Abstract
We investigated whether preoperative perturbation training would help anterior cruciate ligament (ACL) deficient individuals who complain of knee instability (“non-copers”) regain quadriceps strength and walk normally after ACL reconstruction. Nineteen non-copers with acute ACL injury were randomly assigned into a perturbation group (PERT) or a strengthening group (STR). The PERT group received specialized neuromuscular training and progressive quadriceps strength training, whereas the STR group received progressive quadriceps strength training only. We compared quadriceps strength indexes and knee excursions during the mid-stance phase of gait preoperatively to data collected 6 months after ACL reconstruction. Analyses of Variance with repeated measures (time/limb) were conducted to compare quadriceps strength index values over time (time × group) and differences in knee excursions in limbs between groups over time (limb × time × group). If significance was found, post hoc analyses were performed using paired and independent t-tests. Quadriceps strength indexes before intervention (Pert: 87.2%; Str: 75.8%) improved 6 months after ACL reconstruction in both groups (Pert: 97.1%; Str: 94.4%). Non-copers who received perturbation training preoperatively had no differences in knee excursions between their limbs 6 months after ACL reconstruction (p = 0.14), whereas those who received just strength training continued to have smaller knee excursions during the mid-stance phase of gait (p = 0.007). Non-copers strength and knee excursions were more symmetrical 6 months postoperatively in the group that received perturbation training and progressive quadriceps strength training than the group who received strength training alone.
Keywords: anterior cruciate ligament, intervention, quadriceps strength, gait
Internal knee lesions account for 44.8% of athletic injuries, with the anterior cruciate ligament (ACL) being the most prevalent structure treated.1 About 200,000 ACL injuries occur annually in the US.2 Quadriceps strength deficits,3–7 functional decline,8–13 and altered gait patterns6,14,15 are ubiquitous after ACL rupture.16 Only one third of symptomatic ACL-deficient recreational athletes demonstrate the ability to stabilize the knee joint without the ACL.17,18 Nonsurgical interventions have been unsuccessful in restoring stability and strength to patients who complain of knee instability after ACL rupture7; thus athletes are generally counseled that reconstructive surgery is necessary for return to full pre-injury activities.19 Nearly one billion dollars are spent on ACL reconstructions alone,20 yet postoperative quadriceps strength deficits4,5,7 and altered movement patterns21,22 persist, despite restoration of the passive restraint. In fact, in a long-term follow-up study, more knee osteoarthritis (OA) was found after ACL reconstruction compared to those treated conservatively, with similar activity levels in both groups.23
A screening examination and classification system was developed at the University of Delaware. The system can be used early after injury as an effective way to discriminate between those athletes who have good dynamic knee stability and the potential to compensate well after complete ACL rupture (potential copers) from those who have poor dynamic knee stability (non-copers).24,25 Non-copers present with knee instability and truncated involved side knee motion during gait15 to a greater extent when compared to potential copers.6 Non-copers’ quadriceps strength influences the amount of knee flexion used during gait when tested preoperatively.11 Furthermore, there is a significant effect of continued quadriceps weakness on diminished knee angles and knee moments during walking following ACL reconstruction.3
Quadriceps weakness not only contributes to gait and functional decline, but also may be a contributing factor to knee OA.26 ACL rupture is associated with early degenerative changes, which continue after ACL reconstruction.27,28 A myriad of therapeutic interventions have been tested to ascertain the most effective way to treat patients after ACL injury and reconstruction.29–32 The trauma of surgery exacerbates strength and gait abnormalities acutely. A paucity of research exists exploring how best to resolve the strength deficits and gait abnormalities that persist in non-copers despite reconstructive surgery.
A neuromuscular training program, called perturbation training, has improved movement patterns during gait and dynamic knee stabilization in potential copers after training.33 Exposing non-copers, therefore, to perturbations of support surfaces prior to surgery may also be effective for improving gait deviations for this cohort after surgery. Furthermore, progressive quadriceps strength training may be required preoperatively and postoperatively to maximize functional recovery.
Our purpose was to investigate whether preoperative physical therapy that included perturbation training and a progressive quadriceps strengthening program would help non-copers regain more symmetrical quadriceps strength and knee excursions when measured 6 months after ACL reconstruction. We defined quadriceps strength symmetry as a quadriceps index value (involved limb/uninvolved limb) of 90% or greater. All preoperative data were compared to data collected 6 months after surgery. We hypothesized that subjects would demonstrate a difference in preoperative quadriceps strength indexes compared to postoperative values. We also tested whether knee excursions during the mid-stance phase of gait continued to be altered 6 months after ACL reconstruction. We hypothesized that non-copers who received preoperative perturbation training would exhibit symmetrical knee excursions during mid-stance when tested after surgery, whereas the group not receiving preoperative perturbation training would continue to exhibit gait asymmetries.
METHODS
Subjects
Nineteen subjects (13 males, 6 females between the ages of 17 and 50 years old) with complete, acute, isolated ACL rupture were recruited from the University of Delaware Physical Therapy clinic. One surgeon (M.J.A.) referred all subjects and diagnosed all ACL tears via clinical examination and MRI findings. Subjects were regular participants in Level I or II activities (activities involving jumping, cutting, and lateral motion) prior to injury.27 Exclusion criteria were full thickness chondral defects >1 cm, repairable meniscal tears, or concomitant grade III ruptures to other knee ligaments. Our screening examination24 was administered, and only subjects who had been classified as non-copers15 were recruited. Subjects were randomly assigned into a perturbation group (N = 9) or a strengthening group (N = 10). The perturbation group consisted of 6 males and 3 females (28±10.7 years), averaging 9.8±9.5 weeks from the time of injury to the screen. The strength group included 7 males and 3 females (30± 9.4 years) and 12.6±13.1 weeks from the time of injury to the screen. The study was approved by the University’s Institutional Human Subjects Review Board; each subject gave informed consent.
Intervention
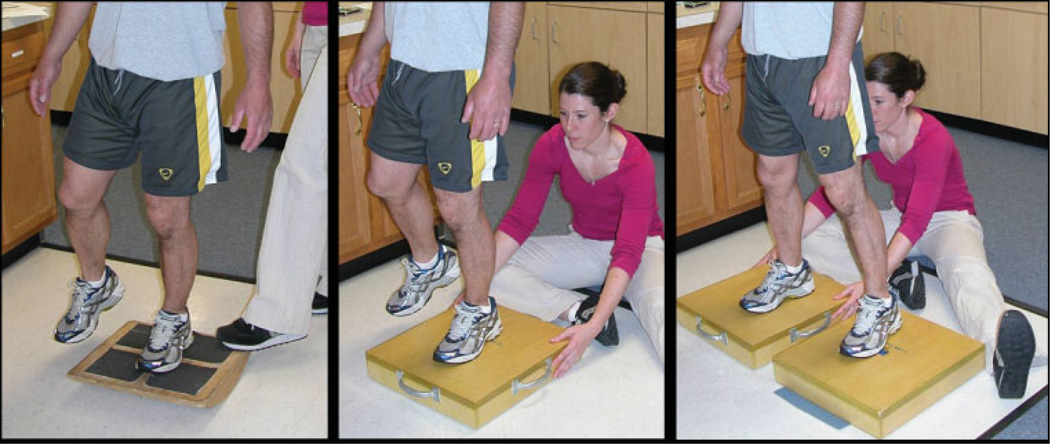
No subjects exercised their lower extremities outside of therapy while participating in the preoperative intervention phase. The strength group received 10 sessions of progressive quadriceps strength training only (average of 3.1 weeks to complete). The perturbation group received 10 sessions of physical therapy including specialized neuromuscular exercises involving systematic translation of support surfaces (Fig. 1) and progressive quadriceps strength training (average of 3.7 weeks to complete). We followed the University of Delaware guidelines for perturbation training,34 the goal being to break up generalized muscle stiffness as subjects were tactilely and verbally cued to elicit selective lower extremity muscle contraction while balancing on a support surface that the physical therapist perturbed.
Figure 1.
Pictures of a subject receiving perturbation training under three conditions (rockerboard, rollerboard, and rollerboard and platform).
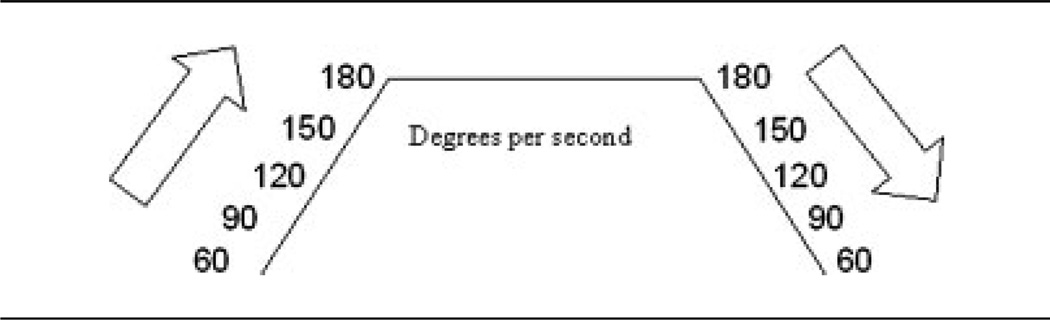
The goal of strength training was to maximize quadriceps force output using high-intensity and low repetitions. Preoperatively, we obtained subjects’ one repetition maximum weight lifted on the injured side while on the leg press and leg extension machines. Subjects then completed three sets of six repetitions at 75% of their one repetition maximum weight. Subjects performed lateral and forward step downs starting at a 4-inch step and progressing in step height when they demonstrated proper technique (knee behind the toes, the mid-line of the patella in alignment with the second toe, the hips level, and touching the heel down softly to the floor). Lastly, subjects completed an isokinetic spectrum routine on a dynamometer (KIN-COM; Chattanooga Corp., Chattanooga, TN). Subjects were encouraged to exert full effort implementing both verbal and visual feedback as motivation (Table 1).
Table 1.
Subjects Completed 10 Repetitions at the Speeds Shown while Performing Both Eccentric and Concentric Quadriceps Muscle Contractions through 10 to 100° of Knee Flexion
 |
After the 10 preoperative sessions were completed, the surgeon (M.J.A.) performed ACL reconstruction using either semitendonosis-gracilis autograft or soft tissue allograft. Graft placement and fixation were similar for all subjects. After surgery, the University of Delaware postoperative ACL protocol was followed by all subjects regardless of group.35 Quadriceps strength percentage, knee effusion grades, and soreness were used as guidelines to progress the subject through the clinical milestones.
Quadriceps Maximum Volitional Isometric Contraction (MVIC) Testing
Injured and uninjured limb quadriceps forces were assessed with MVIC testing using the burst superimposition technique to assure maximal muscle activation.36 Subjects were tested on the KIN-COM dynamometer using the University of Delaware testing procedure,37 with practice trials, verbal encouragement, and visual targeting used to facilitate maximal effort. Quadriceps strength testing was performed prior to the intervention and 6 months after ACL reconstruction.
Motion Analysis
Kinematic data were collected with a passive, eight camera 3-D motion analysis system (VICON; Oxford Metrics Ltd., London, UK). Retro-reflective markers were attached over bony prominences to define the hip, knee, and ankle joint centers with tracking shells affixed with cover rolls15 (Fabrifoam Products, Exton, PA). Kinetic data were collected using a six-component force plate (Bertec Corp., Worthington, OH). Kinematic and kinetic data were collected, filtered, and processed as described prevoiusly.15 Motion capture began once speed over a 13-m walkway was consistent and the foot contacted the force plate without targeting or altering the step pattern. Subjects walked with the markers and tracking shells attached until they were familiar with the task and gait speed was recorded. Variation of only 5% was allowed from that speed. There was no difference in inter-subject gait speed between groups. The kinematic variable of interest was knee excursion during the mid-stance phase of gait.
Data Management and Analysis
The quadriceps strength index was calculated using the highest quadriceps MVIC force output from each limb. The quadriceps index is a ratio of the involved side/uninvolved side reported as a percentage for each subject. Knee motion was calculated using rigid body analysis with Euler angles (C-Motion, Inc., Rockville, MD). A customized LabVIEW software program was written to analyze the kinematic data. Five walking trials were averaged for each limb after the data were normalized to 100% of stance. The first minimum value after initial contact in the sagittal plane knee angle curve denoted peak knee flexion, and the maximum value indicated peak knee extension. The knee excursion during mid-stance was obtained by calculating peak knee extension minus peak knee flexion. Group means were calculated for quadriceps index and kinematics data. Mixed ANOVAs with repeated measures (limb × group × time) were conducted using a statistical software package (SPSS, Chicago, IL) to compare differences between groups over time. If significance was found, post hoc analysis was performed using paired and independent t-tests. Significance was set at p < 0.05.
RESULTS
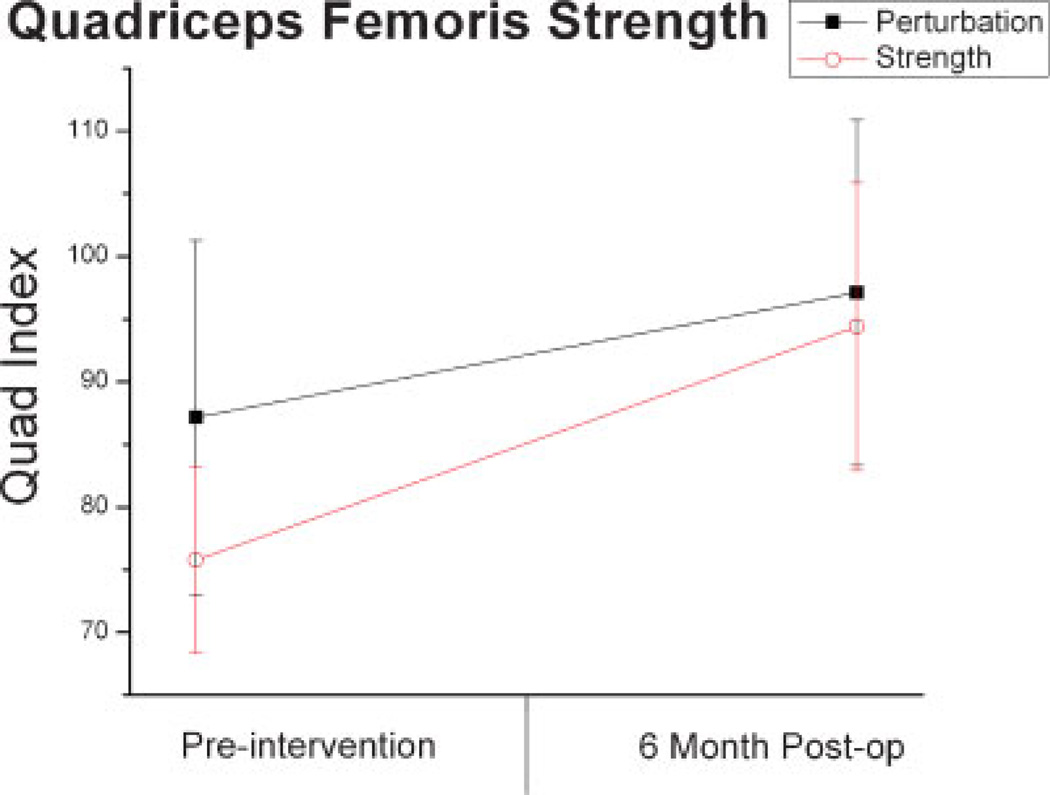
Quadriceps strength indexes improved over time (F = 16.5, observed power = 0.961, p = 0.002). Quadriceps strength indexes before intervention (Pert: 87.2%; Str: 75.8%) improved 6 months after ACL reconstruction in both groups (Pert: 97.1%; Str: 94.4%) (Fig. 2).
Figure 2.
Quadriceps Strength Index (involved force/uninvolved force expressed as a percent) prior to intervention and 6 months after ACL reconstruction for each group. Error bars represent standard deviation.
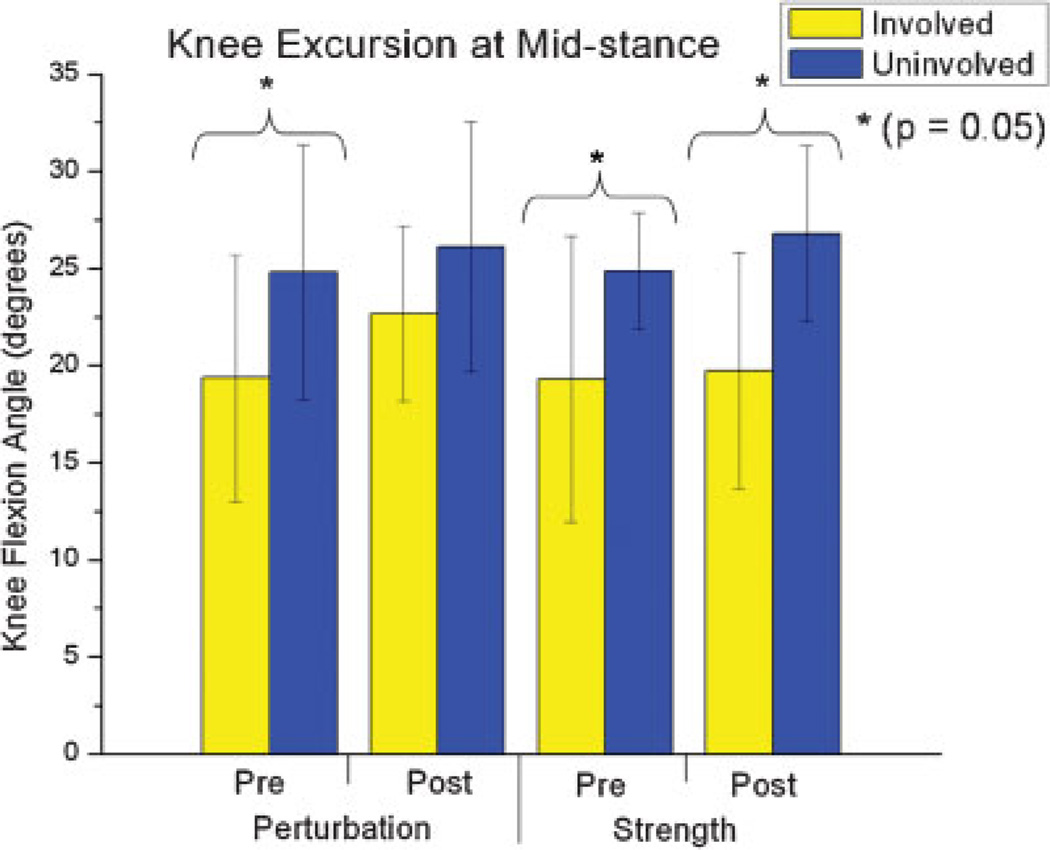
Significant differences were also found in knee excursions between limbs (F = 15.98, observed power = 0.96, p = 0.001) and over time (F = 7.52, observed power = 0.73, p = 0.014). Knee excursions at mid-stance were smaller on the involved side prior to surgery in both groups. The involved limb moved through less flexion in the perturbation groups (Mean: 5.98; 95% CI: 10.2 to 1.5; p = 0.026) and strength (Mean: 5.68; 95% CI: 10.5 to 0.6; p = 0.031) during mid-stance. The perturbation group demonstrated an increase in knee excursion at midstance compared to the uninvolved side, resulting in no significant difference between limbs 6 months after surgery (Mean: 3.58; 95% CI: 8.3 to −1.4; p = 0.14). The mid-stance knee excursions continued to be significantly different between limbs in the strength group 6 months after surgery (Mean 7.08; 95% CI: 11.6 to 2.5; p = 0.007) (Fig. 3).
Figure 3.
Involved knee excursions prior to intervention (Pre) and 6 months after ACL reconstruction (Post) for the involved and uninvolved limb for each group. Error bars represent standard deviation.
DISCUSSION
Quadriceps Strength
As hypothesized, all subjects demonstrated successful quadriceps strength gains 6 months after ACL reconstruction. We operationally defined success as achieving a quadriceps strength index of 90% or greater, a clinically meaningful change achieved by both groups. Our subjects’ successful gains support earlier findings of improved quadriceps strength indexes 6 months after ACL reconstruction,5 though many investigators report deficits 6 months after ACL reconstruction.3–5,7,31
These conflicting results are likely due to discrepancies in quadriceps strength testing and strengthening protocols. Some investigators reported isometric muscle force represented as a quadriceps symmetry index,31,38 while others reported isokinetic strength values of quadriceps symmetry.4,5,7 Our preoperative program focused on intense, progressive quadriceps strengthening on the involved side only with all subjects reporting muscle fatigue after each treatment followed by delayed onset quadriceps soreness. Keays and colleagues7 provided preoperative quadriceps strengthening, though this was predominately home-based and exercise intensity was not specified. Our postoperative protocol35 focused on the importance of early strength gains using neuromuscular electrical stimulation that facilitates quadriceps strength gains more than volitional exercises alone.39,40
Gait Kinematics
As hypothesized, subjects receiving perturbation training demonstrated no difference in knee excursions during mid-stance 6 months after ACL reconstruction. We previously reported preoperative findings of decreased knee excursions in this group of non-copers.15 There were no differences in knee effusion grades during preoperative testing or 6 months following ACL reconstruction between groups, and no subject complained of pain or soreness during gait analysis. Furthermore, all had symmetrical quadriceps strength and knee range of motion without clinically observed antalgic gait patterns, complaints of instability, or episodes of giving way when tested 6-months post-operatively. Yet the strength group continued to display less knee excursion during mid-stance on the involved side.
Interpreting Findings
The quadriceps plays an integral role in concentrically advancing the knee through extension during midstance. The perturbation group demonstrated enhanced ability to use the quadriceps strength gains by moving the involved limb similarly to the uninvolved limb. Perturbation training increases motion and decreases muscle co-contractions in the involved limb during the weight acceptance phase of gait in potential copers after acute ACL rupture.41 Thus, reduction in co-contraction values may be related with our findings of increased motion.
Loss of feedback from mechanoreceptors after ACL rupture and abnormalities in gamma loop information may explain quadriceps weakness.42 Subjects who received perturbation training were trained to focus on the somatosensory input from the weight distribution of the foot contact on the board and the afferent information coming from the lower extremity (joint proprioception and muscle response). The focused awareness of the body in space, along with tactile and verbal feed-forward and feed-back cues during training may have modified gamma loop function. Training may have improved gamma loop feedback and decreased antagonistic muscle activity, enhancing the quadriceps’ ability to stabilize the knee dynamically during gait.
The strength gains demonstrated by both groups may decrease the risk of knee OA. Quadriceps weakness has been shown to be related to the development of knee OA in women.43 However, perturbation training may enhance the sensorimotor characteristics of the muscle more than strengthening alone. Hurley26 inferred that both motor and sensory dysfunction of a muscle are important factors in cartilage degradation. Furthermore, Hurley26 surmised that rehabilitation exercises may reverse sensorimotor dysfunction, thereby delaying or preventing the onset of OA.
The improved inter-limb symmetry displayed during gait by the perturbation group may also have positive implications on joint health. Chaudhari et al.14 surmised that mechanical changes may be the precipitating cause of knee OA as loads shift to areas of cartilage not typically loaded. They documented that cartilage appears to be conditioned to load history and that conditioned cartilage likely has different abilities to respond to loads.14 In vivo studies of non-copers indicate that ACL-deficient limbs shift the contact point between tibia and femur with the tibial point moving more anterior with knee extension.44 Hence, altered knee kinematic changes observed in the sagittal plane may also lead to shift joint load to an infrequently loaded area. Breaking the typical low knee flexion excursion strategy while walking may be advantageous, as joint loads may be distributed over a larger contact area more in line with the conditioned cartilage regions adapted to handle the pre-injury loading pattern.
Despite symmetrical strength achieved by both of our groups, the strength group demonstrated differences in knee excursions between limbs during mid-stance 6 months after ACL reconstruction. This suggests that the neuromuscular system is not controlling the involved limb the same way as the uninvolved limb in both groups. Improved mid-stance excursion in the perturbation group is a promising first indication that neuromuscular training rehabilitation programs can improve movement patterns in the involved limb after ACL reconstruction in non-copers. Investigations that include electromyography are warranted to determine the neuromuscular changes responsible for the perturbation group’s gait adaptations.
ACKNOWLEDGMENTS
This research was supported by the National Institutes of Health (R01AR048212; S10RR022396) and the Foundation of Physical Therapy (PODS I). We acknowledge Sarah Trager for her software programming support, Kyle Fettemore and Greg Seymour for their assistance with data collections and data processing, and the University of Delaware Physical Therapy Clinic for assistance with subject training.
REFERENCES
- 1.Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13:184–188. doi: 10.1016/j.knee.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Miyasaka KC, Daniel DM, Stone ML. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;46:43–48. [Google Scholar]
- 3.Lewek M, Rudolph K, Axe M, et al. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 2002;17:56–63. doi: 10.1016/s0268-0033(01)00097-3. [DOI] [PubMed] [Google Scholar]
- 4.de Jong SN, van Caspel DR, van Haeff MJ, et al. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21–28. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 5.Soon M, Neo CP, Mitra AK, et al. Morbidity following anterior cruciate ligament reconstruction using hamstring autograft. Ann Acad Med Singapore. 2004;33:214–219. [PubMed] [Google Scholar]
- 6.Rudolph KS, Eastlack ME, Axe MJ, et al. 1998 Basmajian Student Award Paper: Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8:349–362. doi: 10.1016/s1050-6411(97)00042-4. [DOI] [PubMed] [Google Scholar]
- 7.Keays SL, Bullock-Saxton J, Keays AC, et al. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8:229–234. doi: 10.1016/s0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 8.Keays SL, Bullock-Saxton J, Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000;373:174–183. doi: 10.1097/00003086-200004000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Keays SL, Bullock-Saxton JE, Newcombe P, et al. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231–237. doi: 10.1016/S0736-0266(02)00160-2. [DOI] [PubMed] [Google Scholar]
- 10.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 11.Rudolph KS, Axe MJ, Buchanan TS, et al. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62–71. doi: 10.1007/s001670000166. [DOI] [PubMed] [Google Scholar]
- 12.Rudolph KS, Axe MJ, Snyder-Mackler L. Dynamic stability after ACL injury: who can hop? Knee Surg Sports Traumatol Arthrosc. 2000;8:262–269. doi: 10.1007/s001670000130. [DOI] [PubMed] [Google Scholar]
- 13.Andriacchi TP, Birac D. Functional testing in the anterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1993;288:40–47. [PubMed] [Google Scholar]
- 14.Chaudhari AM, Briant PL, Bevill SL, et al. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40:215–222. doi: 10.1249/mss.0b013e31815cbb0e. [DOI] [PubMed] [Google Scholar]
- 15.Hurd WJ, Snyder-Mackler L. Knee instability after acute ACL rupture affects movement patterns during the mid-stance phase of gait. J Orthop Res. 2007;25:1369–1377. doi: 10.1002/jor.20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel RR, Hurwitz DE, Bush-Joseph CA, et al. Comparison of clinical and dynamic knee function in patients with anterior cruciate ligament deficiency. Am J Sports Med. 2003;31:68–74. doi: 10.1177/03635465030310012301. [DOI] [PubMed] [Google Scholar]
- 17.Noyes FR, Matthews DS, Mooar PA, et al. The symptomatic anterior cruciate-deficient knee. Part II: the results of rehabilitation, activity modification, and counseling on functional disability. J Bone Joint Surg [Am] 1983;65:163–174. doi: 10.2106/00004623-198365020-00004. [DOI] [PubMed] [Google Scholar]
- 18.Noyes FR, Mooar PA, Matthews DS, et al. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg [Am] 1983;65:154–162. doi: 10.2106/00004623-198365020-00003. [DOI] [PubMed] [Google Scholar]
- 19.Marx RG, Jones EC, Angel M, et al. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 20.Control NCfIPa. CDC injury research agenda. Atlanta, GA: Centers for Disease Control and Prevention; 2002. [Google Scholar]
- 21.Bulgheroni P, Bulgheroni MV, Andrini L, et al. Gait patterns after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1997;5:14–21. doi: 10.1007/s001670050018. [DOI] [PubMed] [Google Scholar]
- 22.Gokeler A, Schmalz T, Knopf E, et al. The relationship between isokinetic quadriceps strength and laxity on gait analysis parameters in anterior cruciate ligament reconstructed knees. Knee Surg Sports Traumatol Arthrosc. 2003;11:372–378. doi: 10.1007/s00167-003-0432-1. [DOI] [PubMed] [Google Scholar]
- 23.Kessler MA, Behrend H, Henz S, et al. Function, osteoarthritis and activity after ACL-rupture: 11 years followup results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16:442–448. doi: 10.1007/s00167-008-0498-x. [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decisionmaking scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8:76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 25.Hurd WJ, Axe MJ, Snyder-Mackler L. A 10-year prospective trial of a patient management algorithm and screening examination for highly active individuals with anterior cruciate ligament injury: part 1, outcomes. Am J Sports Med. 2007;36:40–47. doi: 10.1177/0363546507308190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurley MV. The role of muscle weakness in the pathogenesis of osteoarthritis. Rheum Dis Clin North Am. 1999;25:283–298. doi: 10.1016/s0889-857x(05)70068-5. vi. [DOI] [PubMed] [Google Scholar]
- 27.Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patientAprospective outcome study. Am J Sports Med. 1994;22:632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 28.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39:127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337–342. doi: 10.1007/s001670000143. [DOI] [PubMed] [Google Scholar]
- 30.Morrissey MC, Hudson ZL, Drechsler WI, et al. Effects of open versus closed kinetic chain training on knee laxity in the early period after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2000;8:343–348. doi: 10.1007/s001670000161. [DOI] [PubMed] [Google Scholar]
- 31.Snyder-Mackler L, Delitto A, Bailey SL, et al. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligamentAprospective, randomized clinical trial of electrical stimulation. J Bone Joint Surg [Am] 1995;77:1166–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Gerber JP, Marcus RL, Dibble LE, et al. Safety, feasibility, and efficacy of negative work exercise via eccentric muscle activity following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37:10–18. doi: 10.2519/jospt.2007.2362. [DOI] [PubMed] [Google Scholar]
- 33.Chmielewski TL, Rudolph KS, Snyder-Mackler L. Development of dynamic knee stability after acute ACL injury. J Electromyogr Kinesiol. 2002;12:267–274. doi: 10.1016/s1050-6411(02)00013-5. [DOI] [PubMed] [Google Scholar]
- 34.Fitzgerald GK, Axe MJ, Snyder-Mackler L. Proposed practice guidelines for nonoperative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30:194–203. doi: 10.2519/jospt.2000.30.4.194. [DOI] [PubMed] [Google Scholar]
- 35.Manal T, Snyder-Mackler L. Practice guidelines for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. Oper Tech Orthop. 1996;6:190–196. [Google Scholar]
- 36.Snyder-Mackler L, De Luca PF, Williams PR, et al. Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg [Am] 1994;76:555–560. doi: 10.2106/00004623-199404000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Chmielewski TL, Stackhouse S, Axe MJ, et al. A prospective analysis of incidence and severity of quadriceps inhibition in a consecutive sample of 100 patients with complete acute anterior cruciate ligament rupture. J Orthop Res. 2004;22:925–930. doi: 10.1016/j.orthres.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 38.Lewek MD, Chmielewski TL, Risberg MA, et al. Dynamic knee stability after anterior cruciate ligament rupture. Exerc Sport Sci Rev. 2003;31:195–200. doi: 10.1097/00003677-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Delitto A, Rose SJ, McKowen JM, et al. Electrical stimulation versus voluntary exercise in strengthening thigh musculature after anterior cruciate ligament surgery. Phys Ther. 1988;68:660–663. doi: 10.1093/ptj/68.5.660. [DOI] [PubMed] [Google Scholar]
- 40.Snyder-Mackler L, Ladin Z, Schepsis AA, et al. Electrical stimulation of the thigh muscles after reconstruction of the anterior cruciate ligament. Effects of electrically elicited contraction of the quadriceps femoris and hamstring muscles on gait and on strength of the thigh muscles. J Bone Joint Surg [Am] 1991;73:1025–1036. [PubMed] [Google Scholar]
- 41.Chmielewski TL, Hurd WJ, Rudolph KS, et al. Perturbation training improves knee kinematics and reduces muscle co-contraction after complete unilateral anterior cruciate ligament rupture. Phys Ther. 2005;85:740–754. [PubMed] [Google Scholar]
- 42.Konishi Y, Fukubayashi T, Takeshita D. Possible mechanism of quadriceps femoris weakness in patients with ruptured anterior cruciate ligament. Med Sci Sports Exerc. 2002;34:1414–1418. doi: 10.1097/00005768-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Slemenda C, Heilman DK, Brandt KD, et al. Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998;41:1951–1959. doi: 10.1002/1529-0131(199811)41:11<1951::AID-ART9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 44.Barrance PJ, Williams GN, Snyder-Mackler L, et al. Altered knee kinematics in ACL-deficient non-copers: a comparison using dynamic MRI. J Orthop Res. 2006;24:132–140. doi: 10.1002/jor.20016. [DOI] [PubMed] [Google Scholar]