Abstract
Both researchers and oversight committees share concerns about patient safety in the study-related assessment of suicidality. However, concern about assessing suicidal thoughts can be a barrier to the development of empirical evidence that informs research on how to safely conduct these assessments. A question has been raised if asking about suicidal thoughts can result in iatrogenic increases of such thoughts, especially among at-risk samples. The current study repeatedly tested suicidal ideation at 6-month intervals for up to 2-years. Suicidal ideation was measured with the Suicidal Ideation Questionnaire Junior, and administered to adolescents who had previously received inpatient psychiatric care. Change in suicidal ideation was tested using several analytic techniques, each of which pointed to a significant decline in suicidal ideation in the context of repeated assessment. This and previous study outcomes suggest that asking an at-risk population about suicidal ideation is not associated with subsequent increases in suicidal ideation.
Keywords: Suicidal Ideation, Adolescent, Assessment, Safety, Ethics
Participant safety is the foremost consideration when conducting research with suicidal or potentially suicidal individuals. Inquiring about a participant’s level of suicidal thoughts or behaviors is typically an inherent component to studying these processes. In a clinical setting, asking these types of questions is a necessary standard of care for effective treatment of the patient. However, in observational studies that do not offer the benefit of a treatment or intervention, legitimate questions are raised regarding the risk imparted by asking about suicidal thoughts or behaviors (i.e., an iatrogenic effect). Might asking questions about suicide cause the participant to ruminate on suicidal thoughts or act out suicidal behaviors? This question is of importance to both researchers concerned for the ethical care of their study participants and also regulatory bodies, like institutional review boards, tasked with ensuring participant safety compliance. In a survey of ethics committees (i.e., institutional review boards) about conducting suicide research, the most commonly cited concern was whether asking about suicidality might exacerbate or reinforce such thoughts or behaviors (Lakeman & FitzGerald, 2009). Even though regulatory bodies increasingly express rigorous evaluation of patient safety for studies involving suicidal thoughts or behaviors, there are few empirical studies testing the effects of suicide assessment on subsequent suicidality that might inform these safety questions (Deeley & Love, 2010). The purpose of the current study was to test outcomes of repeated assessment of suicidal ideation over time among adolescents who have received inpatient psychiatric care.
The effects of asking questions about suicidal thoughts and behaviors have rarely been reported in the research literature (Deeley & Love, 2010). A handful of studies have reported that, at the time of the assessment about suicidal ideation, there are either infrequent, small (Deeley & Love, 2010; Langhinrichsen-Rohling, Arata, O’Brien, Bowers, & Klibert, 2006), or no negative (Gould et al., 2005) impact on mood states in general. More specific to the question, one recent study (“Does Participating in a Research Protocol on Suicide and Psychiatric Symptoms Increase Suicide Ideation and Attempts?” Cukrowicz et al., 2010) tested whether asking about suicidality is related subsequent suicidal thoughts or behaviors. In this study, depressed adults were initially assessed with the Beck Scale for Suicidal Ideation along with other measures of mood. Then a subgroup (n = 21) were assessed via telephone approximately 1 and 3 months later and asked open-ended questions of whether they had experienced a change in thoughts about death/suicide or attempted suicide since their initial assessment. The primary outcomes of this study were: (1) the majority of participants experienced a reduction in suicidal ideation from baseline to 1 month follow-up, and experienced no change in suicidal ideation between 1 and 3 month follow-ups; and (2) none of the research participants experienced an increase in suicidal ideation or behaviors across follow-ups (Cukrowicz et al., 2010). This outcome was interpreted as suggesting that basic, non-treatment research on suicidal ideation is not associated with subsequent suicidal behaviors among depressed adults.
The purpose of the current study was to extend research on changes in suicidal thoughts in the context of repeated assessments of suicidal ideation. The current study assessed suicidal ideation among a clinical sample of adolescents who have received inpatient psychiatric care. Suicidal ideation was assessed initially after hospitalization, and then reassessed at 6-month intervals for up to 2 years. We were interested in testing the relationship between repeated assessment of suicidal ideation and change in suicidal ideation over time.
Methods
Participant Recruitment
Adolescents who had experienced psychiatric inpatient care were recruited for this study from both admissions to local adolescent psychiatric inpatient units and from advertisements broadcast in South Central Texas. Regardless of recruitment source, potential participants completed a brief screening regarding general demographic and health characteristics. Participants were included if they were between the ages of 12–17 years old, had received inpatient psychiatric care, and a parent/guardian was willing to participate in the study. Participants were excluded if: they had a past or present medical condition affecting the central nervous system (e.g. seizure disorder or loss of consciousness for > 20 minutes), they had low intellectual functioning (i.e. IQ < 70; Weschler Abbreviated Scale of Intelligence™, The Psychological Corporation, 1999), they had psychotic symptoms that would interfere with the ability to complete the self-report assessments, if they already had a sibling in the study, or if they or their parent could not speak English.
Respondents who were in the target age range, who reported inpatient psychiatric care for themselves or their adolescent (in the case of parent respondents), and who were interested in participating were invited for an initial onsite interview. The interview commenced with an informed consent process that outlined: the purpose of the study, the procedures involved in the assessment of clinical symptoms/behaviors, and procedures for intervening during the study if a patient was at imminent risk of harm to self and/or others. It was explained that this was not a “for benefit” study, meaning that no treatment was provided as part of the study. Those who consented to participate completed a health interview, measures of demographic characteristics, and a variety of clinical questionnaires as part of a larger longitudinal study of adolescent development and psychiatric symptoms.
Participants
The sample was composed of a diverse group (N = 170) of adolescents who had previously been treated in an inpatient psychiatric setting; and as such had wide ranging scores on measures of suicidal ideation at study entry (M = 24.5, SD = 21.9, range 0–79). There were 85 boys and 85 girls who were on average 14 years old (SD = 1.6) and the majority of the sample identified themselves as Hispanic (57% Hispanic, 22% White, 7% African American, 12% more than one race, and 2% of unknown race). Suicidal ideation was tested in the current sample of former psychiatric inpatients within the context of their routine psychiatric care occurring outside the study (i.e. a “treatment-as-usual” sample), which varied widely in terms of intensity (repeated inpatient, outpatient, IOP), frequency/duration, and modality (pharmacotherapy, counseling) of intervention during the course of their time in the study.
Procedures and Materials
Adolescents were assessed at study entry and then re-assessed in-person again at 6-month intervals for a period of up to 2 years (i.e. up to 5 assessments). At each visit, ongoing informed consent was evaluated and suicidal ideation was assessed. Of the 170 adolescents completing the initial visit, 159 completed the second assessment (at 6-months), 126 completed the third assessment, 77 completed the fourth assessment, and 54 completed all 5 assessments. Of those with missed assessments, 3 participants were lost due to attrition all after their 6-month visit. All other missing visits were due to the ongoing nature of the study (i.e. these participants had not been in the study long enough for their later visits to have occurred at the time of this analysis).
Suicidal ideation was assessed throughout the study using the Suicide Ideation Questionnaire Junior (SIQ-JR; Reynolds, 1988). The SIQ-JR is a 15-item self-report questionnaire that is widely used to assess adolescent suicidal ideation (e.g., Becker-Weidman, Jacobs, Reinecke, Silva, & March, 2010; Emslie et al., 2006; Kaminer, Burleson, Goldston, & Burke, 2006; King, Hovey, Brand, & Wilson, 1997; King, O’Mara, Hayward, & Cunningham, 2009; Reynolds & Mazza, 1999). Each item examines a specific suicidal thought (e.g. “I thought about how I would kill myself,” or “I thought about telling people I plan to kill myself”) and the adolescent rates the frequency that the thoughts have occurred over the past month on a 7-point scale ranging from 0 (“I never had this thought”) to 6 (a thought occurred “almost every day”). A total scale score was computed as the primary dependent variable in the current study; the total score can range from 0 to 90, with scores over 30 reflecting increased suicide risk (Reynolds, 1988). The SIQ-JR is a stable measure of suicidal ideation over one to two month periods of time (test-retest reliability = .72 to .89; Reynolds, 1988; Reynolds & Mazza, 1999) and previous research has shown the SIQ-JR predictive of future (6-months later) suicidal ideation among adolescent psychiatric inpatients (King et al., 1997).
Data Analyses
First, Pearson’s product moment correlations were computed for the number of assessments and final suicidal ideation score. This analysis was repeated, partialling the initial suicidal ideation score. Then, frequency analyses were used to test overall change in suicidal ideation across the study. Specifically, we calculated both the direction and magnitude of change for each individual’s suicidal ideation from their first to last assessment. Direction of change in suicidal ideation was defined as increased (more suicidal ideation in the last assessment than the first), no change, or decreased (less suicidal ideation in the last assessment than the first). Magnitude of change was defined in terms of effect sizes of change in suicidal ideation from first to last assessment. That is, each individual’s “magnitude of change” was defined in terms of the standard deviation units between the initial score and final score and in terms of commonly cited cut-off for effect sizes (Cohen, 1988): Large change = greater than 80% SD change from the initial assessment value to the last assessment value, Medium change = between 50% and 80% SD change from the initial assessment value, Small change = between 20% and 50% SD change from the initial assessment value, and No Change = less than 20% SD change from the initial assessment value. We then conducted frequency analyses, on direction and magnitude of change in suicidal ideation (similar to Cukrowicz et al., 2010).
Individual growth curve modeling was conducted to examine the two core questions. First, to reveal the patterns of change in suicidal ideation over time, we examined a set of multilevel random coefficient growth curve models that test an increasingly complex and nuanced perspective on change. Specifically, we began by evaluating the degree to which the average person in the sample experienced steady decreases in suicidal ideation with repeated assessment. We then examined two additional growth curve models that added the higher-order trend into each subsequent model. The linear model was defined as:
In this model, Yij represents person j’s suicidal ideation score at time i, and time is coded 0, 1, 2, 3, and 4, B0j reflects person j’s estimated initial suicidal ideation (i.e., his or her SIQ score at “Time 0”), B1j reflects the degree to which person j’s SIQ scores show a steady change across time (i.e., a positive B1j indicates a steady increase, and a negative B1j indicates a steady decrease). Of most general interest is G10 which reflects the average pattern of linear change across all participants. Subsequent models added terms reflecting decreases followed by a flattening change (quadratic), or alternating decreases and flattened trends (cubic) in suicidal ideation with repeated assessment (i.e., the square and cube of the time variable, respectively).
Second, to more comprehensively examine patterns of change in suicidal ideation, we also tested the possibility that participants’ initial levels of suicidal ideation affected their patterns of change with repeated assessment. That is, do adolescents who began the study with a relatively high level of suicidal ideation experience a different pattern of change in suicidal ideation with repeated assessment than those with initially lower levels of suicidal ideation? We examined this by extending the set of growth curve models to include participants’ initial suicidal ideation as well as interaction terms between initial suicidal ideation and each of the three potential patterns of change (i.e., linear, quadratic, and cubic). Again, each higher-order element was added in subsequent models. Ultimately, the most comprehensive model included predictors reflecting all three elements of change as well as initial status as a “cross-level” interaction term with each element of change:
Note that this model includes Initial SIQ score as a moderator of each component of change. We will use the parameter estimates from this comprehensive model to estimate and plot the patterns of change for participants who begin the study with various levels of suicidal ideation. [To avoid statistical redundancies and problems with the error variance/covariance matrix, we did not estimate a random component (u0j) for the G10 term in the full model]. Finally, to examine the influence of demographic characteristics on study outcomes, we also repeated multilevel random coefficient growth curve models to test for effect of completion status (including only those completing all 5 study visits), recruitment source (recruited via advertisements vs clinics), ethnicity (Hispanic vs non-Hispanic), age, and gender as predictors of suicidal ideation. Only the test of patients with all 5 study visits altered the relationship to change in suicidal ideation and is reported in the Results. All analyses were conducted via SAS 9.2.
Results
Correlation between Suicidal Ideation and Number of Assessments
There was a significant relationship between frequency of assessment and suicidal ideation at the end of the study. Being assessed more often was related to less suicidal ideation by the final assessment (r = −.20, p =.008), and this negative correlation remained significant even after accounting for suicidal ideation at study entry (partial r = −.22, p =.003).
Change in Suicidal Ideation from First to Last Assessment
The most common change in suicidal ideation from first to last assessment was a decrease in suicidal ideation. Overall, significantly more participants experienced a decrease in suicidal ideation than other patterns of change: about half (51%) of the sample experienced a decrease, whereas 29% experienced no change, and 21% experienced an increase in suicidal ideation from their first to last assessment (Chi-square = 24.51, df = 2, p < .001).
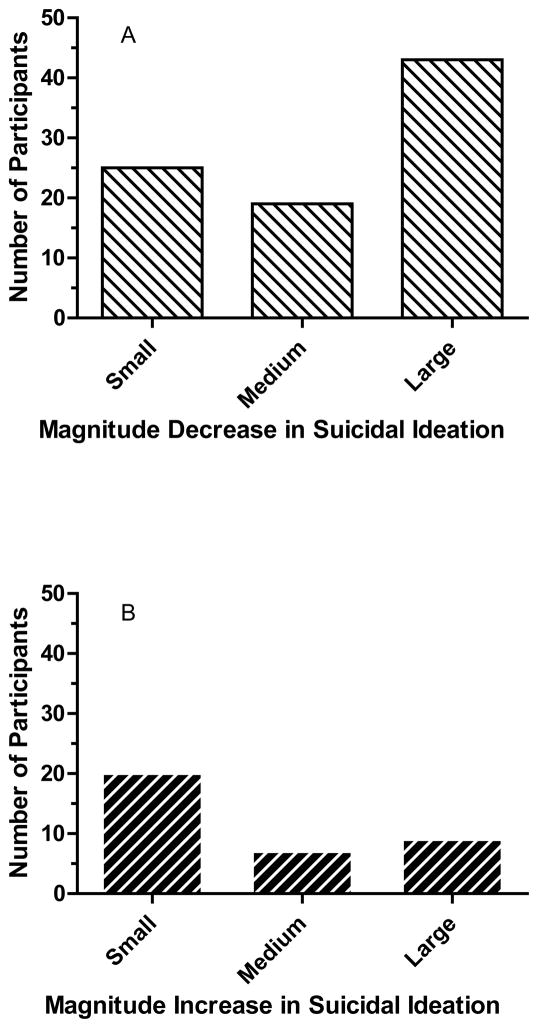
The magnitude of change varied based on whether suicidal ideation decreased or increased from first to last assessment. Among those who experienced decreased suicidal ideation, significantly more participants experienced large decreases than moderate decreases (Chi-square = 8.67, df = 1, p = .003) or small decreases (Chi-square = 4.31, df = 1, p = .04). In contrast, of those who experienced increased suicidal ideation, significantly more participants experienced small increases than moderate increases (Chi-square = 5.54, df = 1, p = .02) or large increases, though the latter difference only approached significance (Chi-square = 3.57, df = 1, p = .06). The number of participants who experienced small, medium, or large decreases (A) or increases (B) in suicidal ideation is shown in Figure 1.
Figure 1.
The number of adolescents with decreases (A) or increases (B) in suicidal ideation, classified by magnitude of change from first to last assessment.
Small effect 20–50%, medium 50–80%, and large > 80% SD group suicidal ideation change from first to last assessment.
Suicidal Ideation across Repeated Assessments
Suicidal ideation did not vary randomly throughout the study, but changed in a monotonically decreasing pattern. Had there been an absence of significant effects in the growth curve modeling, this would have suggested that there was no consistent pattern of change in suicidal ideation in the context of repeated assessment. However, there was in fact a significant, linear reduction in suicidal ideation across assessments, indicating a nearly 3 point decline in ideation per assessment (see Table 1 Model 1 Linear Slope = −2.95, p < .0001). The implication being that the adolescents experienced less suicidal ideation with each assessment. There are, however, two caveats to interpreting this decline with repeated assessment: (1) non-linear patterns of suicidal ideation change across repeated assessment; and (2) the influence of initial suicidal ideation scores on subsequent scores. Table 1’s Models 2–7 represent increasingly complex and comprehensive hierarchical examinations of these caveats; the key result for each model is the final slope (in bold) in its row. Model 7 is the most complete and complex growth curve model, taking into account all three patterns of change (linear, quadratic, and cubic) and their interaction with initial suicidal ideation simultaneously.
Table 1.
Patterns of Change in Suicidal Ideation: Individual Growth Curve Models
| Model & Novel Predictor | Intercept | Patterns of Change
|
Initial Status | Interaction with initial status
|
||||
|---|---|---|---|---|---|---|---|---|
| Linear | Quadratic | Cubic | Linear | Quadratic | Cubic | |||
| M1: Lin | 23.01*** | −2.95*** | ||||||
| M2: Quadratic | 23.92*** | −5.32*** | .69* | |||||
| M3: Cubic1 | 24.46*** | −10.51*** | 4.73** | −.71** | ||||
| M4: Initial Status2 | 24.47*** | −10.78*** | 5.13** | −.79** | .95*** | |||
| M5: Linear x Initial Status | 24.48*** | −10.47*** | 4.80** | −.73* | .97*** | −.19**** | ||
| M6: Quadratic x Initial Status | 24.48*** | −10.40*** | 4.69** | −.71* | .99*** | −.46**** | .07**** | |
| M7: Full Model | 24.48*** | −10.56*** | 4.84** | −.74* | .99*** | −.64**** | .22** | −.03+ |
Note.
p < .10,
p < .05,
p < .01,
p < .001.
In response to variance estimates in preliminary analyses, the cubic term was fixed, not random.
In response to variance estimates in preliminary analyses, the intercept was fixed in all subsequent models. In addition, Initial Status was grand-mean centered for all analyses.
Non-Linear Patterns of Suicidal Ideation Change
First, there was significant variation indicating that individuals differed in the degree to which they experienced a steady change in suicidal ideation with repeated assessment (Variance = 14.36, z = 3.66, p < .0001). In other words there were significant individual differences in the degree to which participants experienced a steady pattern of suicidal ideation change with repeated assessment. This led us to test other, non-linear, models of change in suicidal ideation over time. These tests revealed significant models indicating patterns of initial decreases with a flattening slope as suicidal ideation approached zero at the later assessments (Model 2 Quadratic Slope = .69, p < .05) or even patterns in suicidal ideation showing initial declines followed by flattening and later decline again across repeated assessments (Model 3 Cubic Slope = −.71, p < .01). The Model 2 and Model 3 rows of Table 1 present the intercept and slopes for these models.
Influence of Initial Suicidal Ideation on Subsequent Assessments
Second, the pattern of decline in suicidal ideation was contingent upon the level of suicidal ideation at study entry. Participants who began the study with higher levels of suicidal ideation showed greater significant decreases in suicidal ideation over time (Model 5 Linear Interaction Slope = −.19, p < .0001), meaning that, for participants who began the study with above-average levels of suicidal ideation, there were even greater declines in suicidal ideation, over and above the nearly 3-point linear decrease experienced by the average participant. More specifically, for every point above the average SIQ-JR score (M = 24.5) that a participant began the study with, the participant’s rate of decline was enhanced by approximately .20 points. In other words, while the average patient entering the study (with a mean initial suicidal ideation = 24) would be expected to experience a nearly 3 point decline in ideation with each repeated assessment, someone with an initial score of 34 would show a decline of 5 points in ideation over time. Seventy of the 170 patients had a suicidal ideation score of 34 or higher at study entry. Going further, results indicate that participants who began the study with higher levels of suicidal ideation showed significantly greater curvature in their pattern of change in suicidal ideation, whereas participants who began the study with lower levels of suicidal ideation showed a flatter, straighter pattern of SIQ-JR scores across the assessments (Model 6 Quadratic Interaction Slope = .07, p < .001; Model 7 Cubic Interaction Slope = −.03, p < .10).
The Comprehensive Model: Suicidal Ideation, Patterns of Change, and Initial Values
The most comprehensive model allowed for simultaneous influence of the different patterns of change in suicidal ideation and initial values on suicidal ideation measured over time. Taking into account all these influences, those participants entering the study: (1) with low levels of suicidal ideation tended to not experience meaningful increases in suicidal ideation with repeated assessment; (2) with average initial suicidal ideation generally experienced a decline only from the first to second assessment and no meaningful change thereafter; and (3) with the highest initial levels of suicidal ideation experienced a rapid decline during the first year of assessments (i.e. assessment 1, 2, and 3) followed by a more shallow decline in the second year (assessments 4 and 5). Again, Model 7 is the most complete and complex model, taking into account all three patterns of change in their interaction with initial suicidal ideation simultaneously. Based on estimates from Model 7, Figure 2a presents these patterns of change across repeated assessment (x-axis) plotted as a function of initial level of suicidal ideation (separate lines).
Figure 2.
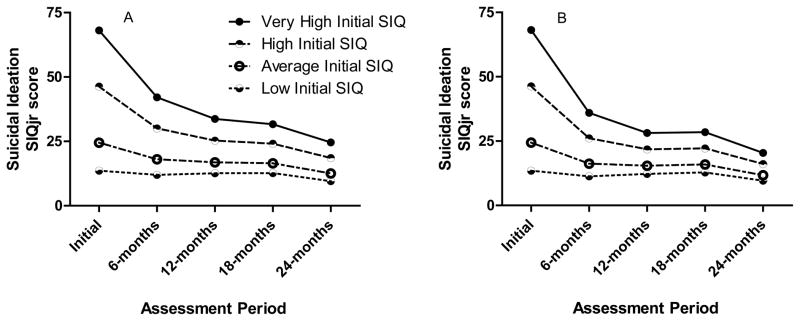
Pattern of change in suicidal ideation score plotted as a function of suicidal ideation at the study outset across 2-years of repeated assessments for the full sample (2a N = 170) and for those cases completing all 5 study visits (2b N = 54).
Very High = 2 SD above the average initial suicidal ideation value, High = 1 SD, Average = the average initial suicidal ideation value, and Low = 0.5 SD below the average initial suicidal ideation.
To explore patterns of suicidal ideation change in the absence of missing data, these analyses were repeated for only those cases completing all 5 assessments (n = 54). There was a slight change in the magnitude of decline of suicidal ideation described by the final model (Model 7) for those completing all assessments in comparison to the full sample (slope −.4, p < .01). Those cases with very high suicidal ideation and high initial change experienced a more robust decline than was found in the full sample, while those with average or low initial suicidal ideation declined less robustly (Figure 2b).
Discussion
This study tested patterns of change in self-reported suicidal ideation with repeated assessment across a period of up to two years. The primary outcome of the study was that repeated assessments of suicidal ideation were associated with decreases in suicidal ideation. This pattern was supported by findings that: (1) suicidal ideation at the end of the study was inversely related to the number of assessments; (2) the most common pattern of change was a large reduction in suicidal ideation from initial to last assessment; (3) there was a significant linear decrease in suicidal ideation in the context of repeated assessment; and (4) the magnitude of the linear decrease in suicidal ideation was modified by influence of other patterns of change (quadratic and cubic) and level of suicidal ideation at study entry.
A barrier to conducting research on suicidality has been the concern that asking questions about suicidal thoughts may result in an iatrogenic effect of subsequent suicidal ideation. The current study of adolescent-aged former inpatients builds on previous research with depressed adults (Cukrowicz et al., 2010) suggesting that there is no relationship between being repeatedly asked about suicidal thoughts and subsequent increased self-reported suicidal ideation. One proposed mechanism of reduction in suicidal ideation with repeated assessment has been that such research interactions provide an experience of interpersonal connectedness (Cukrowicz et al., 2010), a protective factor for suicidal behavior in the context of the Interpersonal Theory of Suicide (Van Orden et al., 2010). Alternatively, connectedness may promote a response bias for the participant to report what they think the experimenter anticipates with regard to suicidal ideation change over time (i.e., the good-subject effect, Nichols & Maner, 2008).
For the current sample, the observed reductions in suicidal ideation may just as likely have been the result of the patient’s usual care or regression-to-the-mean of suicidal ideation scores. Because we tested suicidal ideation among a high-risk group of former psychiatric inpatients, they were all receiving ongoing, routine psychiatric care that may have acted to reduce suicidal ideation over the course of the study. Given the current findings, future research may consider testing for the interaction of repeated assessment of suicidal ideation and psychiatric treatment (and types of treatment) on change in suicidal ideation. Furthermore, suicidal ideation has been conceptualized and measured as a state rather than a trait, which would be expected to fluctuate in intensity over time (Reynolds, 1988). The pattern of fluctuation in suicidal ideation observed in the current study (i.e. steepest reduction in suicidal ideation for those with the highest initial suicidal ideation scores) is consistent with a regression-to-the-mean outcome. Future research may consider randomized control trial methodology for intervention studies or lead-in assessment for observational studies to minimize regression-to-the-mean effects (see Yudkin & Stratton, 1996). While mechanisms of change are a question for future studies, the current findings support the interpretation that patient safety, as it pertains to thoughts of taking one’s own life, is not compromised by assessment of suicidal ideation in the context of participating in a non-treatment research study.
Besides concerns surrounding the safety of particular assessments, another ethical concern to be dealt with in studying high-risk samples is the inherent risks the sample poses to themselves. In other words, “The risk of suicide is not so much intrinsic to the research process as to the individual and population [being studied]” (Lakeman & FitzGerald, 2009; p. 15). Sometimes safety concerns about the sample are erroneously extended to the assessment process; the fear being that those with the highest level of suicide risk (in this case as measured by suicidal ideation) would be most susceptible to adverse impact of being asked about suicide. In fact, the current study found a robust relationship, such that those entering the study with the highest suicidal ideation experienced the greatest reductions in ideation in the context of repeated assessment.
While the current, and Cukrowicz et al., 2010, study outcomes offer encouragement that inquiring about suicidal ideation is not generally associated with later increases in suicidal thoughts, there are inherent challenges to drawing causal inferences about these outcomes. It is difficult to develop safe/ethical control groups for testing causal effects of suicidality assessment on subsequent suicidal thoughts and behaviors when working with at-risk groups. One previous study did develop a research design that safely employed a control group in a general population, screening setting (Gould et al., 2005). In this study, suicidal ideation screening was performed among a sample of high schoolers randomly assigned to one of two groups: an experimental group asked about mood and suicidal ideation twice (2 days apart) and a control group asked about mood the first day and mood plus suicidal ideation on the second assessment day. Suicidal ideation did not differ between the twice assessed (experimental) and once assessed (control) group (Gould et al., 2005). This approach allows for causal inferences to be drawn about the influence of asking about thoughts of suicide and subsequent changes in suicidal ideation. Further, this procedure was justified as safe in the general population screening context in which it was conducted; the sample was not selected on the basis of known risk factors for suicide that might have obligated the researchers to inquire about suicidal ideation at study outset. Applying this approach in the context of the current study would not have been safe. Failure to assess suicidal thoughts, or otherwise establish imminence of suicide risk, in a clinical sample (i.e. a population selected by virtue of their elevated suicide risk) is not ethically justified. The risks to safety outweigh the benefits of being able to draw causal inferences. Therefore, in the absence of proper control groups or ethical control conditions, causal relationships between questions of suicidal ideation and subsequent expression of suicidality among at-risk populations are not feasibly tested. As unsatisfying as this is, some would argue that this question misses the point of ethical research on suicidal thoughts and behaviors. The prevention and intervention fields have concluded that asking about suicidal ideation is a necessary and justifiably safe practice (Pearson et al., 2001): asking about suicidal ideation is a “best practice” for screening the general public and an accepted standard of care for patients. A better question for researchers to pursue may be to test “best practices” for what to do when elevated suicidal ideation is detected in a research setting. While recommended guidelines have been proposed for clinical trials and treatment studies (Pearson et al., 2001), there remain no clear guidelines for managing suicide risk in non-intervention research.
Interpretation of this study’s outcome must be tempered by its limitations. First and foremost, the study design did not allow for causal inferences to be drawn about repeated assessment and subsequent change in suicidal ideation. While there are safety issues inherent to the selection or treatment of a proper control group (described above), their inclusion is necessary for drawing causal inferences and interpreting the direction or magnitude of observed response. Second, the study did not test for mechanisms that might account for change in suicidal ideation observed over time. Consistent with the hypothesis the scope of the study was limited to a test for a relationship between suicidal ideation and repeated assessment, which was confirmed; a test that has been lacking in the literature despite debate about this topic (Cukrowicz et al., 2010). Third, the lack randomization or lead in methodologies precludes us from ruling out regression-to-the-mean as an explanation for the observed reduction in suicidal ideation. Fourth, the study focused solely on suicidal ideation, which is phenomonologically distinct from a suicide plan, suicide attempts, or suicide death (Silverman, Berman, Sanddal, O’Carroll, & Joiner, 2007). Finally, the study’s tests were conducted with a high-risk sample experiencing their usual psychiatric care delivered outside of the study; other outcomes may be expected in the general population or among those not receiving ongoing psychiatric care.
Conclusion
Participant safety is an issue inherent in research with populations at-risk for suicide. Both researchers and oversight committees are sensitive to the population risks and iatrogenic risks of suicide assessment (Lakeman & FitzGerald, 2006, 2009). The level of concern about these risks has not been matched by an outpouring of empirical tests of patient safety of suicidal populations or instruments. Indeed, fears for patient safety may discourage pursuit of empirical evidence necessary to advance our understanding of how to safely conduct research on suicidal thoughts and behaviors. The few studies that have tested safety issues regarding asking about thoughts of taking one’s own life suggest that this assessment is not associated with increases in suicidal ideation.
Acknowledgments
This project would not have been possible without the families donating their time to participate and for the local treatment facilities for their care. The authors would also like to acknowledge the work of Clarity Child Guidance Center (http://www.claritycgc.org/) for their mental health care of children and adolescents.
The authors also appreciate the supportive functions performed for this broader funded project (R01-MH077684) by our valued colleagues: Sharon Cates B.A., Michael A. Dawes M.D., Sarah J. Farris M.A., and Lisa M. James Ph.D.
This project was funded by grants from the National Institute of Mental Health (R01-MH077684). Dr. Dougherty gratefully acknowledges support from the William & Marguerite Wurzbach Distinguished Professorship and the University of Texas Star Program.
References
- Becker-Weidman E, Jacobs RH, Reinecke MA, Silva SG, March JS. Social problem-solving among adolescents treated for depression. Behaviour Research and Therapy. 2010;48:11–18. doi: 10.1016/j.brat.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cukrowicz K, Smith P, Poindexter E. The effect of participating in suicide research: Does participating in a research protocol on suicide and psychiatric symptoms increase suicidal ideation and attempts? Suicide and Life-Threatening Behavior. 2010;40:535–543. doi: 10.1521/suli.2010.40.6.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeley ST, Love AW. Does asking adolescents about suicidal ideation induce negative mood state? Violence and Victims. 2010;25:677–688. doi: 10.1891/0886-6708.25.677. [DOI] [PubMed] [Google Scholar]
- Emslie G, Kratochvil C, Vitiello B, Silva S, Mayes T, McNulty S, Weller E, Waslick B, Casat C, Walkup J, Pathak S, Rohde P, Posner K, March J Columbia Suicidality Classification Group, TADS Team. Treatment for Adolescents with Depression Study (TADS): safety results. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:1440–1455. doi: 10.1097/01.chi.0000240840.63737.1d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould MS, Marrocco FA, Kleinman M, Thomas JG, Mostkoff K, Cote J, Davies M. Evaluating iatrogenic risk of youth suicide screening programs: a randomized controlled trial. Journal of the American Medical Association. 2005;293:1635–1643. doi: 10.1001/jama.293.13.1635. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Goldston DB, Burke RH. Suicidal ideation among adolescents with alcohol use disorders during treatment and aftercare. The American Journal on Addictions. 2006;15:43–49. doi: 10.1080/10550490601006154. [DOI] [PubMed] [Google Scholar]
- King CA, Hovey JD, Brand E, Wilson R. Suicidal adolescents after hospitalization: parent and family impacts on treatment follow-through. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:85–93. doi: 10.1097/00004583-199701000-00021. [DOI] [PubMed] [Google Scholar]
- King CA, O’Mara RM, Hayward CN, Cunningham RM. Adolescent suicide risk screening in the emergency department. Academic Emergency Medicine. 2009;16:1234–1241. doi: 10.1111/j.1553-2712.2009.00500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakeman R, FitzGerald M. The ethics of suicide research: The views of ethics committee members. Crisis. 2006;30:13–19. doi: 10.1027/0227-5910.30.1.13. [DOI] [PubMed] [Google Scholar]
- Lakeman R, FitzGerald M. Ethical suicide research: a survey of researchers. International Journal of Mental Health Nursing. 2009;18:10–17. doi: 10.1111/j.1447-0349.2008.00569.x. [DOI] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Arata C, O’Brien N, Bowers D, Klibert J. Sensitive research with adolescents: just how upsetting are self-report surveys anyway? Violence and Victims. 2006;21:425–444. doi: 10.1891/vivi.21.4.425. [DOI] [PubMed] [Google Scholar]
- Nichols AL, Maner JK. The good-subject effect: investigating participant demand characteristics. The Journal of General Psychology. 2008;135:151–165. doi: 10.3200/GENP.135.2.151-166. [DOI] [PubMed] [Google Scholar]
- Pearson JL, Stanley B, King C, Fisher C. Intervention research with persons at high risk for suicidality. Safety and ethical considerations. Journal of Clinical Psychiatry. 2001;62:17–26. [PubMed] [Google Scholar]
- Reynolds W. Suicidal Ideation Questionnaire: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- Reynolds W, Mazza JJ. Assessment of suicidal ideation in inner-city children and young adolescents: Reliability and validity of the Suicidal Ideation Questionnaire-Jr. School Psychology Review. 1999;28:17–30. [Google Scholar]
- Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE., Jr Rebuilding the Tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors Part 1: Background, Rationale, and Methodology. Suicide and Life-Threatening Behavior. 2007;37:248–263. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychological Review. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yudkin PL, Stratton IM. How to deal with regression to the mean in intervention studies. Lancet. 1996;347:241–243. doi: 10.1016/s0140-6736(96)90410-9. [DOI] [PubMed] [Google Scholar]