Neurol. 2008;7(3):246–55. doi: 10.1016/S1474-4422(08)70040-1. [DOI] [PubMed] [Google Scholar]
- 50.Jellinger KA. The enigma of mixed dementia. Alzheimers Dement. 2007;3(1):40–53. doi: 10.1016/j.jalz.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 51.Viswanathan A, Rocca WA, Tzourio C. Vascular risk factors and dementia. How to move forward? Neurology. 2009;72(4):368–74. doi: 10.1212/01.wnl.0000341271.90478.8e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Royall DR, Lauterbah EC, Cummings JL, Reeve A, Rummans TA, Kaufer DI, et al. Executive control function. A review of its promise and challenges for clinical research. J Neuropsychiatry Clin Neurosci. 2002;14(4):377–405. doi: 10.1176/jnp.14.4.377. [DOI] [PubMed] [Google Scholar]
- 53.Molnar FJ, Byszewski AM, Rapoport M, Dalziel WB. Practical experience-based approaches to assessing fitness to drive in dementia. Geriatr Aging. 2009;12(2):83–92. [Google Scholar]
- 54.Strub RL, Black FW. The mental status examination in neurology. 4th ed. Philadelphia, PA: F.A. Davis Company; 2000. [Google Scholar]
- 55.Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000;55(11):1621–6. doi: 10.1212/wnl.55.11.1621. [DOI] [PubMed] [Google Scholar]
- 56.Neary D, Snowdon J, Mann D. Frontotemporal dementia. Lancet Neurol. 2005;4(11):771–80. doi: 10.1016/S1474-4422(05)70223-4. [DOI] [PubMed] [Google Scholar]
- 57.Kertesz A, Nadkarni N, Davidson W, Thomas AW. The Frontal Behavioral Inventory in the differential diagnosis of frontotemporal dementia. J Int Neuropsychol Soc. 2000;6(4):460–8. doi: 10.1017/s1355617700644041. [DOI] [PubMed] [Google Scholar]
- 58.Mesulam MM. Primary progressive aphasia. Ann Neurol. 2001;49(4):425–32. [PubMed] [Google Scholar]
- 59.Goldmann Gross R, Siderowf A, Hurtig HI. Cognitive impairment in Parkinson’s disease and dementia with Lewy bodies: a spectrum of disease. Neurosignals. 2008;16(1):24–34. doi: 10.1159/000109756. Epub 2007 Dec 5. [DOI] [PubMed] [Google Scholar]
- 60.McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, et al. Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology. 2005;65(12):1863–72. doi: 10.1212/01.wnl.0000187889.17253.b1. Erratum in: Neurology 2005;65(12):1992. [DOI] [PubMed] [Google Scholar]
- 61.McKeith I, Mintzer J, Aarsland D, Burn D, Chiu H, Cohen-Mansfield J, et al. Dementia with Lewy bodies. Lancet Neurol. 2004;3(1):19–28. doi: 10.1016/s1474-4422(03)00619-7. [DOI] [PubMed] [Google Scholar]
- 62.Royall DR, Cordes JA, Polk M. CLOX: an executive clock drawing task. J Neurol Neurosurg Psychiatry. 1998;64(5):588–94. doi: 10.1136/jnnp.64.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Qaseem A, Snow V, Cross JT, Jr, Forciea MA, Hopkins R, Jr, Shekelle P, et al. Current pharmacologic treatment of dementia: a clinical practice guideline from the American College of Physicians and the American Academy of Physicians. Ann Intern Med. 2008;148(5):370–8. doi: 10.7326/0003-4819-148-5-200803040-00008. [DOI] [PubMed] [Google Scholar]
- 64.Bocti C, Black S, Frank C. Management of dementia with a cerebrovascular component. Alzheimers Dement. 2007;3(4):398–403. doi: 10.1016/j.jalz.2007.07.009. Epub 2007 Sep 17. [DOI] [PubMed] [Google Scholar]
- 65.O’Brien JT, Burns A, BAP Dementia Consensus Group Clinical practice with anti-dementia drugs: a revised (second) consensus statement form the British Association for Psychopharmacology. J Psychopharmacol. 2011;25(8):997–1019. doi: 10.1177/0269881110387547. Epub 2010 Nov 18. [DOI] [PubMed] [Google Scholar]