Abstract
Hemothorax due to rupture of metastatic hepatocellular carcinoma (HCC) is a very rare complication with high mortality because of uncontrollable hemorrhage. A 71-year-old man treated by transcatheter arterial embolization for HCC with massive bleeding from chest wall metastasis is reported. Enhanced computed tomography and selective intercostal angiogram showed a hypervascular mass in the right chest wall and extravasation of contrast agent. After successful transcatheter arterial embolization with gelatin sponge particles and metallic coils, the patient recovered from shock without major complication. To our knowledge, a successfully treated case of hemothorax due to rupture of metastatic HCC has not previously been described.
Keywords: Hepatocellular carcinoma, Chest wall metastasis, Rupture, Transcatheter arterial embolization, Hemothorax
INTRODUCTION
Hemoperitoneum caused by ruptured hepatocellular carcinoma (HCC) is not uncommon in patients with HCC. Hemothorax due to rupture of metastatic HCC, however, is a very rare complication with high mortality because of uncontrollable hemorrhage. Transcatheter arterial embolization (TAE) is generally performed for hemorrhagic shock due to rupture of HCC, and there are many reports of its efficacy. However, there have been few reports of TAE performed for hemorrhagic shock due to rupture of chest wall metastases of HCC. An unusual case in which TAE for hemorrhagic shock due to rupture of chest wall metastasis of HCC was life-saving is reported.
CASE REPORT
The patient was a 71-year-old man. He had suffered from HCC and metastatic bone tumors for two years. Since he became ill and developed clouded consciousness (JCS20) while walking at a swimming pool, he was transported to our hospital immediately. He had a tachycardia (135 bpm) on arrival and was in hemorrhagic shock, with a blood pressure of 67/45 mmHg and a Hb of 9.8 g/dL. In addition, the platelet count was low (44000/μL), hepatic enzymes were increased, and total bilirubin was increased (1.82mg/dL).
Since a hypervascular tumor of approximately 2 cm was seen at the right chest wall, with hemothorax and extravasation of contrast agent on contrast-enhanced computed tomography (CT) (Figure 1), rupture of chest wall metastasis of HCC was diagnosed. Therapeutic angiography was performed, and TAE procedures were performed using digital subtraction angiography. After percutaneous insertion of a 4-French sheath (Super Sheath, Medikit, Tokyo, Japan) via the right common femoral artery, aortography was performed using a 4-French pigtail catheter placed at the aortic arch. Tumor stain and extravasation of contrast agent were recognized involving the right fourth and fifth intercostal arteries (Figure 2). Next, a 4-French shepherd hook catheter was inserted into the right fourth and fifth intercostal arteries, with a microcatheter (2.0-Fr tip Sniper 2, Clinical Supply, Gifu, Japan) advanced coaxially into the distal site of the right fourth and fifth intercostal arteries for insertion. The embolic agent used was gelatin sponge particles. In order to avoid non target embolization by backflow, we didn’t use n-butyl 2-cyanoacrylate. Gelatin sponge particles mixed with 10 mL of saline solution, 10 mL of contrast medium (iopamidol), and one half sheet of Spongel (Spongel, Astellas Pharma, Tokyo, Japan) were administered using the pumping method. The size of most gelatin sponge particles was approximately 1 mm. Thereafter, gelatin sponge particles were infused very slowly under fluoroscopy until the tumor stain disappeared and the distal portions of the right fourth and fifth intercostal arteries were completely occluded on fluoroscopy. Then, the right fifth intercostal artery was embolized with metallic coils (Tornado Embolization Microcoil, 2/4 mm, COOK MEDICAL). Finally, no tumor stain and no further extravasation of contrast from the right fourth and fifth intercostal arteries were observed on selective angiography (Figure 3). After embolization, the patient recovered from shock. No rebleeding and no complications, such as chest wall necrosis or nerve disorders, occurred during the follow-up period. Later, radiation therapy (50 gray/25 fractions) to the chest wall metastasis was performed, and the tumor volume decreased. On enhanced CT 2 and 9 mo after TAE (Figure 4), the volume of the chest wall metastasis had decreased. Although the lung metastasis and bone metastases deteriorated further, the patient is still alive 15 mo after TAE.
Figure 1.
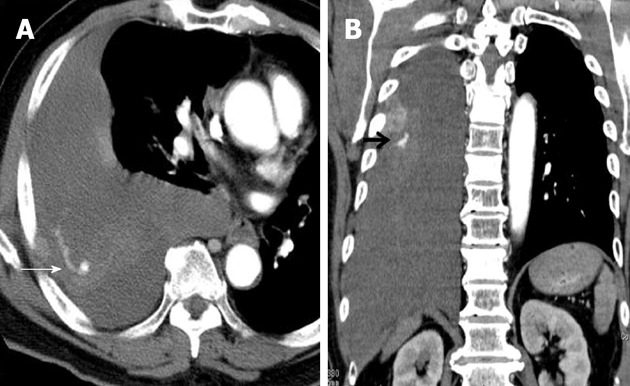
Contrast-enhanced computed tomography shows massive right hemothorax, tumor stain, and extravasation of contrast agent (arrow) in the right chest wall.
Figure 2.
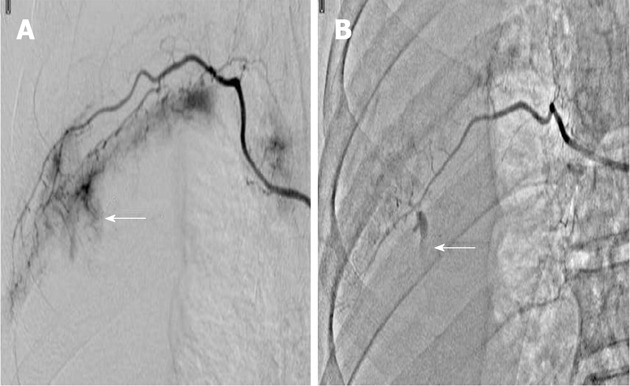
Arteriography shows tumor stain and extravasation of contrast agent (arrows). A: Right fourth intercostal artery; B: Right fifth intercostal artery.
Figure 3.

After embolization with gelatin sponge particles and isolation with microcoils, arteriography shows disappearance of the tumor stain and extravasation of contrast agent. A: Right fourth intercostal artery; B: Right fifth intercostal artery.
Figure 4.
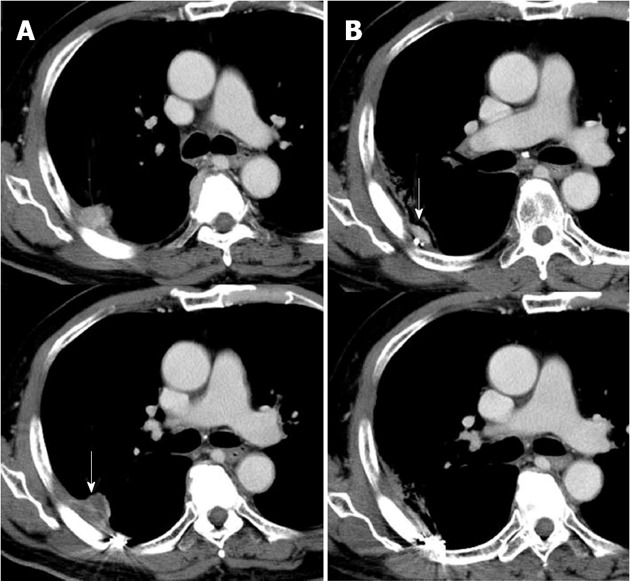
Contrast-enhanced computed tomography shows residual tumor stain in the right chest wall, it shows decreased tumor volume from radiation treatment (arrow). A: Two months after transcatheter arterial embolization (TAE); B: 9 mo after TAE.
DISCUSSION
Hemothorax is the presence of a significant amount of blood in the pleural space. The most common cause of hemothorax is trauma. Other various etiologies include neoplasm (primary or metastatic), dissecting aortic aneurysm, coagulation disorders, pulmonary embolism with infarction, and some lung diseases[1]. Surgical intervention is indicated in cases of massive hemothorax.
HCC has a high potential for metastasis. The most frequent sites of HCC metastases are the lung, lymph nodes, adrenal gland, and bones[2]. Metastatic HCCs, like their primaries, are usually hypervascular and may rupture spontaneously or secondary to trauma and cause massive hemorrhage.
The incidence of spontaneous rupture of HCC is less than 3% in Europe and the United States, but since the prevalence of hepatitis B virus and hepatitis C virus infection is higher in the Asian region, the incidence is much higher (12%-14%) in Asia. As a reference, the incidence was 10% in Japan[3]. The death rate by rupture is over 50%; spontaneous rupture of HCC can be a fatal event in patients with advanced tumor stage and poor liver function. There is a report that TAE for ruptured HCC can result in long-term and even tumor-free survival[4]. Although there are many reports of hemothorax after radiofrequency ablation, case reports of hemothorax due to pleural dissemination and rupture of chest wall metastases of HCC can only be seen occasionally (Table 1)[5-11]. The death rate at the time of symptom occurrence, however, was high. In two reports, surgery was performed for hemothorax from ruptured metastases, but these two patients died 6 d and 3 mo after intervention, respectively. In only one report, TAE was performed for hemothorax for ruptured HCC. Although the hemothorax could be controlled, and rebleeding was not observed after TAE, the patient died after 3 mo due to exacerbation of the HCC. In the present case, a good hemostatic effect for hemorrhagic shock caused by rupture of chest wall metastasis of HCC was obtained with TAE. There was no rebleeding or complications, such as chest wall necrosis or nerve disorders, after TAE. In addition, radiation therapy resulted in favorable local control. Radiotherapy has been widely used in patients with primary or metastatic chest wall tumors[12]. Radiotherapy with a total dose of 50 Gy in 20 fractions followed by TAE was successfully used in one patient with metastatic chest wall HCC[13].
Table 1.
List of the repoted cases of ruptured hepatocellular carcinoma (metastasis)
| Ref. | Age (yr)/gender | Meta | Symptom | Treatment | Outcome |
| This report | 70/M | Chest wall metastasis | Dyspnea shock | TAE intercostal artery | 17 mo alive |
| Wei et al[5] | 42/M | Chest wall metastasis | Massive hemoptysis | Tube thoracotom surgery | 6 d die MOF |
| Sohara et al[6] | 64/F | Chest wall metastasis | Hypotension | Conservative | 1 d die hypovolemic shock |
| Ogata et al[7] | 64/M | Rib metastasis | Right chest pain | Conservative | 27 h die respiratory and liver failure |
| Takagi et al[8] | 70/F | Pleural metastasis | Dyspnea | Conservative | 2 wk die respiratory failure |
| Akimaru et al[9] | 67/M | Lung metastasis | Dyspnea palpitation | Conservative | 36 h die |
| Masumoto et al[10] | 64/M | Pleural dissemination | Pleural effusion | TAE RIPA | 3 mo die HCC progression |
| Kamiyoshihara et al[11] | 68/M | Rib metastasis | Chest pain | Rib resection | 3 mo die bone meta |
M: Male; F: Female; MOF: Multiple organ failure; RIPA: Right inferior phrenic artery; TAE: Transcatheter arterial embolization; HCC: Hepatocellular carcinoma.
A rare case of hemorrhagic shock due to rupture of a chest wall metastasis of HCC in which TAE was life-saving was reported.
Footnotes
P- Reviewer Loffroy R S- Editor Gou SX L- Editor A E- Editor Xiong L
References
- 1.Martinez FJ, Villanueva AG, Pickering R, Becker FS, Smith DR. Spontaneous hemothorax. Report of 6 cases and review of the literature. Medicine (Baltimore) 1992;71:354–368. [PubMed] [Google Scholar]
- 2.Graeber GM, Snyder RJ, Fleming AW, Head HD, Lough FC, Parker JS, Zajtchuk R, Brott WH. Initial and long-term results in the management of primary chest wall neoplasms. Ann Thorac Surg. 1982;34:664–673. doi: 10.1016/s0003-4975(10)60906-x. [DOI] [PubMed] [Google Scholar]
- 3.Rustgi VK. Epidemiology of hepatocellular carcinoma. Gastroenterol Clin North Am. 1987;16:545–551. [PubMed] [Google Scholar]
- 4.Tarantino L, Sordelli I, Calise F, Ripa C, Perrotta M, Sperlongano P. Prognosis of patients with spontaneous rupture of hepatocellular carcinoma in cirrhosis. Updates Surg. 2011;63:25–30. doi: 10.1007/s13304-010-0041-8. [DOI] [PubMed] [Google Scholar]
- 5.Wei YF, Wang HC, Chang YC. Hemothorax due to metastatic hepatocellular carcinoma presenting with massive hemoptysis. J Formos Med Assoc. 2006;105:346–348. doi: 10.1016/S0929-6646(09)60127-3. [DOI] [PubMed] [Google Scholar]
- 6.Sohara N, Takagi H, Yamada T, Abe T, Mori M. Hepatocellular carcinoma complicated by hemothorax. J Gastroenterol. 2000;35:240–244. doi: 10.1007/s005350050337. [DOI] [PubMed] [Google Scholar]
- 7.Ogata H, Tsuji H, Hashiguchi M, Azuma K, Shimono J, Fujishima M. Hepatocellular carcinoma with metastasis to the rib complicated by hemothorax. An autopsy case. Fukuoka Igaku Zasshi. 1999;90:342–346. [PubMed] [Google Scholar]
- 8.Takagi H, Shimoda R, Uehara M, Takayama H, Yamada T, Ojima T, Abe T, Mori M, Takehara K, Suka K, et al. Hepatocellular carcinoma with pleural metastasis complicated by hemothorax. Am J Gastroenterol. 1996;91:1865–1866. [PubMed] [Google Scholar]
- 9.Akimaru K, Miyairi K, Tanaka H, Imai S, Iwase I, Uchiyama K, Shibuya T, Shoji T. A rupture of lung metastasis of hepatocellular carcinoma causing haemothorax. J Gastroenterol Hepatol. 1993;8:613–615. doi: 10.1111/j.1440-1746.1993.tb01661.x. [DOI] [PubMed] [Google Scholar]
- 10.Masumoto A, Motomura K, Uchimura K, Morotomi I, Morita K. Case Report: haemothorax due to hepatocellular carcinoma rupture successfully controlled by transcatheter arterial embolization. J Gastroenterol Hepatol. 1997;12:156–158. doi: 10.1111/j.1440-1746.1997.tb00399.x. [DOI] [PubMed] [Google Scholar]
- 11.Kamiyoshihara M, Ibe T, Takeyoshi I. Hepatocellular carcinoma associated with hemorrhaging from iatrogenic rupture of a rib metastasis. Gen Thorac Cardiovasc Surg. 2009;57:49–52. doi: 10.1007/s11748-008-0320-1. [DOI] [PubMed] [Google Scholar]
- 12.Torre W, Rodriguez-Spiteri N, Sierrasesumaga L. Current role for resection of thoracic metastases in children and young adults--do we need different strategies for this population? Thorac Cardiovasc Surg. 2004;52:90–95. doi: 10.1055/s-2004-817811. [DOI] [PubMed] [Google Scholar]
- 13.Yamanaka T, Shiraki K, Ito T, Sugimoto K, Sakai T, Ohmori S, Takase K, Nakano T. Transcatheter arterial embolization and extrabeam radiation therapy for subcutaneous seeding of hepatocellular carcinoma by percutaneous ethanol injection. Hepatogastroenterology. 2002;49:1656–1658. [PubMed] [Google Scholar]


