Abstract
Little is known about how place affects childrens’ access to dental care. We analyzed data for 25,908 Iowa Medicaid-enrolled children with chronic conditions to identify the county-level determinants of dental utilization. Our analyses suggest that higher levels of poverty and designation as a dental health professional shortage area at the county-level are associated with lower probability of child-level dental use. There are significant interactions between child-level race/ethnicity and county-level poverty as well as between child-level disability and county-level unemployment. We present a new descriptive model on dental utilization that emphasizes county-level factors as well as interactions between county-level and child-level factors.
Keywords: Residence characteristics, Dental care for children, Healthcare disparities, Medicaid, Dental health services
1. Introduction
The 2008 World Health Organization’s Report “Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health” highlights the importance of intervening on the social determinants of health (Commission on Social Determinants of Health, 2008). An important but poorly understood determinant of children’s dental care utilization includes the places in which children are born, grow, and live (World Health Organization, 2011). Place is likely to play a significant role in developing interventions and policies, including those aimed at improving dental care use for vulnerable children at increased risk for dental caries and poor oral health. However, very little is known about how place affects dental utilization for vulnerable children.
1.1. Dental caries etiology and prevention
Dental caries (tooth decay) is the most common childhood disease in the U.S. (U.S. Department of Health and Human Services 2000). Caries is an infectious disease caused by mutans streptococci, lactobacilli, and other bacterial species (Berkowitz, 2006). These bacteria colonize tooth surfaces, metabolize carbohydrates introduced into the oral cavity, and produce acid byproducts that lead to tooth decay (Selwitz et al., 2007). Similar to childhood diseases like asthma (Mendes et al., 2011) and obesity (Centers for Disease Control and Prevention, 2009), tooth decay is a multi-factorial disease. When left untreated, tooth decay can lead to pain, localized infection, disfigurement, hospitalization, and in rare cases death caused by sepsis (Nuttall et al., 2006; Lewis and Stout, 2010). Poor oral health is associated with cardiovascular disease, stroke, and kidney disease (Franco et al., 1996; Ylöstalo et al., 2006; Nakano et al., 2007; Zoellner, 2011; Lalla et al., 2006; Fisher and Taylor, 2009) as well as increased levels of inflammatory mediators (e.g., cytokines, C-reactive proteins) involved in chronic disease processes (Hayashi et al., 2010; Teles and Wang, 2011). These studies suggest links between oral and systemic health. Equally important, poor oral health has consequences over the life course that manifest as learning difficulties in the classroom, school absenteeism, lost work days, difficulties eating, and low oral health-related quality of life (Gift et al., 1992; Patel et al., 2007; Zeng et al., 2008; Jackson et al., 2011). Most cases of tooth decay can be prevented by engaging in home-based preventive behaviors such as brushing twice daily with fluoride toothpaste, drinking optimally fluoridated water, and limiting intake of sugared foods and beverages (Tinanoff et al., 2002).
1.2. Importance of dental visits
Dental visits play a central role in a comprehensive tooth decay prevention and management strategy for children for two main reasons. First, dental visits allow caregivers the opportunity to receive prevention-oriented oral health education from dentists in the form of anticipatory guidance (Plutzer and Spencer, 2008). Second, children are able to benefit directly from diagnostic and preventive treatment (e.g., radiographs, examinations, pit and fissure sealants, topical fluoride treatments) as well as restorative care when disease is already present (American Academy of Pediatric Dentistry, 2011). Dental care can help improve health outcomes in children with chronic conditions such as leukemia and other malignancies during bone marrow transplant treatment (Vaughan et al., 2005) by preventing systemic infections. Another example relates to children with orofacial conditions, many of whom require multiple dental and medical surgical interventions. Addressing the complex oral health care needs of children with orofacial conditions is likely to improve their quality of life (Locker et al., 2005) as well as other factors such as family functioning (Locker et al., 2002).
1.3. Medicaid-enrolled children encounter barriers to dental care use
Not all children have equal access to dental care. Disparities in dental care use affect a number of subgroups, including children with chronic conditions, for whom dental care is the most common unmet health care need (Newacheck et al., 2000; Lewis et al., 2005). This is a significant clinical and public health problem because as many as 1 in 5 children in the U.S. have a chronic condition, defined as a developmental, physical, behavioral, or emotional ailment expected to last at least 12 months (Muldoon et al., 1997). Medicaid (Title XIX of the U.S. Social Security Amendments of 1964) is a publicly-financed health insurance program aimed at improving access to health care services for low-income children, including those with chronic conditions. Under the federal Early, Periodic Screening, Diagnosis, and Treatment (EPSDT) Program, state Medicaid programs are required to provide children with preventive and basic restorative dental care services. Over 70% of low-income children with chronic conditions in the U.S. participate in Medicaid (Kaiser Commission on Medicaid and the Uninsured, 2007). While children in Medicaid are more likely to use dental care than children without dental insurance, they are significantly less likely to use dental care than privately-insured children (Dubay and Kenney, 2001; Bloom et al., 2006; Fisher and Mascarenhas, 2007). Previous studies have documented dentist-reported barriers to care such as limited knowledge on how to manage children with chronic conditions, insufficient reimbursement rates, and administrative burdens associated with filing Medicaid claims (Casamassimo et al., 2004; Blackwelder and Shulman, 2007). Caregiver-reported barriers include low oral health literacy, inability to find a dental office that accepts Medicaid insurance, discrimination by front office staff, and unreliable transportation (Lam et al., 1999; Kelly et al., 2005; Brickhouse et al., 2009). Child-level barriers to dental care that specifically affect Medicaid-enrolled children with chronic conditions include older age, male gender, having a severe chronic health condition, having a caregiver enrolled in Medicaid, and living in a dental Health Professional Shortage Area (Chi et al., 2011).
1.4. Factors associated with place may explain heterogeneity in dental use
There has been strong interest in understanding how and why place contributes to health disparities (Kramer and Hogue, 2008). These disparities are present at multiple levels (e.g., states, neighborhoods) (Bethell et al., 2010). For example, racial and ethnic residential segregation is one of the key contributors to health inequalities (White et al., 2012) and neighborhood-level social disadvantage has been documented as a risk factor for childhood obesity (Grow et al., 2010). Work from the dental literature suggests that peer density is related to self-reported oral health for older adults in urban settings (Widener et al., 2012). While previous work has examined the impact of city-level socioeconomic status and caries in children (Antunes et al., 2003), no studies have examined the relationship between place and dental use for socioeconomically and medically vulnerable children.
There are a number of policies and interventions that seek to improve dental care use among Medicaid-enrolled children. A common policy approach is to increase dental reimbursement rates (Eklund et al., 2003). While this may encourage additional dentists to treat Medicaid-enrolled children, such approaches that focus solely on supply side economics are unlikely to lead to drastic improvements in dental use (Kenney et al., 2011) because patient demand for care is unaltered. There are two examples of place-based oral health interventions aimed at Medicaid-enrolled children. The first is North Carolina’s Into the Mouth of Babes Program, which focuses on the delivery of preventive dental care within medical office settings (Close et al., 2010). While over 70% of recruited medical providers participated in the program, little is known about the place-based factors related to variation in provider participation. The second example is Washington State’s Access to Baby and Child Dentistry (ABCD) Program, which adopts a comprehensive approach by increasing reimbursement rates, training dentists on advanced child behavior management techniques, and providing enhanced dental benefits for children and case coordination services to families (Grembowski and Milgrom, 2000). However, even programs like ABCD have led to unequal improvements in dental use by Medicaid-enrolled children across counties (Washington State Health Care Authority, 2012). While changes to Medicaid dental programs are legislated at the state-level, implementation occurs at the county-level. A possible explanation for county-level heterogeneity in dental use within interventions like the ABCD Program is a failure to account for area-level factors that differ across counties.
We currently have no knowledge about the particular features of place that affect dental care use for Medicaid-enrolled children with chronic conditions. The goals of this study were to test three hypotheses: (1) county-level factors are important determinants of child-level dental care use for Medicaid-enrolled children with chronic conditions; (2) there are interactions between child-level factors (within-level interactions); and (3) there are interactions between child- and county-level factors (cross-level interactions). We expect to generate the knowledge needed to develop interventions and policies that account for place and ultimately reduce disparities in dental care use for publicly-insured children.
2. Methods
2.1. Conceptual framework
This study was guided by an ecological model of health (McLeroy et al., 1988). An important feature of the ecological model is the recognition that the determinants of health exist at multiple levels. We defined place as counties as in previous population-based studies (Hatzenbuehler et al., 2011). Predictor variables were organized into two levels: child-level or county-level (see Section 2.4).
2.2. Study population
We focused on children ages 3–14 years who were enrolled in the Iowa Medicaid Program for 11–12 months in 2005 and 2006. The 11–12 month criterion is consistent with Healthcare Effectiveness Data and Information Set (HEDIS) specifications (Healthcare Effectiveness Data and Information Set, 2012). Each child in the study had a chronic condition as identified by the 3M Clinical Risk Grouping (CRG) software—a validated risk-adjustment tool used to identify children with long-term medical conditions from large claims datasets (Hughes et al., 2004; Neff et al., 2010). We excluded: (1) children younger than age 3 because chronic conditions are not typically diagnosed until age 3 (Pinto-Martin et al., 2005) and dental use for infants is low (Kanellis et al., 1997), which suggests heterogeneous determinants of dental use for very young children; (2) children ages 15–18 because this subgroup exhibits dental utilization patterns that are unique to late adolescence (Eklund et al., 2003); and (3) children with malignancies because these individuals have health utilization patterns that are different from other children with chronic conditions (Merrill et al., 2007). Our final study population consisted of 25,908 children ages 3–14 years.
2.3. Data
This study was approved by the University of Washington Institutional Review Board. There were two data sources linked by a county variable available in both. The first was child-level enrollment and claims data from the Iowa Medicaid Program from 2003 to 2006. The enrollment files included the child’s date of birth, gender, race/ethnicity, Medicaid eligibility program, zip code, and county of residence. The claims files included all medical diagnoses by International Classification of Diseases, 9th Revision, Clinical Modifications (ICD-9) code, inpatient, out-patient, pharmacy, and dental claims (data needed by the CRG software to identify chronic conditions in children). Dental claims were identified by Current Dental Terminology (CDT) Codes, five digit alphanumeric codes used for reimbursement. The second data source was county-level data from the U.S. Department of Health and Human Services Area Resource Files (ARF).
2.4. Measures
2.4.1. Outcome variable
The main outcome measure was child-level dental care use in 2006. A child with at least one claim for any dental service was classified as having used dental care. All other children were classified as not having used dental care.
2.4.2. Child-level predictor variables
We included eight child-level variables in our models: age (3–5, 6–11, 12–14 years), gender (male/female), and race/ethnicity (White, Black, other, missing/unknown). Intellectual or developmental disability (IDD) status (no/yes) was assessed by applying five criteria used in a previous study to identify Medicaid-enrolled children with IDD using claims data (Chi et al., 2010). Chronic condition severity was defined as the condition-stable clinical group to which the child was assigned (episodic, life-long, or complex chronic condition) (Chi et al., 2011). The remaining child-level predictor variables were measures (no/yes) of whether the child had a Medicaid-enrolled sibling, a Medicaid-enrolled caregiver, and preventive medical care use in 2005.
2.4.3. County-level predictor variables
We focused on 11 county-level factors relevant to child dental utilization (continuous measures unless otherwise noted). County-level factors were organized into two conceptual domains (Table 2).
Table 2.
Linear regression models of dental utilization for Medicaid-enrolled children with chronic conditions (N=25,908 children; n=99 counties).
| β coefficient* | Robust standard error | Robust z value | P-value | |
|---|---|---|---|---|
| County-level factors | ||||
| Socioeconomic environment | ||||
| Percent population in poverty (2005) | −0.0084 | 0.0018 | −4.57 | <0.0001 |
| Unemployment rate for persons ages 16 and older (2005) | −0.0190 | 0.0118 | −1.60 | 0.1096 |
| Health resource environment | ||||
| County designated as a dental Health Professional Shortage Area (2004) | 0.0283 | |||
| No | Reference | – | – | |
| Yes | −0.0338 | 0.0154 | −2.19 | |
| Rurality (2003) | ||||
| Metropolitan | Reference | – | – | – |
| Urban adjacent to metropolitan | −0.0280 | 0.0183 | −1.53 | 0.1259 |
| Urban not adjacent to metropolitan | −0.0210 | 0.0249 | −0.85 | 0.3981 |
| Rural | −0.0044 | 0.0227 | −0.19 | 0.8459 |
Adjusted for child-level predictor variables (age, gender, race/ethnicity, IDD status, chronic condition severity, sibling enrolled in Medicaid, caregiver enrolled in Medicaid, used preventive medical care).
2.4.3.1. Socioeconomic environment (degree of environmental social disadvantage)
Per capita income, population poverty, child poverty, unemployment, percent uninsured, percent of population on food assistance, percent of children in Medicaid.
2.4.3.2. Health resource environment (health workforce and service utilization environment)
Dental Health Professional Shortage Area designation (no/yes), physician density, emergency department visits, rurality (four categories consistent with the U.S. Department of Agriculture Urban-Rural Continuum Codes: metropolitan, urban adjacent to metropolitan, urban not adjacent to metropolitan, rural).
2.5. Statistical analyses and model building
We used linear probability models because they yield estimates of differences in the probability of utilization between groups, which are more easily interpretable than estimates (such as odds ratios) from other models commonly used for binary data (Caudill, 1988), as illustrated by recent examples in social science and medicine (Tsai et al., 2006; Kakaiya et al., 2010; Ngo et al. (2006)). The use of linear models for binary data is also justified by the large sample size (Lumley et al., 2002). Although we did not use logistic regression models to estimate odds ratios, to assess the sensitivity of our statistical approach, we repeated the analyses using logistic regression models and verified that the observed statistical significance levels of model terms were similar for linear and logistic models. The multilevel nature of the data was accounted for in all analyses using the robust variance estimate of generalized estimating equations (Zeger et al., 1988). We determined a priori to include all eight child-level variables in the final models. To minimize potential collinearity problems associated with including all 11 county-level variables, we reduced the number of county-level variables in the final model using a two-step statistical and conceptual modeling approach: (1) assess results from the linear regression analyses and eliminate any variables from the socioeconomic environment domain with P > 0.05; and (2) include variables with the greatest relevance in developing place-based interventions and policies. Finally, we tested for within-level interactions between factors associated with chronic conditions (intellectual or developmental disability status and chronic condition severity) as well as cross-level interactions between the final county-level measures of socioeconomic environment (poverty and unemployment) and the following child-level variables: race/ethnicity, intellectual or developmental disability status, and chronic condition severity. All analyses were conducted using R for Windows v2.12.
3. Results
3.1. Descriptive statistics
The mean age of children in the study was 8.9 ± 3.4 years and about 60% of the population was male (data not shown). Over 70% of children were White, 9.1% were Black, and 13.2% had missing race/ethnicity data. About 10% of children had an intellectual or developmental disability and most children had an episodic chronic condition (69.6%). Over two–thirds of the children had a sibling who was enrolled in Medicaid and 56% had a Medicaid-enrolled caregiver. Finally, 88.8% of children used preventive medical care in 2005.
Across the 99 study counties in Iowa, the mean per capita income was $28,914 (2005 dollars). The mean population poverty rate was 10.8% and the mean child poverty rate was 14.4%. Unemployment ranged from 3% in Sioux County to 7.1% in Lee County. The proportion of persons under age 65 without health insurance was 11.5%. The proportion of children in each county in Medicaid ranged from 41% (Ringgold) to 62% (Buena Vista). Three out of four counties in Iowa were designated as dental Health Professional Shortage Areas.
3.2. County-level factors and dental care use
Of the seven county-level measures of the socioeconomic environment, five were significantly associated with child-level dental utilization (Table 1). Per capita income at the county-level was positively associated with child-level dental utilization (P < 0.01). Higher levels of population poverty, child poverty, unemployment, and percent of population on food assistance were all negatively associated with dental use at the child-level. Designation as a dental Health Professional Shortage Area was negatively associated and county-level per capita income was positively associated with child-level dental use (P=0.025 and P < 0.001, respectively).
Table 1.
Linear regression models to evaluate independent relationships between each county-level factor and child-level dental utilization.
| β coefficient* | Robust standard error | Robust z value | P-value | |
|---|---|---|---|---|
| Socioeconomic environment | ||||
| Per capita income, $ (2005) | 0.0053 | 0.0017 | 3.10 | 0.0019 |
| Percent population in poverty (2005) | −0.0108 | 0.0030 | −3.64 | 0.0003 |
| Percent children ages 0 to 17 years in poverty (2005) | −0.0101 | 0.0022 | −4.63 | <0.0001 |
| Unemployment rate for persons ages 16 and older (2005) | −0.0391 | 0.0136 | −2.87 | 0.0042 |
| Percent of persons under age 65 years without health insurance (2005) | 0.0084 | 0.0045 | 1.85 | 0.0643 |
| Percent of population on food assistance (2005) | −0.0139 | 0.0040 | −3.46 | 0.0005 |
| Percent of child population in Medicaid (2005) | −0.0031 | 0.0028 | −1.11 | 0.2684 |
| Health resource environment | ||||
| County designated as a dental Health Professional Shortage Area (2004) | 0.0252 | |||
| No | Reference | – | – | |
| Yes | −0.0486 | 0.0218 | −2.24 | |
| Per capita family medicine physicians and pediatricians (2005) | 0.0307 | 0.0290 | 1.06 | 0.2895 |
| Per capita emergency department visits (2005) | −0.0615 | 0.0811 | −0.76 | 0.4481 |
| Rurality (2003) | ||||
| Metropolitan | Reference | – | – | – |
| Urban adjacent to metropolitan | −0.0321 | 0.0226 | −1.42 | 0.1553 |
| Urban not adjacent to metropolitan | −0.0444 | 0.0336 | −1.32 | 0.1862 |
| Rural | −0.0223 | 0.0262 | −0.85 | 0.3937 |
Adjusted for child-level predictor variables (age, gender, race/ethnicity, IDD status, chronic condition severity, sibling enrolled in Medicaid, caregiver enrolled in Medicaid, used preventive medical care).
3.3. Final regression models
Of the four county-level variables included in the final multiple variable linear regression model, two were significantly associated with child-level dental care use (Table 2). Higher levels of county-level population poverty and designation as a dental Health Professional Shortage Area were negatively associated with child-level dental use (P < 0.0001 and P=0.028, respectively). While there were tendencies of lower dental use for children living in higher unemployment and non-metropolitan counties, both variables failed to reach statistical significance.
In the final models that included interaction terms, there was no evidence of a within-level interaction between IDD status and chronic condition severity (Table 3). Our models revealed cross-level interactions between race/ethnicity and percent population poverty as well as between IDD status and unemployment. With the model covariates fixed at the reference category (age category=3–5 years) or mean, the probability of dental use at the lowest levels of county-level poverty (5%) was highest for children in the other category (65%) and lowest for Black children (53%). At the highest levels of poverty (20%), the probability of dental utilization was highest for White children (46%) and lowest for other children (25%). For the interaction between IDD status and county-level unemployment, the probability lines intersect at about 6% unemployment. At unemployment rates below 6%, the probability of dental use is higher for children without an IDD than children with an IDD (56% and 44%, respectively). The reverse is true beyond 6% unemployment whereby the probability of dental use is higher for children with an IDD than for children without an IDD (52% and 46%, respectively).
Table 3.
Statistical significance of each interaction term in linear regression models of dental utilization for Medicaid-enrolled children with chronic conditions (N=25,908 children; n=99 counties).*
| Interaction term | β coefficient* | Robust standard error | Robust z value | P-value |
|---|---|---|---|---|
| Within-level interaction | ||||
| Intellectual or developmental disability (IDD) status × chronic condition severity | ||||
| IDD (yes) × episodic chronic condition | Reference | – | – | – |
| IDD (yes) × life-long chronic condition | 0.0015 | 0.0297 | 0.05 | 0.9600 |
| IDD (yes) × complex chronic condition | 0.0283 | 0.0684 | 0.41 | 0.6788 |
| Cross-level interactions | ||||
| Race/ethnicity × percent population in poverty | ||||
| White × percent poverty | Reference | – | – | – |
| Black × percent poverty | −0.0074 | 0.0036 | −2.06 | 0.0394 |
| Other × percent poverty | −0.0190 | 0.0078 | −2.44 | 0.0149 |
| Missing × percent poverty | −0.0015 | 0.0039 | −0.39 | 0.6969 |
| Race/ethnicity × unemployment | ||||
| White × unemployment | Reference | – | – | – |
| Black × unemployment | 0.0076 | 0.0216 | 0.35 | 0.7243 |
| Other × unemployment | −0.0254 | 0.0387 | −0.65 | 0.5127 |
| Missing × unemployment | 0.0114 | 0.0207 | 0.55 | 0.5815 |
| Intellectual or developmental disability status × percent population in poverty | 0.0044 | 0.0045 | 0.97 | 0.3322 |
| Intellectual or developmental disability status × unemployment | 0.0405 | 0.0186 | 2.18 | 0.0296 |
| Chronic condition severity × percent population in poverty | ||||
| Episodic chronic condition × poverty | Reference | – | – | – |
| Life-long chronic condition × poverty | 0.0013 | 0.0027 | 0.50 | 0.6205 |
| Complex chronic condition × poverty | 0.0098 | 0.0091 | 1.08 | 0.2817 |
| Chronic condition severity × unemployment | ||||
| Episodic chronic condition × unemployment | Reference | – | – | – |
| Life-long chronic condition × unemployment | 0.0024 | 0.0124 | 0.19 | 0.8456 |
| Complex chronic condition × unemployment | 0.0173 | 0.0362 | 0.48 | 0.6326 |
Adjusted for child-level predictors variables (age, gender, race/ethnicity, IDD status, chronic condition severity, sibling enrolled in Medicaid, caregiver enrolled in Medicaid, used preventive medical care) and county-level predictor variables (population poverty, unemployment, dental Health Professional Shortage Area designation, rurality).
Results from the linear and logistic regression models resulted in similar beta-coefficients and P-values (results presented online as Supplemental materials).
4. Discussion
This is the first study, to our knowledge, to specifically model the effects of county-level factors on dental utilization for Medicaid-enrolled children with chronic conditions. We tested three hypotheses. The first hypothesis was that county-level factors are important determinants of child-level dental care use. Our findings suggest that two of the four county-level factors from the final regression models were significantly associated with dental utilization (Table 2). Specifically, higher levels of poverty (a measure of the socioeconomic environment) and designation as a dental HPSA (a measure of health resource environment) were both significantly related to lower probabilities of dental care use. Previous studies have also found that variations in area-level social factors predict demand for health care services (Wennberg, 2002; Joines et al., 2003). There are two explanations for our findings. First, dentists may be less willing to practice in these areas because of economic and cultural reasons (Rosenblatt et al., 2006). Second, even though child Medicaid dental benefits are provided at no-cost, caregivers living in areas of socioeconomic deprivation may have other priorities that take precedence over dental care for their children (Maserejian et al., 2008). This suggests that behaviorally-mediated barriers to dental care such as low response efficacy (e.g., dental care is not effective at preventing dental disease in my child) or low self-efficacy (e.g., it is difficult for me to find dental care for my child) may aggregate in disadvantaged counties. Based on our findings, we confirm our first hypothesis.
The second hypothesis was that there would be important within-level interactions. Based on our final models (Table 3), we found no evidence of a significant within-level interaction between intellectual or developmental disability (IDD) status and chronic condition severity. This suggests that the deficit in dental care use associated with IDD is not different for children with severe chronic conditions than for children with less severe conditions. Based on our findings, we reject our second hypothesis.
The third hypothesis was that there were would be important cross-level interactions. There were two significant cross-level interactions. The interaction between child-level race/ethnicity and county-level poverty suggests that in poorer areas, poverty adversely affects dental use for non-White children with chronic conditions at greater rates than for White children with chronic conditions. This is consistent with previous findings on the negative health effects of cumulative social disadvantage in children (Bauman et al., 2006; Larson et al., 2008). In addition, there was a cross-level interaction between IDD status and unemployment where dental use was higher for children without IDD in counties with lower unemployment rates but higher for children with IDD in counties with higher unemployment rates. In another study, a similar cross-level interaction was detected between ward-level inactivity and adult-level disability in the United Kingdom (Fone et al., 2007). Based on these findings, we partially validate our third hypothesis.
Collectively, our findings form the basis for a new descriptive model of dental use for Medicaid-enrolled children with chronic conditions (Fig. 1). This model includes child-level factors, county-level factors (e.g., percent population poverty, unemployment, dental Health Professional Shortage Area designation), and cross-level interaction terms and has four methodological strengths. The first strength is that covariates are modeled on two levels (child- and county-level), which is an explicit recognition of the multilevel determinants of dental care use. However, we also recognize that there are levels that exist between the child- and county-levels (e.g., family-, neighborhood-) as well as multiple place-relevant levels beyond the county-level (e.g., state-, region-, country-) (Kendrick et al., 2005; Fisher-Owens et al., 2007). The second strength is that we include child-level measures of overall health and cognitive status. Models and analyses that fail to include measures of comorbidities and other features of chronic conditions (e.g., physical impairment, medication use, social and emotional health) may lead to confounded analyses (Manski, 1995). Our model is not likely to be confounded because of a missing comorbidity measure. The third strength is that our county-level factors measure different aspects of the social environment in which Medicaid-enrolled children with chronic conditions live. For instance, under the socioeconomic environment domain, we included measures that capture different aspects of social disadvantage and financial hardship. The fourth strength is that we include both within- and cross-level interaction terms. This is a strength because interaction terms are commonly excluded from children’s oral health models (e.g., Bramlett et al., 2010), which could lead to model misspecification.
Fig. 1.
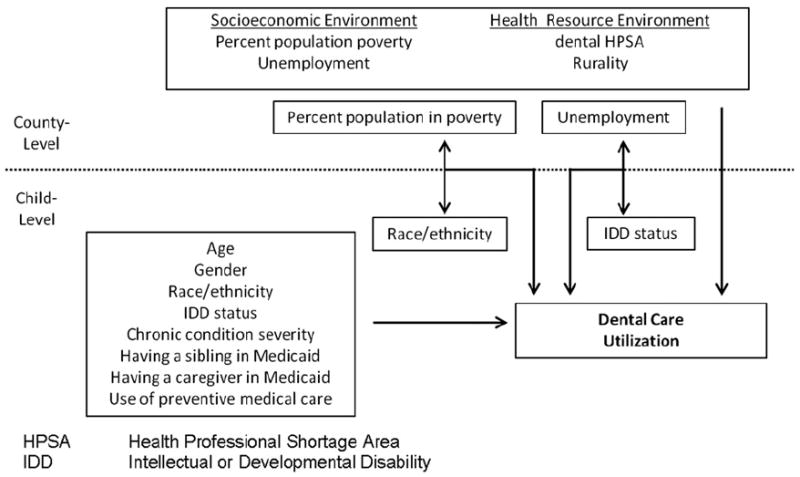
Description of study findings regarding dental care utilization for Medicaid-enrolled children with chronic conditions with child-level factors and county-level factors.
There are three main limitations with the current study. First, our findings are generalizable to Medicaid-enrolled children with chronic conditions in Iowa. Studies based on multiple state or national data might be conducted in the future to identify important trends that could help to shape national Medicaid policies. Second, our analyses were cross-sectional. However, all the child- and county-level variables were measured before 2006, the year in which dental utilization was measured, which eliminates problems associated with temporality. Future studies might adopt longitudinal statistical models to identify how changes in area-level factors over time are related to dental use. Third, our model focuses on secondary data, which do not include behavioral measures as potential determinants, mediators, and moderators of dental care use. For instance, factors such as caregiver-level self-efficacy and social support might serve as behavioral mediators through which place affects child-level dental care use. Subsequent studies could collect behavior data from caregivers, link these data with existing sources, and introduce more complex models of dental care use. Data from such studies could then be used to develop comprehensive, appropriately-targeted interventions and policies aimed at improving dental care use for Medicaid-enrolled children with chronic conditions.
Supplementary Material
Acknowledgments
Dr. Chi’s work was supported by the National Institute of Dental and Craniofacial Research (NIDCR) Grant K08DE020856 and the National Institute on Minority Health and Health Disparities (NIMHHD) Grant L60D003921. We would like to thank the Iowa Department of Human Services for granting access to Medicaid data and the 3M Corporation for a no-cost research license for the CRG Software.
Footnotes
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.healthplace.2012.07.007.
Parts of the manuscript were presented at the 139th American Public Health Association (APHA) Annual Meeting and Exposition in Washington, DC (October 2011).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- American Academy of Pediatric Dentistry. Clinical guidelines on periodicity of examination, preventive dental services, anticipatory guidance, and oral treatment for infants, children, and adolescents. Pediatric Dentistry. 2011;33:102–109. [Google Scholar]
- Antunes JL, Junqueira SR, Frazão P, Bispo CM, Pegoretti T, Narvai PC. City-level gender differentials in the prevalence of dental caries and restorative dental treatment. Health & Place. 2003;9:231–239. doi: 10.1016/s1353-8292(02)00055-2. [DOI] [PubMed] [Google Scholar]
- Bauman LJ, Silver EJ, Stein RE. Cumulative social disadvantage and child health. Pediatrics. 2006;117:1321–1328. doi: 10.1542/peds.2005-1647. [DOI] [PubMed] [Google Scholar]
- Berkowitz RJ. Mutans streptococci: acquisition and transmission. Pediatric Dentistry. 2006;28:106–109. [PubMed] [Google Scholar]
- Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state, and local disparities in childhood obesity. Health Affairs (Millwood) 2010;29:347–356. doi: 10.1377/hlthaff.2009.0762. [DOI] [PubMed] [Google Scholar]
- Blackwelder A, Shulman JD. Texas dentists’ attitudes toward the Dental Medicaid program. Pediatric Dentistry. 2007;29:40–46. [PubMed] [Google Scholar]
- Bloom B, Dey AN, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2005. Vital Health Statistics. 2006;10:1–84. [PubMed] [Google Scholar]
- Bramlett MD, Soobader M, Fisher-Owens SA, Weintraub JA, Platt LJ, Gansky SA, Newacheck PW. Assessing a multilevel model of young children’s oral health with national survey data. Community Dentistry and Oral Epidemiology. 2010;38:287–298. doi: 10.1111/j.1600-0528.2010.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brickhouse TH, Farrington FH, Best AM, Ellsworth CW. Barriers to dental care for children in Virginia with autism spectrum disorders. Journal of Dentistry for Children (Chic) 2009;76:188–193. [PubMed] [Google Scholar]
- Casamassimo PS, Seale NS, Ruehs K. General dentists’ perceptions of educational and treatment issues affecting access to care for children with special health care needs. Journal of Dental Education. 2004;68:23–28. [PubMed] [Google Scholar]
- Caudill SB. An advantage of the linear probability model over probit or logit. Oxford Bulletin of Economics & Statistics. 1988;50:425–427. [Google Scholar]
- Centers for Disease Control and Prevention. Obesity Prevalence among Low-Income, Preschool-Aged Children—United States, 1998–2008. Morbidity and Mortality Weekly Report. 2009;58:769–73. [PubMed] [Google Scholar]
- Chi DL, Momany ET, Kuthy RA, Chalmers JM, Damiano PC. Preventive dental utilization for Medicaid-enrolled children in Iowa identified with intellectual and/or developmental disability. Journal of Public Health Dentistry. 2010;70:35–44. doi: 10.1111/j.1752-7325.2009.00141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi DL, Momany ET, Neff J, Jones MP, Warren JJ, Slayton RL, Weber-Gasparoni K, Damiano PC. Impact of chronic condition status and severity on dental utilization for Iowa Medicaid-enrolled children. Medical Care. 2011;49:180–192. doi: 10.1097/MLR.0b013e3181f81c16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Close K, Rozier RG, Zeldin LP, Gilbert AR. Barriers to the adoption and implementation of preventive dental services in primary medical care. Pediatrics. 2010;125:509–517. doi: 10.1542/peds.2009-1008. [DOI] [PubMed] [Google Scholar]
- Commission on Social Determinants of Health. Final Report of the Commission on Social Determinants of Health. World Health Organization; Geneva: 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. [Google Scholar]
- Dubay L, Kenney GM. Health care access and use among low-income children: who fares best? Health Affairs (Millwood) 2001;20:112–121. doi: 10.1377/hlthaff.20.1.112. [DOI] [PubMed] [Google Scholar]
- Eklund SA, Pittman JL, Clark SJ. Michigan Medicaid’s Healthy Kids Dental program: an assessment of the first 12 months. Journal of the American Dental Association. 2003;134:1509–1515. doi: 10.14219/jada.archive.2003.0083. [DOI] [PubMed] [Google Scholar]
- Fisher MA, Mascarenhas AK. Does Medicaid improve utilization of medical and dental services and health outcomes for Medicaid-eligible children in the United States? Community Dentistry and Oral Epidemiology. 2007;35:263–271. doi: 10.1111/j.1600-0528.2007.00341.x. [DOI] [PubMed] [Google Scholar]
- Fisher MA, Taylor GW. A prediction model for chronic kidney disease includes periodontal disease. Journal of Periodontology. 2009;80(1):16–23. doi: 10.1902/jop.2009.080226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader M, Bramlett MD, Newacheck PW. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120:e510–e520. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- Fone D, Dunstan F, Williams G, Lloyd K, Palmer S. Places, people and mental health: a multilevel analysis of economic inactivity. Social Science & Medicine. 2007;64:633–645. doi: 10.1016/j.socscimed.2006.09.020. [DOI] [PubMed] [Google Scholar]
- Franco E, Saunders CP, Roberts GJ, Suwanprasit A. Dental disease, caries related microflora and salivary IgA of children with severe congenital cardiac disease: an epidemiological and oral microbial survey. Pediatric Dentistry. 1996;18:228–235. [PubMed] [Google Scholar]
- Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. American Journal of Public Health. 1992;82:1663–1668. doi: 10.2105/ajph.82.12.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grembowski D, Milgrom PM. Increasing access to dental care for medicaid preschool children: the Access to Baby and Child Dentistry (ABCD) program. Public Health Reports. 2000;115:448–459. doi: 10.1093/phr/115.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grow HM, Cook AJ, Arterburn DE, Saelens BE, Drewnowski A, Lozano P. Child obesity associated with social disadvantage of children’s neighborhoods. Social Science & Medicine. 2010;71:584–591. doi: 10.1016/j.socscimed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Wieringa NF, Keyes KM. Community-level determinants of tobacco use disparities in lesbian, gay, and bisexual youth: results from a population-based study. Archives of Pediatric and Adolescent Medicine. 2011;165:527–532. doi: 10.1001/archpediatrics.2011.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi C, Madrigal AG, Liu X, Ukai T, Goswami S, Gudino CV, Gibson FC, 3rd, Genco CA. Pathogen-mediated inflammatory atherosclerosis is mediated in part via Toll-like receptor 2-induced inflammatory responses. Journal of Innate Immunology. 2010;2:334–343. doi: 10.1159/000314686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthcare Effectiveness Data and Information Set 2012. Technical Specifications. Vol. 2. National Committee for Quality Assurance; Washington, DC: 2012. [Google Scholar]
- Hughes JS, Averill RF, Eisenhandler J, Goldfield NI, Muldoon J, Neff JM, Gay JC. Clinical Risk Groups (CRGs): a classification system for risk-adjusted capitation-based payment and health care management. Medical Care. 2004;42:81–90. doi: 10.1097/01.mlr.0000102367.93252.70. [DOI] [PubMed] [Google Scholar]
- Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. American Journal of Public Health. 2011;101:1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joines JD, Hertz-Picciotto I, Carey TS, Gesler W, Suchindran C. A spatial analysis of county-level variation in hospitalization rates for low back problems in North Carolina. Social Science & Medicine. 2003;56:2541–2553. doi: 10.1016/s0277-9536(02)00295-2. [DOI] [PubMed] [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. [January 13, 2012];Aging Out of EPSDT, 2007 Issues for Young Adults with Disabilities. Issue Paper 7491, Available at < http://www.kff.org/medicaid/upload/7491.pdf>.
- Kakaiya RM, Triulzi DJ, Wright DJ, Steele WR, Kleinman SH, Busch MP, Norris PJ, Hillyer CD, Gottschall JL, Rios JA, Carey P, Glynn SA. For the National Heart, Lung, and Blood Institute (NHLBI) retrovirus epidemiology donor study-II 2010 prevalence of HLS antibodies in remotely transfused or alloexposed volunteer blood donors. Transfusion. 50:1328–1334. doi: 10.1111/j.1537-2995.2009.02556.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanellis MJ, Damiano PC, Momany ET. Utilization of dental services by Iowa Medicaid-enrolled children younger than 6 years old. Pediatric Dentistry. 1997;19:310–314. [PubMed] [Google Scholar]
- Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children’s oral health among low-income caregivers. American Journal of Public Health. 2005;95(8):1345–1351. doi: 10.2105/AJPH.2004.045286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick D, Mulvaney C, Burton P, Watson M. Relationships between child, family and neighbourhood characteristics and childhood injury: a cohort study. Social Science & Medicine. 2005;61:1905–1915. doi: 10.1016/j.socscimed.2005.04.003. [DOI] [PubMed] [Google Scholar]
- Kenney GM, Marton J, Klein AE, Pelletier JE, Talbert J. The effects of Medicaid and CHIP policy changes on receipt of preventive care among children. Health Services Research. 2011;46:298–318. doi: 10.1111/j.1475-6773.2010.01199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer MR, Hogue CR. Place matters: variation in the black/white very preterm birth rate across U.S. metropolitan areas, 2002–2004. Public Health Reports. 2008;123:576–585. doi: 10.1177/003335490812300507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalla E, Cheng B, Lal S, Tuker S, Greenberg E, Goland R, Lamster IB. Periodontal changes in children and adolescents with diabetes: a case-control study. Diabetes Care. 2006;29:295–309. doi: 10.2337/diacare.29.02.06.dc05-1355. [DOI] [PubMed] [Google Scholar]
- Lam M, Riedy CA, Milgrom P. Improving access for Medicaid-insured children: focus on front-office personnel. Journal of the American Dental Association. 1999;130:365–373. doi: 10.14219/jada.archive.1999.0206. [DOI] [PubMed] [Google Scholar]
- Larson K, Russ SA, Crall JJ, Halfon N. Influence of multiple social risks on children’s health. Pediatrics. 2008;121(2):337–344. doi: 10.1542/peds.2007-0447. [DOI] [PubMed] [Google Scholar]
- Lewis C, Robertson AS, Phelps S. Unmet dental care needs among children with special health care needs: implications for the medical home. Pediatrics. 2005;116:e426–e431. doi: 10.1542/peds.2005-0390. [DOI] [PubMed] [Google Scholar]
- Lewis C, Stout J. Toothache in US children. Archives of Pediatric and Adolescent Medicine. 2010;164:1059–1063. doi: 10.1001/archpediatrics.2010.206. [DOI] [PubMed] [Google Scholar]
- Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, Guyatt G. Family impact of child oral and oro-facial conditions. Community Dentistry and Oral Epidemiology. 2002;30:438–448. doi: 10.1034/j.1600-0528.2002.00015.x. [DOI] [PubMed] [Google Scholar]
- Locker D, Jokovic A, Tompson B. Health-related quality of life of children aged 11 to 14 years with orofacial conditions. The Cleft Palate-Craniofacial Journal. 2005;42:260–266. doi: 10.1597/03-077.1. [DOI] [PubMed] [Google Scholar]
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annual Review of Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- Manski RJ. Variable confounding and the influence of non economic determinants on dental utilization for the elderly. Maryland State Dental Association Journal. 1995;38:171–174. [PubMed] [Google Scholar]
- Maserejian NN, Trachtenberg F, Link C, Tavares M. Underutilization of dental care when it is freely available: a prospective study of the New England children’s amalgam trial. Journal of Public Health Dentistry. 2008;68:139–148. doi: 10.1111/j.1752-7325.2007.00074.x. [DOI] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Education Quarterly. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- Mendes AP, Zhang L, Prietsch SO, Franco OS, Gonzáles KP, Fabris AG, Catharino A. Factors associated with asthma severity in children: a case-control study. Journal of Asthma. 2011;48:235–240. doi: 10.3109/02770903.2011.555039. [DOI] [PubMed] [Google Scholar]
- Merrill CT, Nagamine M, Hambrick MM. HCUP Statistical Brief 37. Agency for Healthcare Research and Quality; Rockville, MD: 2007. [January 10, 2012]. Pediatric Hospital Stays for Cancer, 2005. Available at < http://www.hcup-us.ahrq.gov/reports/statbriefs/sb37.pdf>. [PubMed] [Google Scholar]
- Muldoon J, Neff J, Gay J. Profiling the health service needs of populations using diagnosis-based classification systems. Journal of Ambulatory Care Management. 1997;20:1–18. doi: 10.1097/00004479-199707000-00002. [DOI] [PubMed] [Google Scholar]
- Nakano K, Nemoto H, Nomura R, Homma H, Yoshioka H, Shudo Y, Hata H, Toda K, Taniguchi K, Amano A, Ooshima T. Serotype distribution of Streptococcus mutans a pathogen of dental caries in cardiovascular specimens from Japanese patients. Journal of Medical Microbiology. 2007;56:551–556. doi: 10.1099/jmm.0.47051-0. [DOI] [PubMed] [Google Scholar]
- Neff JM, Clifton H, Park KJ, Goldenberg C, Popalisky J, Stout JW, Danielson BS. Identifying children with lifelong chronic conditions for care coordination by using hospital discharge data. Academic Pediatrics. 2010;10:417–423. doi: 10.1016/j.acap.2010.08.009. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, McManus M, Fox HB, Hung YY, Halfon N. Access to health care for children with special health care needs. Pediatrics. 2000;105:760–766. doi: 10.1542/peds.105.4.760. [DOI] [PubMed] [Google Scholar]
- Ngo FT, Paternoster R, Cullen FT, Mackenzie DL. Life domains and crime: a tests of Agnew’s general theory of crime and delinquency. Journal of Criminal Justice. 2006;39:302–311. [Google Scholar]
- Nuttall NM, Steele JG, Evans D, Chadwick B, Morris AJ, Hill K. The reported impact of oral condition on children in the United Kingdom, 2003. British Dental Journal. 2006;200:551–555. doi: 10.1038/sj.bdj.4813586. [DOI] [PubMed] [Google Scholar]
- Patel RR, Tootla R, Inglehart MR. Does oral health affect self perceptions, parental ratings and video-based assessments of children’s smiles? Community Dentistry and Oral Epidemiology. 2007;35:44–52. doi: 10.1111/j.1600-0528.2007.00327.x. [DOI] [PubMed] [Google Scholar]
- Pinto-Martin JA, Dunkle M, Earls M, Fliedner D, Landes C. Developmental stages of developmental screening: steps to implementation of a successful program. American Journal of Public Health. 2005;95:1928–1932. doi: 10.2105/AJPH.2004.052167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plutzer K, Spencer AJ. Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dentistry and Oral Epidemiology. 2008;36:335–346. doi: 10.1111/j.1600-0528.2007.00414.x. [DOI] [PubMed] [Google Scholar]
- Rosenblatt RA, Andrilla CH, Curtin T, Hart LG. Shortages of medical personnel at community health centers: implications for planned expansion. Journal of the American Medical Association. 2006;295:1042–1049. doi: 10.1001/jama.295.9.1042. [DOI] [PubMed] [Google Scholar]
- Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007;369:51–59. doi: 10.1016/S0140-6736(07)60031-2. [DOI] [PubMed] [Google Scholar]
- Teles R, Wang CY. Mechanisms involved in the association between periodontal diseases and cardiovascular disease. Oral Diseases. 2011;17:450–461. doi: 10.1111/j.1601-0825.2010.01784.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinanoff N, Kanellis MJ, Vargas CM. Current understanding of the epidemiology mechanisms, and prevention of dental caries in preschool children. Pediatric Dentistry. 2002;24:543–551. [PubMed] [Google Scholar]
- Tsai AC, Votruba M, Bridges JFP, Cebul RD. Overcoming bias in estimating the volume-outcome relationship. Health Services Research. 2006;41:252–264. doi: 10.1111/j.1475-6773.2005.00461.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan MD, Rowland CC, Tong X, Srivastava DK, Hale GA, Rochester R, Kaste SC. Dental abnormalities in children preparing for pediatric bone marrow transplantation. Bone Marrow Transplantation. 2005;36:863–866. doi: 10.1038/sj.bmt.1705111. [DOI] [PubMed] [Google Scholar]
- [January 9];Washington State Health Care Authority Website. 2012 Available at: < http://hrsa.dshs.wa.gov/DentalProviders/dental_data.htm>.
- White K, Haas JS, Williams DR. Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Services Research. 2012;47:1278–1299. doi: 10.1111/j.1475-6773.2012.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widener MJ, Metcalf SS, Northridge ME, Chakraborty B, Marshall SM, Lamster IB. Exploring the role of peer density in the self-reported oral health outcomes of older adults: a kernel density based approach. Health & Place. 2012;18:782–788. doi: 10.1016/j.healthplace.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. [December 28];Social Determinants of Health Website. 2011 Available at: < http://www.who.int/social_determinants/en/>.
- Ylöstalo PV, Järvelin MR, Laitinen J, Knuuttila ML. Gingivitis, dental caries and tooth loss: risk factors for cardiovascular diseases or indicators of elevated health risks. Journal of Clinical Periodontology. 2006;33:92–101. doi: 10.1111/j.1600-051X.2005.00875.x. [DOI] [PubMed] [Google Scholar]
- Zeger S, Liang K-Y, Albert P. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- Zeng X, Sheiham A, Tsakos G. Relationship between clinical dental status and eating difficulty in an old Chinese population. Journal of Oral Rehabilitation. 2008;35:37–44. doi: 10.1111/j.1365-2842.2007.01811.x. [DOI] [PubMed] [Google Scholar]
- Zoellner H. Dental infection and vascular disease. Seminars on Thrombosis and Hemostasis. 2011;37:181–192. doi: 10.1055/s-0031-1273082. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


