Abstract
Here, we report an extremely rare case of acquired nasolacrimal duct obstruction caused by oncocytic carcinoma. A 64-year-old man presented to the hospital complaining of epiphora and left-side nasal obstruction. Ophthalmic and otolaryngology examination revealed a left lacrimal duct obstruction caused by a mass in the left nasal cavity and lacrimal drainage system. The mass was removed and confirmed as an oncocytic carcinoma. Nine months after surgery, without adjuvant radiotherapy, a left orbital mass was observed and the patient underwent reoperation. The mass proved to be recurrent oncocytic carcinoma. The patient underwent adjuvant radiotherapy to eradicate any residual tumor and the patient remains tumor-free one year post-radiotherapy.
Keywords: Nasolacrimal duct, Oxyphilic adenoma
Oncocytic carcinoma, also referred to as malignant oncocytoma or oncocytic adenocarcinoma, is an extremely rare malignant tumor of the head and neck. Approximately 60 cases of oncocytic carcinoma have been reported to date, and most oncocytic carcinoma lesions involve the salivary glands [1]. In the present paper, we discuss a case of nasolacrimal duct obstruction caused by oncocytic carcinoma and management of this unusual malignancy in the nasolacrimal duct.
Case Report
A 64-year-old man was referred to the ophthalmology department of Pusan National University Hospital for evaluation of tearing, nasal obstruction, and trifling epistaxis of the left side that had arisen 12 months earlier. His medical history was free of allergies, chronic sinusitis, and rhinologic pathologies. Ophthalmologic examination confirmed mild swelling in the left medial canthal area and obstruction in the area of the left lacrimal duct (Fig. 1A). Visual acuity, intraocular pressure, ocular motility, and the anterior segment were within normal limits. There was no exophthalmos. The patient was referred to the otolaryngology department, and nasal endoscopies revealed the presence of a diffuse, smooth, and flush swelling mass in the inferior meatus. Computed tomography (CT) revealed that the tumor extended from inferior meatus to the entire length of the left nasolacrimal duct and sac, with involvement of the medial wall of the maxillary sinus (Fig. 1B). We observed neither regional lymph node involvement nor metastasis to other organs. We performed external dacryocystectomy to remove the lacrimal sac and proximal nasolacrimal duct and endoscopic inferior medial maxillectomy, including medial wall of maxillary sinus, inferior turbinate, and lateral wall of nasal cavity.
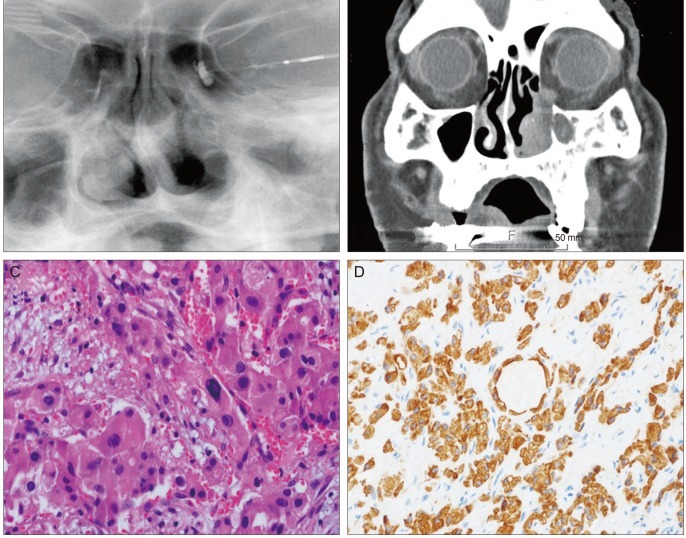
Fig. 1.
(A) Left dacryocystography demonstrates nasolacrimal duct obstruction. (B) Computed tomography revealed that the tumor in the left nasal cavity extended to the nasolacrimal duct and sac, and that the mass did not extend into the orbit. (C) Histological examination of the tumor revealed an oncocytic carcinoma; a destructive, infiltrating pattern and tumor cells composed of eccentrically located nuclei with abundant eosinophilic cytoplasm (hematoxylin-eosin, ×400). (D) Pancytokeratin is strongly positive in tumor cells.
Microscopically, the tumor demonstrated a destructive, infiltrative growth pattern and was composed of numerous irregular small nests of pleomorphic oncocytic epithelial cells with abundant eosinophilic cytoplasm. It was positive for pancytokeratin (Fig. 1C and 1D). Adjuvant radiotherapy was recommended to the patient after surgery, but the patient refused further treatment. Nine months after surgery, the patient complained of purulent discharge with tearing, swelling, and tenderness in the medial canthal area of the left eye. An orbital CT revealed a mass in the medial orbital wall (Fig. 2A).
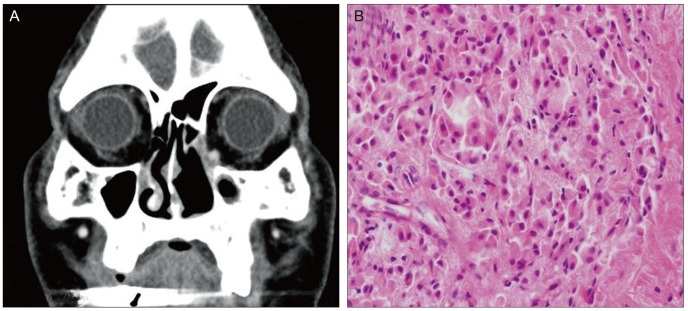
Fig. 2.
(A) Orbital computed tomography demonstrated an orbital mass located in the medial wall of the left orbit. (B) The recurrent tumor demonstrates the same morphology as the original tumor. The recurrent tumor is also composed of oncocytic epithelial cells with abundant eosinophilic cytoplasm (hematoxylin-eosin, ×400).
The orbital mass was removed through an inferior transconjunctival approach, and histological examination confirmed oncocytic carcinoma recurrence (Fig. 2B). The patient was referred for adjuvant radiotherapy to eradicate any residual tumor. He received computer controlled radiation therapy as 60 Gy in 33 fractions over 8 weeks. The patient remains free of tumor recurrence after 1 year.
Discussion
Although a neoplastic acquired nasolacrimal duct obstruction is an unusual condition, most of these tumors (75% to 90%) are malignant [2]. Clinically, the presence of some specific signs, such as bloody reflux, epistaxis, failure of dacryocystorhinostomy, and a palpable mass above the medial canthal tendon, are helpful for diagnosing tumors of the lacrimal sac and nasolacrimal duct. A history of malignancy, especially of sinus or nasopharyngeal origin, also warrants further investigation into this unusual situation. However, a neoplasm should be considered in any patient presenting with nasolacrimal duct obstruction, and the most essential element in the early diagnosis and initiation of treatment is awareness of these rare clinical features.
An oncocytic neoplasm is characterized by abundant, granular and eosinophilic cytoplasm, due to increased numbers of mitochondria, which are the most characteristic features of an oncocyte [1,3]. Diagnosis of malignancy in oncocytomas depends on the criteria defined by Gray et al. [4] destructive, infiltrating growth; cellular pleomorphism with scattered mitoses; lymphovascular or perineural invasion; regional or distant metastasis. Most of these carcinomas develop de novo, although malignant transformations of preexisting oncocytomas after long intervals have been reported [5].
The majority of oncocytic tumors in the head and neck arise in the parotid gland, though they can arise in the minor salivary and seromucous glands [3,5,6]. We assumed that the tumor in the current patient originated from a seromucous gland in the sinonasal tract, and enlarged and invaded into the nasolacrimal duct and sac.
A malignant oncocytoma is a rare tumor of the head and neck; approximately 60 cases of oncocytic carcinomas have been reported to date and the majority of these involved the major salivary gland [1,3]. A nasal cavity oncocytic carcinoma is an extremely rare condition. To our knowledge, 14 cases of oncocytic carcinoma arising in the nasal cavity have been reported, and details of previous reports and the current case are given in Table 1.
Table 1.
Reports of oncocytic carcinoma in the nasal cavity
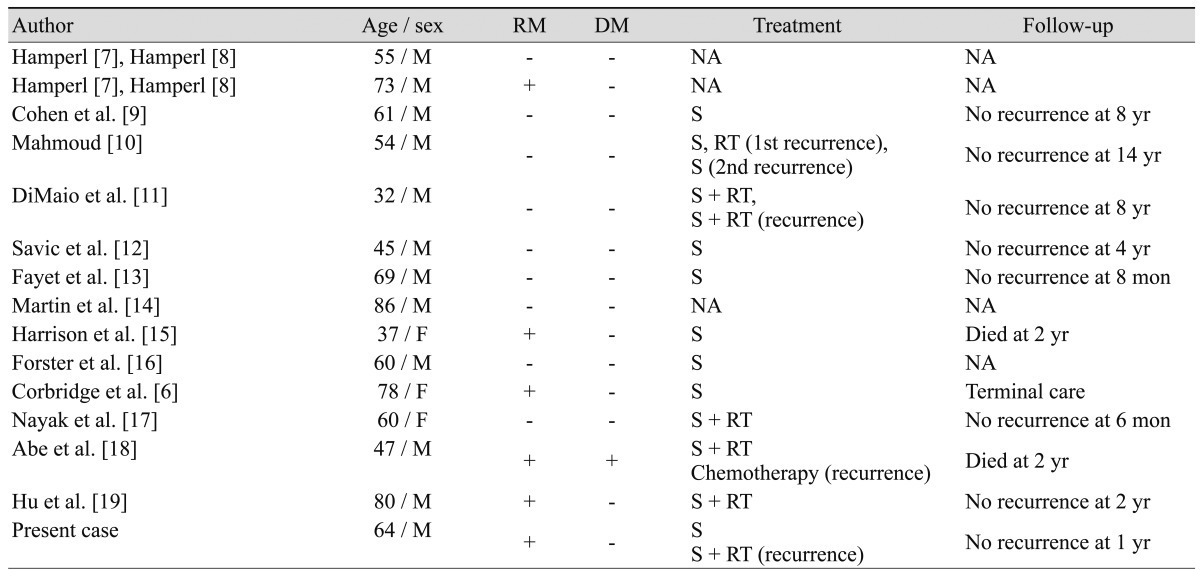
RM = regional metastasis; DM = distance metastasis; NA = not available; S = surgery; RT = radiotherapy.
Oncocytic carcinomas in the head and neck are a high grade neoplasm and appear aggressive from the onset: almost 85% of oncocytic carcinomas develop regional or distant metastases and 32% develop local recurrence [3]. Wide, complete local excision is the treatment of choice, and adjuvant radiation therapy should be strongly considered to prevent recurrence. Due to the rarity of these tumors affecting nasal cavity and nasolacrimal duct, the pattern of clinical behavior and long-term follow-up is difficult to predict. However, postoperative radiation therapy has been demonstrated to reduce local recurrence rates in parotid gland malignancies and previous case reports [3,17,19]. We hypothesize that delayed radiotherapy may explain the local recurrence in the present patient.
Although tumors of the lacrimal sac and nasolacrimal duct are rare, physicians must consider the possibility of lacrimal sac tumors, nasolacrimal duct tumors, or other nasal cavity pathology, such as an oncocytic carcinoma, whenever symptoms are not typical.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Wakely PE., Jr Oncocytic and oncocyte-like lesions of the head and neck. Ann Diagn Pathol. 2008;12:222–230. doi: 10.1016/j.anndiagpath.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Anderson NG, Wojno TH, Grossniklaus HE. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2003;19:173–176. doi: 10.1097/01.iop.0000066646.59045.5a. [DOI] [PubMed] [Google Scholar]
- 3.Gnepp DR, Henley JD, Roderick HW. Salivary and lacrimal glands: oncocytic lesions and tumors. In: Gnepp DR, editor. Diagnostic surgical pathology of the head and neck. Philadelphia: Saunders Elsevier; 2009. pp. 413–561. [Google Scholar]
- 4.Gray SR, Cornog JL, Jr, Seo IS. Oncocytic neoplasms of salivary glands: a report of fifteen cases including two malignant oncocytomas. Cancer. 1976;38:1306–1317. doi: 10.1002/1097-0142(197609)38:3<1306::aid-cncr2820380333>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 5.Nakada M, Nishizaki K, Akagi H, et al. Oncocytic carcinoma of the submandibular gland: a case report and literature review. J Oral Pathol Med. 1998;27:225–228. doi: 10.1111/j.1600-0714.1998.tb01946.x. [DOI] [PubMed] [Google Scholar]
- 6.Corbridge RJ, Gallimore AP, Dalton CG, O'Flynn PE. Oncocytomas of the upper jaw. Head Neck. 1996;18:374–380. doi: 10.1002/(SICI)1097-0347(199607/08)18:4<374::AID-HED9>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 7.Hamperl H. Benign and malignant oncocytoma. Cancer. 1962;15:1019–1027. doi: 10.1002/1097-0142(196209/10)15:5<1019::aid-cncr2820150519>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 8.Hamperl H. Onkocytoma of the salivary glands. Z Krebsforsch. 1962;64:427–440. [PubMed] [Google Scholar]
- 9.Cohen MA, Batsakis JG. Oncocytic tumors (oncocytomas) of minor salivary glands. Arch Otolaryngol. 1968;88:71–73. doi: 10.1001/archotol.1968.00770010073013. [DOI] [PubMed] [Google Scholar]
- 10.Mahmoud NA. Malignant oncocytoma of the nasal cavity. J Laryngol Otol. 1979;93:729–734. doi: 10.1017/s0022215100087612. [DOI] [PubMed] [Google Scholar]
- 11.DiMaio SJ, DiMaio VJ, DiMaio TM, et al. Oncocytic carcinoma of the nasal cavity. South Med J. 1980;73:803–806. doi: 10.1097/00007611-198006000-00041. [DOI] [PubMed] [Google Scholar]
- 12.Savic D, Djeric D, Jasovic A. Oncocytoma of the nose and ethmoidal and sphenoidal sinuses. Rev Laryngol Otol Rhinol (Bord) 1989;110:481–483. [PubMed] [Google Scholar]
- 13.Fayet B, Bernard JA, Zachar D, et al. Malignant nasal oncocytoma disclosed by mucocele of the lacrimal sac with hemolacrimia. J Fr Ophtalmol. 1990;13:153–158. [PubMed] [Google Scholar]
- 14.Martin H, Janda J, Behrbohm H. Locally invasive oncocytoma of the nasal cavity. Zentralbl Allg Pathol. 1990;136:703–706. [PubMed] [Google Scholar]
- 15.Harrison DF, Lund VJ. Tumours of the upper jaw. Edinburgh: Churchill Livingstone; 1993. p. 108. [Google Scholar]
- 16.Forster C, Ostertag H. Oncocytoma of the nose: a case report and review of the literature. Pathologe. 1995;16:431–433. doi: 10.1007/s002920050126. [DOI] [PubMed] [Google Scholar]
- 17.Nayak DR, Pillai S, Balakrishnan R, et al. Malignant oncocytoma of the nasal cavity: a case report. Am J Otolaryngol. 1999;20:323–327. doi: 10.1016/s0196-0709(99)90035-2. [DOI] [PubMed] [Google Scholar]
- 18.Abe T, Murakami A, Nakajima N, et al. Oncocytic carcinoma of the nasal cavity with widespread lymph node metastases. Auris Nasus Larynx. 2007;34:393–396. doi: 10.1016/j.anl.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 19.Hu YW, Lin CZ, Li WY, et al. Locally advanced oncocytic carcinoma of the nasal cavity treated with surgery and intensity-modulated radiotherapy. J Chin Med Assoc. 2010;73:166–172. doi: 10.1016/S1726-4901(10)70033-2. [DOI] [PubMed] [Google Scholar]