Abstract
Shift work is associated with a number of negative health outcomes, although it is not known whether it is associated with sick leave. This systematic review therefore aimed to determine whether an association exists between shift work and sick leave. A systematic literature search was conducted in six databases on observational studies. Two reviewers independently selected relevant articles and appraised methodological quality. Data extraction was performed independently by review couples. Articles were categorised according to shift work characteristics and summarised using a levels of evidence synthesis. In total, the search strategy yielded 1207 references, of which 24 studies met the inclusion criteria. Nine studies were appraised as high quality and used in the levels of evidence synthesis. Two high quality longitudinal studies found a positive association between fixed evening shifts and longer sick leave for female healthcare workers. The evidence was assessed as strong. Evidence was inconclusive for rotating shifts, shift work including nights, for fixed night work, and for 8-hour and 12-hour shifts. The association found between evening work and sick leave in female healthcare workers implies that the association between shift work and sick leave might be schedule and population specific. To study the association further, more high quality studies are necessary that assess and adjust for detailed shift work exposure.
Keywords: Work schedule tolerance, shift work, sick leave, systematic review, epidemiology, materials, exposures and occupational groups, fatigue, methodology, speciality, sickness absence, ergonomics, health promotion, musculoskeletal, exposure assessment
What this paper adds.
Strong evidence was found for a positive association between fixed evening work and sick leave in female healthcare workers.
The findings imply that the association between shift work and sick leave is schedule specific.
The findings call for research where schedule characteristics are assessed and used in the analyses.
Introduction
Within various industries and business sectors, continuous production processes and services are needed to facilitate the demands of a 24-h economy and increased globalisation. The healthcare sector, too, works around the clock, monitoring patients in need of care. This necessitates the availability of staff outside regular working hours on both evening and night shifts. It is estimated that 17% of the European work force works in shifts.1
Shift work has been associated with negative consequences for the employee. These include impacts on health and psychosocial well-being, such as work-family conflict,2 increased fatigue,3 problems with adapting and readapting to night work,4 and an increased risk for cardiovascular disease,5 gastrointestinal problems,6 7 and cancer.8
Sick leave is a widely used outcome within occupational health research9 due to its predictive value of medically certified sick spells of >7 days for all-cause mortality.10 11 Sick leave is defined as ‘absence from work that is attributed to sickness by the employee and accepted as such by the employer’.12 However, sick leave may also mirror a variety of social, economic and psychological processes that need not be associated with an underlying illness.13
The financial costs related to sick leave are high for the employer as well as for society.14 These include sick leave benefits and salary costs of the absentee as well as salary costs of replacement staff, costs associated with lost productivity, and reduced quality of services.12 14 Long-term sick leave is seen to contribute disproportionately to these costs, while it makes up only a small fraction of the absence episodes.14 For the employee, long-term sick leave is associated with a lower probability to return to work,15 16 leading to financial deprivation as well as social isolation through exclusion from the job market.13
It is unknown whether shift work is associated with sick leave. Determining whether such an association exists can contribute to the theoretical understanding of health and psychosocial consequences of shift work. Additionally, if any such association exists, it will be clear whether interventions are necessary to improve shift workers' health and to alleviate the economic burden and social isolation associated with sick leave.
A number of reviews have been undertaken to study shift work in relation to various outcomes, such as general health outcomes,6 17–19 safety outcomes20 and work–family balance.21 However, to date, no review has been conducted that has specifically studied the association between shift work and sick leave. Thus, this review aims to establish whether an association exists between shift work and sick leave.
Methods
A systematic review was conducted to summarise the evidence for a possible association between shift work and sick leave. For the purpose of this review, shift work was defined as regular employment outside the hours 06:00–18:0022 in schedules that include evening and/or night shifts. The definition encompasses three important assumptions: (1) repetitive and regular exposure to shift work contributes to negative effects,23 24 (2) early morning work is regarded as shift work, and (3) inclusion of evening and/or night shifts ensures that a substantial amount of time is regularly spent outside standard working hours.
Search methods
Sources
Medline, CINAHL and PsycINFO were searched using EBSCOhost. EMBASE, Web of Science and NIOSHTIC-2 were searched using their internet interfaces. The electronic databases were searched from inception to 21 April 2010 for peer-reviewed articles. Additionally, references of relevant articles were hand-searched.
Search strategy
The search strategy was developed by the first author in conjunction with a search specialist affiliated with the VU University Medical Center in Amsterdam, The Netherlands. The MeSH Browser, EMTREE (EMBASE) and Major Subject Headings (PsycINFO) were consulted to retrieve useful search terms. Key terms included: work schedule tolerance (MeSH), personnel staffing and scheduling (MeSH), work rest cycles (Major Subject Heading), shift work, night shift, compressed weeks and irregulars working hours; and absenteeism (MeSH), sick leave (MeSH) and absence duration. The Boolean operators AND & OR, as well as the proximity operator NEAR, were incorporated into the search terms. (See appendix A online for the full search strategy per database.)
Selection process
Articles eligible for inclusion in the review were assessed with a selection table in which reasons for inclusion/exclusion could be indicated. One exclusion criterion was enough to exclude the study from the review. Eligibility for inclusion was restricted to the following criteria:
Language and literature: Peer-reviewed, full text articles written in English, Norwegian, Danish, Swedish, German, French, or Dutch.
Design: Observational studies: cross-sectional, case-control, and prospective or retrospective cohort studies.
Exposure: Shift work in both traditional (8-h) and compressed (10 – 12-h) style.
Control group: Day workers with working hours between 06:00 and 18:00 on week days.
Outcome: Sick leave due to illness, not due to accidents.
Data analysis: For reasons of transparency and validity, the data analysis techniques had to be reported. Further, a comparison had to have been made between the shift work and control groups.
Results: For reasons of accuracy and precision, numerical results of the comparison between the shift work and control groups had to be given, together with the 95% CI or level of significance. If the latter had not been done, data should have been provided in order for the review team to perform the calculations.
Two levels of screening were used. In the first level, titles and abstracts found in the search databases were screened for eligibility. This was done independently by two reviewers (SLM and AvD). In the second level, the full text articles were evaluated that were deemed eligible for inclusion in the first level or for which insufficient information was available to determine eligibility. In a consensus meeting agreement was reached on the full text selections. Where agreement could not be reached eligibility was settled by an arbitrator (KAH). If a full text article was written in a language foreign to reviewer AvD, then a third reviewer was asked to assess eligibility (ML). Inter-rater agreement was calculated for the full text selections using Cohen's κ coefficient.
Methodological quality assessment
Issues of selection bias, information bias and confounding were systematically appraised with a standardised checklist modified from other systematic reviews.25–27 A checklist was made for each study design: cross-sectional, prospective or retrospective cohort, and case-control. (See table 1 for an overview of the items.)
Table 1.
Standardised checklist for the assessment of methodological quality for cross-sectional (CS), case-control (CC), and prospective or retrospective cohort (PRC) studies modified from van der Windt et al,25 Hayden et al 26 and van Drongelen et al 27
| Study objective | ||
| 1. | Positive if a specific, clearly stated objective is described | CS, CC, PRC |
| Study population | ||
| 2. | Positive if the main features of the study population are described (sampling frame and distribution of the population by age and sex) | CS, CC, PRC |
| 3. | Positive if the participation rate is ≥80% or if participation rate is 60%–80% and non-response is not selective (data presented) | CS, CC, PRC |
| 3A. | Positive if the participation rate at main moment of follow-up is ≥80% or if the non-response is not selective (data presented) | PRC |
| 3A. | Positive if cases and controls were drawn from the same population and a clear definition of cases and controls was stated | CC |
| 3B. | Positive if contrast between cases and controls are big enough (controls should not be on sick leave at the time of study nor should they have been on sick leave within 6 months prior to inclusion in the study) | CC |
| Exposure assessment: shift work | ||
| 4. | Positive if data are collected and presented about shift work (starting/ending times of shifts and rotating/fixed schedule) | CS, CC, PRC |
| 5. | Method for measuring shift work: company records or personal recall during the past 3 months (+), personal recall only for a duration longer than 3 months (−) | CS, CC, PRC |
| Exposure assessment: compressed weeks | ||
| 6. | Positive if data are collected and presented about compressed weeks (no. of working hours and no. of consecutive days) | CS, CC, PRC |
| 7. | Method for measuring compressed weeks: company records or personal recall during the past 3 months (+), personal recall only for a duration longer than 3 months (−) | CS, CC, PRC |
| Outcome assessment | ||
| 8. | Method for assessing sick leave: company records or personal recall over the past 3 months (+), personal recall only for a duration longer than 3 months (−) | CS, CC, PRC |
| 8A. | Positive if data were collected for 1 year or longer | PRC |
| 8A. | Positive if exposure is measured in an identical manner in cases and controls | CC |
| Confounding assessment | ||
| 9. | Positive if data are collected and presented about occupational exposure to irregular working hours in the past | CS, CC, PRC |
| 10. | Positive if the most important confounders (age, health status) are measured and used in the analysis | CS, CC, PRC |
| 11. | Positive if data are collected and presented about the history of sick leave | CS, CC, PRC |
| 12. | Positive if confounders are measured the same for all participants using standardised methods of acceptable quality (company records or personal recall over the past 3 months) | CS, CC, PRC |
| 12A | Positive if incident cases are used (prospective enrolment) | CC |
| Analysis and data presentation | ||
| 13. | Positive if measures of association are presented (OR/RR), including 95% CIs and numbers in the analysis (totals) | CS, CC, PRC |
| 14. | Positive if the number of cases in the multivariate analysis is at least 10 times the number of independent variables in the analysis (final model) | CS, CC, PRC |
| 15. | Positive if the appropriate statistical model is used | CC |
| 15A. | Positive if a logistic regression model is used in the case of an unmatched case-control study and a conditional logistic regression model in the case of a matched case-control study | CS, PRC |
Two reviewers independently assessed the methodological quality of the studies (SLM and AvD). Items were scored positive (+) if sufficient information was given in the original article; items were scored negative (−) if the item was not considered. Items were scored non-applicable (NA) if the item did not apply to the article. If insufficient information was given, the item was scored ‘do not know’ (?). A consensus meeting was held to reach agreement on the quality items. If agreement could not be reached, the quality of an item was decided by arbitration (KAH). When an item was scored ‘do not know’, the authors of the articles were contacted and asked to elaborate on the items.
Quality scores were assigned to each article by dividing the number of positive items by the total number of applicable items. High quality studies scored over 50% and additionally reported adjusted outcomes. Low quality studies scored 50% or lower and/or only reported crude outcomes.28–30 When at least two high quality studies were available for each analysis, the low quality studies were excluded from analysis.28
Evidence synthesis
To summarise the results on the relationship between shift work and sick leave, levels of evidence synthesis was performed. This was based on the methodological quality, study design and the consistency of the study outcomes. The following criteria were based on Ariëns et al: 31
Strong evidence: Consistent findings in multiple high quality cohort or case-control studies.
Moderate evidence: Consistent findings in one high quality cohort or case-control study and multiple high quality cross-sectional studies.
Some evidence: Findings of one cohort or case-control study or consistent findings in multiple cross-sectional studies, of which at least one study was of high quality.
Inconclusive evidence: All other cases (consistent findings in multiple low quality cross-sectional studies or inconsistent findings in multiple studies).
The study outcomes were first inspected for statistical significance (p<0.05). In the case of no statistical significance, it was checked whether the effect estimates were meaningful, defined as RR/OR/HR >1.4 or <0.71. The meaningful cut-off point 1.4 was based on the upper range for significant effect estimates of work-related predictors for sick leave.32 33 The cut-off point 0.71 is the inverse of 1.4. Findings were considered to be consistent if ≥75% of the studies showed significant or meaningful results, as previously defined, in the same direction.
Data extraction
A reviewer couple independently extracted data from each article with the help of a data extraction table. One reviewer (SLM) extracted data from all included articles, while ML, TL, KAH and AvD formed a review couple with SLM for individual articles. ML and TL extracted data from 10 and 11 articles, respectively. TL was a coauthor of an additional two articles included in the review; therefore, KAH performed the data extraction from those articles. One article was written in a language that was foreign to ML, TL and KAH, and therefore AvD performed the data extraction from that article.
The following details were extracted from the articles: language, country, study design, population characteristics, sample size, participation rate (all designs), participation rate at main moment of follow-up (cohort design), working times and shift characteristics, outcome assessment, confounders measured, analysis technique used, and adjusted results.
Results
Search
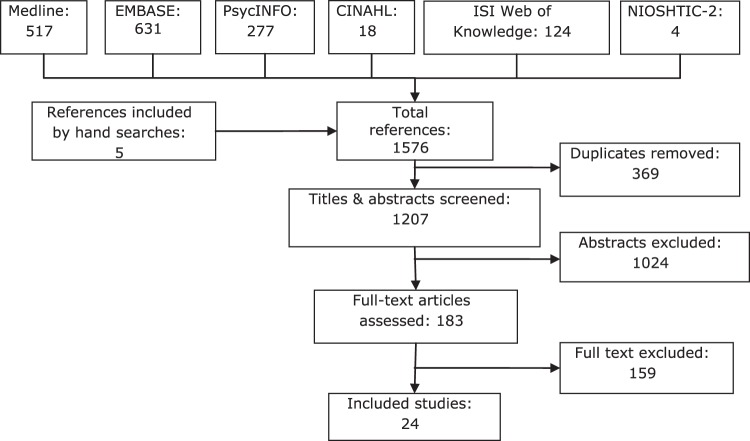
An overview of the references found in the different databases and the selection process is given in figure 1. The search strategy yielded a total of 1576 references. After removing the duplicates, 1207 titles and abstracts were screened for eligibility. From these, 183 full text articles were retrieved and further examined. This resulted in 24 articles that met the inclusion criteria.
Figure 1.
An overview of the number of articles found, screened and included in the review.
Reader couple SLM and ML assessed one full text article for eligibility, and agreed on exclusion. Reader couple SLM and AvD examined the remaining 182 full text articles. This resulted in an 80% agreement, with a Cohen's κ value of 0.52, indicating a fair inter-rater agreement.34 The main reasons for exclusion were a lack of reporting analysis techniques and numerical results.
Methodological quality assessment
The outcome of the methodological quality assessment is given in table 2. The inter-rater agreement for the quality assessment was 81%, resulting in a Cohen's κ of 0.70, reflecting good agreement between the two reviewers.34
Table 2.
Methodological quality appraisal of the studies
| Study references | Methodological items | Score (%) | Adjusted analysis | Quality | |||||||||||||||||||
| 1 | 2 | 3 | 3A | 3B | 4 | 5 | 6 | 7 | 8 | 8A | 9 | 10 | 11 | 12 | 12A | 13 | 14 | 15 | 15A | ||||
| Prospective/retrospective cohort studies | |||||||||||||||||||||||
| Tüchsen et al 35 | + | – | – | +* | – | + | NA | NA | + | + | – | + | – | + | + | +* | + | 67 | Yes | High | |||
| Tüchsen et al 36 | + | + | – | + | – | +* | NA | NA | + | + | – | + | – | + | + | ? | + | 67 | Yes | High | |||
| Angersbach et al 37 | + | – | + | – | NA | NA | + | + | + | + | – | – | – | + | – | NA | – | 50 | No | Low | |||
| Case-control studies | |||||||||||||||||||||||
| Kleiven et al 38 | + | + | + | + | – | + | + | NA | NA | + | + | – | – | – | + | + | + | + | + | 76 | Yes | High | |
| Bourbonnais et al 39 | – | + | + | + | – | – | + | NA | NA | + | + | – | – | – | + | – | + | + | + | 59 | Yes | High | |
| Cross-sectional studies | |||||||||||||||||||||||
| Higashi et al 40 | + | + | + | + | + | NA | NA | + | – | – | – | + | – | NA | + | 67 | Yes | High | |||||
| Niedhammer et al 41 | + | + | + | – | +† | NA | NA | – | – | – | – | + | + | + | + | 62 | Yes | High | |||||
| Böckerman and Laukkanen42 | + | + | – | – | +* | NA | NA | – | – | – | – | + | + | +* | + | 54 | Yes | High | |||||
| Ohayon et al 43 | + | + | – | + | + | NA | NA | – | – | – | – | + | – | + | + | 54 | Yes | High | |||||
| Eyal et al 44 | + | + | ?‡ | – | + | NA | NA | + | – | – | – | + | – | + | + | 54 | Yes | High | |||||
| Chan et al 45 | + | + | + | NA | NA | + | + | + | + | – | – | + | – | NA | + | 75 | No | Low | |||||
| Koller46 | + | + | + | + | + | NA | NA | – | + | – | – | + | – | NA | + | 67 | No | Low | |||||
| Smith et al 47 | + | + | + | – | + | NA | NA | + | – | – | – | NA | – | NA | + | 55 | No | Low | |||||
| Colligan et al 48 | + | + | + | – | + | NA | NA | + | – | – | – | + | – | NA | – | 50 | No | Low | |||||
| Drake et al 49 | + | + | – | – | + | NA | NA | + | – | – | – | + | – | NA | + | 50 | No | Low | |||||
| Chee and Rampal50 | + | + | –* | – | +* | + | +* | – | – | – | – | NA | – | NA | + | 46 | No | Low | |||||
| Lambert et al 51 | + | + | – | – | – | NA | NA | – | – | + | – | + | – | + | + | 46 | No | Low | |||||
| Olsen and Dahl52 | + | – | – | – | +† | NA | NA | – | – | – | – | + | + | + | + | 46 | No | Low | |||||
| Jamal and Baba53 | – | + | – | + | + | NA | NA | + | – | – | – | + | – | NA | – | 42 | No | Low | |||||
| Sveinsdottir54 | + | + | – | – | + | NA | NA | – | – | – | – | + | – | NA | + | 42 | No | Low | |||||
| Demerouti et al 55 | + | + | – | + | –* | NA | NA | – | – | – | – | + | – | + | – | 38 | No | Low | |||||
| Aguirre and Foret56 | + | + | ?‡ | + | – | NA | NA | – | + | – | – | – | – | NA | + | 42 | No | Low | |||||
| Drago and Wooden57 | + | + | – | – | – | NA | NA | – | – | – | – | + | – | + | + | 38 | No | Low | |||||
| Fawer and Lob58 | – | – | + | – | – | NA | NA | – | – | – | – | NA | – | NA | + | 18 | No | Low | |||||
Item changed from ‘?’ after information was retrieved from the authors.
Item changed from ‘?’ after a copy of the questionnaire was found on the internet.
Not able to establish contact with the corresponding author.
Methodological quality was appraised as high for nine of the 24 studies. The majority of all included studies received positive scores on items describing the study objectives and the study population (items 1 and 2), as well as the appropriateness of analyses (items 15 and 15A). In addition, when confounders were measured, this was done with tools of acceptable quality (item 12). However, it can be seen that confounding variables that are specific to the possible association between shift work and sick leave were seldom measured or used in the analyses (items 9, 10 and 11).
Study characteristics
Of the 24 included studies, 13 originated in Europe, six were conducted in North America, four were performed in Asia and one was a cross-country study. In all, 23 studies specified the sex of the participants: 12 studies included both male and female workers, five studies included only male participants and six studies included only female workers. A variety of populations were studied, including nurses and healthcare workers, general working populations, chemical industry workers, and law enforcement personnel.
Statistical pooling
There was a wide variation in outcome measures, study designs and shift schedules, making statistical pooling of the results impossible. Therefore, the results were summarised qualitatively.
Study quality and design
From the 24 studies that reported on the difference between shift work and day work, nine studies were assessed as high quality. These nine high quality studies were included in the levels of evidence synthesis. Four of the nine studies had a longitudinal design: two were prospective cohort studies35 36 and two were case-control studies.38 39 The remaining five had a cross-sectional design.40–44 (See table 3 for the study characteristics, table 4 for shift schedules assessed and table 5 for the outcomes and conclusions of the high quality studies.)
Table 3.
Study characteristics of the high quality studies
| Study | Quality score | Study population | Sex | Sample size | Participation rate (%) | Exposure shift workers | Recall/register period | Outcome measures |
| Prospective cohort studies | ||||||||
| Tüchsen et al 35 | 67% | Danish carers of the older population: social, nursing home, home care and healthcare assistants/helpers | Female |
|
78.7% | Fixed evening, fixed night, rotating shifts | Register: 52 weeks |
|
| Tüchsen et al 36 | 67% | Danish working population, random sample |
|
|
75% | Irregular working hours | Register: 78 weeks |
|
| Case-control studies | ||||||||
| Kleiven et al 38 | 76% | Norwegian chemical plant workers | Cases: 91.8% male Referents: 91.5% male | Cases/references: N=3580/7582 | NA: Data retrieved from registers | 3-Shift system | Register: 10 years | Sick spells >3 days |
| Bourbonnais et al 39 | 59% | Canadian nurses with sick leave diagnosed ‘most likely to be related to work load’ | Female |
|
NA: Data retrieved from registers | Fixed evening, fixed night and rotating shifts |
|
Sick spells ≥6 days for full-time workers, ≥8 days for part-time workers |
| Cross-sectional studies | ||||||||
| Higashi et al 40 | 67% | Japanese chemical fibre and textile workers in production, maintenance and service departments | Male |
|
NA: Data retrieved from registers | 3-Shift system | Register: 1 year |
|
| Niedhammer et al 41 | 62% | French workers, random sample from voluntarily participating occupational physicians | 58.2% male |
|
96.5% | Shift work without nights, fixed night, shift work including nights | Recall: 12 months | Proportion of workers who had at least 1 sick leave spell of >8 days |
| Böckerman and Laukkanen42 | 54% | Finnish workers from all sectors of the economy: mostly blue-collar workers | 58% male |
|
69% | Shift and period work as one group | Recall: 12 months | Proportion of workers with ≥2 sick leave days |
| Ohayon et al 43 | 54% | French psychiatric hospital staff: medical, maintenance, social services and administrative staff |
|
|
40.7% | 2-Shift system, fixed/rotating nights | Recall: 12 months | Proportion of workers who had at least 1 sick day |
| Eyal et al 44 | 54% | Israeli shift workers in a company: industry unknown | Male |
|
NA: Data retrieved from registers | Shift work | Register: 12 months | ≥20 accumulated days of registered absence |
Table 4.
Overview over the shift schedules for the high quality studies
| Study | Quality score | Exposure shift workers | Continuity (including/excluding weekends) | Rotation | Shift work experience | Exposure day workers |
| Prospective cohort studies | ||||||
| Tüchsen et al 35 | 67% |
|
Not given | Fixed and rotating (speed/direction not given) | Not given | Day work |
| Tüchsen et al 36 | 67% | Irregular working hours: 2-shift system, fixed evening shifts, 3-shift system and fixed nights | Not given | Fixed and rotating |
|
Permanent day work |
| Case-control studies | ||||||
| Kleiven et al 38 | 76% | 3-Shift system: slowly rotating between day/evening/night | Not given |
|
|
Day work |
| Bourbonnais et al 39 | 59% | ‘Evening, night, shift’: assumed fixed evening, fixed night and rotating shift schedules | Not given | Fixed and rotating (speed/direction not given) |
|
Day work |
| Cross-sectional studies | ||||||
| Higashi et al 40 | 67% | 3-Shift system: rotated between starting times: 06:00, 14:00 and 22:00 h | Continuous | Rotating (speed/direction not given) | Not given | Not given |
| Niedhammer et al 41 | 62% |
|
Not given | Fixed and rotating (speed/direction not given) | Not given | Day work |
| Böckerman and Laukkanen42 | 54% | Shift and period work as one group (definition used: hours worked not limited to the usual daily/weekly hours) | Not given | Not given | Not given | Non-shift and non-period workers |
| Ohayon et al 43 | 54% |
|
Not given | Fixed and rotating (speed/direction not given) | Not given | Daytime (08:00–09:00 h to 16:00–17:00 h) |
| Eyal et al 44 | 54% | Shift work | Not given | Not given |
|
Day work: white collar workers |
Table 5.
Outcomes and conclusions for the high quality studies
| Study | Quality Score | Analysis | Confounder used in analysis | Adjusted outcomes | Conclusions | ||
| Prospective cohort studies | |||||||
| Tüchsen et al 35 | 67% | Poisson regression model |
|
|
|
|
Fixed evening workers had a significantly increased risk for taking a ≥2-week and a ≥8-week sick leave spell in model 1. When additionally adjusting for work environment factors (model 2), the increased risk was still evident for ≥2-week sick leave spells, but not for ≥8-week sick leave spells |
| Tüchsen et al 36 | 67% | Cox proportional hazards model |
|
|
|
|
After adjusting for age, only shift working men showed a significantly increased risk for taking a ≥8-week sick leave spell in a year. In model 2 this association was ameliorated |
| Case-control studies | |||||||
| Kleiven et al 38 | 76% | Logistic regression, stratification | Age, sex, seniority |
|
No significant difference was found between 3-shift workers and day workers for taking sick spells lasting >3 days | ||
| Bourbonnais et al 39 | 59% | χ2 Tests, multiple logistic regression | Duration of stay, nurse to patient ratio, job title, interaction between nurse to patient ratio and job title, job classification |
|
Working night and evening shifts significantly increased the odds for sick leave, rotating shifts showed a meaningfully increased odds | ||
| Cross-sectional studies | |||||||
| Higashi et al 40 | 67% | Mantel–Haenszel test | Age |
|
3-Shift workers had a significantly lower percentage of sick leave spells than day workers, but not % lost work days | ||
| Niedhammer et al 41 | 62% | Logistic regression | Age, decision latitude, psychological demands, social support, bullying, aggression from public, occupation, work status, work hours, and physical-, ergonomic-, biological- and chemical exposure |
|
Men working shifts including nights, as well as shifts excluding nights, showed a significantly increased odds for taking sick leave. No associations were found for women | ||
| Böckerman and Laukkanen42 | 54% | Logistic regression | Sex, work sector, education, children at home, company size, replacement, work hours, match in work hours, sick leave policy | Marginal effect: 0.075 (p=0.045) | Participation in shift or period work significantly increases the prevalence of sickness absenteeism by 8% | ||
| Ohayon et al 43 | 54% | χ2, logistic regression | Age, sex, profession, children at home, daytime sleepiness, sleep duration, circadian rhythm disorders, obstructive sleep apnoea syndrome, insomnia disorder |
|
2-Shift workers had a significantly increased OR for sick leave than day workers. No difference was found between night time/rotating shifts and day workers | ||
| Eyal et al 44 | 54% | RR | Age | RR to take ≧20 days sick leave: 1.3 (p<0.05) | Blue-collar shift workers had a significantly increased RR for sick leave | ||
Summary findings
The effect estimates for an association between shift work and sick leave varied among the included studies from protective (OR 0.75; NS) to an increased risk for sick leave (OR 2.6; p<0.05). One out of the four high quality studies with a longitudinal design reported a significant increase in sick leave due to night and evening work, and a meaningful increase for rotating shift work,39 while one study found a significant increased effect for evening workers only.35
It is concluded that the findings are inconsistent (two out of four), and that there is inconclusive evidence for an association between sick leave and shift work. Including the high quality cross-sectional studies, of which four showed an increased risk for sick leave,41–44 would not have changed the consistency of the review findings (six out of nine studies with a positive association).
From table 4 it is clear that various shift schedules were included in the different studies. Shift schedules could have different effects on sick leave; therefore, a subdivision according to schedule characteristics was made. Six out of nine high quality studies described the shift schedules sufficiently to be able to group them into a category.
Evening work
Four high quality studies reported on shift work excluding nights, that is, evening work: one prospective cohort study,35 one case-control study39 and two cross-sectional studies.41 43 Tüchsen et al 35 found that fixed evening workers had a significantly increased RR for sick leave spells of ≥2 weeks. Bourbonnais et al 39 found a significantly increased OR for fixed evening shifts to take sick leave for ≥6–8 days. Niedhammer et al 41 found a significantly increased odds for male shift workers who did not work nights to take sick leave spells for >8 days, while this was not found for women. Ohayon et al 43 found a significantly increased OR for two-shift workers to take >1 day sick leave in the 12 months preceding the study.
It is concluded that the findings in the studies are consistent (three out of four) for an association between shift work excluding nights and sick leave. Two of the studies had a longitudinal design with findings in the same direction for fixed evening work among a female healthcare population. Therefore, the evidence was assessed as strong for an increased risk for sick leave with fixed evening work.
Night work
Five high quality studies reported on the association between shift work including night work and sick leave. Of these studies one had a prospective cohort design,35 two had a case-control design,38 39 and two had a cross-sectional design.40 41 Tüchsen et al 35 did not find a significant association between fixed night work or schedules that could include night work and sick leave. Kleiven et al 38 did not find a significant association between working in three shifts and taking sick leave spells >3 days. Bourbonnais et al 39 found a significantly increased odds for taking sick leave spells for ≥6-8 days for fixed night workers. Niedhammer et al 41 did not find a significant association between fixed night work and sick leave. They did find a significantly increased odds for men working shifts including nights to take sick leave spells for >8 days, with similar effect estimates for women. Higashi et al 40 found that three-shift workers had a significantly lower percentage of sick leave spells than day workers, but no significant difference was found for percentage lost days. When considering meaningful results, only Bourbonnais et al 39 found an increased meaningful result for rotating shift workers.
The findings from the studies were inconsistent. This applies to the studies with a longitudinal as well as a cross-sectional design. In total, two studies did not find an association between shift work including nights and sick leave; one study found a significantly increased odds for fixed night work, and a meaningful increase for rotating night work; one study found a significantly increased odds for men; and one study found a significantly lower sick leave. Furthermore, one study found an increased odds for sick spells but not for days lost. It is concluded that the evidence for an association between shift work including nights and sick leave was inconclusive.
Fixed shifts
Three studies focused on fixed evening and/or night shifts: one prospective cohort study,35 one case-control,39 and one cross-sectional study.41 As stated before, Tüchsen et al 35 and Bourbonnais et al 39 found significantly increased risks for fixed evening workers to take sick leave. Bourbonnais et al 39 found a significantly increased OR for fixed night shift workers to take sick leave. Tüchsen et al 35 and Niedhammer et al 41 did not find an association between fixed night shifts and sick leave.
In summary, two studies reported on fixed evening shifts, and three reported on fixed night shifts. The findings were inconsistent. The same two studies that were described under the heading ‘Evening work’ found an association between fixed evening shifts and sick leave. One study found an association between fixed night shifts and sick leave, while two did not find the latter association. It was concluded, as before, that there was strong evidence for an association between fixed evening work and sick leave. It is further concluded that there was inconclusive evidence for an association between fixed night shifts and sick leave.
Rotating shifts
Six high quality studies assessed shift work in a rotating schedule: one prospective cohort study,35 two case-control studies,38 39 and three cross-sectional studies.40 41 43 Tüchsen et al 35 and Kleiven et al 38 found no significant association between rotating shift work and sick leave. Bourbonnais et al 39 found a meaningful increased risk for rotating shifts on sick leave. Higashi et al 40 found that rotating shift workers had a significantly lower risk for percentage sick spells, but not for percentage sick days. Niedhammer et al 41 found a significantly increased odds for male rotating shift workers to take sick leave. Ohayon et al 43 found that rotating two-shift workers showed a significantly increased odds for sick leave compared with day workers.
It is concluded that the study findings are inconsistent and that there is inconclusive evidence for an association between rotating shift work and sick leave. Two studies with a longitudinal design found no association between rotating shift work and sick leave, while one found a meaningful increased risk. Two cross-sectional studies reported an increased odds for sick leave, while one reported a risk reduction.
Shift duration
Four high quality studies reported on traditional 8-h shift work in comparison with day work. One had a prospective cohort design,35 one had a case-control design,38 and two had a cross-sectional design.40 43
Tüchsen et al 35 found a significantly increased risk for 8-h fixed evening shift workers to take sick leave, but they did not find an association for 8-h rotating schedules. Kleiven et al 38 did not find an association between 8-h shifts and sick leave. Higashi et al 40 found a significantly lower risk for rotating three-shift workers to take sick leave spells, but did not find the association for individual sick days. Ohayon et al 43 found a significantly increased risk for two-shift workers to take sick leave, but not for rotating or night shift workers. The findings for 8-h shifts were inconsistent; there is inconclusive evidence for an association between 8-h shift work and sick leave.
Two low quality studies37 45 reported on 12-h shifts in comparison with day work. They both had a cross-sectional design and did not report adjusted outcomes. It was therefore concluded that there is inconclusive evidence for the association between 12-h shifts and sick leave.
Discussion
The review found strong evidence for a positive association between fixed evening work and sick leave among female healthcare workers. Evidence was assessed as inconclusive for the following associations with sick leave: rotating shifts, shift work including nights, fixed night shifts, as well as 8-h and 12-h shifts.
Strengths and limitations of the review
A strength of the current review is the addition of the criterion ‘reporting adjusted outcomes’ to the high quality scores. The quality assessment form used in this review was based on previous systematic reviews where all items were weighed equally.25–27 Weighing selection bias, information bias and confounding equally assumes that the biases are equally important in influencing the study outcomes and can therefore overestimate the quality of the studies. Adding an important criterion to the quality score can adjust for this overestimation. The most often assessed quality item in systematic reviews is ‘adjustment for confounding’,59 and therefore this was used as the additional quality criterion.
An additional strength of the review was the modification of the levels of evidence from an earlier review by Ariëns et al. 31 The moderate level of evidence was revised from ‘consistent findings in multiple cohort or case-control studies, of which only one study was of high quality’ to ‘consistent findings in one high quality cohort or case-control study and multiple high quality cross-sectional studies’. The version by Ariëns et al 31 was based on the assumption that longitudinal study designs increase the validity of evidence for an association between two variables when compared with cross-sectional studies. As the validity of a study depends more on the quality of the study than on its design, the levels of evidence were adapted to increase the weight of high quality cross-sectional studies over low quality longitudinal studies.
The levels of evidence synthesis in this review were based on significant and/or meaningful effect estimates; both approaches have strengths and limitations. The strength of significant findings is their valid effect estimates in 95% of similar studies when repeated, yet the effect warrants discussion as to whether the size is important. The strength of including non-significant meaningful effects is not missing studies that can contribute to the building of evidence. However, use of arbitrary cut-off points, as done in previous reviews,60 61 questions the legitimacy of the meaningfulness. In the current review, on the contrary, the cut-off points were based on effect estimates found in the sick leave literature.32 33 Caution should be applied in using meaningful estimates, as they are only valid in studies with overall high quality yet low sample sizes. For instance, Bourbonnais et al 39 found a non-significant association between rotating shifts and sick leave. Use of a meaningful estimate was plausible, reasoning that in this high quality study a larger sample would narrow the 95% CI and make the association significant. This changed the conclusion from a strong level of evidence for no association between rotating shifts and sick leave to inconclusive evidence for this association. This warrants further research into the topic.
Strengths and limitations of the studies
The included studies often lacked detailed information on schedule characteristics, whereby the differentiations were not clear-cut, making it difficult to interpret the schedule characteristics' effects on sick leave. Additionally, three included studies appraised as high quality did not specify or differentiate between schedule characteristics,36 42 44 and could not be used in the detailed analysis. Reducing the number of studies in the analysis lowers the chance to detect moderate or strong evidence for associations, which means that if the studies had included schedule characteristics this could have led to different conclusions of this review.
In the scientific literature there is little agreement on definition, measurement methods and reporting units of sick leave.9 This was reflected in the included studies. The definition of sick leave was not given in some studies,41 43 while in other studies it was defined42 or categorised according to diagnosis.38 40 Various reporting units were used: average number of sick leave (spells) per group, proportions of sick leave41 42 and sick leave for time at risk.35 As sick leave is regarded to mirror a variety of factors, such as health,14 15 and psychosocial processes,14 a uniform sick leave outcome could increase the understanding of the processes that underlie sick leave.
Possible explanations of the findings
In the nine studies that reported adjusted results, differences existed in the size of the adjusted effect estimates. A source of between-study variance could lie in the different confounders that were adjusted for. Adjusting for confounders is important in sick leave research due to the multifactorial causes of sick leave.14 Adjustment leads to a more precise effect estimate for the association between shift work and sick leave, with important confounders being age, shift work experience, work environmental factors as well as health indicators. Six of the nine high quality articles adjusted for work environmental factors or proxies thereof;35 36 39 41–43 however, only two articles adjusted for health indicators,35 43 and none adjusted for shift work experience. Adjustment for psychosocial and physical work environment factors could have led to lower effect estimates for shifts excluding night work35 39 41 than when no adjustment was made for these factors.43 Adjusting for work environmental factors could also explain the lower effect estimates found for fixed night shifts35 41 than when adjusting for proxies of work environment factors.39 The two articles that adjusted for health indicators varied to such an extent that it cannot be stated which effect the adjustment had on the size of the effect estimates.
The positive association found between fixed evening shifts and sick leave was based on two studies with similar effect sizes as found in other research for work-related factors.32 33 The relatively low estimates (RR 1.2935 and OR 1.67)39 are regarded to be a consequence of the multifactorial nature of sick leave. The study outcomes were long-term sick leave spells of ≥2 weeks35 and ≥6–8 days,39 respectively. The predictive value of longer sick leave spells of >3 or >7 days for all-cause mortality15 16 and disability pensioning62 suggests that long-term sick leave mirrors an underlying biomedical condition. It could therefore imply that fixed evening work is associated with ill health in female healthcare workers. Whether this is a causal relation remains unknown.
Possible explanations for the association could not be found in the articles; therefore, only hypotheses can be proposed that can be tested further. First, a plausible hypothesis is sick leave as a consequence of repetitive exposure to the same tasks inherent to working fixed shifts. A similar population of female evening workers reported more physical handling tasks than day workers,63 which in the study by Tüchsen et al 35 could have caused musculoskeletal problems and sick leave. Second, low management support is associated with sick leave in women,64 and was evident in a similar population.63 Management staff are often less available in evening hours which could explain the low management support. Last, it is proposed that willingness to work fixed evenings could be a coping behaviour: night workers or day workers with existing health problems could transfer to evening work due to the lower overall work load associated with it.63
Contrary to expectations, the evidence for an association between shift work including nights and sick leave was inconclusive. Current research is focusing on night work as the main contributing factor for ill health,8 65 66 yet this review did not support this hypothesis. Possible differences between studies with regard to the data extracted on population characteristics (sex, country of origin, work sector, confounders) that could explain the varying study outcomes were not found.
A possible explanation could include differences between studies with regard to population characteristics that were not measured, such as shift work experience and health indicators that could lead to the ‘healthy worker effect’. It is a common phenomenon in the shift work literature, where shift work tolerant individuals are hypothesised to be relatively healthy and continue working in shifts (selection into shift work), while those who are less tolerant stop working shifts (selection out of shift work).3 It is possible that the participants of some studies included in this review were relatively healthy individuals, thereby underestimating the association between shift work and sick leave.
Recommendations for future research
The review findings indicate that the existence of an association between shift work and sick leave is schedule specific, due to the strong association found for fixed evening work and inconclusive evidence for other shift types. This indicates that shift work, as a collective phrase, is too broad and that the phrase should be broken down into exposure characteristics and studied accordingly. Surprisingly, a relatively large number of high quality studies (three out of nine) included in the review did not do this. It is therefore recommended to gather more specific information with regard to shift schedule characteristics and use them in the analyses.
Just over a third of the included studies adjusted for confounding, and none adjusted for an important confounder, namely shift work experience. The cumulative effects of exposure to shift work on shift work tolerance and health are hypothesised to have a high explanatory value,23 24 but it was often not assessed or reported. Seniority or time at a company, as reported in three articles,38 39 44 is a poor proxy for shift work experience. It does not take into account that employees can change between shift work and day work, and thereby might overestimate the exposure to shift work. It is recommended to assess shift work experience in more detail in future studies on shift work and sick leave.
Conclusions
Fixed evening work was found to be positively associated with sick leave in female healthcare workers. This implies that a possible association between shift work and sick leave might be dependent on schedule characteristics as well as population characteristics. Future research should include the assessment of schedule characteristics and exposure to these characteristics over time when studying the association between shift work and sick leave.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the contribution of René Otten at the VU Amsterdam Medical Library for his contribution in the development of the search strategy.
Footnotes
Contributors: It is stated that all the authors contributed sufficiently to the conception and design of the paper as well as to the data collection. All authors additionally contributed sufficiently to the critical revision of the paper for important intellectual content, and approve of the final version to be submitted for review.
Funding: This review received funding from the Research Council of Norway.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. European foundation for the improvement of living and working conditions. Changes over time – First findings from the fifth European Working Conditions Survey. Luxembourg: Publications Office of the European Union, 2011 [Google Scholar]
- 2. Haines VY, Marchand A, Rousseau V, et al. The mediating role of work-to-family conflict in the relationship between shiftwork and depression. Work Stress 2008;22:341–56 [Google Scholar]
- 3. Jansen NW, van Amelsvoort LG, Kristensen TS, et al. Work schedules and fatigue: a prospective cohort study. Occup Environ Med 2003;60(Suppl 1):i47–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bjorvatn B, Kecklund G, Akerstedt T. Rapid adaptation to night work at an oil platform, but slow readaptation after returning home. J Occup Environ Med 1998;40:601–8 [DOI] [PubMed] [Google Scholar]
- 5. van der Hulst M. Long workhours and health. Scand J Work Environ Health 2003;29:171–88 [DOI] [PubMed] [Google Scholar]
- 6. Harrington JM. Shift work and health - a critical review of the literature on working hours. Ann Acad Med Singapore 1994;23:699–705 [PubMed] [Google Scholar]
- 7. Knutsson A, Bøggild H. Gastrointestinal disorders among shift workers. Scand J Work Environ Health 2010;36:85–95 [DOI] [PubMed] [Google Scholar]
- 8. Pesch B, Harth V, Rabstein S, et al. Night work and breast cancer - results from the German GENICA study. Scand J Work Environ Health 2010;36:134–41 [DOI] [PubMed] [Google Scholar]
- 9. Hensing G, Alexanderson K, Allebeck P, et al. How to measure sickness absence? Literature review and suggestion of five basic measures. Scand J Soc Med 1998;26:133–44 [DOI] [PubMed] [Google Scholar]
- 10. Kivimaki M, Head J, Ferrie JE, et al. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003;327:364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vahtera J, Pentti J, Kivimaki M. Sickness absence as a predictor of mortality among male and female employees. J Epidemiol Community Health 2004;58:321–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Whitaker SC. The management of sickness absence. Occup Environ Med 2001;58:420–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Labriola M. Conceptual framework of sickness absence and return to work, focusing on both the individual and the contextual level. Work 2008;30:377–87 [PubMed] [Google Scholar]
- 14. Henderson M, Glozier N, Holland EK. Long term sickness absence. BMJ 2005;330:802–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Borg K, Hensing G, Alexanderson K. Predictive factors for disability pension - a 11-year follow up of young persons on sick leave due to neck, shoulder, or back diagnoses. Scand J Public Health 2001;29:104–12 [PubMed] [Google Scholar]
- 16. Kivimaki M, Forma P, Wikstrom J, et al. Sickness absence as a risk marker for future disability pension: the 10-town study. J Epidemiol Community Health 2004;58:710–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Smith L, Folkard S, Tucker P, et al. Work shift duration: a review comparing eight hour and 12 hour shift systems. Occup Environ Med 1998;55:217–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Knutsson A. Health disorders of shift workers. Occup Med (Lond) 2003;53:103–8 [DOI] [PubMed] [Google Scholar]
- 19. Bambra CL, Whitehead MM, Sowden AJ, et al. Shifting schedules: the health effects of reorganizing shift work. Am J Prev Med 2008;34:427–34 [DOI] [PubMed] [Google Scholar]
- 20. Wagstaff AS, Sigstad Lie JA. Shift and night work and long working hours - a systematic review of safety implications. Scand J Work Environ Health 2011;37:173–85 [DOI] [PubMed] [Google Scholar]
- 21. Bambra C, Whitehead M, Sowden A, et al. “A hard day's night?” The effects of compressed working week interventions on the health and work-life balance of shift workers: a systematic review. J Epidemiol Community Health 2008;62:764–77 [DOI] [PubMed] [Google Scholar]
- 22. Albertsen K, Rafnsdottir GL, Grimsmo A, et al. Workhours and worklife balance. SJWEH supplements 2008;5:14–21 [Google Scholar]
- 23. Costa G. The impact of shift and night work on health. Appl Ergon 1996;27:9–16 [DOI] [PubMed] [Google Scholar]
- 24. Rouch I, Wild P, Ansiau D, et al. Shiftwork experience, age and cognitive performance. Ergonomics 2005;48:1282–93 [DOI] [PubMed] [Google Scholar]
- 25. van der Windt DA, Thomas E, Pope DP, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Environ Med 2000;57:433–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med 2006;144:427–37 [DOI] [PubMed] [Google Scholar]
- 27. van Drongelen D, Boot C, Merkus SL, et al. The effects of shift work on body weight change - a systematic review of longitudinal studies. Scand J Work Environ Health 2011;37:263–75 [DOI] [PubMed] [Google Scholar]
- 28. Hoogendoorn WE, van Poppel MN, Bongers PM, et al. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine (Phila Pa 1976) 2000;25:2114–25 [DOI] [PubMed] [Google Scholar]
- 29. van Tulder M, Furlan A, Bombardier C, et al. Updated method Guidelines for systematic reviews in the Cochrane Collaboration back review group. Spine (Phila Pa 1976) 2003;28:1290–9 [DOI] [PubMed] [Google Scholar]
- 30. Wai EK, Roffey DM, Bishop P, et al. Causal assessment of occupational lifting and low back pain: results of a systematic review. Spine J 2010;10:554–66 [DOI] [PubMed] [Google Scholar]
- 31. Ariëns GA, van Mechelen W, Bongers PM, et al. Physical risk factors for neck pain. Scand J Work Environ Health 2000;26:7–19 [DOI] [PubMed] [Google Scholar]
- 32. Ala-Mursula L, Vahtera J, Kivimaki M, et al. Employee control over working times: associations with subjective health and sickness absence. J Epidemiol Community Health 2002;56:272–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Labriola M, Lund T, Burr H. Prospective study of physical and psychosocial risk factors for sickness absence. Occup Med (Lond) 2006;56:469–74 [DOI] [PubMed] [Google Scholar]
- 34. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, 2011. Version 5.1. [updated March 2011]. http://www.cochrane-handbook.org [Google Scholar]
- 35. Tüchsen F, Christensen KB, Nabe-Nielsen K, et al. Does evening work predict sickness absence among female carers of the elderly? Scand J Work Environ Health 2008;34:483–6 [DOI] [PubMed] [Google Scholar]
- 36. Tüchsen F, Christensen KB, Lund T. Shift work and sickness absence. Occup Med (Lond) 2008;58:302–4 [DOI] [PubMed] [Google Scholar]
- 37. Angersbach D, Knauth P, Loskant H, et al. A retrospective cohort study comparing complaints and diseases in day and shift workers. Int Arch Occup Environ Health 1980;45:127–40 [DOI] [PubMed] [Google Scholar]
- 38. Kleiven M, Bøggild H, Jeppesen HJ. Shift work and sick leave. Scand J work Environ health 1998;24(Suppl 3):128–33 [PubMed] [Google Scholar]
- 39. Bourbonnais R, Vinet A, Vezina M, et al. Certified sick leave as a non-specific morbidity indicator: a case-referent study among nurses. Br J Ind Med 1992;49:673–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Higashi T, Sakurai H, Satoh T, et al. Absenteeism of shift and day workers with special reference to peptic ulcer. Asia Pac J Public Health 1988;2:112–19 [DOI] [PubMed] [Google Scholar]
- 41. Niedhammer I, Chastang JF, David S. Importance of psychosocial work factors on general health outcomes in the national French SUMER survey. Occup Med (Lond) 2008;58:15–24 [DOI] [PubMed] [Google Scholar]
- 42. Böckerman P, Laukkanen E. What makes you work while you are sick? Evidence from a survey of workers. Eur J Public Health 2010;20:43–6 [DOI] [PubMed] [Google Scholar]
- 43. Ohayon MM, Lemoine P, Arnaud-Briant V, et al. Prevalence and consequences of sleep disorders in a shift worker population. J Psychosom Res 2002;53:577–83 [DOI] [PubMed] [Google Scholar]
- 44. Eyal A, Carel RS, Goldsmith JR. Factors affecting long-term sick leave in an industrial population. Int Arch Occup Environ Health 1994;66:279–82 [DOI] [PubMed] [Google Scholar]
- 45. Chan OY, Gan SL, Yeo MH. Study on the health of female electronics workers on 12 hour shifts. Occup Med (Lond) 1993;43:143–8 [DOI] [PubMed] [Google Scholar]
- 46. Koller M. Health risks related to shift work. An example of time-contingent effects of long-term stress. Int Arch Occup Environ Health 1983;53:59–75 [DOI] [PubMed] [Google Scholar]
- 47. Smith MJ, Colligan MJ, Tasto DL. Health and safety consequences of shift work in the food processing industry. Ergonomics 1982;25:133–44 [DOI] [PubMed] [Google Scholar]
- 48. Colligan MJ, Frockt IJ, Tasto DL. Frequency of sickness absence and worksite clinic visits among nurses as a function of shift. Appl Ergon 1979;10:79–85 [DOI] [PubMed] [Google Scholar]
- 49. Drake CL, Roehrs T, Richardson G, et al. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004;27:1453–62 [DOI] [PubMed] [Google Scholar]
- 50. Chee HL, Rampal KG. Relation between sick leave and selected exposure variables among women semiconductor workers in Malaysia. Occup Environ Med 2003;60:262–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lambert EG, Edwards C, Camp SD, et al. Here today, gone tomorrow, back again the next day: antecedents of correctional absenteeism. J Crim Justice 2005;33:165–75 [Google Scholar]
- 52. Olsen KM, Dahl SA. Working time: implications for sickness absence and the work-family balance. Int J Soc Welf 2010;19:45–53 [Google Scholar]
- 53. Jamal M, Baba VV. Shiftwork, burnout, and well-being: a study of Canadian nurses. Int J Stress Manag 1997;4:197–204 [Google Scholar]
- 54. Sveinsdóttir H. Self-assessed quality of sleep, occupational health, working environment, illness experience and job satisfaction of female nurses working different combination of shifts. Scand J Caring Sci 2006;20:229–37 [DOI] [PubMed] [Google Scholar]
- 55. Demerouti E, Geurts SA, Bakker AB, et al. The impact of shiftwork on work-home conflict, job attitudes and health. Ergonomics 2004;47:987–1002 [DOI] [PubMed] [Google Scholar]
- 56. Aguirre A, Foret J. Irregularity of working hours in railway workers and types of complaints. Int Arch Occup Environ Health 1994;65:367–71 [DOI] [PubMed] [Google Scholar]
- 57. Drago R, Wooden M. The determinants of labor absence - economic-factors and workgroup norms across countries. Ind Labor Relat Rev 1992;45:764–78 [Google Scholar]
- 58. Fawer R, Lob M. Pathology of shift work. Study of 4 state-owned factories. Soz Praventivmed 1979;24:264. [DOI] [PubMed] [Google Scholar]
- 59. Mallen C, Peat G, Croft P. Quality assessment of observational studies is not commonplace in systematic reviews. J Clin Epidemiol 2006;59:765–9 [DOI] [PubMed] [Google Scholar]
- 60. Kuijpers T, van der Windt DA, van der Heijden GJ, et al. Systematic review of prognostic cohort studies on shoulder disorders. Pain 2004;109:420–31 [DOI] [PubMed] [Google Scholar]
- 61. Ijmker S, Huysmans MA, Blatter BM, et al. Should office workers spend fewer hours at their computer? A systematic review of the literature. Occup Environ Med 2007;64:211–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kivimaki M, Ferrie JE, Hagberg J, et al. Diagnosis-specific sick leave as a risk marker for disability pension in a Swedish population. J Epidemiol Community Health 2007;61:915–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Nabe-Nielsen K, Tüchsen F, Christensen KB, et al. Differences between day and nonday workers in exposure to physical and psychosocial work factors in the Danish eldercare sector. Scand J Work Environ Health 2009;35:48–55 [DOI] [PubMed] [Google Scholar]
- 64. Vaananen A, Toppinen-Tanner S, Kalimo R, et al. Job characteristics, physical and psychological symptoms, and social support as antecedents of sickness absence among men and women in the private industrial sector. Soc Sci Med 2003;57:807–24 [DOI] [PubMed] [Google Scholar]
- 65. Conway PM, Campanini P, Sartori S, et al. Main and interactive effects of shiftwork, age and work stress on health in an Italian sample of healthcare workers. Appl Ergon 2008;39:630–9 [DOI] [PubMed] [Google Scholar]
- 66. Frost P, Kolstad HA, Bonde JP. Shift work and the risk of ischemic heart disease - a systematic review of the epidemiologic evidence. Scand J Work Environ Health 2009;35:163–79 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.