Abstract
Objective
To study, in a sample of French Family Practitioners (FPs), beliefs and attitudes toward depression and how they vary according to training received in mental health.
Methods
The Depression Attitude Questionnaire (DAQ) was completed by 468 FPs from all regions of France, recruited by pharmaceutical company representatives to attend focus groups on the management of depression in general practice.
Results
A three factor model was derived from the DAQ, accounting for 37.7% of the total variance. The correlations between individual items of each component varied from 0.4 to 0.65 with an overall internal consistency of 0.47 (Cronbach’s alpha). FPs had an overall neutral position on component 1, professional ease, a positive view on the origins of depression and its amenability to change (component 2), and a belief in the necessity of medication and the benefit of antidepressant therapy (component 3). Training in mental health, specifically through continuing medical education and postgraduate psychiatric hospital training, was significantly and positively associated with both professional ease and a medication approach to treating depression.
Conclusion
this study is the first description of the beliefs and attitudes of French FPs towards depression using a standardized measure, the DAQ, despite the instrument’s limited psychometric properties. It shows the positive effect of training in mental health on attitudes towards depression.
Keywords: Adult; Attitude of Health Personnel; Depressive Disorder; psychology; therapy; Education, Medical, Continuing; Family Practice; methods; Female; France; Health Knowledge, Attitudes, Practice; Humans; Male; Mental Health Services; Middle Aged; Physicians, Family; education; Principal Component Analysis; Psychometrics; methods; Questionnaires
Introduction
The attitudes and beliefs of health professionals are of prime importance to the consultation process and outcome [1,2], and influence their ability to recognise symptoms, make diagnoses and offer adequate treatment for common mental disorders [3–6]. They are closely interlinked with various patient and practice factors, such as patients’ beliefs and explanatory models of illness [7,8], symptom presentation and somatisation [9–12], which facilitate or impede recognition and management of disorders.
There are few instruments available to measure clinicians’ attitudes to depression and its management [5,13]. The most widely used measure, the Depression Attitude Questionnaire (DAQ) [14], is a self-report scale for investigating attitudes to depression comprising 20 items scored on a 10 cm visual analogue scale ranging from ‘strongly disagree’ (0 cm) to ‘strongly agree’ (10 cm). Four main attitudinal components were initially identified by Principal Component Analysis (PCA) in a sample of 72 British FPs: professional unease in dealing with depressed patients; the belief that depressive symptoms are inevitable; recognition of depression as a clinical disorder and attitudes towards treatment. There is doubt however as to the validity of these attitudinal components in other primary care organisations [15]. Subsequent studies have used the DAQ in general practice and other settings to describe clinician’s attitudes. Kerr et al. compared attitudes to depression of psychiatrists and FPs and found FPs to show less professional ease than psychiatrists [16]. In a comparison of British and Brazilian FPs, Brazilian FPs differed from British FPs in considering care for depressed patients less rewarding and patients in need of antidepressant medication to be better off with a psychiatrist [17]. The DAQ has been used successfully as a measure of change to assess the effectiveness of teaching FPs skills in cognitive behaviour therapy [18], to predict clinical behaviour [19,20] and to assess attitudes in nursing staff [15,21–24]. Ross et al. using a modified version of the DAQ found that FPs with a pessimistic view of depression were less willing to be actively involved in its treatment [20].
Regarding the effect of mental health training on FPs’ attitudes, Richards et al. found that completing mental health training in the past 5 years was related to positive attitudes towards depression and more specifically to the DAQ dimensions of ‘FP helplessness’ and ‘FP effort’ in assisting depressed patients [5]. No association was found for postgraduate mental health qualifications. More recently, it has been shown that FPs with more complex psychosocial explanations of common mental disorders had greater interest, more training in mental health and more positive attitudes to depression [25], , using a composite of the four DAQ components identified by Botega et al. [14].
In France, research in primary care mental health is relatively recent and data are scarce on the detection and management of depression in this setting [26,27]. Yet, the organisation of French general practice differs substantially from that of other European countries with FPs working mainly alone, with no ancillary staff. There is limited collaboration with specialised mental health services and rapid referral of patients for specialised care or obtaining advice from specialists is thus difficult [28,29]. Postgraduate training of FPs in psychiatry is limited, with no compulsory clinical training. There is no compulsory continuing medical education training in mental health either [30]. The aim of this study is to describe the beliefs and attitudes of French FPs towards depression and investigate how these vary according to FP characteristics. A secondary aim is to evaluate the psychometric properties of the DAQ in this sample and compare the scales derived with those obtained elsewhere, in particular the DAQ validation study [17].
Methods
Sample
In 2006, approximately 5000 FPs from all over France were contacted via regional representatives of a pharmaceutical company to participate in focus groups to discuss the recognition and management of depression in their daily practice. There were no specific inclusion or exclusion criteria. The focus groups were organised by Lundbeck in collaboration with the Institut de Recherche en Médecine Générale (IRMG), an association of French FPs engaged in research. The pharmaceutical company sponsored the meetings but did not participate or listen to the discussions. Prior to the meeting the FPs were asked to complete the DAQ.
Questionnaire
FPs completed anonymously the DAQ along with a brief questionnaire eliciting their socio-demographic and practice characteristics, the year when they obtained their medical thesis, training in mental health, the type of training received and the need for future training. For the type of training received, FPs could tick any of the following: CME seminar (2 days); CME evening; hospital training in psychiatry as a FP trainee; belonging to a Balint group; personal training (in or through psychotherapy or psychoanalysis).
The DAQ had been translated and back-translated by independent bilingual researchers at Inserm Unit 1061 and piloted in a prior study with 46 FPs based in Montpellier (results not published). One item (12) however was not directly transferrable to French general practice: as there are no practice nurses, this was reformulated as a hypothetical situation.
Data analysis
Initial examination of the shared variance between the 20 DAQ responses revealed a Kaiser-Meyer-Olkin measure of sampling adequacy of 0.73, demonstrating adequacy of the sample to provide stable factor solutions. Examination of individual measures of sampling adequacy led to the exclusion of item 1 (adequacy level <0.5). PCA using scree plots and varimax rotation was performed on the remaining 19 items. Examination of the scree plot indicated a three-factor solution. Items 4 and 12 exhibiting weak (<0.35) loadings only and items 16 and 17 revealing complex loadings (two loadings > 0.35) were excluded. Scores on factors with negative loadings were transformed by subtracting the actual score from 10. For interpretation purposes, components 2 and 3 were inversed so that a positive score reflected what was considered as a positive attitude. Component scores were calculated for each FP as the average of the relevant items. Overall and component-specific internal consistency was measured using Cronbach’s alpha.
For the associations between each of the three DAQ components and FP characteristics, both univariate and multivariate analyses were carried out. Finally three multiple linear regression models were constructed, entering simultaneously sex of FP, age, training in mental health and need for training. Each model was then run substituting training in mental health by each of the 5 types of training. Both training in mental health and need for training were included in the models as there was no significant association between them. There was no interactive effect of the two variables on any of the three attitudinal components. Number of years of practice was highly correlated with age so was excluded from the analysis. Statistical significance was set at p<0.05. Statistical analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC, USA).
Results
Of the approximate 5000 FPs invited to participate in the focus groups, 10% accepted to participate. In all, 504 FPs from all regions of France participated in 84 focus group discussions and 468 FPs completed the DAQ.
Socio-demographic characteristics of the FP sample
Of the sample, 78.1% were male and 21.9% female. Mean age was 49.9 years (SD 7.76) with 24.1% of FPs aged under 45 years. On average FPs had been qualified for 22.9 years (SD 8.4).
Of the FPs reporting on past training, about two-thirds (307/452) declared having received some form of training in mental health; 235 (52%) a continuing medical education (CME) evening seminar, 159 (35.2%) a CME 2-day seminar, 68 (15%) personal training (psychotherapy, psychoanalysis), 62 (13.7%) as a FP trainee in a psychiatric hospital and 25 (5.5%) belonged to a Balint group. 84% of FPs declared a need for further training in mental health. In responses to an open question on the desired topic, the following areas were given: psychotherapy (34.6%), depression, anxiety and mourning (16.4%), conducting an interview (10.7%) and prescribing psychotropic medication (9.1%).
Responses to individual DAQ items
Mean scores for the 20 DAQ items, plotted on a 10 cm visual analogue scale with 95% confidence intervals, are shown in Figure 1.
Figure 1.
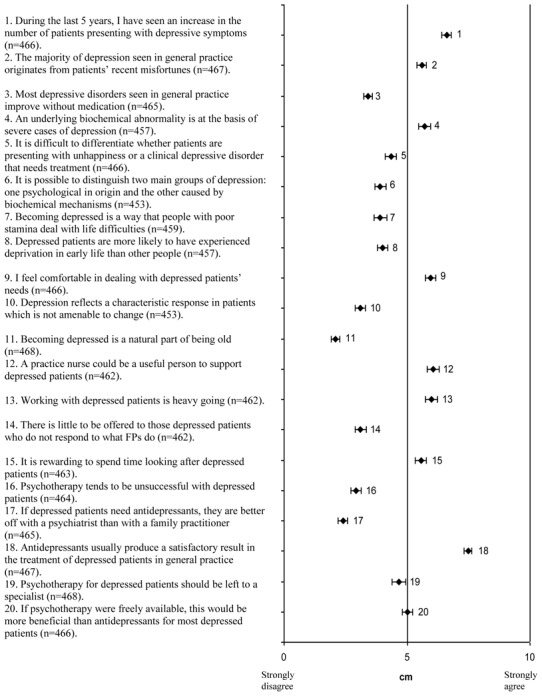
Mean scores presented with 95% confidence intervals on the DAQ items.
Ratings in three broad categories (agree, disagree, neutral) for the items are similar to those found in the Montpellier study and the DAQ validation study for 14 of the 20 items. Ratings are significantly different from those in the Montpellier study for items 3, 6 and 20 (Table 1).
Table 1.
Main differences in DAQ item scores between the current study and (a) the Montpellier study (b) the DAQ validation study, and sets of components identified in each study
| Current study (1) | Montpellier study (2) (unpublished data) | Validation study‡ [14] | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| DAQ | Summary score | mean (std) | Summary score | mean (std) | p (1/2) | Summary score |
| Item 3 | -ve | 3.41 (1.92) | -ve | 4.19 (2.00) | ** | +ve |
| Item 5 | -ve | 4.35 (2.44) | Neutral | 4.61 (2.58) | Neutral | |
| Item 6 | -ve | 3.92 (2.36) | Neutral | 4.86 (2.34) | * | Neutral |
| Item 8 | -ve | 4.01 (2.40) | Neutral | 4.55 (2.62) | +ve | |
| Item 19 | -ve | 4.66 (2.97) | Neutral | 5.22 (3.23) | Neutral | |
| Item 20 | Neutral | 5.02 (2.32) | +ve | 6.68 (2.42) | *** | +ve |
|
| ||||||
| DAQ Components (items and loadings) | DAQ Components (items and loadings) | DAQ Components (items and loadings) | ||||
|
| ||||||
| I-Professional ease (9,15 +ve, 5,13,14,19 –ve) II-Origins of depression and amenability to change (2,6,7,8,10,11 +ve) III- treatment of depression and benefit of antidepressant medication (3,20 +ve, 18 -ve) |
I- Origins of depression and necessity of treatment (2,3,5,7,8,11,12 +ve) II- Positive attitude to psychotherapy and treatment of depression in general practice (4,14,17,20 +ve, 1 –ve) III-Professional burden (13,19 +ve, 9 –ve) |
I-Preference for antidepressants over psychotherapy (4,7,16,18 +ve, 3,20 -ve II-Professional unease (13,19 +ve, 9,15 -ve) III-Inevitable course of depression(8,10,11,17 +ve) IV- Identification of depression (2,5,14 +ve) |
||||
Summary score:
-ve= mean score and 95% confidence interval lies between 0cm and 5cm reflecting disagreement
+ve= mean score and 95% confidence interval lies between 5cm and 10cm reflecting agreement
Neutral= the 95% confidence interval overlaps the middle boundary reflecting a neutral position
mean scores and 95% CI were not available
p values:
<0.05,
<0.01,
<0.001
Principal Components Analysis
A three-factor solution based on 15 of the 20 DAQ items (exclusion of items 1, 4, 12, 16, 17) was obtained by PCA, explaining 37.7% of the variance: Component 1 ‘professional ease’ (items 5, 9, 13, 14, 15, 19) (18.1% of the variance), Component 2 ‘origins of depression and its amenability to change’ (items 2, 6, 7, 8, 10, 11) (11%) and Component 3 ‘treatment of depression and benefit of antidepressant medication’ (items 3, 18, 20) (8.6%). Internal consistency between individual items of each component were 0.65, 0.54 and 0.4 for the first, second and third component respectively, and 0.47 for the 15 items.
Overall, FPs scored positively (mean score: 5.6, 95% CI: 5.4–5.7 ) on Component 1, suggesting they globally feel at ease recognising and treating depressed patients, and find it rewarding. The mean score on Component 2 (6.2, 95% CI: 6.1–6.4), suggests that FPs have a positive view of depression (not induced by old age, poor stamina or deprivation) which is considered to be amenable to change. Moreover, FPs believe medication is necessary to treat most depressed patients, with a positive view of antidepressants (mean score on Component 3: 6.3, 95% CI: 6.2–6.5).
Attitudinal components according to FP characteristics
Significance status for the associations between the mental health training variables and the three attitudinal components did not differ between the univariate and multivariate analyses. Training of some form in mental health is significantly associated with professional ease (Component 1), when adjusting for sex, age and expressing the need for training in this area (Table 2). This association is significant for all types of training, except CME evening courses. The mean score on Component 3 is significant higher among FPs trained in mental health, for 2-day and evening CME training courses and hospital training but not for Balint group participation or personal training.
Table 2.
Relationship between mental health training and the 3 DAQ components: multivariate analysis.
| Variables | N* | Component 1 Professional ease |
Component 2 Origins of depression and its amenability to change |
Component 3 Treatment of depression and benefit of antidepressant medication |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Mean (SD) | β (SE)** | p** | Mean (SD) | β (SE)** | p** | Mean (SD) | β (SE)** | p** | |||
|
| |||||||||||
| Need for training | No | 63 | 5.85 (1.75) | ref | 6.28 (1.32) | 6.61 (1.34) | |||||
| Yes | 333 | 5.52 (1.45) | −0.35 (0.20) | 0.08 | 6.24 (1.22) | −0.05 (0.17) | 0.75 | 6.32 (1.35) | −0.29 (0.18) | 0.10 | |
|
| |||||||||||
| Training in MH | No | 134 | 5.14 (1.52) | ref | 6.23 (1.17) | 6.17 (1.44) | |||||
| Yes | 262 | 5.79 (1.46) | 0.62 (0.16) | <0.0001 | 6.25 (1.26) | 0.02 (0.13) | 0.89 | 6.48 (1.29) | 0.30 (0.14) | 0.032 | |
|
| |||||||||||
| Types of training: | |||||||||||
|
| |||||||||||
| 2-day CME seminar | No | 262 | 5.38 (1.48) | ref | 6.20 (1.19) | ref | 6.26 (1.38) | ref | |||
| Yes | 134 | 5.94 (1.49) | 0.55 (0.15) | 0.0004 | 6.33 (1.31) | 0.11 (0.13) | 0.39 | 6.59 (1.25) | 0.33 (0.14) | 0.019 | |
|
| |||||||||||
| Evening CME seminar | No | 189 | 5.48 (1.53) | ref | 6.33 (1.23) | ref | 6.26 (1.35) | ref | |||
| Yes | 207 | 5.66 (1.45) | 0.21 (0.15) | 0.15 | 6.17 (1.23) | −0.15 (0.12) | 0.23 | 6.52 (1.31) | 0.31 (0.13) | 0.019 | |
|
| |||||||||||
| Hospital psychiatry | No | 340 | 5.45 (1.47) | ref | 6.21 (1.25) | ref | 6.34 (1.34) | ref | |||
| Yes | 56 | 6.30 (1.40) | 0.82 (0.21) | <0.0001 | 6.44 (1.11) | 0.23 (0.18) | 0.19 | 6.74 (1.21) | 0.40 (0.19) | 0.034 | |
|
| |||||||||||
| Balint Group | No | 376 | 5.38 (1.43) | ref | 6.19 (1.22) | ref | 6.38 (1.34) | ref | |||
| Yes | 20 | 6.63 (1.39) | 1.33 (0.32) | <0.0001 | 6.52 (1.24) | −0.25 (0.28) | 0.37 | 6.50 (1.34) | −0.08 (0.30) | 0.79 | |
|
| |||||||||||
| Personal training | No | 335 | 5.50 (1.46) | ref | 6.26 (1.23) | ref | 6.40 (1.34) | ref | |||
| Yes | 61 | 6.87 (1.48) | 1.21 (0.19) | <0.0001 | 5.94 (1.06) | 0.32 (0.17) | 0.06 | 6.25 (1.27) | 0.02 (0.18) | 0.91 | |
numbers vary slightly for each component. They are presented for component 2 which has the most missing values.
adjusted for age of FP, sex and need for training in mental health or training received in MH
Discussion
Scores on DAQ items
Despite caution required in comparing DAQ findings between studies, our scores on the specific DAQ items are very close to those found in the Montpellier study of 46 French FPs (unpublished data) (Table 1). The only significant differences are for items 3, 6 and 20 which may be explained by the different FP selection procedures: in the current national study FPs were invited to participate by pharmaceutical laboratory representatives, which may have led to the selection of FPs most in favour of medication for treating depression. In the regional Montpellier primary care study, FPs were randomly selected, with a 32% response rate [27]. Neither sample can be considered representative of French FPs.
Compared to the British DAQ validation study [14], there are only 6 items (3, 5, 6, 8, 19, 20) on which FPs seem to disagree (this is established by comparing scores plotted on visual analogue scales as the data from the British DAQ study were not available). Differences could be due to country differences in the organisation and delivery of primary care as well as to the timing of the studies, the DAQ validation study having been carried out 15 years earlier than the current study. As opposed to the French FPs, the British FPs globally agree that most depressive disorders seen in general practice improve without medication (item 3). This fits with findings from the WHO Mental Illness in General Health care study, where the overall prescription rate of tranquilizers and antidepressants was almost twice as high in the Paris study centre compared to the Manchester centre (18.5% versus 10.5%) [35]. However results from elsewhere suggest that the difference for antidepressant medication prescription alone would be much smaller [27,36]. Both British and French FPs agree with the statement that antidepressants produce satisfactory results in general practice (item 18). However British FPs are more open to psychotherapy as being a beneficial alternative to antidepressants (item 20). Contrary to the British FP sample, FPs in the current study disagree with the statement that it is difficult to differentiate whether patients are presenting with unhappiness or a clinical depressive disorder that needs treatment (item 5), suggesting greater ease at establishing a diagnosis of depression. Yet in the WHO study, FPs in the Paris and Manchester samples identified respectively 61.5% and 69.9% of ICD-10 depression cases [37]. Disagreement on item 5 would more likely be explained by the above-mentioned FP inclusion bias in the current study. Agreement with the statement that a practice nurse could be a useful person to support depressed patients (item 12), suggests French FPs would be open to more shared-care in group practices with paramedical staff as in the UK. At present, French FPs have little contact with mental health care teams and report communication with psychiatrists to be particularly difficult [29,38], whilst it has been shown that FPs with access to collaborative care with psychiatric services report greater knowledge, better skills and more comfort in managing psychiatric disorders [39].
Scores on DAQ components
Caution is needed in discussing the DAQ components as the measures of internal consistency of the scales are low, specifically for the second and third component (Cronbach’s alpha values of 0.65, 0.54 and 0.4 for the first, second and third component, respectively). With regard to Component 1, professional ease, FPs who had followed a training course in mental health, save evening seminars, belonged to a Balint group or had undertaken personal training, scored higher, than those who had not. Although differences in mean scores are small, these associations remained significant after adjusting for age and sex of FP and declared need for training in mental health. Evening seminars are mostly given by pharmaceutical companies may not provide adequate training, whether in length or content, for helping FPs feel at ease managing depressed patients [40]. Although FPs with more positive attitudes may select themselves for more intense forms of training, our findings suggest that training in mental health helps FPs feel more at ease in dealing with depression. This fits with the finding that Australian FPs who completed mental health training in the past 5 years felt less strain and stress in assisting their patients [5]. Comparisons between studies of components-specific as opposed to item-specific DAQ results is difficult as the number and types of components differ (see above).
In so far as Component 3, the belief in the benefits of medication treatment for depression, can be considered as a reliable subscale, FPs having trained in hospital psychiatry scored significantly higher on this subscale than others suggesting this type of training is beneficial to FPs. However, this holds only for severe cases of depression on which antidepressant medication has shown to be efficacious. Psychological interventions are recommended, with combined psychological therapy and antidepressant medication introduced in a stepped-care approach, for the frequent cases of subthreshold or mild depression encountered in primary care [41]. However, the DAQ does not take into account the severity of depression, or the concept of stepped-care and combined treatment. FPs participating in evening or 2-day CME seminars also scored significantly higher on Component 3. Hospital training in psychiatry is not compulsory in France, the only compulsory hospital placements being adult medicine, emergency medicine and gynaecology/paediatrics. To date, CME is compulsory for French FPs, although not for any specific discipline [30]. A third of the study FPs had never received formal training in mental health, and among those who had, 68% had only ever followed evening CME courses. Furthermore 80% of FPs stated they needed training in the management of depressed patients. Our findings therefore highlight the importance of developing structured and compulsory CME in mental health.
The recognition and treatment of depression is becoming an increasingly important part of the work of FPs throughout the world [42]. Our findings suggests training in mental health increases their ability to feel comfortable dealing with depression, which although not shown so far [19] could also improve their ability at evaluating symptom severity and establishing accurate diagnoses. Despite its limits, the DAQ is thus a practical and useful instrument for identifying FPs who may be in need of mental health training and can also be used as a training evaluation tool to compare pre and post-intervention beliefs and attitudes. With respect to the type and content of training, FPs need to be made aware of existing guidelines, although so far evidence suggests training FPs to follow guidelines does not improve outcome [43,44]. Other types of interventions to improve FPs management of depression include ‘collaborative care’, an enhanced form of consultation-liaison which includes a case manager to deliver care and liaise between GP specialist and patient [45]. Such models implemented in the USA [46,47] and the UK [48,49] have shown to be effective in terms of symptoms remission [46,48,49], as well as response to treatment and patient satisfaction with care for the RESPECT Care management model [46]. FPs experiencing this management model report it to be beneficial in terms of care to their patients and an attractive care management option for them [50]. FPs attitudes and behaviour about depression are also significantly modified by such experiences [47]. Obstacles to collaborative care are FPs working in solo-practices, unfamiliar with the concept of collaboration, the lack or type of reimbursement scheme [51] and facing competing demands [46]. Collaborative care has proven to be an effective and attractive care model for improving the management of depression in primary care. However its implementation in other settings such as France is a long-term perspective as it will require structural as well as cultural changes in the organisation and delivery of primary care.
Study limitations
The main limitation of the study is that it was carried out in a volunteer sample of FPs recruited, with no specific inclusion or exclusion criteria, by pharmaceutical company representatives. Not all FPs are willing to see pharmaceutical representatives, which introduces bias into the sample recruitment with the selection of a subset probably more interested in mental health. As we have no information on refusals, it is not possible to estimate the extent of the bias. Random recruitment of FPs for research studies yields poor results, with participation rates rarely exceeding 40%, which may introduce as much bias as other FP recruitment methods [27,31,32]. We compared the study sample with national figures for age and sex: male FPs are overrepresented in the study sample (76.9% compared to 60.5% for France as a whole), and FPs are also older with 12.4% under 40, 31.2% aged 40–49 and 56.4% aged 50 years and above compared to 17%, 32.8% and 50.3% respectively for France as a whole [33]. In the Montpellier FP sample, 56.5% of FPs were male, 30% were aged under 40, 35% 40–49 and 35% 50 years and above.
Another important limitation is the reliability of the DAQ. Findings from studies using this measure are inconsistent, identifying three ([20]; the Montpellier study (unpublished)), four [5] and even five [23] attitudinal components, which challenges the validity of the original four components [34]. Measures of validity have been reported in one study only [15], confirming our finding that the internal consistency of the measure and its derived subscales as well as the variance explained by the factor structure are low, suggesting the DAQ may be in need of revision.
The main strength of this study is that it was carried out in a large sample of FPs. The sampling means that the scores reported here cannot be taken as representative of French FPs. On the other hand, the large sample makes internal comparisons of subgroups feasible.
Conclusion
This study is the first description of the beliefs and attitudes of French FPs to depression, using a validated self-report scale. Overall, the study FPs had an optimistic attitude towards depression as being amenable to change with a positive view towards treatment with antidepressant medication. Professional ease (component 1) and belief in the benefits of antidepressants (component 3), were both significantly and positively associated with training, of different types, in mental health. This positive effect of mental health training has seldom been shown before [5]. A more detailed study of the types, contents, and satisfaction with training, as well as other types of interventions such as collaborative care, and their influence on daily practice and attitudes - using a more reliable and valid measure - is now warranted, specifically given the reported need for training and support by a large majority of FPs.
Acknowledgments
The authors would like to thank Lundbeck Laboratories for their support in recruiting the FPs, organising the focus groups and covering the financial costs associated with the meetings. They would also like to thank all of the FPs who participated, with no financial compensation, in the study.
Footnotes
None of the authors have any conflicts of interest.
References
- 1.Cooper LA, Brown C, Vu HT, et al. Primary care patients’ opinions regarding the importance of various aspects of care for depression. Gen Hosp Psychiatry. 2000;22:163–73. doi: 10.1016/s0163-8343(00)00073-6. [DOI] [PubMed] [Google Scholar]
- 2.Link BG, Struening EL, Neese-Todd S, et al. Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatr Serv. 2001;52:1621–6. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- 3.Marks JN, Goldberg DP, Hillier VF. Determinants of the ability of general practitioners to detect psychiatric illness. Psychol Med. 1979;9:337–53. doi: 10.1017/s0033291700030853. [DOI] [PubMed] [Google Scholar]
- 4.Ormel J, Giel R. Medical Effects of Nonrecognition of Affective Disorders in Primary Care. In: Sartorius N, Goldberg D, de Girolamo G, et al., editors. Psychological Disorders in General Medical Settings. Toronto: Hogrefe & Huber Publishers on behalf of the WHO; 1990. [Google Scholar]
- 5.Richards JC, Ryan P, McCabe MP, et al. Barriers to the effective management of depression in general practice. Aust N Z J Psychiatry. 2004;38:795–803. doi: 10.1080/j.1440-1614.2004.01464.x. [DOI] [PubMed] [Google Scholar]
- 6.Koenig HG. Physician attitudes toward treatment of depression in older medical inpatients. Aging Ment Health. 2007;11:197–204. doi: 10.1080/13607860600844457. [DOI] [PubMed] [Google Scholar]
- 7.Weich S, Morgan L, King M, Nazareth I. Attitudes to depression and its treatment in primary care. Psychol Med. 2007;37:1239–48. doi: 10.1017/S0033291707000931. [DOI] [PubMed] [Google Scholar]
- 8.Araya R, Lewis GH, Rojas G, Mann AH. “Patient knows best”-detection of common mental disorders in Santiago, Chile: cross sectional study. Bmj. 2001;322:79–81. doi: 10.1136/bmj.322.7278.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maginn S, Boardman AP, Craig TK, et al. The detection of psychological problems by General Practitioners--influence of ethnicity and other demographic variables. Soc Psychiatry Psychiatr Epidemiol. 2004;39:464–71. doi: 10.1007/s00127-004-0751-7. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg E, Lussier MT, Beaudoin C, et al. Determinants of the diagnosis of psychological problems by primary care physicians in patients with normal GHQ-28 scores. Gen Hosp Psychiatry. 2002;24:322–7. doi: 10.1016/s0163-8343(02)00197-4. [DOI] [PubMed] [Google Scholar]
- 11.Tylee A, Jones R. Managing depression in primary care. Bmj. 2005;330:800–1. doi: 10.1136/bmj.330.7495.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wittchen HU, Hofler M, Meister W. Prevalence and recognition of depressive syndromes in German primary care settings: poorly recognized and treated? Int Clin Psychopharmacol. 2001;16:121–35. doi: 10.1097/00004850-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 13.McCall L, Clarke DM, Rowley G. A questionnaire to measure general practitioners’ attitudes to their role in the management of patients with depression and anxiety. Aust Fam Physician. 2002;31:299–303. [PubMed] [Google Scholar]
- 14.Botega N, Mann AH, Blizard R, Wilkinson G. General practitioners and depression - First use of the Depression Attitude Questionnaire. International Journal of Methods in Psychiatric Research. 1992;2:169–180. [Google Scholar]
- 15.Haddad M, Walters P, Tylee A. District nursing staff and depression: a psychometric evaluation of Depression Attitude Questionnaire findings. Int J Nurs Stud. 2007;44:447–56. doi: 10.1016/j.ijnurstu.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Kerr M, Blizard R, Mann A. General practitioners and psychiatrists: comparison of attitudes to depression using the depression attitude questionnaire. Br J Gen Pract. 1995;45:89–92. [PMC free article] [PubMed] [Google Scholar]
- 17.Botega NJ, Silveira GM. General practitioners attitudes towards depression: a study in primary care setting in Brazil. Int J Soc Psychiatry. 1996;42:230–7. doi: 10.1177/002076409604200307. [DOI] [PubMed] [Google Scholar]
- 18.King M, Davidson O, Taylor F, et al. Effectiveness of teaching general practitioners skills in brief cognitive behaviour therapy to treat patients with depression: randomised controlled trial. Bmj. 2002;324:947–50. doi: 10.1136/bmj.324.7343.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dowrick C, Gask L, Perry R, et al. Do general practitioners’ attitudes towards depression predict their clinical behaviour? Psychol Med. 2000;30:413–9. doi: 10.1017/s0033291799001531. [DOI] [PubMed] [Google Scholar]
- 20.Ross S, Moffat K, McConnachie A, et al. Sex and attitude: a randomized vignette study of the management of depression by general practitioners. Br J Gen Pract. 1999;49:17–21. [PMC free article] [PubMed] [Google Scholar]
- 21.Butler M, Quayle E. Training primary care nurses in late-life depression: knowledge, attitude and practice changes. International Journal of Older People Nursing. 2007;2:25–35. doi: 10.1111/j.1748-3743.2007.00054.x. [DOI] [PubMed] [Google Scholar]
- 22.Haddad M, Plummer S, Taverner A, et al. District nurses’ involvement and attitudes to mental health problems: a three-area cross-sectional study. J Clin Nurs. 2005;14:976–85. doi: 10.1111/j.1365-2702.2005.01196.x. [DOI] [PubMed] [Google Scholar]
- 23.Payne F, Harvey K, Jessopp L, et al. Knowledge, confidence and attitudes towards mental health of nurses working in NHS Direct and the effects of training. J Adv Nurs. 2002;40:549–59. doi: 10.1046/j.1365-2648.2002.02413.x. [DOI] [PubMed] [Google Scholar]
- 24.Waller R, Hillam J. Assessment of depression in older medical inpatients: practice, attitudes and the effect of teaching. Aging and Mental Health. 2000;4:275–277. [Google Scholar]
- 25.Cape J, Morris E, Burd M, Buszewicz M. Complexity of GPs’ explanations about mental health problems: development, reliability, and validity of a measure. Br J Gen Pract. 2008;58:403–8. 410. doi: 10.3399/bjgp08X299281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lecrubier Y, Boyer P, Lepine J, Weiller E. Results from the Paris Centre. In: Ustun TB, Sartorius N, editors. Mental Illness in General Health Care. An International Study. Chichester: John Wiley & Sons; 1995. [Google Scholar]
- 27.Norton J, De Roquefeuil G, Boulenger JP, et al. Use of the PRIME-MD Patient Health Questionnaire for estimating the prevalence of psychiatric disorders in French primary care: comparison with family practitioner estimates and relationship to psychotropic medication use. Gen Hosp Psychiatry. 2007;29:285–93. doi: 10.1016/j.genhosppsych.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Norton J, David M, Boulenger JP. General Practitioners are bearing an increasing burden of the care of common mental disorders in France. Eur J Psychiat. 2007;21:63–70. [Google Scholar]
- 29.Rapport de l’enquête 2000 du Réseau de Promotion pour la Santé Mentale dans les Yvelines Sud. La Lettre de Promotion Santé Mentale Yvelines Sud; 2003. Réseau de Promotion pour la Santé Mentale 78; p. 4. [Google Scholar]
- 30.Ministère de la Santé et des Solidarités. Arrêté du 13 juillet 2006 portant l’homologation des règles de validation de la formation médicale continue. Journal Officiel de la République Française. 2006 [Google Scholar]
- 31.Deehan A, Templeton L, Taylor C, et al. The effect of cash and other financial inducements on the response rate of general practitioners in a national postal study. Br J Gen Pract. 1997;47:87–90. [PMC free article] [PubMed] [Google Scholar]
- 32.Templeton L, Deehan A, Taylor C, et al. Surveying general practitioners: does a low response rate matter? Br J Gen Pract. 1997;47:91–4. [PMC free article] [PubMed] [Google Scholar]
- 33.DREES. Les médecins: estimations au 1er janvier 2007. Vol. 2007. Ministère de l’Emploi et de la Solidarité; Aout-Sep. 2007. [Google Scholar]
- 34.Thornett AM, Pickering RM, Willis T, Thompson C. Dowrick et al. found no relationship between the scores on the Depression Attitude Questionnaire and GPs’ ability to identify depressed individuals in the surgery. Psychol Med. 2001;31:181. doi: 10.1017/s0033291799003190. [DOI] [PubMed] [Google Scholar]
- 35.Linden M, Lecrubier Y, Bellantuono C, et al. The prescribing of psychotropic drugs by primary care physicians: an international collaborative study. J Clin Psychopharmacol. 1999;19:132–40. doi: 10.1097/00004714-199904000-00007. [DOI] [PubMed] [Google Scholar]
- 36.Hull SA, Aquino P, Cotter S. Explaining variation in antidepressant prescribing rates in east London: a cross sectional study. Fam Pract. 2005;22:37–42. doi: 10.1093/fampra/cmh712. [DOI] [PubMed] [Google Scholar]
- 37.Ustun TB, Sartorius N, editors. An International Study. Chichester: John Wiley & Sons; 1995. Mental Illness in General Health Care. [Google Scholar]
- 38.Verger P. Déterminants de l’hétérogénéité des pratiques de prise en charge des problèmes de santé mentale en médecine de ville: étude des prescriptions d’antidépresseurs par les médecins généralistes de la région Provence-Alpes-Côte d’Azur (PACA). Colloque “Représentations des troubles psychiques, pratiques de soins et vécu des malades”; Paris. 4 décembre 2006; 2006. [Google Scholar]
- 39.Kisely S, Duerden D, Shaddick S, Jayabarathan A. Collaboration between primary care and psychiatric services: does it help family physicians? Can Fam Physician. 2006;52:876–7. [PMC free article] [PubMed] [Google Scholar]
- 40.Andersson SJ, Lindberg G, Troein M. What shapes GPs’ work with depressed patients? A qualitative interview study. Fam Pract. 2002;19:623–31. doi: 10.1093/fampra/19.6.623. [DOI] [PubMed] [Google Scholar]
- 41.National Clinical Practice Guideline 90. London: National Institute for Health and Clinical Excellence. National Health Service; 2009. The NICE Guideline on the Treatment and Management of Depression in Adults. [Google Scholar]
- 42.WHO. Investing in Mental Health. Geneva: World Health Organisation; 2003. [Google Scholar]
- 43.Croudace T, Evans J, Harrison G, et al. Impact of the ICD-10 Primary Health Care (PHC) diagnostic and management guidelines for mental disorders on detection and outcome in primary care. Cluster randomised controlled trial. Br J Psychiatry. 2003;182:20–30. doi: 10.1192/bjp.182.1.20. [DOI] [PubMed] [Google Scholar]
- 44.Thompson C, Kinmonth AL, Stevens L, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet. 2000;355:185–91. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 45.Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003;289:3145–51. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- 46.Dietrich AJ, Oxman TE, Williams JW, Jr, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004;329:602. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Upshur C, Weinreb L. A survey of primary care provider attitudes and behaviors regarding treatment of adult depression: what changes after a collaborative care intervention? Prim Care Companion J Clin Psychiatry. 2008;10:182–6. doi: 10.4088/pcc.v10n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chew-Graham CA, Lovell K, Roberts C, et al. A randomised controlled trial to test the feasibility of a collaborative care model for the management of depression in older people. Br J Gen Pract. 2007;57:364–70. [PMC free article] [PubMed] [Google Scholar]
- 49.Richards DA, Lovell K, Gilbody S, et al. Collaborative care for depession in UK primary care: a randomized controlled trial. Psychol Med. 2008;38:279–87. doi: 10.1017/S0033291707001365. [DOI] [PubMed] [Google Scholar]
- 50.Nutting PA, Gallagher K, Riley K, et al. Care management for depression in primary care practice: findings from the RESPECT-Depression trial. Ann Fam Med. 2008;6:30–7. doi: 10.1370/afm.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Jong FJ, van Steenbergen-Weijenburg KM, Huijbregts KM, et al. The Depression Initiative. Description of a collaborative care model for depression and of the factors influencing its implementation in the primary care setting in the Netherlands. Int J Integr Care. 2009;9:e81. doi: 10.5334/ijic.313. [DOI] [PMC free article] [PubMed] [Google Scholar]


