Abstract
Background
Alcoholics Anonymous (AA) began as a male organization, but about one third is now female. Studies have found that women participate at least as much as men and benefit equally from AA, but it is unclear whether women benefit from AA in the same or different ways as men. This study tested whether gender moderated the mechanisms through which AA aids recovery.
Methods
A cohort study of alcohol dependent adults (N=1,726; 24% female; Project MATCH) was assessed on AA attendance during treatment; with mediators at 9 months; outcomes (Percent Days Abstinent [PDA] and Drinks per Drinking Day [DDD]) at 15 months. Multiple mediator models tested whether purported mechanisms (i.e., self-efficacy, depression, social networks, spirituality/religiosity) explained AA's effects differently for men and women controlling for baseline values, mediators, treatment, and other confounders.
Results
For PDA, the proportion of AA's effect accounted for by the mediators was similar for men (53%) and women (49%). Both men and women were found to benefit from changes in social factors but these mechanisms were more important among men. For DDD, the mediators accounted for 70% of the effect of AA for men and 41% for women. Again, men benefitted mostly from social changes. Independent of AA's effects, negative affect self-efficacy was shown to have a strong relationship to outcome for women but not men.
Conclusions
The recovery benefits derived from AA differ in nature and magnitude between men and women and may reflect differing needs based on recovery challenges related to gender-based social roles and drinking contexts.
Keywords: Alcoholics Anonymous, gender, recovery, addiction treatment, 12-step, women
1. INTRODUCTION
In most developed nations, alarming increases in the prodigious economic, social, and medical burden attributable to alcohol and other drug misuse has opened the door for greater coordination among formal and informal intervention and support services to help reduce harm, curb health care costs, and enhance long term recovery (Bouchery et al., 2011; Centers for Disease Control and Prevention, 2012; Office of National Drug Control Policy, 2011; U.S. Department of Justice, 2011; UK Drug Strategy, 2010). Significant increases in the quantity and quality of professional addiction treatment has been paralleled by increases in the spread of addiction mutual-help organizations (Humphreys, 2004; Kelly et al., in press, 2008). The most ubiquitous of these is Alcoholics Anonymous (AA).
The most recent areas of investigation have been in examining AA's mechanisms of behavior change as well as potential moderators of its effects; specifically, increasing research has been conducted on the psychological and social change processes that are mobilized by AA and which subsequently lead to recovery (i.e., mediator analyses); and whether particular subgroups benefit more or less from AA (i.e., moderator analyses) (Kelly et al., 2012a, 2009). Research has also begun to combine these two types of analytic questions to examine whether the mechanisms through which AA works depend on certain characteristics of patients (i.e., investigations of “moderated mediation” (Muller et al., 2005), such as the degree of alcohol involvement and impairment (Kelly et al., 2012a) and age (Blonigen et al., 2011). Kelly and colleagues (2012a), for example, found that, compared to less alcohol-impaired patients, more alcohol-impaired patients benefitted from AA more through decreases in depression symptoms and increases in spirituality/religious practices, and Blonigen and colleagues (2011) found that impulsivity was a mediator of AA's effects on subsequent outcomes for younger, but not older, patients. Another important characteristic of patients that is particularly intriguing when it comes to AA is gender, as the appropriateness of AA for women has been questioned.
About one third of AA members are women, placing them in minority status in a predominantly male organization (Alcoholics Anonymous, 2012). Moreover, during AA's formative years, the organization was almost entirely composed of men. Consequently, it has remained somewhat unclear whether a program derived from its successful application to male alcohol dependent cases, would cater to and be as effective for women. Also, much of the literature on which AA is based is written using the male pronoun (i.e., “he”, “him” “his”) when describing the “alcoholic” (Alcoholics Anonymous, 1939, 1952), tacitly alienating women potentially further. In addition, some have objected to the 12-step focus on “powerlessness” espoused in step one of the AA program (Powell, 1987), contending that this emphasis may further disenfranchise an already disenfranchised group. Although, “powerlessness” stated in step one refers to alcohol and not other aspects of individuals’ lives (i.e., “We admitted we were powerless over alcohol- that our lives had become unmanageable”), this concern has lingered nonetheless (Del Boca et al., 2001).
These concerns, however, have not been borne out empirically. Studies that have examined whether women engage and benefit from AA as much as men have found that women become as, or more, involved, as their male counterparts, and also benefit as much or more than men (Del Boca et al., 2001; Humphreys et al., 1994; Kaskutas et al., 2008; Krentzman et al., 2012; Moos et al., 2006; Timko et al., 2002; Witbrodt et al., 2011, 2010). Unclear, however, is whether women benefit from AA in the same or different ways as men. For example, recent findings suggest AA leads to enhanced alcohol outcomes by mobilizing recovery-supportive social changes in the networks of its members (i.e., leads to increases in pro-abstainers and decreases in pro-drinkers), and by increasing attendees’ confidence in their ability to remain abstinent in high risk social situations or when experiencing negative affect, such as depression (Kelly et al., 2012a, 2010). As noted above, AA participation has been shown also to lead to better outcomes by reducing depression symptoms and by increasing spiritual practices, particularly for more severely alcohol-impaired individuals (Kelly et al., 2012a, 2010, 2011a; Krentzman et al., 2012; Zemore, 2007). However, given gender differences in the prevalence of depression among men and women (Maier et al., 1999; Piccinelli and Wilkinson, 2000), and differing gender-related social roles (e.g., motherhood, homemaking; Cha, 2010; Nolen-Hoeksema, 2004; Wilsnack and Wilsnack, 1997), alcohol use contexts (e.g., drinking less in bars; Paradis, 2011), and work patterns (Kuntsche et al., 2009, 2011) which may present different stressors and recovery needs, it is currently unclear whether the similar, or greater, AA-related recovery benefits observed among women are derived through the same mechanisms, and if so, to the same degree, or through completely different mechanisms. Greater knowledge in this regard would help reveal the nature of any gender-specific benefits related to AA participation and also inform the broader field about the mechanisms through which men and women may recover from alcohol addiction (Potenza et al., 2012).
With the aid of a uniquely large clinical sample (N=1,726; Project MATCH Research Group, 1993), we conducted state of the art multiple mediator analysis to examine this question of whether AA benefits men and women differently (Muller et al., 2005). Based on prior mediational findings (Kelly et al., 2012a, 2009), we examined six mediators of AA's effects on alcohol use outcomes: changes in pro-drinking and pro-abstaining social network ties; changes in abstinence self-efficacy in coping with risky social situations and when experiencing negative affect; changes in depression symptoms; and, changes in spiritual practices. We did not have strong directional hypotheses about gender differences. However, based on the relatively higher prevalence of depression among women than men (Piccinelli et al., 2000) and differences in social roles and drinking contexts (Weich et al., 1998), we anticipated that AA may operate differently across gender lines on these mediatiors.
2. METHODS
2.1. Participants
Participants were 1,726 treatment-seeking adults suffering from alcohol use disorder (AUD) who participated in 12 weeks of outpatient treatment (24% female; n=419; Project MATCH Research Group, 1993).
Project MATCH inclusion criteria were: current DSM-III-R AUD diagnosis; alcohol as principal drug of misuse; drinking during 3 months prior to study; 18 or older; minimum sixth grade reading level. Exclusion criteria were: current DSM-III-R diagnosis of dependence on sedative-hypnotics, stimulants, cocaine or opiates; intravenous drug use in prior 6 months; danger to self/others; probation/parole requirements that might interfere with participation; risk of residential instability; inability to identify at least one “locator” person to assist tracking; psychosis/organic impairment; involvement in alternative treatment other than MATCH (i.e., > 6 hours, except for self-help groups).
2.2. Procedure
Subjects were randomly assigned to 1 of 3 individually-delivered, psychosocial interventions: cognitive behavioral therapy (CBT; Kadden et al., 1992), motivational enhancement therapy (MET; Miller et al., 1992), and 12-step facilitation therapy (TSF; Nowinski et al., 1992). Participants were reassessed at 3, 6, 9, 12, and 15 months following study intake, with follow-up rates over 90%. More complete details can be found elsewhere (Project MATCH Research Group, 1997). This study focused on baseline, 3-, 9-, and 15-month follow-ups because only these time points contained the necessary variables needed for our fully lagged analyses.
2.3. Measures
2.3.1 Alcohol Use
Alcohol consumption was assessed using the Form 90 (Miller et al., 1994), which combines an interview procedure with calendar-based and drinking pattern estimates. Two drinking outcomes were based on the past 90 days: percent days abstinent (PDA) and number of drinks per drinking day (DDD).
2.3.2 Alcoholics Anonymous Attendance
AA attendance was also assessed using the Form 90, which captured the number of AA meetings attended during the past 90 days at intake and 3, 9, and 15 months. The proportion of days attending AA was created by dividing the number of days attended by total number of days in period.
2.3.3. Self-efficacy
The Alcohol Abstinence Self-Efficacy Scale (DiClemente et al., 1994) is a 20-item scale that assesses self-efficacy using four subscales (Negative Affect, Social/Positive, Physical and Other Concerns, Withdrawal and Urges). Each item is rated on a 5-point Likert scale (“not at all confident” to “extremely confident”). In this study, two subscales were included (“Negative Affect”: men α=0.92 women; α=0.92; “Social/Positive”: men α=0.91 women α=0.89), shown to be mediators of the effect of AA attendance on alcohol outcomes (Owen et al., 2003). Negative affect assesses an individual's confidence in their ability to successfully abstain when experiencing negative emotions; social self-efficacy assesses confidence in an individual's ability to abstain when encountering a high risk social drinking situation.
2.3.4 Spiritual/Religious practices
Spirituality/religiousness was assessed with the religious background and behavior instrument (RBB; Connors et al., 1996). Total scores were based on self-reported religious status on a 5-point scale [“I do not believe in God,” (Atheist) coded “0,” “I believe we can't really know about God” (Agnostic) coded “1,” through “Unsure,” coded “2,” “I believe in God, but I'm not religious (Spiritual) coded “3,” “I believe in God and practice religion (Religious), coded “4”], and past 90-day religious and spiritual practices (i.e., ”thought about God”, “prayed”, “meditated”, “attended worship services”, “read or studied scriptures/ holy writings”, and “had direct experiences of God”), rated on 8-point Likert-scale (“never” to “more than once a day”). As in previous research (Yung, 2008), RBB questions pertaining to lifetime religious practices were excluded from our total score, because this study examined changes in spirituality/religiousness.
2.3.5 Depression
Depression symptoms were assessed using the Beck Depression Inventory (BDI; Beck et al., 1961). This 21-item measure assesses past-week depression symptom severity; higher values indicate greater depression severity. The measure is well established psychometrically, with good internal consistency, test-retest stability and construct validity (Beck et al., 1988; men α=0.89, women α=0.88).
2.3.6 Social Networks
The Important People and Activities Instrument (IPA; Clifford et al., 1991) characterized patients’ social networks on two dimensions: “pro-drinking” and “pro-abstinence”. In the IPA, patients name the four most important people of the past 6 months, and rate how each reacts to their abstinence or drinking. A person was coded as “pro-abstinence” if s/he either encouraged abstinence or discouraged drinking, or both. A person was coded as “pro-drinking” if s/he either encouraged drinking or discouraged abstinence, or both. The number of each type of network members was summed to produce a scale range 0–4. Someone could list four people all neutral about drinking, in which case they would get a count of 0 for both measures. Based on previous research (Kelly et al., 2011a), these two variables were chosen as the most salient descriptors of social networks, as they mediated relationship between AA and alcohol outcomes most consistently.
2.3.7 Baseline Characteristics
At intake, demographic information and the number of prior alcohol treatments were recorded. Gender, marital status, and employment status were coded binary variables; race was coded as a 3-level categorical variable dummy-coded in the SEM (see Table 1). Compared to men, women tended to be more depressed, and had fewer prior alcohol treatments, a higher PDA, a lower number of DDD, lower negative affect self-efficacy, and higher religiosity (Table 1). The majority of participants (94.6%) reported 4 or fewer prior alcohol treatments, but some reported up to 40. To reduce the influence of these outliers, the number of prior alcohol treatments was capped at four (range 0-4).
Table 1.
Project MATCH sample description at Intake
| Men (n=1,307) |
Women (n=419) |
t / χ2 | |||
|---|---|---|---|---|---|
| mean / % | SD / n | mean / % | SD / n | ||
| Demographics | |||||
| Age | 40.3 | 10.8 | 41.3 | 11.6 | 0.16 |
| Race (%) | 1.03 | ||||
| White | 81.9 | 1071 | 81.9 | 343 | |
| Hispanic | 9.5 | 124 | 10.7 | 45 | |
| Black | 8.6 | 112 | 7.4 | 31 | |
| Marital Status (% married / cohabiting) | 36.6 | 478 | 29.6 | 124 | 6.80** |
| Employment Status (% full-time) | 52.6 | 687 | 40.1 | 168 | 19.73** |
| Intake Clinical Descriptors | |||||
| Percent of days abstinent (PDA) | 29.7 | 29.4 | 34.7 | 31.5 | -2.77** |
| Drinks per drinking day | 18.0 | 10.9 | 12.3 | 8.2 | 12.17** |
| # of prior Alcohol Treatments (max=4) | 1.1 | 1.3 | 0.9 | 1.2 | 3.57** |
| AA attendance | |||||
| (BL) Ever attended AA in past 3-months | 26.8 | 350 | 25.5 | 107 | 0.26 |
| (BL) If attended, % of days | 13.5 | 17.8 | 14.7 | 19.3 | -0.63 |
| (3-mo) Ever attended AA in past 3-months | 63.2 | 797 | 59.3 | 239 | 1.92 |
| (3-mo) If attended, % of days | 33.0 | 26.9 | 33.1 | 30.0 | -0.03 |
| Intake levels of mediators | |||||
| Self-Efficacy (NA) | 2.9 | 1.1 | 2.7 | 1.1 | 3.54** |
| Self-Efficacy (Soc) | 2.9 | 1.1 | 2.9 | 1.1 | 1.38 |
| Religiosity | 23.7 | 9.0 | 24.8 | 9.1 | -2.20* |
| Depression† | 9.7 | 7.9 | 11.8 | 9.0 | -4.20** |
| SocNet: pro-abst. | 2.9 | 1.2 | 2.8 | 1.2 | 1.32 |
| SocNet: pro-drk. | 1.2 | 1.2 | 1.0 | 1.1 | 1.92 |
Note:
p < 0.05
p < 0.01
Satterthwaite t-test for unequal variances was used; self-efficacy (NA) and self-efficacy (Soc) = participants confidence in abstaining from alcohol when experiencing negative emotions or when faced with high risk social situations, respectively. SocNet: pro-abst, and SocNet: pro-drk = number of pro-abstainers and pro-drinkers, respectively, that participants reported in their social network.
2.4. Analytic Strategy
2.4.1. Data Preparation
The dependent variables (i.e., PDA and DDD) and the independent AA attendance variable were transformed prior to analyses (PDA/ arcsine transformed; DDD/ square root transformed, and AA attendance/ log transformed).
2.4.2 Mediational Analyses
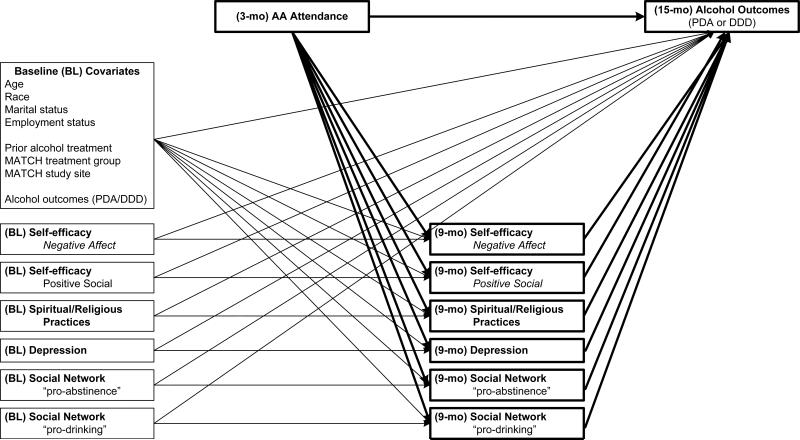
To avoid temporal confounding among the predictor variable (i.e., AA attendance), the mediators, and the outcome variables, and thus enhance causal inference (Kazdin et al., 2003), we employed a fully lagged mediational design. We examined AA attendance during Project MATCH treatment (months 0-3), mediators at 9 month follow-up, and alcohol outcomes (PDA; DDD) at 15 month follow-up (Figure 1). In addition, to help rule out other causes of change in the mediators and outcomes (i.e., other than AA), we controlled also for demographic variables, MATCH treatment assignment and treatment program site, prior alcohol treatment, and the baseline levels of the outcome and mediator variables.
Figure 1.
Path diagram of the mediational model fit for men and women. Baseline covariates are included to help rule out other causes of change in the mediators and outcomes (i.e., other than AA).
We used a structural equation modeling multi-group approach to test for gender differences in the mediational paths in the previously tested multiple mediator model (Kelly et al., 2012a). That is, we fit the multiple mediator model (Figure 1) simultaneously but separately for men and women. We had considered including interaction terms (i.e., each of the six mediators x gender) in a single model, but this created even greater complexity to an already complex analysis and was overly cumbersome. Thus we opted for the less complicated separate models. To assess the overall equivalence of the model for men and women, we first fit a model in which we constrained all parameter estimates to be equal for men and women, and compared it to a model in which all parameter estimates could differ. Then, because we were interested in gender differences in specific parameter estimates, we used the second model to conduct planned comparisons of mediational paths.
Based on this second model, we tested mediation separately for men and women using the product-of-coefficients approach (Sobel, 1986, 1982). This approach extends directly to multiple mediator models, where the total indirect effect is simply the sum of the mediator-specific indirect effects (Mackinnon, 2008; Preacher et al., 2008). Using equations provided by Mackinnon (2008), we calculated the specific indirect effects, where we constructed 95% confidence intervals using the Monte Carlo Method for Assessing Mediation (MCMAM; Mackinnon et al., 2004), and implemented them using the interactive tool created by Selig and Preacher (Selig et al., 2008). We fitted models for both alcohol outcomes (i.e., PDA and DDD) using SAS 9.3 PROC CALIS.
2.4.3. Missing Data
Missing data were observed for 3.6% at 3-month, 9.5% (for social networks) to 13.6% (for self-efficacy) at 9-month, and 9.1% at 15-month. To address missing data, the maximum likelihood estimation approach was used (Schafer et al., 2002). We first estimated the variance-covariance matrix using all available data (using the iterative expectation-maximization (EM) algorithm [SAS 9.3 Proc MI]), and then used this matrix for fitting models (Figure 1).
3. RESULTS
3.1. Gender Differences in Mediational Relationships
Prior to mediational analyses, we tested if there was an overall effect of AA attendance on alcohol outcomes. Regression analyses indicated that this effect was significant for men and women for both alcohol outcomes (PDA in men: t=97.3, p < .001; DDD in men: t=84.4, p < .001; PDA in women: t=30.4, p < .001; DDD in men: t=25.7, p < .001). For both PDA and DDD, the direct effect of AA attendance on alcohol outcomes was not significantly different for men and women (χ2(1)=0.2, p > .05 and χ2(1)=1.5, p > .05, respectively), nor was the effect of AA attendance on the mediators (χ2(6)=4.6, p > .05 and χ2(1)=4.3, p > .05, respectively). There were, however, differences in the effect of the mediators on the alcohol outcomes (χ2(6)=39.7, p < .01 and χ2(6)=43.2, p < .01, respectively), which were largely due to differences in self-efficacy. Here, the effect of self-efficacy in negative affect situations on alcohol outcomes was larger in women than men, while the reverse was true for self-efficacy in high risk social situations (see Table 2).
Table 2.
Sex differences in the mediational paths
| Percent of Days Abstinent (PDA) |
Drinks per Drinking Day (DDD) |
||||||
|---|---|---|---|---|---|---|---|
| b(♂) - b(♀) | df | χ 2 | b(♂) - b(♀) | df | χ 2 | ||
| Direct effect: AA attendance predicting alcohol outcomes | 1 | 0.2 | 1 | 1.5 | |||
| AA attendance | → PDA/DDD | 0.00 | 1 | 0.2 | 0.03 | 1 | 1.5 |
| Mediational path: AA attendance predicting mediators | 6 | 4.6 | 6 | 4.3 | |||
| AA attendance | → Self-Efficacy (NA) | -0.02 | 1 | 0.7 | -0.02 | 1 | 0.9 |
| AA attendance | → Self-Efficacy (Soc) | 0.00 | 1 | 0.0 | 0.00 | 1 | 0.0 |
| AA attendance | → Religiosity | 0.17 | 1 | 2.0 | 0.16 | 1 | 1.6 |
| AA attendance | → Depression | 0.00 | 1 | 0.0 | 0.07 | 1 | 0.2 |
| AA attendance | → SocNet: pro-abst. | 0.02 | 1 | 0.9 | 0.02 | 1 | 0.8 |
| AA attendance | → SocNet: pro-drk. | -0.02 | 1 | 0.9 | -0.02 | 1 | 0.8 |
| Mediational path: Mediators predicting alcohol outcomes | 6 | 39.7** | 6 | 43.2** | |||
| Self-Efficacy (NA) | → PDA/DDD | -0.07 | 1 | 14.7** | 0.24 | 1 | 14.2** |
| Self-Efficacy (Soc) | → PDA/DDD | 0.06 | 1 | 9.4** | -0.35 | 1 | 27.3** |
| Religiousness | → PDA/DDD | -0.01 | 1 | 3.5 | 0.00 | 1 | 0.0 |
| Depression | → PDA/DDD | 0.01 | 1 | 5.6 | -0.01 | 1 | 0.9 |
| SocNet: pro-abst. | → PDA/DDD | 0.02 | 1 | 1.0 | -0.01 | 1 | 0.0 |
| SocNet: pro-drk. | → PDA/DDD | 0.03 | 1 | 2.2 | -0.06 | 1 | 0.8 |
Note:
* p < 0.05
p < 0.01.
A positive difference between parameter estimates indicates that the effect was stronger for men than for women; a negative difference indicates that the effect was stronger for women than for men.
3.2. Multiple Mediation Effects for Men and Women
Mediation through the multiple mediators was statistically significant for both outcomes in both men and women (z=7.03 for men PDA, z=3.80 for women PDA, z=-6.21 for men DDD, and z=-3.29 for women DDD, all p < .05). The proportion of the total effect of AA on alcohol use outcomes accounted for by the six mediators ranged from 40.7% (DDD for women) up to 70.0% (DDD for men; Table 3). Direct effects were not always significant given indirect effects, but the total effect of AA attendance on drinking outcomes was. The total effect (i.e., direct and indirect) tended to be larger for women than men, for both PDA (R2=0.36 vs. 0.30) and DDD (R2=0.29 vs. 0.20). Not all of the specific mediators were significant (Table 5). To better understand the nature of the non-significant mediations, we examined the standardized parameter estimates of the mediational paths (Table 5) together with the tests of mediation of the specific mediators (Table 4).
Table 3.
Partioning of the standardized effect of AA on drinking outcome: Total, direct and indirect effects
| Drinking Outcome | Total | Direct | Indirect | |||
|---|---|---|---|---|---|---|
| Sample | EST | R2 | EST | % | EST | % |
| Percent of Days Abstinent | ||||||
| Men | 0.25** | 0.30 | 0.13** | 50.8% | 0.12** | 49.2% |
| Women | 0.22** | 0.36 | 0.11 | 47.5% | 0.12** | 52.5% |
| Drinks per Drinking Day | ||||||
| Men | -0.15** | 0.20 | -0.04 | 30.1% | -0.10** | 70.0% |
| Women | -0.25** | 0.29 | -0.15* | 59.4% | -0.10** | 40.7% |
Note:
p < 0.05
p < 0.01
Table 5.
Standardized path parameter estimates of the multiple mediator model
| Type of Path | Percent of Days Abstinent | Drinks per Drinking Day | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men (adj. n=1,166) | Women (adj. n=378) | Men (adj. n=1,166) | Women (adj. n=378) | ||||||||||
| Path | β | SE | t | β | SE | t | β | SE | t | β | SE | t | |
| Direct effect: AA predicting alcohol outcomes | |||||||||||||
| AA attendance | → PDA/DDD | 0.13 | 0.03 | 3.82* | 0.11 | 0.06 | 1.89 | -0.04 | 0.04 | -1.23 | -0.15 | 0.06 | -2.45* |
| Mediational path: AA predicting mediators | |||||||||||||
| AA attendance | → Self-Efficacy (NA) | 0.04 | 0.03 | 1.17 | 0.10 | 0.06 | 1.63 | 0.05 | 0.03 | 1.31 | 0.11 | 0.06 | 1.83 |
| AA attendance | → Self-Efficacy (Soc) | 0.15 | 0.03 | 4.44* | 0.14 | 0.06 | 2.49* | 0.15 | 0.03 | 4.54* | 0.15 | 0.06 | 2.48* |
| AA attendance | → Religiosity | 0.19 | 0.02 | 8.22* | 0.13 | 0.04 | 3.24* | 0.19 | 0.02 | 8.14* | 0.13 | 0.04 | 3.28* |
| AA attendance | → Depression | -0.07 | 0.03 | -2.12* | -0.07 | 0.06 | -1.18 | -0.07 | 0.03 | -2.16* | -0.10 | 0.06 | -1.70 |
| AA attendance | → SocNet: pro-abst. | 0.20 | 0.03 | 6.13* | 0.14 | 0.06 | 2.46* | 0.20 | 0.03 | 6.20* | 0.15 | 0.06 | 2.55* |
| AA attendance | → SocNet: pro-drk. | -0.16 | 0.03 | -4.84* | -0.10 | 0.06 | -1.69 | -0.16 | 0.03 | -4.85* | -0.11 | 0.06 | -1.76 |
| Mediational path: Predicting alc. outcomes | |||||||||||||
| Self-Efficacy (NA) | → PDA/DDD | 0.03 | 0.03 | 0.95 | 0.24 | 0.05 | 5.24* | -0.06 | 0.03 | -1.97* | -0.29 | 0.05 | -6.38* |
| Self-Efficacy (Soc) | → PDA/DDD | 0.28 | 0.03 | 11.01* | 0.13 | 0.05 | 2.93* | -0.26 | 0.03 | -9.35* | 0.00 | 0.05 | -0.02 |
| Religiousness | → PDA/DDD | 0.05 | 0.04 | 1.28 | 0.13 | 0.07 | 1.87 | -0.08 | 0.04 | -1.86 | -0.09 | 0.07 | -1.28 |
| Depression | → PDA/DDD | -0.01 | 0.03 | -0.48 | -0.15 | 0.05 | -3.20* | 0.12 | 0.03 | 3.94* | 0.21 | 0.05 | 4.32* |
| SocNet: pro-abst. | → PDA/DDD | 0.17 | 0.03 | 6.38* | 0.13 | 0.05 | 2.71* | -0.08 | 0.03 | -2.86* | -0.09 | 0.05 | -1.81 |
| SocNet: pro-drk. | → PDA/DDD | -0.21 | 0.03 | -7.86* | -0.28 | 0.04 | -6.72* | 0.12 | 0.03 | 4.24* | 0.19 | 0.05 | 4.16* |
Note: “adj. n” = avg no. participants with data for the 8 variables; not shown but included are baseline covariates (see Figure 1).
p < 0.05
Table 4.
Test of mediation for specific indirect (i.e., mediated) effects using the Product of Coefficients approach
| Alcohol Outcome Mediator | Men (adj. n=1,166) |
Women (adj. n=378) |
||||||
|---|---|---|---|---|---|---|---|---|
| EST | SE | 95% CI | %† | EST | SE | 95% CI | %† | |
| Percent of Days Abstinent (PDA) | ||||||||
| Self-Efficacy (NA) | 0.000 | 0.000 | [0.000 - 0.000] | 0.8% | 0.003 | 0.001 | [0.000 - 0.006] | 19.4% |
| Self-Efficacy (Soc) | 0.005 | 0.001 | [0.003 - 0.008]* | 34.9% | 0.002 | 0.001 | [0.000 - 0.005]* | 16.6% |
| Religiousness | 0.001 | 0.033 | [-0.001 - 0.003] | 7.9% | 0.002 | 0.037 | [0.000 - 0.005] | 14.2% |
| Depression | 0.000 | 0.009 | [0.000 - 0.001] | 0.7% | 0.001 | 0.018 | [0.000 - 0.004] | 8.6% |
| SocNet: pro-abst. | 0.004 | 0.001 | [0.003 - 0.006]* | 28.3% | 0.002 | 0.001 | [0.000 - 0.005]* | 15.3% |
| SocNet: pro-drk. | 0.004 | 0.001 | [0.002 - 0.006]* | 27.4% | 0.003 | 0.002 | [0.000 - 0.008] | 25.5% |
| Drinks per Drinking Day (DDD) | ||||||||
| Self-Efficacy (NA) | -0.001 | 0.003 | [-0.004 - 0.001] | 2.4% | -0.012 | 0.016 | [-0.026 - 0.001] | 32.7% |
| Self-Efficacy (Soc) | -0.018 | 0.013 | [-0.027 - -0.010]* | 39.0% | 0.000 | 0.001 | [-0.006 - 0.006] | 0.2% |
| Religiousness | -0.007 | 0.032 | [-0.014 - 0.000] | 14.6% | -0.004 | 0.039 | [-0.013 - 0.002] | 12.3% |
| Depression | -0.004 | 0.009 | [-0.008 - 0.000]* | 8.0% | -0.008 | 0.026 | [-0.018 - 0.001] | 20.9% |
| SocNet: pro-abst. | -0.008 | 0.004 | [-0.014 - -0.002]* | 16.6% | -0.005 | 0.006 | [-0.013 - 0.000] | 13.3% |
| SocNet: pro-drk. | -0.009 | 0.007 | [-0.015 - -0.004]* | 19.3% | -0.008 | 0.014 | [-0.018 - 0.001] | 20.8% |
Note: “adj. n” refers to average no. of participants with data for the 8 structural variables
% of total indirect effects attributable to specific mediators (can total >100%, if specific indirect effects in opposite directions
p < 0.05 based on 95% CIs using Monte Carlo Method for Assessing Mediation (MCMAM)(Mackinnon et al., 2004)
3.3. Mediational Effects on PDA
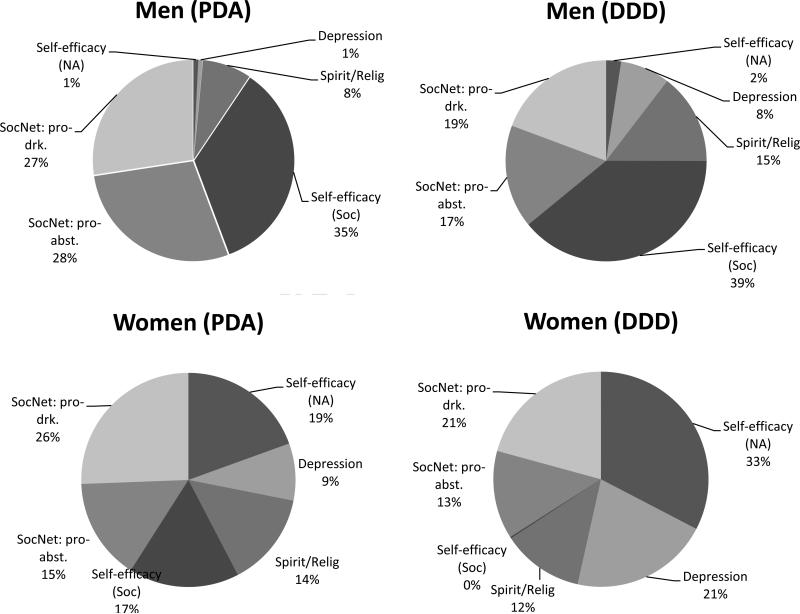
For PDA, greater self-efficacy in high-risk social situations and a higher number of pro-abstinence social network members were significant mediators of lower PDA for both men and women. These two mediators appeared to be more influential in men than women, as indicated by the higher percentage of the overall effect that was mediated in men (Figure 2). A higher number of pro-drinking social network members was a similarly important mediator of lower PDA in men and women, though it was only statistically significant in men. Inspection of the standardized path estimates (Table 5) revealed that in women, the effect of AA attendance on this mediator was not significant, while the effect of pro-drinking social network members on PDA was, in both men and women.
Figure 2.
The unique proportion of each mediators’ effects in expalining AA's influence on subsequent alcohol use outcomes.
The mediation through self-efficacy in negative affect situations accounted for 19.4% of the total effect in women (vs. 0.8% in men) though again the mediation was not statistically significant. Here as well, the effect of AA on this mediator was not significant, but the effect of self-efficacy in negative social situations on PDA was. Indeed, it was among the largest effects for women (β=0.24), second only to the number of pro-drinking social network members (β =-0.28), while largely absent in men (β =0.03), as suggested previously by the significant gender difference test (Table 2).
3.4. Mediational Effects on DDD
For DDD, significant mediation of fewer DDD occurred through higher self-efficacy in high risk social situations (39%), a lower number of pro-drinking (19%) and a higher number of pro-abstinence (17%) social network members and lower depression (8%) in men. In women, none of the specific mediators were statistically significant. In women, either the effect of AA on the mediator was present, or the effect of the mediator on DDD, but not both. Judging by the percentages of the effect of AA attendance that was mediated by each mediator (Table 4), it appears as though women had similar (though not statistically significant) effects for the social network mediators as men. That is to say, in both men and women an increase in social network members advocating abstinence and a reduction of social network members advocating drinking was related to a reduction in DDD. Men and women differed in the effects of self-efficacy on DDD. Similar to the findings regarding PDA, but more pronounced for DDD, self-efficacy in positive social situations was a powerful mediator in men (39% of the mediation), but absent in women (0.2%). Meanwhile, self-efficacy in negative affect situations was important for women (32.7%) but not men (2.4%).
4. DISCUSSION
With the aid of a uniquely large, and geographically diverse, U.S. clinical sample of adults suffering from alcohol use disorder, and employing state of the art methodology to examine multiple mediators simultaneously, this study examined whether the mechanisms through which AA aids recovery from alcohol dependence differed by gender. In line with prior studies, we found significant independent beneficial effects of AA attendance on alcohol use outcomes that did not differ between men and women. Also, the effect of AA on the mediators did not differ by gender. Differences were found, however, in the significance and magnitude of some of the full tested mediational pathways suggesting that men and women seeking recovery may benefit from and/or use AA differently.
In terms of the ways in which AA helped increase abstinence, significant mediation was found for both men and women through social self-efficacy and pro-abstainer pathways. As shown in Table 4 and illustrated in Figure 2, however, the magnitude of these effects differed, with a substantially larger proportion of AA's effect accounted for by these mediators for men (90.6%) than women (57.4%). Thus, while AA appears to work across both genders by increasing attendees’ confidence in their ability to abstain in high risk social situations and by increasing the number of abstainers in their social networks, the substantial difference in magnitude could be explained by differences in relapse risks that are related to gender-based social roles and drinking contexts (e.g., Cha, 2010; Nolen-Hoeksama, 2004). AA may help men more by facilitating reductions in high risk drinkers in favor of new sober friends while simultaneously boosting ability to cope with what may be more commonly encountered “male-specific” high risk situations (e.g., when attending or watching sporting events at friends’ homes; Paradis, 2011). While these mechanisms also appear to be some of the ways in which women benefit from AA, for women these risky social contexts may be less frequently encountered, and, consequently, women do not benefit as much in this way.
In terms of the full mediational paths through which AA helped reduce drinking intensity, there were differences found between men and women. For men, AA attendance led to significant reductions in heavier drinking by increasing social abstinence self-efficacy, decreasing depression, increasing pro-abstinent network members, and by reducing pro-drinking network members. However, for women, none of the full mediational paths were significant. This was either because AA did not affect the mediator (negative affect self-efficacy, depression, pro-drinkers), or because the mediator did not predict drinking intensity (social self-efficacy, spirituality/religiousness, pro-abstainers) for women. As with the findings for PDA, the majority of the effect of AA on reducing drinking intensity for men was by facilitating recovery-supportive social- changes and may reflect the greater need for men to find new ways of coping with common social risks. Indeed, the large meditational effect found for social self-efficacy for men (39%), was strikingly non-existent as a mediator for women, having no relationship to DDD (0.2%). Women at this life-stage (i.e., between 30-50 yrs) may be more likely to drink outside of social contexts (e.g., at home alone), obviating the need for socially-relevant abstinence self-efficacy.
Related to this pattern of findings was that while the total mediated effect of the six mediators was similar across men and women for PDA, the six variables explained almost double the amount of AA's effect on reducing DDD for men (70%) than for women (41%). This indicates that other AA mechanisms not specified in the current model are playing an important role in reducing women's levels of drinking intensity. These will need to be delineated and tested in future research.
Despite not being a mediational pathway (AA was not significantly related to it) noteworthy was the importance of negative affect self-efficacy on both abstinence and drinking intensity among women, but not men. Women's alcohol use outcomes appear to be strongly related to their ability to cope with negative affect. Such gender-based differences are reflected too in the differences in the meditational effects on abstinence discussed above. Viewed more broadly, these findings suggest there may be gender-related differences in relapse precipitants with women generally more susceptible to negative affect and men more susceptible to cue-induced social precursors.
4.1. Limitations
Patients self-select into AA and we cannot rule out “third” variable effects. Difference in sample sizes between men and women may have resulted in some findings being statistically significant for men but not women despite similar effect size. The sample, although large, is treatment–seeking, mostly White and middle-aged and results reflect changes early in recovery. Caution should be taken when extrapolating these findings to others. There were long time lags between measures; future research should examine relationships using finer temporal resolutions (i.e., across days/weeks rather than months). Data were collected in the 1990s; to the extent that changes have occurred in sociocultural, gender, treatment, and/or AA aspects, it is possible that replications of the study today may result in different estimates of these effects.
4.2. Conclusions
Similar to the psychotherapy literature on “how patients make therapy work” (Bohart et al., 1999), and placing these findings in the context of others that have examined mechanisms of behavior change within AA (e.g., Blonigen et al., 2011; Kelly et al., 2009, 2012a), rather than thinking about “how AA works” it may be more accurate and useful to think about “how individuals make AA work for them”. It is likely that AA participants attend to, and use, whichever of a variety of helpful aspects that may be on offer in AA that have the most salience and relevance at that particular time in their phase of recovery. Men may use AA more than women to help them buffer socially-relevant relapse risks. Women appear to benefit in similar ways, but more work is needed to understand the additional ways women derive recovery benefit from AA. The pattern of findings underscores some gender-based differences that may have broader implications for the addiction treatment and recovery field. For women between the ages of 30 and 50, a focus on finding alternative ways to cope with negative affect may yield recovery benefits, while among men in the same life-stage, a relatively greater focus on coping with high risk social situations may yield recovery related benefits.
Acknowledgments
Role of funding source This research was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism (NIAAA R21 AA016762; Mechanisms and Moderators of Behavior Change in Alcoholics Anonymous) and a grant from the National Institute on Drug Abuse (K01 DA027097). NIAAA and NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors Authors Kelly and Hoeppner designed the study and wrote the protocol. Author Kelly managed the literature searches and summaries of previous related work. Author Hoeppner undertook the statistical analysis, and authors Kelly and Hoeppner wrote the first draft of the manuscript. Both authors contributed to and have approved the final manuscript.
Conflict of interest The authors have no conflict of interest, including specific financial interests and relationships and affiliations relevant to the subject of this manuscript.
REFERENCES
- Alcoholics Anonymous . Alcoholics Anonymous: The Story of How Thousands of Men and Women have Recovered from Alcoholism. 3 ed. Alcoholics Anonymous World Services; New York: 1939. [Google Scholar]
- Alcoholics Anonymous . Twelve Steps and Twelve Traditions. Alcoholics Anonymous World Services; New York: 1952. [Google Scholar]
- Alcoholics Anonymous . 2011 Membership Survey. Alcoholics Anonymous World Services; New York: 2012. [Google Scholar]
- Beck AT, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch. Gen. Psychiatr. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Blonigen DM, Timko C, Finney JW, Moos BS, Moos RH. Alcoholics Anonymous attendance, decreases in impulsivity and drinking and psychosocial outcomes over 16 years: moderated-mediation from a developmental perspective. Addiction. 2011;106:2167–2177. doi: 10.1111/j.1360-0443.2011.03522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohart AC, Tallman K. How Clients Make Therapy Work: The Process of Active Self-Healing. American Psychological Association; Washington, DC: 1999. [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the U.S. 2006. Am. J. Prev. Med. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Binge Drinking. Vital Signs. 2012 Retrieved from: www.cdc.gov/vitalsigns/bingedrinking/
- Cha Y. Reinforcing separate spheres: the effect of spousal overwork on men's and women's employment in dual-earner households. Am. Sociol. Rev. 2010;75:303–329. [Google Scholar]
- Clifford PR, Longabaugh R. Center for Alcohol and Addiction Studies. Brown University; Providence: 1991. Manual for the Administration of the Important People and Activities Instrument: Adapted for use by Project MATCH for NIAAA 5R01AA06698-05. [Google Scholar]
- Connors GJ, Tonigan JS, Miller WR. Measure of religious background and behavior for use in behavior change research. Psychol. Addict. Behav. 1996;10:90–96. [Google Scholar]
- Del Boca FK, Mattson ME. The gender matching hypothesis. In: Longabaugh R, Wirtz P, editors. Project MATCH Hypotheses: Results and Causal Chain Analysis. Project MATCH Monograph Series. Vol. 8. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2001. [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. J. Stud. Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: What is Currently Known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. Rutgers Center of Alcohol Studies; Rutgers: 1993. pp. 41–76. [Google Scholar]
- Ferri M, Amato L, Davoli M. Alcoholics Anonymous and other 12-step programmes for alcohol dependence. Cochrane Database Syst. 2006 doi: 10.1002/14651858.CD005032.pub2. Rev. 3, CD005032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield TK, Weisner C. Drinking problems and self-reported criminal behavior, arrests and convictions: 1990 US alcohol and 1989 county surveys. Addiction. 1995;90:361–373. doi: 10.1046/j.1360-0443.1995.9033616.x. [DOI] [PubMed] [Google Scholar]
- Humphreys K. Circles of recovery: Self-help Organizations for Addictions. Cambridge University Press; Cambridge: 2004. [Google Scholar]
- Humphreys K, Mavis B, Stofflemayr B. Are twelve step programs appropriate for disenfranchised groups? In: Lavoie F, Borkman T, Gidron B, editors. Mutual Aid and Mutual Aid Groups: International and Multicultural Perspectives. Haworth Press; New York: 1994. [Google Scholar]
- Humphreys K, Moos R. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcohol. Clin. Exp. Res. 2001;25:711–716. [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Encouraging posttreatment self-help group involvement to reduce demand for continuing care services: two-year clinical and utilization outcomes. Alcohol. Clin. Exp. Res. 2007;31:64–68. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Broadening the Base of Treatment for Alcohol Problems. National Academy Press; Washington, DC: 1990. [PubMed] [Google Scholar]
- Kadden RM, Carroll KM, Donovan D, ooney N, Monti P, Abrams D, Litt M, Hester R. Cognitive-behavioral coping skills therapy manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Project MATCH Monograph Series. 1992;4 (DHHS Publication No. (ADM) 92-1895) [Google Scholar]
- Kaskutas LA. Alcoholics anonymous effectiveness: faith meets science. J. Addict. Dis. 2009;28:145–157. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Ye Y, Greenfield TK, Witbrodt J, Bond J. Epidemiology of Alcoholics Anonymous participation. Rec. Dev. Alcohol. 2008;18:261–282. doi: 10.1007/978-0-387-77725-2_15. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J. Child Psychol. Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelly JF. Self-help for substance use disorders: history, effectiveness, knowledge gaps research opportunities. Clin. Psychol. Rev. 2003;23:639–663. doi: 10.1016/s0272-7358(03)00053-9. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Hoeppner BB, Stout RL, Pagano M. Determining the relative importance of the mechanisms of behavior change within Alcoholics Anonymous: a multiple mediator analysis. Addiction. 2012a;107:289–299. doi: 10.1111/j.1360-0443.2011.03593.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addict. Res. Theory. 2009;17:236–259. [Google Scholar]
- Kelly JF, Stout RL, Magill M, Tonigan JS. The role of Alcoholics Anonymous in mobilizing adaptive social network changes: a prospective lagged mediational analysis. Drug Alcohol Depend. 2011a;114:119–126. doi: 10.1016/j.drugalcdep.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Mechanisms of behavior change in alcoholics anonymous: does Alcoholics Anonymous lead to better alcohol use outcomes by reducing depression symptoms? Addiction. 2010;105:626–636. doi: 10.1111/j.1360-0443.2009.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Magill M, Tonigan JS, Pagano ME. Spirituality in recovery: a lagged mediational analysis of alcoholics anonymous’ principal theoretical mechanism of behavior change. Alcohol. Clin. Exp. Res. 2011b;35:454–463. doi: 10.1111/j.1530-0277.2010.01362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, White WL. Broadening the base of addiction mutual-help group organizations. J. Groups Addict. in press Recover.
- Kelly JF, Yeterian JD. Mutual-help groups. In: O'Donohue W, Cunningham JA, editors. Evidence-Based Adjunctive Treatments. Elsevier; New York: 2008. [Google Scholar]
- Kelly JF, Yeterian JD. Empirical awakening: the new science on mutual help and implications for cost containment under health care reform. Subst. Abuse. 2012b;33:85–91. doi: 10.1080/08897077.2011.634965. [DOI] [PubMed] [Google Scholar]
- Kownacki RJ, Shadish WR. Does Alcoholics Anonymous work? The results from a meta-analysis of controlled experiments. Subst. Use Misuse. 1999;34:1897–1916. doi: 10.3109/10826089909039431. [DOI] [PubMed] [Google Scholar]
- Krentzman AR, Brower KJ, Cranford JA, Bradley JC, Robinson EAR. Gender and extroversion as moderators of the association between Alcoholics Anonymous and sobriety. J. Stud. Alcohol Drugs. 2012;73:44–52. doi: 10.15288/jsad.2012.73.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche S, Knibbe R, Kuntsche E, Gmel G. Housewife or working mum--each to her own? The relevance of societal factors in the association between social roles and alcohol use among mothers in 16 industrialized countries. Addiction. 2011;106:1925–1932. doi: 10.1111/j.1360-0443.2011.03507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche S, Knibbe RA, Gmel G. Social roles and alcohol consumption: a study of 10 industrialised countries. Soc. Sci. Med. 2009;68:1263–1270. doi: 10.1016/j.socscimed.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP. Introduction to Statistical Mediation Analysis. Taylor & Francis Group/Lawrence Erlbaum Associates; New York: 2008. [Google Scholar]
- Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behav. Res. 2004;39:99. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maier W, Gansicke M, Gater R, Rezaki M, Tiemens B, Urzua RF. Gender differences in the prevalence of depression: a survey in primary care. J. Affect. Disord. 1999;53:241–252. doi: 10.1016/s0165-0327(98)00131-1. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. J. Stud. Alcohol Suppl. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Moos RH, Moos BS, Timko C. Gender, treatment and self-help in remission from alcohol use disorders. Clin. Med. Res. 2006;4:163–174. doi: 10.3121/cmr.4.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. J. Person. Soc. Psychol. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin. Psychol. Rev. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K, editors. Twelve-Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. Vol. 4. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Office of National Drug Control Policy . National Drug Control Strategy. Washington, DC: 2011. [DOI] [PubMed] [Google Scholar]
- Owen PL, Slaymaker V, Tonigan JS, McCrady BS, Epstein EE, Kaskutas LA, Humphreys K, Miller WR. Participation in Alcoholics Anonymous: intended and unintended change mechanisms. Alcohol. Clin. Exp. Res. 2003;27:524–532. doi: 10.1097/01.ALC.0000057941.57330.39. [DOI] [PubMed] [Google Scholar]
- Paradis C. Parenthood, drinking locations and heavy drinking. Soc. Sci. Med. 2011;72:1258–1265. doi: 10.1016/j.socscimed.2011.02.025. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression. Critical review. Br. J. Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Potenza MN, Hong KI, Lacadie CM, Fulbright RK, Tuit KL, Sinha R. Neural correlates of stress-induced and cue-induced drug craving: influences of sex and cocaine dependence. Am. J. Psychiatry. 2012;169:406–414. doi: 10.1176/appi.ajp.2011.11020289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell TJ. Self-help Organizations and Professional Practice. NASW Press; Silver Spring, MD: 1987. [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol. Clin. Exp. Res. 1993;17:1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J. Stud. Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Rice JP, Neuman RJ, Saccone NL, Corbett J, Rochberg N, Hesselbrock V, Bucholz KK, McGuffin P, Reich T. Age and birth cohort effects on rates of alcohol dependence. Alcohol. Clin. Exp. Res. 2003;27:93–99. doi: 10.1097/01.ALC.0000047303.89421.AA. [DOI] [PubMed] [Google Scholar]
- Room R, Greenfield T. Alcoholics anonymous, other 12-step movements and psychotherapy in the US population, 1990. Addiction. 1993;88:555–562. doi: 10.1111/j.1360-0443.1993.tb02062.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol. Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Monte Carlo method for assessing mediation: an interactive tool for creating confidence intervals for indirect effects [Computer software] 2008 Available from http://quantpsy.org/
- Sobel ME. Some new results on indirect effects and their standard errors in covariance structure models. In: Tuma N, editor. Sociological Methodology 1986. American Sociological Association; Washington, DC: 1986. pp. 159–186. [Google Scholar]
- Sobell ME. Asymptotic confidence intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological Methodology 1982. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . The NSDUH Report: Participation in Self-Help Groups for Alcohol and Illicit Drug Use: 2006 and 2007. Office of Applied Studies; Rockville, MD: 2008. [Google Scholar]
- Timko C, Moos RH, Finney JW, Connell EG. Gender differences in help-utilization and the 8-year course of alcohol abuse. Addiction. 2002;97:877–889. doi: 10.1046/j.1360-0443.2002.00099.x. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. J. Stud. Alcohol Drugs. 1996;57:65–72. doi: 10.15288/jsa.1996.57.65. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice . The Economic Impact of Illicit Drug Use on American Society. Washington, DC: 2011. [Google Scholar]
- UK Drug Strategy . Reducing demand, restricting supply, building recovery: supporting people to live a drug-free life. HM Government; London: 2010. [Google Scholar]
- Weich S, Sloggett A, Lewis G. Social roles and gender difference in the prevalence of common mental disorders. Br. J. Psychiatry. 1998;173:489–493. doi: 10.1192/bjp.173.6.489. [DOI] [PubMed] [Google Scholar]
- White WL. Great Lakes Addiction Technology Transfer Center and Philadelphia. Department of Behavioral Health and Mental Retardation Services; Chicago, IL: 2009. Peer-based Addiction Recovery Support: History, Theory, Practice, and Scientific Evaluation. [Google Scholar]
- Wilsnack R, Wilsnack S. Gender and Alcohol: Individual and Social Perspectives. 3rd Ed. Rutgers Center of Alcohol Studies; Rutgers: 1997. [Google Scholar]
- Witbrodt J, Delucchi K. Do women differ from men on alcoholics anonymous participation and abstinence? A multi-wave analysis of treatment seekers. Alcohol. Clin. Exp. Res. 2011;35:2231–2241. doi: 10.1111/j.1530-0277.2011.01573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt J, Romelsjo A. Gender differences in mutual-help attendance one year after treatment: Swedish and U.S. samples. J. Stud. Alcohol Drugs. 2010;71:125–135. doi: 10.15288/jsad.2010.71.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yung YF. Testing and Contrasting Mediation or Indirect Effects in SEM: An Analytic Approach and its Implementation.. Paper presented at the Paper presented at the 73rd Annual Meeting of the Psychometric Society.2008. [Google Scholar]
- Zemore SE. A role for spiritual change in the benefits of 12-step involvement. Alcohol. Clin. Exp. Res. 2007;31(Suppl. 10):76s–79s. doi: 10.1111/j.1530-0277.2007.00499.x. [DOI] [PubMed] [Google Scholar]