Abstract
AIM: To analyze our results after the introduction of a fast-track (FT) program after laparoscopic liver surgery in our Hepatobiliarypancreatic Unit.
METHODS: All patients (43) undergoing laparoscopic liver surgery between March 2004 and March 2010 were included and divided into two consecutive groups: Control group (CG) from March 2004 until December 2006 with traditional perioperative cares (17 patients) and fast-track group (FTG) from January 2007 until March 2010 with FT program cares (26 patients). Primary endpoint was the influence of the program on the postoperative stay, the amount of re-admissions, morbidity and mortality. Secondarily we considered duration of surgery, use of drains, conversion to open surgery, intensive cares needs and transfusion.
RESULTS: Both groups were homogeneous in age and sex. No differences in technique, time of surgery or conversion to open surgery were found, but more malignant diseases were operated in the FTG, and then transfusions were higher in FTG. Readmissions and morbidity were similar in both groups, without mortality. Postoperative stay was similar, with a median of 3 for CG vs 2.5 for FTG. However, the 80.8% of patients from FTG left the hospital within the first 3 d after surgery (58.8% for CG).
CONCLUSION: The introduction of a FT program after laparoscopic liver surgery improves the recovery of patients without increasing complications or re-admissions, which leads to a reduction of the stay and costs.
Keywords: Liver surgery, Laparoscopy, Fast-track
INTRODUCTION
During the last two decades, we have attended to the progressive introduction and development of laparoscopy for the treatment of different disorders. Thus, laparoscopy has become the gold-standard for some of them (cholelithiasis, morbid obesity, reflux and adrenal diseases)[1]. Among the advantages, we can find a faster recovery of patients, better aesthetic results and a reduction of the postoperative stay[2].
Therefore laparoscopic liver surgery has many requirements, such as a large experience in liver surgery and advanced laparoscopy, resolutive skills in haemorrhage control, availability of specific equipment for parenchymal transection, etc.[3]. For these reasons, the evolution of laparoscopy in this particular area has been slower. However, nowadays its indications and results are totally comparable to open procedures[4].
“Fast-track” (FT) was introduced by Kehlet[5] in 1997. It is known as a group of perioperative assessments aimed to enhance recovery of patients undergoing surgery by minimizing organ dysfunction caused by the surgery. Patient’s collaboration and acknowledgement of the procedures (early oral intake and deambulation, multimodal and opioid-sparing analgesia¡) as well as collaboration of other professionals [anaesthesiologists, intensive care units (ICU), nurses, etc.] are essential for the achievement of a FT program. Regarding this, minimally invasive surgery, appropriate use of drains and probes, strict control of fluids and regional anaesthesia, are definitely the tools leading to a faster recovery of our patients. No increase of morbidity must be associated with the adoption of these therapeutic options, and normally a decrease of hospital stay may be reached. Evidence with these programs exists in colon surgery[6,7], but there is still limited information about its feasibility in liver surgery, either open or laparoscopic[8-10].
We report our results after the implantation of a FT program in patients undergoing laparoscopic liver surgery in a specialized Unit of Hepatobiliarypancreatic Surgery.
MATERIALS AND METHODS
Design
We designed an analytic observational study, over a cohort of consecutive patients undergoing laparoscopic liver surgery during the period from March 2004 to March 2010. For the analysis, we considered a control group (CG) of patients operated between March 2004 and December 2006, who had traditional perioperative cares (17 cases), and a fast track group (FTG), including the patients operated between January 2007 and March 2010, with the perioperative cares of the FT program (26 cases).
Basically, our FT program for laparoscopic liver surgery consisted in: (1) reduction of indications of drains after surgical procedure; (2) changing location of patients in the early post-operative period, considering not necessary ICU admission for patients without severe morbidity, undergoing atypical resections or typical up to two segments, without transfusions and without/less than 30 min vascular clamping; (3) obviate necessity of a nasogastric tube; (4) prescription of early oral intake and ambulation (introduced the same evening of surgery, 6-8 h after); and (5) optimization of analgesia, according with Anaesthesia Department suggestions, with metamizol/8 h and paracetamol/8 h alternating, initially intravenous and oral afterwards, avoiding opioids. A description of the whole FT program is shown in Table 1.
Table 1.
Fast track program in laparoscopic liver surgery
| Preoperative cares |
| No liquid intake 8 h before surgery |
| Administration of anaesthetic premedication |
| Intraoperative cares |
| Control of fluids |
| Removing nasogastric tube at the end of surgery |
| No urinary tubes in procedures of < 180 min |
| Selection of indications of intraabdominal drains |
| Postoperative cares |
| Early: ICU/recovery room |
| Oral intake 6-8 h after the surgery |
| Mobilization 6-8 h after the surgery |
| Analgesia: intravenous metamizol/8 h + intravenous paracetamol/8 h within the first 24 h and then oral analgesia |
| Removal of drains (when used) 24-48 h |
| Blood test 24 h after (haemogram, coagulation and hepatic profile) |
ICU: Intensive care unit.
Primary endpoint of our study was to settle the influence of the FT program on the postoperative stay, defined as number of nights at hospital, including readmissions during the following 30 d[8,9]. Also morbidity and mortality were considered. Secondarily, we considered duration of surgery, use of drains, conversion to open surgery, transfusions and the need of intensive cares in both groups. Time until reintroduction of oral intake, ambulation and withdrawal of nasogastric tube were also considered.
Patients were all previously informed about the FT program, understanding and accepting all the explanations about their clinical course during postoperative period. All of them left the hospital after ambulation and positive oral diet without vomiting. Follow-up was accomplished by the same surgeon the following day after leaving the hospital (by telephone) and 7 d after discharge.
Surgery
All the surgeries were performed, in both periods, by a qualified surgeon of the Hepatobiliarypancreatic and Transplantation Surgery Unit. We included as candidates for laparoscopic surgery those patients with lesions located in segments II, III, IVb, V and VI. Eventually we included lesions in segment VII. Patients with lesions located in segment VIII or IVa were excluded.
According to location of the lesions, patients were placed in French position (anterior segments and left lobe) or left lateral decubitus (segments VI-VII). Pneumoperitoneum was made with Verres Needle or Hasson’s trocar, depending on the preference of the surgeon. Four or five trocars were used depending on the size and location of lesions. Pringle’s manoeuvre was applied when it was necessary, using a vascular tape around the hepatic hilum (we find very useful Fabretti’s retractor for this manoeuvre).
Parenchymal transection was performed using Ligasure Atlas, achieving haemostasis and biliostasis using Tissue-Link. Portal pedicles and suprahepatic veins were controlled with vascular staplers. Surgical specimens were removed with a plastic bag through scars of previous surgeries (appendectomy, laparoscopic cholecystectomy or median laparotomy), widening a trocar incision or performing a Pfannestiel incision. An additional surgical technique was indicated in 11 occasions (9 cholecystectomies and 2 appendectomies).
Statistical analysis
Statistical analysis was made with SPSS version 15.0 for Windows (SPSS, Chicago, IL, United States). Continuous variables (age, sex, post-operative stay and duration of surgery) were defined by median (rank) or mean and analyzed with the Mann-Whitney U test. Qualitative variables (use of drains, conversion, transfusion, intensive cares, readmissions and morbidity) were defined by percentages and analyzed by χ2 test with Yates correction and Fisher’s exact test.
RESULTS
Both groups were homogeneous in age, sex and anaesthetic risk (all patients were classified as ASA II-III). However, more patients with malignant diseases were operated in the FTG (17.5% vs 46.2%, P < 0.05) (Table 2).
Table 2.
Demographic data n (%)
| Control group (n = 17) | Fast-track group (n = 26) | P value | |
| Age (yr) | 52.5 (29-84) | 58.3 (29-77) | NS |
| Sex (M:F) | 10:7 | 15:11 | NS |
| ASA | NS | ||
| II | 8 (47.05) | 13 (50) | |
| III | 9 (52.94) | 13 (50) | |
| Indication | < 0.05 | ||
| Benign/malignant | 14 (82.4)/ 3 (17.6) | 14 (53.8)/ 12 (45.2) | |
| Pathology | |||
| Haemangioma | 1 | 1 | |
| Hidatidosis | 1 | 2 | |
| FNH | 6 | 4 | |
| HCC | 3 | 3 | |
| ColangioCa | 0 | 1 | |
| Metastasis | 0 | 8 | |
| Policystosis/simple cyst | 5 | 7 | |
| Others | 1 | 0 |
ASA: American society of anaesthesiologists index; FNH: Focal Nodular hyperpasia; HCC: Hepatocelular carcinoma; ColangioCa: Colangiocarcinoma; M: Male; F: Female; NS: Not significant.
Table 3 shows results related with the surgical procedure. The surgical technique (atypical resection, unroofing, lobectomy, etc.), the duration of surgery [177.35 min vs 180.19 min, not significant (NS)] and Pringle’s manoeuvre (29.4% vs 26.9%, NS) were all similar in both groups. The number of transfusions was higher in FTG (5.8% vs 19.2%, P < 0.05). Conversion to open surgery was similar in both groups (11.8% vs 19.2%, NS), caused principally by difficulty in haemorrhage control of portal pedicles or suprahepatic veins (5 cases). Technical difficulties were the reason in the other two cases. Drains were considered necessary during a significantly higher number of procedures in the GC (88.2% vs 23.1%, P < 0.001).
Table 3.
Surgical procedure results n (%)
| Control group (n = 17) | Fast-track group (n = 26) | P value | |
| Technique | NS | ||
| Left lateral sectionectomy | 4 (23.5) | 5 (19.2) | |
| Atypical resection | 7 (41.2) | 12 (46.2) | |
| Unroofing | 5 (29.4) | 7 (26.9) | |
| Cystopericystectomy | 1 (5.9) | 2 (7.7) | |
| Surgery time, min (range) | 177 (80-300) | 180 (60-345) | NS |
| Conversion | 2 (11.8) | 5 (19.2) | NS |
| Pringle | 5 (29.4) | 7 (26.9) | NS |
| Transfusion | 1 (5.8) | 5 (19.2) | < 0.05 |
| Drains | 15 (88.2) | 6 (23.1) | < 0.000 |
| ICU | 12 (70.6) | 4 (15.4) | < 0.000 |
ICU: Intensive care unit; NS: Not significant.
The location of patients in the early postoperative time changed drastically after the introduction of the FT program. We found that 70.6% of patients of the CG had intensive cares, and only 15.3% of them in FTG (P < 0.001). Meanwhile a nasogastric tube was prescribed to all patients in CG, only one patient in the FTG needed a nasogastric tube in postoperative time due to a contained evisceration. Early oral intake and mobilization (defined as the moment when the patient is able to get up and leave the bed) were introduced the same evening of surgery (6-8 h) in all of the patients not needing intensive cares in the FTG. In the CG these events were always introduced after the first post-operative day, with a rank of 1-4 d for intake and 1-7 d for mobilization. With the sequence of analgesia prescribed a good control was achieved in 95% of cases in the FTG, and thus neither epidural pumps nor opioids during post-operative time were indicated
Complications were present in five patients (11.62%): two cases in CG and three in FTG (11.8% vs 11.5%, NS). Those in CG were both respiratory infections (basal atelectasia and right basal pneumonia). These complications prolonged hospital stay 5 d and 22 d, respectively. Those in FTG were an evisceration of the laparotomy through which the specimen was removed, a gaseous embolism and a perihepatic haematoma not surgically treated. Stay was prolonged because of these complications 15 d, 39 d and 17 d respectively. None of the patients presented biliary fistula or hepatic failure and no mortality was found in both groups. Readmissions were similar (5.8% vs 3.8%, NS), due to a pneumonia in the CG and an intraabdominal haematoma in the FTG (Table 4). Postoperative stay (defined as the number of nights at the hospital including the readmissions in the 30 d after the surgery) was slightly higher in the CG [3 (1-22) vs 2.5 (1-39), NS]. Likewise, in the FTG, 80.8% of the patients could leave the hospital within the next 3 d after the surgery, whereas in the CG, only the 58.8% of them could do so (NS) (Figure 1). Even when not statistically significant, the reduction of costs with this event was estimated in around 30%.
Table 4.
Complications, postoperative stay, morbidity and mortality n (%)
| Control group (n = 17) | Fast-track group (n = 26) | P value | |
| Postoperative stay | 3 (1-22) | 2.5 (1-39) | NS |
| < 3 d | 10 (58.8) | 7 (41.2) | |
| > 3 d | 21 (80.8) | 5 (19.2) | |
| Complications | 2 (11.8) | 3 (11.5) | NS |
| Readmissions | 1 (5.8) | 1 (3.8) | NS |
| Mortality | 0 | 0 |
NS: Not significant.
Figure 1.
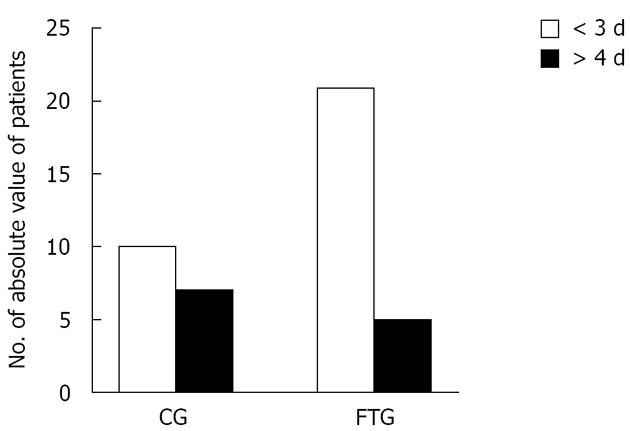
Graphic of post-operative stay (more or less than 3 d). CG: Control group; FTG: Fast-track group.
DICUSSION
Laparoscopy in liver surgery provides a reduction of postoperative stay comparing to traditional surgery[3,11]. Despite the lack of evidence, some studies show a reduction of postoperative stay (in both open and laparoscopic surgery) after the introduction of FT programs[8,9]. The early oral intake and mobilization after surgery is well known to reduce postoperative ileus as well as the need of intravenous fluids[12,13]. In our FT program, we reintroduced oral intake 6-8 h after surgery and mobilization is initiated the same evening of the surgery. This sequence is very similar to van Dam’s group, starting oral intake 4h after surgery[8].
Systematic use of drains has been abandoned in this type of surgery, using them only in 6 patients (23%). Nowadays, evidence supports that drains cannot prevent either biliary collection or reoperation[14], and it has been reported that they may lead to intraabdominal abscess formation[15].
The fact that all of our patients underwent laparoscopic surgery has helped us to an adequate control of pain, using conventional intravenous analgesia during the first 24 h (oral analgesia afterwards), not being necessary thoracic epidural catheters. In Stoot et al[9] study all the resections were also laparoscopic, but it is not clarified the way to control postoperative pain. It is proved that laparoscopic surgery reduces pain and analgesia requirements.
We did not find a reduction of the time of surgery, but the need of transfusions was higher in the FTG, probably related with the higher rate of malignant diseases operated during this period, defining a group of patients with a higher complexity (chirrosis, previous chemotherapy...). Stoot et al[9] reported times slightly shorter and less haemorrhages, and this is explained by the fact of having improved their technique.
We found a very similar morbidity rate in both groups (11.8% vs 11.5%), since complications such as fistula, haemorrhage or hepatic failure are not related with the postoperative cares[3]. Eighty percent of our complications occurred in patients with malignant diseases (hepatocellular carcinoma and metastasis), which suits perfectly with the results reported as these patients must be identified as having a higher postoperative risk (50% vs 11%)[16].
Our study shows a tendency to reduction of postoperative stay after the introduction of a FT program (median: 2.5 d). As well as in Scott’s series, we could not find statistical significance, probably because the number of patients is still very small, but tendency is clearly shown in Figure 1. However, in both studies the stay is slightly reduced comparing to other series[11,17]. van Dam et al[8] found differences in open hepatic surgery of 161 patients after a FT program (6 d vs 8 d, P < 0.0001). In colon surgery the reduction of the stay is clearly proved in several studies[6,7,18], up to 3-4 d.
Differences between our FT program and classical clinical pathway for patients who undergo laparoscopic liver surgery begin preoperatively. Due to the special characteristics of liver surgery, the possibility of being discharged less than 3 d after surgical procedure may be inconceivable. This is the reason why a FT program must begin with the identification of potential candidates for laparoscopic approach (exclusion of lesions on segments IVa and VIII) and with detailed preoperative information to be sure that the patients understand and accept this policy. Even when other FT programs establish age > 70 years as the limit for including patients, in our opinion age per se must not be considered a formal contraindication, but patients with inadequate performance status or ASA > III must be excluded. Perioperatively, indication of nasogastric and urinary tubes or drainages must be strongly restricted to selected cases. After surgery, ICU must be avoided if atypical resections or typical less than 2 segments have been perfomed, without or with no more than 30 min of hilar clamping and if transfusions have not been necessary. Oral intake and mobilization must be prescribed as soon as possible, and opioids must not be used as analgesia. After discharge, patients must be comfortable and must feel that hospital devices and organization are behind them, so we consider essential the immediate follow-up that we carry out the day after and 7 d after patients leave the hospital. In summary, this study shows the applicability of a FT program in laparoscopic liver surgery, leading to an early recovery of patients, without increasing morbidity, mortality or the amount of readmissions, leading to a considerable reduction of costs.
COMMENTS
Background
Abdominal surgeons are progressively incorporating new strategies for improving the recovery of their patients. Laparoscopic approach has been one of the most important advances in abdominal surgery, and recently fast-track (FT) programs show great advantages in postoperative course and in early discharge without increasing morbidity. However, liver surgery remains being considered as of high complexity and the application of laparoscopic approach and FT tendencies in this field may be controversial.
Research frontiers
Since laparoscopy must be considered an approach, there is no formal contraindication for its use in liver surgery. However, well designed, randomized and controlled studies might be performed for better understanding the role of FT programs in liver surgery. Repercussion on costs should be better studied.
Innovations and breakthroughs
Previous reports show benefits with the application of FT tendencies to liver surgery. Another papers report the advantages of laparoscopic approach to this surgical field. Very few, however, have considered the option of joining laparoscopy and FT in liver surgery. In this paper, a control group of patients who underwent laparoscopic liver surgery with traditional postoperative cares was included.
Applications
This study suggests that the incorporation of a FT program to laparoscopic liver surgery is feasible and may be instituted as usual for selected patients. Recovery of patients may be improved, hospital stay may be decreased and costs may be reduced.
Terminology
FT should be defined as the totality of therapeutic options (including laparoscopic approach) adopted to improve recovery of surgical patients, pre, peri and postoperatively. They are all aimed to enhance recovery by minimizing organ dysfunction associated with surgical aggression. A decrease in hospital stay may result from the application of these lines, but no increase in morbidity should be associated.
Peer review
This study shows the applicability of a fast tract program in laparoscopic liver surgery, leading to an early recovery of patients, this is an well written paper.
Footnotes
Peer reviewer: Chen-Guo Ker, MD, PhD, FACS, Superintendent and Professor, Department of GI Surgery, Yuan’s General Hospital, Kaohsiung 80249, Taiwan
S- Editor Wen LL L- Editor A E- Editor Zheng XM
References
- 1.Ramírez-Plaza CP, Rodríguez-Cañete A, Domínguez-López ME, Valle-Carbajo M, Jiménez-Mazure C, Marín-Camero N, Gallego-Perales JL, Santoyo-Santoyo J. [Development and evolution of laparoscopic adrenalectomy in an specialized team: from the beginning to the outpatient setting] Endocrinol Nutr. 2010;57:22–27. doi: 10.1016/S1575-0922(10)70005-X. [DOI] [PubMed] [Google Scholar]
- 2.Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004;91:1111–1124. doi: 10.1002/bjs.4640. [DOI] [PubMed] [Google Scholar]
- 3.Cugat E, Marco C. [Laparoscopic liver surgery. A mature option?] Cir Esp. 2009;85:193–195. doi: 10.1016/j.ciresp.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831–841. doi: 10.1097/SLA.0b013e3181b0c4df. [DOI] [PubMed] [Google Scholar]
- 5.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–617. doi: 10.1093/bja/78.5.606. [DOI] [PubMed] [Google Scholar]
- 6.Muller S, Zalunardo MP, Hubner M, Clavien PA, Demartines N. A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology. 2009;136:842–847. doi: 10.1053/j.gastro.2008.10.030. [DOI] [PubMed] [Google Scholar]
- 7.Hammer J, Harling H, Wille-Jørgensen P. Implementation of the scientific evidence into daily practice--example from fast-track colonic cancer surgery. Colorectal Dis. 2008;10:593–598. doi: 10.1111/j.1463-1318.2007.01469.x. [DOI] [PubMed] [Google Scholar]
- 8.van Dam RM, Hendry PO, Coolsen MM, Bemelmans MH, Lassen K, Revhaug A, Fearon KC, Garden OJ, Dejong CH. Initial experience with a multimodal enhanced recovery programme in patients undergoing liver resection. Br J Surg. 2008;95:969–975. doi: 10.1002/bjs.6227. [DOI] [PubMed] [Google Scholar]
- 9.Stoot JH, van Dam RM, Busch OR, van Hillegersberg R, De Boer M, Olde Damink SW, Bemelmans MH, Dejong CH. The effect of a multimodal fast-track programme on outcomes in laparoscopic liver surgery: a multicentre pilot study. HPB (Oxford) 2009;11:140–144. doi: 10.1111/j.1477-2574.2009.00025.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacKay G, O’Dwyer PJ. Early discharge following liver resection for colorectal metastases. Scott Med J. 2008;53:22–24. doi: 10.1258/rsmsmj.53.2.22. [DOI] [PubMed] [Google Scholar]
- 11.Morino M, Morra I, Rosso E, Miglietta C, Garrone C. Laparoscopic vs open hepatic resection: a comparative study. Surg Endosc. 2003;17:1914–1918. doi: 10.1007/s00464-003-9070-4. [DOI] [PubMed] [Google Scholar]
- 12.Henriksen MG, Hansen HV, Hessov I. Early oral nutrition after elective colorectal surgery: influence of balanced analgesia and enforced mobilization. Nutrition. 2002;18:263–267. doi: 10.1016/s0899-9007(01)00749-3. [DOI] [PubMed] [Google Scholar]
- 13.Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet. 2002;359:1812–1818. doi: 10.1016/S0140-6736(02)08711-1. [DOI] [PubMed] [Google Scholar]
- 14.Petrowsky H, Demartines N, Rousson V, Clavien PA. Evidence-based value of prophylactic drainage in gastrointestinal surgery: a systematic review and meta-analyses. Ann Surg. 2004;240:1074–1084; discussion 1084-1085. doi: 10.1097/01.sla.0000146149.17411.c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Figueras J, Llado L, Miro M, Ramos E, Torras J, Fabregat J, Serrano T. Application of fibrin glue sealant after hepatectomy does not seem justified: results of a randomized study in 300 patients. Ann Surg. 2007;245:536–542. doi: 10.1097/01.sla.0000245846.37046.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L, et al. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg. 2002;236:90–97. doi: 10.1097/00000658-200207000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dagher I, Proske JM, Carloni A, Richa H, Tranchart H, Franco D. Laparoscopic liver resection: results for 70 patients. Surg Endosc. 2007;21:619–624. doi: 10.1007/s00464-006-9137-0. [DOI] [PubMed] [Google Scholar]
- 18.Zargar-Shoshtari K, Connolly AB, Israel LH, Hill AG. Fast-track surgery may reduce complications following major colonic surgery. Dis Colon Rectum. 2008;51:1633–1640. doi: 10.1007/s10350-008-9386-1. [DOI] [PubMed] [Google Scholar]


