Abstract
Background
The gap between the supply of organs available for transplantation and demand is growing, especially among ethnic groups.
Objective
To evaluate the effect of a video designed to address concerns of ethnic groups about organ donation.
Design
Cluster randomized, controlled trial. Randomization was performed by using a random-number table with centralized allocation concealment. Participants and investigators assessing outcomes were not blinded to group assignment. (ClinicalTrials.gov registration number: NCT00870506)
Setting
Twelve branches of the Ohio Bureau of Motor Vehicles in northeastern Ohio.
Participants
952 participants aged 15 to 66 years.
Intervention
Video (intervention; n = 443) or usual Bureau of Motor Vehicles license practices (control; n = 509).
Measurements
The primary outcome was the proportion of participants who provided consent for organ donation on a newly acquired driver’s license, learner’s permit, or state identification card. Secondary outcomes included willingness to make a living kidney donation to a family member in need and personal beliefs about donation.
Results
More participants who viewed the video consented to donate organs than control participants (84% vs. 72%; difference, 12 percentage points [95% CI, 6 to 17 percentage points]). The video was effective among black participants (76% vs. 54%; difference, 22 percentage points [CI, 9 to 35 percentage points]) and white participants (88% vs. 77%; difference, 11 percentage points [CI, 5 to 15 percentage points]). At the end of the trial, fewer intervention than control participants reported having insufficient information about organ donation (34% vs. 44%; difference, −10 percentage points [CI, −16 to −4 percentage points]), wanting to be buried with all of their organs (14% vs. 25%; difference, −11 percentage points [CI, −16 to −6 percentage points]), and having conflicts with organ donation (7% vs. 11%; difference, −4 percentage points [CI, −8 to −2 percentage points]).
Limitation
How the observed increases in consent to donate organs might translate into a greater organ supply in the region is unclear.
Conclusion
Exposure to a brief video addressing concerns that ethnic groups have about organ donation just before obtaining a license, permit, or identification card increased consent to donate organs among white and black participants.
Primary Funding Source
National Institutes of Health and the Robert Wood Johnson Foundation.
More than 100 000 individuals are currently on the active waiting list for organ transplants in the United States, and about 50 000 are added to the list each year. However, fewer than 30 000 transplantations are performed annually (1). As a result, many patients die while waiting for a transplant. The gap between supply and demand is especially striking among ethnic groups, who comprise more than 50% of those on waiting lists but only 30% of donors and 30% of the general population (1, 2). An increase in organ donation would help narrow the gap between supply and demand, and an increase by ethnic groups would be especially helpful because genetic similarities within these groups improve the likelihood of good tissue-type matches between donors and recipients.
Although much attention has been devoted to organ donation, few interventions to increase the number of persons willing to donate organs have been developed and tested. Prior work has identified the concerns of ethnic groups about organ donation, including not having enough information, wanting to be buried with all organs intact, and having personal conflicts about donation (3–7). We developed a brief video to address these concerns and tested its effect on consent for organ donation by whites and ethnic groups at local branches of the Ohio Bureau of Motor Vehicles (BMV). The branches have varying educational materials that they provide about organ donation, and staff discussions of organ donation with patrons also differ; however, most patrons are asked whether they want to be future donors when they apply for a driver’s license (8). We hypothesized that the video intervention would be associated with an increase in the proportion of patrons who consented to organ donation on a newly acquired driver’s license, learner’s permit, or state identification card.
Methods
Study Overview
This was a cluster randomized, controlled trial conducted at the 12 branches of the Ohio BMV located within 25 miles of downtown Cleveland. Recruitment occurred during normal operating hours (Monday through Saturday) from July 2008 until the target sample size was reached in December 2009.
Study coordinators clearly identified as being affiliated with Case Western Reserve University stood outside the entrance of each BMV branch, approached patrons as they entered the facility, described the study, and determined the patron’s willingness and eligibility to participate. English-speaking patrons who planned to obtain a license, permit, or identification card who had not previously consented to organ donation were eligible for inclusion; those who were visiting the BMV for other reasons (for example, vehicle registration) or who did not receive a license, permit, or identification card were not. We obtained consent from a parent or legal guardian of patrons younger than 18 years. Participants were given $10 at the end of the study to thank them for their participation. The institutional review board of MetroHealth Medical Center, Cleveland, Ohio, approved this study.
Randomization
All 12 BMV branches agreed to participate. We visited each branch in alphabetical order by city, alternating between locations close to (<10 miles) and far from (>10 miles) the study office to minimize fatigue and maximize the safety of the research staff who drove to each site. We visited each branch over 2 consecutive days during the week (Monday and Tuesday, or Wednesday and Thurs-day) or on Saturday mornings; Fridays were reserved for missed visits. This schedule was followed until the target sample size was obtained. With the exception of Saturday, each day of visitation was divided into 2 half-day blocks of 4 hours (4 blocks for a 2-day visitation at each site). Half-day blocks on Saturdays were distributed over 4 consecutive weeks to minimize the possibility that study activities performed with intervention participants might affect control participants. We used a random-number table to assign the first half-day block at each BMV branch to view the video (intervention) or undergo usual BMV license procedures (control). The group assignment for the afternoon of the first day of visitation was then the opposite of the morning assignment, and the group assignments for each half-day block of the second day were the opposite of those on the first day. This ensured that all 4 blocks at each study site would have 2 control half-days and 2 intervention half-days. The randomization schedule was concealed by using sealed envelopes. On the morning of the first day that a new site was to be visited, research assistants would open the envelope and learn how the 4 ensuing half-days at each site would be spent. To prevent an imbalance in enrollment of patrons by site, a maximum of 7 participants per research assistant could be enrolled per half-day.
Intervention Group
The intervention was a 5-minute video that participants watched using an iPod classic or iPod touch (Apple, Cupertino, California) with noise-cancelling headphones. The professionally produced video addressed 6 concerns that have been expressed in previous research about organ donation: desire not to think about death and subsequent disfigurement, concern that potential donors may not receive adequate medical care if found to be carrying a donor card, distrust of the medical establishment, belief that religion may not support donation, desire to be buried with organs intact, and lack of knowledge about the need for organs (3–7). The video depicted a discussion among an ethnically diverse group of 20 persons of various ages with various relationships to organ donation and transplantation, including organ donors and recipients, family members of organ donors and recipients, and family members of those who died while waiting for organ transplants. Both living and deceased organ donation were discussed. After viewing the video, participants entered the BMV branch to obtain their license, permit, or identification card. After exiting the BMV, participants were interviewed by the study coordinator and were asked to show their new license, permit, or identification card, on which their donor status was printed. The participants were then given written information on organ donation provided by Life-banc (the organ procurement organization for northeastern Ohio) and the Cleveland branch of the Minority Organ Tissue Transplant Education Program.
Control Group
After consenting to participate, control group participants obtained their license, permit, or identification card in the usual manner. Similar to the intervention group, control participants were interviewed by a study coordinator and were asked to show their license, permit, or iden-tification card after exiting the BMV. After the interview and collection of study data, participants were given written information on organ donation provided by Lifebanc and the Cleveland branch of the Minority Organ Tissue Transplant Education Program. This ensured that all study participants received factual information about organ donation.
Interview Content
We asked intervention and control participants questions about their age, sex, race/ethnicity, religiosity, self-reported health status, and knowledge of organ donation and transplantation. We used instruments developed spe-cifically for this study to measure religiosity and self-reported health status. On the basis of responses to 12 factual statements used by our group and others in previous work (3, 7, 9), we assessed knowledge of donation and transplantation in 6 distinct areas: ethnic composition of the waiting list and disparities in waiting times, the process of organ allocation, fairness and equity of the organ allocation system, funding of organ donation and transplant operations, success of and quality of life after transplantation, and living donation (score range, 0 to 12 [based on “true” or “false” responses to each question]). We also asked about their agreement with the 6 commonly cited barriers to organ donation addressed in the video, whether they had donated blood in the past year, whether they were willing to become living kidney donors, and whether BMV staff asked them if they wanted to become organ donors. We recorded any passive mention of adverse effects of the study by participants and asked all intervention participants if they had viewed and heard the video intervention in its entirety. Finally, we asked all participants to show their newly obtained license, permit, or identification card so that we could verify whether they consented to organ donation.
Blinding
Because study coordinators carried out the intervention, it was not possible for them to be blinded to group assignment. However, the intervention occurred outside of each BMV branch, so it was unlikely that BMV staff would learn the group assignment of study participants or alter their behaviors if they did.
Outcomes
The primary outcome of the trial was organ donor designation on a license, permit, or identification card. Secondary outcomes were willingness to be a living kidney donor for a family member in need and the 6 commonly stated concerns about donation.
Statistical Analysis
On the basis of prior work (3, 8, 10), we anticipated that as many as 50% of the control participants would consent to donation. Based on our experience, expertise, and available resources, we sought to detect an absolute difference in organ donation consent of 12% between groups. Detection of an effect size of 12% with a 2-tailed α level of 0.05 and 80% power required a total of 535 participants. The sample size was increased by an inflation factor of 1.52 to account for possible clustering of outcomes (intraclass cluster coefficient, 0.01) within BMV branches and an additional 10% for possible dropouts, leading to a final total sample size of 895 participants.
Analyses were conducted according to original random assignment regardless of protocol adherence. Study participants were the unit of analysis. We used a generalized estimating equations approach with identity link to estimate the risk difference (intervention minus control, unadjusted for covariates) for each binary outcome. We computed a 95% CI for each outcome, allowing for a nonzero within-site correlation and based on a robust estimate of the SE. We used a generalized estimating equations approach with logit link for a binary outcome to assess the effect of the video intervention on the log odds of signing a donor card, adjusting for race (white vs. other), sex, age, religiosity, and knowledge score. We allowed for possible clustering within BMV branches in the SE estimation by using an exchangeable working correlation structure. We also investigated possible clustering within time but did not find evidence that this was present. We report nominal P values without adjustment for multiple testing; we interpreted each result separately and used actual Likert scale responses in tests of significance. We repeated the analyses within prespecified race/ethnicity subgroups (white, black, Hispanic, or other) and performed formal testing for interactions by using a race by intervention group interaction term. We present nominal (unadjusted) P values for our exploratory subgroup analysis and analysis of secondary outcomes.
Our analysis of the primary outcome excluded 50 participants who withdrew from the trial or declined to show their card. Among the remaining trial population (n = 952), data were missing only for the religiosity variable (n = 11), which we handled by using a multiple imputation procedure. Specifically, we estimated the missing values on the basis of the other model covariates and the outcome by using predicted mean matching. This approach uses randomly drawn observed values from individuals whose predicted values are similar to those of the individual with the missing data. We obtained 10 complete data sets by using this imputation. We analyzed each data set by using a generalized estimating equation and combined the results by using the Rubin formula (11). We also tested for an intervention effect by using the Rubin approach to account for within-imputation and between-imputation variation (12).
Our analysis of the secondary outcome of willingness to donate a kidney excluded 35 participants who withdrew from the trial but included 15 who declined to show their card. Among the remaining trial population (n = 967), data were missing only for the religiosity variable (n = 12), which we handled by using the same multiple imputation procedure.
For the 50 participants (17 in the intervention group and 33 in the control group) who withdrew from the trial or declined to show their license, we imputed data for their regression model covariates on the basis of study group and study site. We then performed a “worst-case” sensitivity analysis assuming all 33 persons in the control group signed donor cards and all 17 in the intervention group did not sign donor cards.
Analyses were performed by using Stata, release 9.2 (StataCorp, College Station, Texas) and SAS, version 9.2 (SAS Institute, Cary, North Carolina).
Role of the Funding Source
This trial was funded by the National Institute on Minority Health and Health Disparities and the National Center for Research Resources of the National Institutes of Health and the Robert Wood Johnson Foundation. The funders had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Results
Participant Characteristics
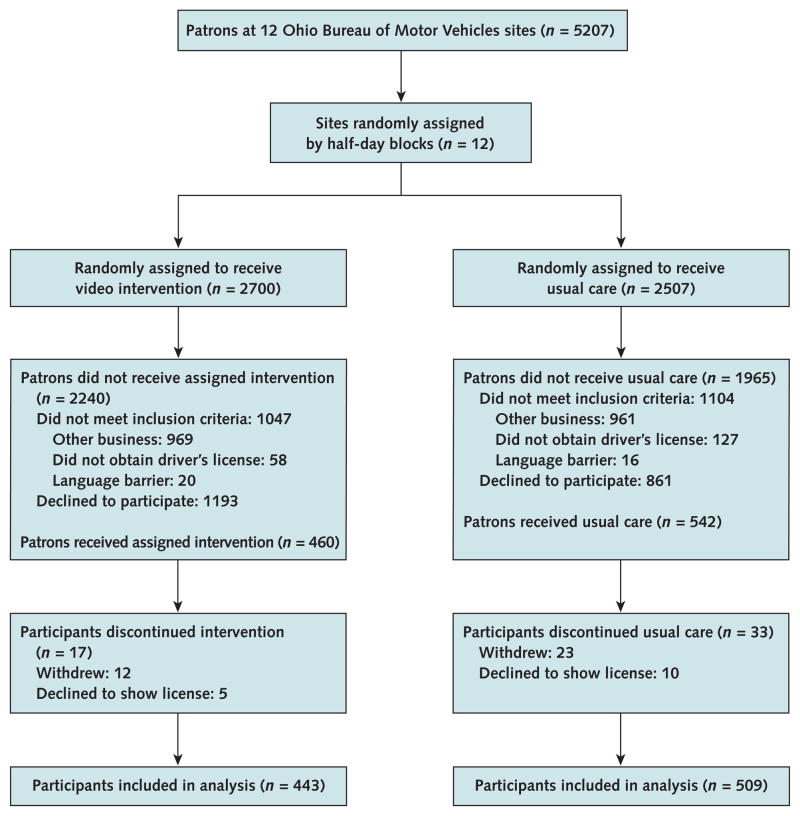
Of 5207 BMV patrons, 2151 did not meet eligibility criteria (did not visit the branch to obtain a license, were unable to obtain a license, or did not speak English) and 2054 declined to participate (44% in the intervention group and 34% in the control group). Of the remaining sample of 1002 participants, 35 withdrew from the study before completing the interview and 15 did not allow the study coordinator to examine their driver’s license, leaving 952 in the analysis (443 in the intervention group and 509 in the control group) (Figure). The median number of participants at each site was 80 (interquartile range, 49 to 99) (Appendix Tables 1 to 12, available at www.annals.org).
Figure 1.
Figure Study flow diagram.
All intervention participants reported viewing the video in its entirety. Intervention and control participants had similar baseline characteristics (Table 1). The most common license type was a first-time driver’s license. About one sixth of participants in each group stated that they had donated blood within the past year. Virtually all participants (91%) were asked about organ donation by BMV staff; in informal conversation during the exit interview, many of the remaining 9% expressed concern that they had not been asked. Participant characteristics were similar across sites except for sex and license type (Appendix Tables 1 to 12).
Table 1.
Participant Characteristics at Baseline
| Characteristic | Intervention Group (n = 443) | Control Group (n = 509) |
|---|---|---|
| Mean age (SD), y | 24 (10) | 25 (12) |
|
| ||
| Male, n (%) | 212 (48) | 236 (46) |
| Race/ethnicity, n (%) | ||
|
| ||
| Non-Hispanic white | 306 (69) | 362 (71) |
|
| ||
| Non-Hispanic black | 87 (20) | 95 (19) |
|
| ||
| Hispanic | 16 (3) | 12 (2) |
|
| ||
| Other | 34 (8) | 40 (8) |
|
| ||
| Mean influence of religion in participants’ lives (SD)* | 6.1 (3.0) | 6.0 (3.0) |
|
| ||
| License type, n (%) | ||
|
| ||
| First-time license | 146 (33) | 165 (32) |
|
| ||
| Learner’s permit | 144 (32) | 148 (29) |
|
| ||
| License renewal | 118 (27) | 147 (29) |
|
| ||
| Other | 35 (8) | 49 (10) |
|
| ||
| Mean self-reported health status (SD)† | 87 (13) | 88 (12) |
|
| ||
| Donated blood within past year, n (%) | 74 (17) | 83 (16) |
|
| ||
| Mean knowledge score (SD)‡ | 5.5 (2.3) | 5.3 (2.3) |
|
| ||
| Asked to donate organs by BMV staff, n (%) | 405 (91) | 464 (91) |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence. Data were missing for 11 participants.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Measured on a scale of 0 to 12 in which 0 indicates low knowledge of donation and transplantation and 12 indicates high knowledge.
Consent for Organ Donation
Intervention participants were more likely than control participants to consent to organ donation (84% vs. 72%; unadjusted absolute difference, 12 percentage points [95% CI, 6 to 17 percentage points]; adjusted odds ratio [OR], 2.05 [CI, 1.49 to 2.81]; interclass correlation coef-ficient [ICC] <0.006) (Table 2). A worst-case sensitivity analysis, which assumed that the 17 excluded intervention participants did not consent and the 33 excluded control participants did consent, yielded similar results (adjusted OR, 1.48 [CI, 1.08 to 2.01]). The intervention effect was evident among black participants (76% vs. 54%; unadjusted absolute difference, 22 percentage points [CI, 9 to 35 percentage points]) and white participants (unadjusted absolute difference, 11 percentage points [CI, 5 to 15 percentage points]) but not among Hispanic participants, who comprised only 5% of the trial population. A formal test of interaction across racial groups was not significant (P = 0.11). Similarly high percentages of intervention and control participants indicated their willingness to make a living kidney donation to a loved one (96% vs. 97%; unadjusted absolute difference, −1 percentage point [CI, −3 to 0.6 percentage points]; adjusted OR, 0.67 [CI, 0.39 to 1.15]).
Table 2.
Proportion of Participants Who Consented to Donate Organs and Who Were Willing to Make a Living Kidney Donation
| Variable | Intervention Group, n/N (%) | Control Group, n/N (%) | Unadjusted Absolute Risk Estimate (95% CI) | Adjusted Odds Ratio (95% CI)* |
|---|---|---|---|---|
| Consented to organ donation, total | 372/443 (84) | 369/509 (72) | 12 (6 to 17) | 2.05 (1.49 to 2.81) |
| Non-Hispanic white | 268/306 (88) | 280/362 (77) | 11 (5 to 15) | 1.91 (1.39 to 2.62) |
| Non-Hispanic black | 66/87 (76) | 51/95 (54) | 22 (9 to 35) | 2.85 (1.45 to 5.57) |
| Hispanic | 14/16 (87) | 7/12 (58) | 29 (−8 to 65) | 7.25 (0.52 to 100.96) |
| Other | 24/34 (71) | 31/40 (77) | −6 (−17 to 3) | 0.64 (0.37 to 1.11) |
| Willing to donate a kidney while living to a loved one | 429/443 (96) | 491/509 (97) | −1 (−3 to 0.6) | 0.67 (0.39 to 1.15) |
Odds ratios derived from a generalized estimating equation by using logit link for a binary outcome adjusting for race (white vs. other), sex, age, religiosity, and knowledge score. Religiosity data imputed for adjusted odds of signing a donor card (11 participants) and willingness to donate a kidney (12 participants). See text for details.
Donation Perceptions
At the end of the trial, intervention participants were less likely than control participants to report having insufficient information about donation (34% vs. 44%; adjusted OR, 0.67 [CI, 0.52 to 0.86]; ICC, −0.002), wanting to be buried with all of their organs (14% vs. 25%; adjusted OR, 0.46 [CI, 0.34 to 0.63]; ICC, −0.005), and having conflicts with organ donation (7% vs. 11%; adjusted OR, 0.53 [CI, 0.37 to 0.78]; ICC, −0.002) (Table 3). No difference was noted between intervention and control participants in reporting trust that organs would be allocated fairly (91% vs. 89%; adjusted OR, 1.16 [CI, 0.83 to 1.62]; ICC, −0.002), and concern that carrying a donor card would lead to insufficient medical care (17% vs. 20%; adjusted OR, 0.83 [CI, 0.61 to 1.12]; ICC, 0.003).
Table 3.
Barriers to Organ Donation Cited Among Participants
| Barrier | Intervention Group, n/N (%) | Control Group, n/N (%) | Unadjusted Absolute Risk Estimate (95% CI) | Adjusted Odds Ratio (95% CI)* |
|---|---|---|---|---|
| Insufficient information regarding donation | 152/448 (34) | 228/523 (44) | −10 (−16 to −4) | 0.67 (0.52 to 0.86) |
| Lack of trust that organs will be distributed fairly | 409/450 (91) | 467/524 (89) | 2 (−1 to 5) | 1.16 (0.83 to 1.62) |
| Desire to be buried or cremated with all organs | 61/449 (14) | 128/519 (25) | −11 (−16 to −6) | 0.46 (0.34 to 0.63) |
| Personal conflict with or moral objection to organ donation | 30/449 (7) | 60/524 (11) | −4 (−8 to −2) | 0.53 (0.37 to 0.78) |
| Concern that carrying a donor card will lead to insufficient care | 75/448 (17) | 104/509 (20) | −3 (−8 to 1) | 0.83 (0.61 to 1.12) |
Odds ratios derived from a generalized estimating equation by using logit link for a binary outcome adjusting for race (white vs. other), sex, age, religiosity, and knowledge score. See text for details. Includes participants who answered ≥1 question before withdrawing from the study.
Adverse Effects
There were no reported adverse effects from the video intervention.
Discussion
In this cluster randomized trial, we found that a brief video addressing the concerns of ethnic groups about organ donation increased consent to donate organs among white and black participants as measured by donor status on driver’s licenses, learner’s permits, or state identification cards. The video intervention also resulted in favorable changes in perceptions of donation.
We searched PubMed for the terms organ donation and intervention to identify trials published between 1982 and 2011 that evaluated interventions to increase organ donation. We identified 8 such efforts that either showed no effect or were limited by nonrandomized designs or a lack of validation of self-reported willingness to donate by examining driver’s licenses (13–21). For example, a randomized, controlled trial involving 9 churches found that educational materials tailored toward black adults did not differ from standard educational materials in increasing consent for donation on licenses or separate donor cards (13). However, 1 study that used a pre–post design found increases in willingness to donate and willingness to join a donor registry among visitors to a Web site designed to educate visitors on organ donation (14). Using a similar method and intervention, another study randomly assigned 490 high school students from 81 schools in Michigan to view either a Web site on organ donation education or one designed to educate viewers on avoiding the common cold (15). Twenty-two percent of those in the intervention group contacted the Michigan donor registry compared with 16% in the control group (P < 0.07). A multifaceted print and video intervention among American Indians resulted in a 20% increase in consent for donation in a pre–post design (16, 17). In addition, a workplace intervention involving employees at 21 corporations resulted in a 14% increase in self-reported willingness to donate (18). In a different pre–post design study, a 14% increase in rates of organ donor registration was also found in counties with motor vehicle bureau staff who attended a 1-hour training program on organ donation compared with counties that used untrained staff (19). Among town hall meetings in which participants were exposed to a 1-hour lecture on organ donation and offered monetary or raffled prize incentives, persons who were randomly assigned to have organ donor registration forms collected at the end of the meeting had a greater registration rate than those who were given the option to mail their forms (21). Finally, a randomized, controlled trial conducted in an intensive care unit found that using collaborative requesting with an organ procurement officer and physician was not superior to requests from a physician alone in increasing organ donation rates (20).
Our video intervention targeted several barriers to donation that we and others have identified. First, people are generally reluctant to consider their own mortality (22, 23). Second, many individuals are concerned that they may receive substandard care or prematurely be declared dead if they carry a donor card (24). Third, distrust of the medical establishment, religious concerns, and a desire for body integrity for burial may be impediments to organ donation (4, 24). Fourth, many persons are simply not exposed to the topic of donation (25). Our video specifically addressed these barriers while also emphasizing the positive effects of donation. This combination has been suggested as a promising approach to increasing donation rates (25, 26).
Advantages of our video intervention include low cost, brevity, and ease of implementation. The potency of the intervention may have been enhanced by provision of relevant, targeted information just before individuals were required to declare their organ donation status. The use of iPods with noise-cancelling headphones allowed the video to be privately viewed without distractions.
In this study, 9% of participants were not asked about their willingness to donate by BMV staff. During interviews with patrons after they obtained their licenses, many were disconcerted that they had not been asked. This omission reflects a potential missed opportunity to increase organ donation consent. Organ procurement organizations in Ohio and the Minority Organ Tissue Transplant Education Program have been working on addressing this issue (Bowen G, Robinson M. Personal communication.), and this should be an area of focus in subsequent donation interventions at the BMV.
Several limitations must be considered in interpreting our results. Because we compared the video intervention with no intervention, we cannot determine which component of the intervention (the video, the iPod, or both) was responsible for the increased consent for donation. Members of the study staff were not blinded to study group and may have interacted with members of each group differently. The study results may not be generalizable beyond northeastern Ohio. The proportion of control participants who consented to organ donation (71%) was higher than that reported in the general population (about 50%) (10), suggesting that individuals who were more interested in organ donation may have been more likely to participate in the study. Despite this possibility, a higher proportion of intervention participants consented to organ donation than control participants. In the intervention group, 34% of participants reported still lacking sufficient information about organ donation. This suggests areas of further intervention to increase donation. Similarly, the intervention did not seem to affect participant trust that organs would be distributed fairly. This may represent a ceiling effect (because both groups reported <12% distrust) or an area that was not sufficiently addressed by the video. The video did not seem to increase distrust because there was no difference in distrust between the 2 groups. On average, participants were younger than the general population and thus the intervention may not be generalizable to older groups. We could not determine why 50 participants withdrew or declined to show their licenses. Although we spec-ified racial subgroups in advance, we considered the analyses of racial subgroup and of secondary outcomes exploratory and hypothesis-generating rather than confir-matory. Finally, and perhaps most important, no evidence exists on how or whether the increase in organ donation consent seen in this trial might translate into a greater future supply of organs in the region.
In summary, we found that a brief video intervention delivered on an iPod at the point where BMV patrons were asked to decide organ donor status increased consent for donation. Because tens of millions of Americans obtain driver’s licenses annually, this approach has the potential to substantially increase the number of potential organ donors (27). Future research should explore the effects of video interventions to increase organ donation in other settings and by using other forms of delivery.
Context
The gap between the supply of organs available for transplantation and demand is growing.
Contribution
In this cluster randomized trial, patrons of the Ohio Bureau of Motor Vehicles who viewed a short video about concerns people have about organ donation were more likely to identify themselves as organ donors on their driver’s licenses, learner’s permits, or state identification cards than patrons who did not view the video.
Caution
How the observed increases in consent to donate organs might translate into a greater organ supply in the region and beyond is unclear.
Implication
Exposure to a brief video addressing concerns about organ donation can increase consent to donate organs.
—The Editors
Acknowledgments
Grant Support: By the National Institute on Minority Health and Health Disparities (grant 1-P60MD002265-01), National Center for Research Resources (grant UL1RR024989), and Robert Wood Johnson Harold Amos Medical Faculty Development Program.
Appendix Table 1.
Participant Characteristics at Baseline at Ohio BMV Site 1
| Characteristic | Intervention Group (n = 37) | Control Group (n = 33) | P Value |
|---|---|---|---|
| Mean age (SD), y | 25 (11) | 25 (12) | 0.92 |
| Male, n (%) | 21 (57) | 16 (48) | 0.49 |
| Race/ethnicity, n (%) | — | — | 0.167 |
| Non-Hispanic white | 27 (73) | 25 (76) | — |
| Non-Hispanic black | 9 (24) | 4 (12) | — |
| Hispanic | 0 | 0 | — |
| Other | 1 (3) | 4 (12) | — |
| Mean influence of religion in participants’ lives (SD)* | 6.6 (2.8) | 6.9 (2.7) | 0.60 |
| License type, n (%) | — | — | 0.83 |
| First-time license | 10 (27) | 9 (27) | — |
| Learner’s permit | 11 (30) | 8 (24) | — |
| License renewal | 12 (32) | 10 (30) | — |
| Other | 4 (11) | 6 (18) | — |
| Mean self-reported health status (SD)† | 84 (11) | 88 (10) | 0.164 |
| Donated blood within past year, n (%) | 7 (19) | 8 (24) | 0.59 |
| Asked to donate organs by BMV staff, n (%) | 35 (95) | 31 (94) | 0.91 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 2.
Participant Characteristics at Baseline at Ohio BMV Site 2
| Characteristic | Intervention Group (n = 20) | Control Group (n = 25) | P Value |
|---|---|---|---|
| Mean age (SD), y | 18 (2.8) | 25 (15) | 0.06 |
| Male, n (%) | 8 (38) | 11 (46) | 0.6 |
| Race/ethnicity, n (%) | — | — | 0.23 |
| Non-Hispanic white | 20 (95) | 22 (92) | — |
| Non-Hispanic black | 0 | 2 (8) | — |
| Hispanic | 1 (5) | 0 | — |
| Other | 0 | 0 | — |
| Mean influence of religion in participants’ lives (SD)* | 5.2 (2.9) | 5.7 (3.4) | 0.63 |
| License type, n (%) | — | — | 0.26 |
| First-time license | 11 (52) | 8 (33) | — |
| Learner’s permit | 5 (24) | 8 (33) | — |
| License renewal | 5 (24) | 5 (21) | — |
| Other | 0 | 3 (13) | — |
| Mean self-reported health status (SD)† | 88 (12) | 88 (10) | 0.83 |
| Donated blood within past year, n (%) | 5 (24) | 1 (4) | 0.05 |
| Asked to donate organs by BMV staff, n (%) | 20 (95) | 24 (100) |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 3.
Participant Characteristics at Baseline at Ohio BMV Site 3
| Characteristic | Intervention Group (n = 43) | Control Group (n = 48) | P Value |
|---|---|---|---|
| Mean age (SD), y | 25 (10) | 26 (14) | 0.77 |
| Male, n (%) | 24 (56) | 22 (46) | 0.85 |
| Race/ethnicity, n (%) | — | — | 0.61 |
| Non-Hispanic white | 30 (70) | 35 (73) | — |
| Non-Hispanic black | 8 (19) | 6 (12) | — |
| Hispanic | 1 (2) | 1 (2) | — |
| Other | 4 (9) | 5 (12) | — |
| Mean influence of religion in participants’ lives (SD)* | 6.1 (3.2) | 6.1 (3.1) | 0.94 |
| License type, n (%) | — | — | 0.40 |
| First-time license | 10 (23) | 18 (38) | — |
| Learner’s permit | 10 (23) | 12 (25) | — |
| License renewal | 20 (47) | 15 (31) | — |
| Other | 3 (7) | 3 (6) | — |
| Mean self-reported health status (SD)† | 90 (8) | 89 (9) | 0.66 |
| Donated blood within past year, n (%) | 9 (21) | 8 (17) | 0.81 |
| Asked to donate organs by BMV staff, n (%) | 40 (93) | 44 (92) | 0.34 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 4.
Participant Characteristics at Baseline at Ohio BMV Site 4
| Characteristic | Intervention Group (n = 10) | Control Group (n = 11) | P Value |
|---|---|---|---|
| Mean age (SD), y | 34 (11) | 30 (11) | 0.45 |
| Male, n (%) | 2 (20) | 1 (9) | 0.47 |
| Race/ethnicity, n (%) | — | — | 0.4 |
| Non-Hispanic white | 0 | 2 (18) | — |
| Non-Hispanic black | 8 (80) | 8 (73) | — |
| Hispanic | 1 (10) | 1 (9) | — |
| Other | 1 (10) | 0 | — |
| Mean influence of religion in participants’ lives (SD)* | 7.1 (3.4) | 7 (2.7) | 0.94 |
| License type, n (%) | — | — | 0.43 |
| First-time license | 4 (40) | 2 (18) | — |
| Learner’s permit | 0 | 2 (18) | — |
| License renewal | 3 (30) | 3 (27) | — |
| Other | 3 (30) | 4 (37) | — |
| Mean self-reported health status (SD)† | 79 (28) | 83 (20) | 0.69 |
| Donated blood within past year, n (%) | 2 (20) | 0 | 0.12 |
| Asked to donate organs by BMV staff, n (%) | 10 (100) | 11 (100) | — |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 5.
Participant Characteristics at Baseline at Ohio BMV Site 5
| Characteristic | Intervention Group (n = 58) | Control Group (n = 70) | P Value |
|---|---|---|---|
| Mean age (SD), y | 23 (10) | 23 (11) | 0.93 |
| Male, n (%) | 35 (60) | 35 (50) | 0.24 |
| Race/ethnicity, n (%) | — | — | 0.92 |
| Non-Hispanic white | 46 (79) | 58 (83) | — |
| Non-Hispanic black | 8 (14) | 7 (10) | — |
| Hispanic | 1 (2) | 1 (1) | — |
| Other | 3 (5) | 4 (6) | — |
| Mean influence of religion in participants’ lives (SD)* | 6.4 (2.8) | 5.9 (2.9) | 0.4 |
| License type, n (%) | — | — | 0.38 |
| First-time license | 25 (43) | 22 (31) | — |
| Learner’s permit | 22 (38) | 26 (37) | — |
| License renewal | 8 (14) | 16 (23) | — |
| Other | 3 (5) | 6 (9) | — |
| Mean self-reported health status (SD)† | 89 (8) | 86 (14) | 0.16 |
| Donated blood within past year, n (%) | 13 (22) | 11 (16) | 0.35 |
| Asked to donate organs by BMV staff, n (%) | 57 (98) | 69 (99) | 0.89 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 6.
Participant Characteristics at Baseline at Ohio BMV Site 6
| Characteristic | Intervention Group (n = 47) | Control Group (n = 49) | P Value |
|---|---|---|---|
| Mean age (SD), y | 23 (10) | 26 (14) | 0.101 |
| Male, n (%) | 21 (45) | 22 (45) | 0.98 |
| Race/ethnicity, n (%) | — | — | 0.61 |
| Non-Hispanic white | 13 (27) | 16 (34) | — |
| Non-Hispanic black | 28 (60) | 30 (62) | — |
| Hispanic | 1 (2) | 0 | — |
| Other | 5 (11) | 3 (4) | — |
| Mean influence of religion in participants’ lives (SD)* | 6.6 (2.9) | 6.6 (3.2) | 0.95 |
| License type, n (%) | — | — | 0.78 |
| First-time license | 11 (23) | 16 (33) | — |
| Learner’s permit | 16 (34) | 15 (31) | — |
| License renewal | 13 (28) | 11 (22) | — |
| Other | 7 (15) | 7 (14) | — |
| Mean self-reported health status (SD)† | 88 (12) | 88 (15) | 0.89 |
| Donated blood within past year, n (%) | 8 (17) | 9 (19) | 0.83 |
| Asked to donate organs by BMV staff, n (%) | 38 (81) | 32 (65) | 0.09 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 7.
Participant Characteristics at Baseline at Ohio BMV Site 7
| Characteristic | Intervention Group (n = 41) | Control Group (n = 61) | P Value |
|---|---|---|---|
| Mean age (SD), y | 25 (12) | 24 (8) | 0.42 |
| Male, n (%) | 10 (24) | 29 (47) | 0.018 |
| Race/ethnicity, n (%) | — | — | 0.13 |
| Non-Hispanic white | 20 (49) | 36 (59) | — |
| Non-Hispanic black | 17 (41) | 18 (30) | — |
| Hispanic | 2 (5) | 0 | — |
| Other | 2 (5) | 7 (11) | — |
| Mean influence of religion in participants’ lives (SD)* | 5.5 (3.1) | 5.4 (3.3) | 0.95 |
| License type, n (%) | — | — | 0.02 |
| First-time license | 8 (20) | 21 (34) | — |
| Learner’s permit | 17 (41) | 9 (15) | — |
| License renewal | 14 (34) | 27 (44) | — |
| Other | 2 (5) | 4 (7) | — |
| Mean self-reported health status (SD)† | 88 (11) | 89 (9.1) | 0.87 |
| Donated blood within past year, n (%) | 4 (7) | 12 (20) | 0.77 |
| Asked to donate organs by BMV staff, n (%) | 35 (85) | 51 (84) | 0.81 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 8.
Participant Characteristics at Baseline at Ohio BMV Site 8
| Characteristic | Intervention Group (n = 51) | Control Group (n = 49) | P Value |
|---|---|---|---|
| Mean age (SD), y | 24 (12) | 23 (12) | 0.81 |
| Male, n (%) | 28 (55) | 27 (55) | 0.98 |
| Race/ethnicity, n (%) | — | — | 0.58 |
| Non-Hispanic white | 47 (92) | 42 (86) | — |
| Non-Hispanic black | 1 (2) | 2 (4) | — |
| Hispanic | 0 | 0 | — |
| Other | 3 (6) | 5 (10) | — |
| Mean influence of religion in participants’ lives (SD)* | 6.0 (3.2) | 5.8 (3.0) | 0.76 |
| License type, n (%) | — | — | 0.104 |
| First-time license | 23 (45) | 19 (39) | — |
| Learner’s permit | 10 (20) | 13 (26) | — |
| License renewal | 11 (21) | 15 (33) | — |
| Other | 7 (14) | 1 (2) | — |
| Mean self-reported health status (SD)† | 87 (16) | 87 (12) | 0.99 |
| Donated blood within past year, n (%) | 9 (18) | 9 (18) | 0.18 |
| Asked to donate organs by BMV staff, n (%) | 48 (94) | 47 (96) | 0.68 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 9.
Participant Characteristics at Baseline at Ohio BMV Site 9
| Characteristic | Intervention Group (n = 26) | Control Group (n = 36) | P Value |
|---|---|---|---|
| Mean age (SD), y | 24 (12) | 25 (14) | 0.96 |
| Male, n (%) | 15 (58) | 15 (42) | 0.21 |
| Race/ethnicity, n (%) | — | — | 0.5 |
| Non-Hispanic white | 21 (81) | 31 (86) | — |
| Non-Hispanic black | 1 (4) | 2 (6) | — |
| Hispanic | 0 | 1 (3) | — |
| Other | 4 (15) | 2 (6) | — |
| Mean influence of religion in participants’ lives (SD)* | 6 (3) | 5.6 (2.7) | 0.61 |
| License type, n (%) | — | — | 0.74 |
| First-time license | 6 (23) | 13 (36) | — |
| Learner’s permit | 11 (42) | 13 (36) | — |
| License renewal | 7 (27) | 8 (22) | — |
| Other | 2 (8) | 2 (6) | — |
| Mean self-reported health status (SD)† | 84 (20) | 88 (10) | 0.31 |
| Donated blood within past year, n (%) | 6 (23) | 7 (19) | 0.73 |
| Asked to donate organs by BMV staff, n (%) | 25 (96) | 34 (94) | 0.76 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 10.
Participant Characteristics at Baseline at Ohio BMV Site 10
| Characteristic | Intervention Group (n = 84) | Control Group (n = 101) | P Value |
|---|---|---|---|
| Mean age (SD), y | 22 (8) | 24 (11) | 0.103 |
| Male, n (%) | 38 (45) | 53 (53) | 0.33 |
| Race/ethnicity, n (%) | — | — | 0.174 |
| Non-Hispanic white | 62 (71) | 69 (68) | — |
| Non-Hispanic black | 6 (7) | 17 (17) | — |
| Hispanic | 9 (11) | 9 (9) | — |
| Other | 9 (11) | 6 (6) | — |
| Mean influence of religion in participants’ lives (SD)* | 6.1 (3.0) | 6.3 (3.0) | 0.78 |
| License type, n (%) | — | — | 0.053 |
| First-time license | 33 (39) | 31 (31) | — |
| Learner’s permit | 35 (42) | 32 (31) | — |
| License renewal | 11 (13) | 26 (26) | — |
| Other | 5 (6) | 12 (12) | — |
| Mean self-reported health status (SD)† | 87 (12) | 88 (14) | 0.69 |
| Donated blood within past year, n (%) | 9 (11) | 10 (11) | 0.95 |
| Asked to donate organs by BMV staff, n (%) | 74 (88) | 94 (94) | 0.157 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 11.
Participant Characteristics at Baseline at Ohio BMV Site 11
| Characteristic | Intervention Group (n = 24) | Control Group (n = 32) | P Value |
|---|---|---|---|
| Mean age (SD), y | 19 (5) | 26 (17) | 0.063 |
| Male, n (%) | 11 (46) | 12 (37) | 0.53 |
| Race/ethnicity, n (%) | — | — | 0.54 |
| Non-Hispanic white | 21 (88) | 25 (78) | — |
| Non-Hispanic black | 1 (4) | 4 (13) | — |
| Hispanic | 0 | 0 | — |
| Other | 2 (8) | 3 (9) | — |
| Mean influence of religion in participants’ lives (SD)* | 5.4 (3.3) | 6.0 (2.9) | 0.45 |
| License type, n (%) | — | — | 0.99 |
| First-time license | 6 (25) | 8 (25) | — |
| Learner’s permit | 8 (33) | 11 (34) | — |
| License renewal | 9 (38) | 12 (38) | — |
| Other | 1 (4) | 1 (3) | — |
| Mean self-reported health status (SD)† | 89 (11) | 86 (17) | 0.46 |
| Donated blood within past year, n (%) | 2 (8) | 9 (28) | 0.065 |
| Asked to donate organs by BMV staff, n (%) | 23 (96) | 31 (97) | 0.25 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Appendix Table 12.
Participant Characteristics at Baseline at Ohio BMV Site 12
| Characteristic | Intervention Group (n = 10) | Control Group (n = 10) | P Value |
|---|---|---|---|
| Mean age (SD), y | 39 (17) | 50 (18) | 0.21 |
| Male, n (%) | 3 (30) | 4 (40) | 0.64 |
| Race/ethnicity, n (%) | — | — | 0.58 |
| Non-Hispanic white | 5 (50) | 6 (60) | — |
| Non-Hispanic black | 4 (40) | 4 (40) | — |
| Hispanic | 0 | 0 | — |
| Other | 1 (10) | 0 | — |
| Mean influence of religion in participants’ lives (SD)* | 6.8 (3.6) | 7 (2.7) | 0.89 |
| License type, n (%) | — | — | — |
| First-time license | 0 | 0 | — |
| Learner’s permit | 0 | 0 | — |
| License renewal | 10 (100) | 10 (100) | — |
| Other | 0 | 0 | — |
| Mean self-reported health status (SD)† | 86 (14) | 83 (7.4) | 0.63 |
| Donated blood within past year, n (%) | 2 (20) | 0 | 0.136 |
| Asked to donate organs by BMV staff, n (%) | 7 (70) | 9 (90) | 0.26 |
BMV = Bureau of Motor Vehicles.
Measured on a scale of 1 to 10 in which 1 indicates no influence and 10 indicates very strong influence.
Measured on a scale of 0 to 100 in which 0 indicates worst health and 100 indicates best health.
Footnotes
Disclaimer: Drs. Thornton and Albert had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All persons who contributed substantially to this work were included in the author list.
Potential Conflicts of Interest: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum3M11-0571.
Reproducible Research Statement: Statistical code: Available from Dr. Thornton (daryl.thornton@case.edu). Study protocol and data set: Not available.
Current author addresses and author contributions are available at www.annals.org.
Author Contributions: Conception and design: J. Thornton, J. León, J. Albert, J. Martin, M. Allen, A. Sehgal.
Analysis and interpretation of the data: J. Thornton, M. Alejandro-Rodriguez, J. Albert, L. De Jesus, C. Heald, A. Sehgal.
Drafting of the article: J. Thornton.
Critical revision of the article for important intellectual content: J. Thornton, J. Martin, G. Bowen, A. Sehgal.
Final approval of the article: J. Thornton, J. Martin, C. Heald, G. Bo-wen, A. Sehgal.
Provision of study materials or patients: J. Thornton, M. Alejandro-Rodriguez, J. Martin, K. Wong, M. Allen.
Statistical expertise: J. Thornton, J. Albert, C. Heald, A. Sehgal.
Obtaining of funding: J. Thornton, J. León, M. Allen, A. Sehgal.
Administrative, technical, or logistic support: J. Thornton, M. Alejandro-Rodriguez, J. León, L. De Jesus, S. Hossain, J. Martin, M. Robinson, G. Bowen, A. Sehgal.
Collection and assembly of data: J. Thornton, M. Alejandro-Rodriguez, E. Baldeon, L. De Jesus, A. Gallardo, S. Hossain, E. Perz, J. Martin, S. Lasalvia.
References
- 1.Health Resources and Services Administration. Organ Procurement and Transplantation Network. Washington, DC: U.S. Department of Health & Human Services; 2011. [14 February 2012]. Accessed at http://optn.transplant.hrsa.gov/latestData/step2.asp? on. [Google Scholar]
- 2.U.S. Census Bureau. American FactFinder. Washington, DC: U.S. Census Bureau; 2011. [24 December 2011]. Accessed at http://factfinder.census.gov on. [Google Scholar]
- 3.Thornton JD, Wong KA, Cardenas V, Curtis JR, Spigner C, Allen MD. Ethnic and gender differences in willingness among high school students to donate organs. J Adolesc Health. 2006;39:266–74. doi: 10.1016/j.jadohealth.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 4.Callender CO, Bayton JA, Yeager C, Clark JE. Attitudes among blacks toward donating kidneys for transplantation: a pilot project. J Natl Med Assoc. 1982;74:807–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Horton RL, Horton PJ. Knowledge regarding organ donation: identifying and overcoming barriers to organ donation. Soc Sci Med. 1990;31:791–800. doi: 10.1016/0277-9536(90)90174-q. [DOI] [PubMed] [Google Scholar]
- 6.Morgan SE, Harrison TR, Afifi WA, Long SD, Stephenson MT. In their own words: the reasons why people will (not) sign an organ donor card. Health Commun. 2008;23:23–33. doi: 10.1080/10410230701805158. [DOI] [PubMed] [Google Scholar]
- 7.Siminoff LA, Burant C, Youngner SJ. Death and organ procurement: public beliefs and attitudes. Soc Sci Med. 2004;59:2325–34. doi: 10.1016/j.socscimed.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Wagstaff DA, Korda H, McCleary KJ. African Americans’ organ donor intentions: who has used which registration mode to express her or his intentions? J Public Health Manag Pract. 2008;14:E7–E13. doi: 10.1097/01.PHH.0000303420.83518.65. [DOI] [PubMed] [Google Scholar]
- 9.Gallup. The American public’s attitudes toward organ donation and transplantation. Boston: Gallup; 1992. [Google Scholar]
- 10.Boulware LE, Ratner LE, Sosa JA, Cooper LA, LaVeist TA, Powe NR. Determinants of willingness to donate living related and cadaveric organs: identifying opportunities for intervention. Transplantation. 2002;73:1683–91. doi: 10.1097/00007890-200205270-00029. [DOI] [PubMed] [Google Scholar]
- 11.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: Wiley-Interscience; 2004. [Google Scholar]
- 12.Little RJ, Rubin DB. Statistical Analysis with Missing Data. 2. Hoboken, NJ: Wiley-Interscience; 2002. [Google Scholar]
- 13.Arriola K, Robinson DH, Thompson NJ, Perryman JP. Project ACTS: an intervention to increase organ and tissue donation intentions among African Americans. Health Educ Behav. 2010;37:264–74. doi: 10.1177/1090198109341725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merion RM, Vinokur AD, Couper MP, Jones EG, Dong Y, Wimsatt M, et al. Internet-based intervention to promote organ donor registry participation and family notification. Transplantation. 2003;75:1175–9. doi: 10.1097/01.TP.0000062845.51042.DD. [DOI] [PubMed] [Google Scholar]
- 15.Vinokur AD, Merion RM, Couper MP, Jones EG, Dong Y. Educational web-based intervention for high school students to increase knowledge and promote positive attitudes toward organ donation. Health Educ Behav. 2006;33:773–86. doi: 10.1177/1090198106288596. [DOI] [PubMed] [Google Scholar]
- 16.Fahrenwald NL, Belitz C, Keckler A. Outcome evaluation of ‘sharing the gift of life’: an organ and tissue donation educational program for American Indians. Am J Transplant. 2010;10:1453–9. doi: 10.1111/j.1600-6143.2010.03120.x. [DOI] [PubMed] [Google Scholar]
- 17.Fahrenwald NL, Belitz C, Keckler A, Sharma M. Sharing the gift of life: an intervention to increase organ and tissue donation for American Indians. Prog Transplant. 2007;17:281–7. doi: 10.1177/152692480701700405. [DOI] [PubMed] [Google Scholar]
- 18.Quinn MT, Alexander GC, Hollingsworth D, O’Connor KG, Meltzer D Consortium for the Corporate Contributions for Life. Design and evaluation of a workplace intervention to promote organ donation. Prog Transplant. 2006;16:253–9. doi: 10.1177/152692480601600312. [DOI] [PubMed] [Google Scholar]
- 19.Harrison TR, Morgan SE, Di Corcia MJ. Effects of information, education, and communication training about organ donation for gatekeepers: clerks at the Department of Motor Vehicles and organ donor registries. Prog Transplant. 2008;18:301–9. doi: 10.1177/152692480801800414. [DOI] [PubMed] [Google Scholar]
- 20.ACRE Trial Collaborators. Effect of “collaborative requesting” on consent rate for organ donation: randomised controlled trial (ACRE trial) BMJ. 2009;339:b3911. doi: 10.1136/bmj.b3911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alvaro EM, Siegel JT, Jones SP. Increasing organ donor registration rates by providing an immediate and complete registration opportunity: an experimental assessment of the IIFF model. Psychol Health Med. 2011;16:686–94. doi: 10.1080/13548506.2011.564353. [DOI] [PubMed] [Google Scholar]
- 22.Horton RL. Marketing the concept of becoming a potential organ donor. J Health Care Mark. 1991;11:36–45. [PubMed] [Google Scholar]
- 23.Prottas JM. Encouraging altruism: public attitudes and the marketing of organ donation. Milbank Mem Fund Q Health Soc. 1983;61:278–306. [PubMed] [Google Scholar]
- 24.Siminoff LA, Lawrence RH, Arnold RM. Comparison of black and white families’ experiences and perceptions regarding organ donation requests. Crit Care Med. 2003;31:146–51. doi: 10.1097/00003246-200301000-00023. [DOI] [PubMed] [Google Scholar]
- 25.Skumanich SA, Kintsfather DP. Promoting the organ donor card: a causal model of persuasion effects. Soc Sci Med. 1996;43:401–8. doi: 10.1016/0277-9536(95)00404-1. [DOI] [PubMed] [Google Scholar]
- 26.Winkel FW. Public communication on donorcards: a comparison of persuasive styles. Soc Sci Med. 1984;19:957–63. doi: 10.1016/0277-9536(84)90325-3. [DOI] [PubMed] [Google Scholar]
- 27.Ohio Bureau of Motor Vehicles. 2009 BMV Facts & Figures. Columbus, OH: Ohio Department of Public Safety; 2010. [1 September 2010]. Accessed at http://bmv.ohio.gov/facts_figures09.stm on. [Google Scholar]