Abstract
Dementia and hip fractures are 2 conditions that are seen primarily in older adults, and both are associated with substantial morbidity and mortality. An individual with dementia is up to 3 times more likely than a cognitively intact older adult to sustain a hip fracture. This may occur via several mechanisms, including (1) risk factors that are common to both outcomes; (2) the presence of dementia increasing hip fracture incidence via intermediate risk factors, such as falls, osteoporosis, and vitamin D; and (3) treatment of dementia causing side effects that increase hip fracture risk. We describe a model that applies these 3 mechanisms to explain the relationship between dementia and hip fractures. Comprehensive understanding of these pathways and their relative influence on the outcome of hip fracture will guide the development of effective interventions and potentially improve prevention efforts.
Keywords: multimorbidity, pathogenesis, cognitive impairment, Alzheimer disease, fragility fractures
Introduction
Dementia and hip fractures are 2 conditions that are seen predominantly in older adults, and particularly in the oldest old. Both are associated with a high level of morbidity and mortality, as well as financial and human cost, to the health care system, to patients, and to caregivers. As the “gerontic boom” continues, with the population over the age of 85 years continuing to be the fastest growing segment of the United States, it is increasingly important to understand these two conditions, their risk factors, and how they impact each other. Insight into the relationship between dementia and hip fractures will enable improved efforts to prevent the adverse outcomes associated with these 2 conditions.
Dementia prevalence increases exponentially with age, from 3.0% among those aged 65 to 74 years to 18.7% among 75 to 84 year olds and 47.2% in individuals over the age of 85 years.1 It is estimated that the prevalence of dementia worldwide will double every 20 years, reaching over 81 million by 2040, likely as a result of the growing older adult population.2 Dementia is a progressive disorder of cognition that by definition interferes with usual activities of daily life and social interaction.3 Individuals with moderate-to-severe cognitive impairment have a relative risk of death of 2.3 compared with their cognitively intact counterparts.4
Eighty-six percent of hip fractures occur in individuals over the age of 65 years.5 At age 50 years, the lifetime risk of sustaining a hip fracture is 15.6% and 5.6% for white and black women, respectively, and 5.2% and 2.8% for white and black men, respectively.6 Although there is some evidence that age-adjusted incidence of hip fractures may be declining,7,8 the rapid increase in the elderly population makes it possible that the total number of hip fractures worldwide may increase from 1.7 million in 1990 to 6.3 million by 2050.9 A year following a hip fracture, approximately one fourth of individuals who were living in the community prior to the fracture require long-term nursing home care,10 and only one half of hip fracture patients regain their prefracture mobility.11 Mortality following a hip fracture is 5-fold to 8-fold higher than in age- and sex-matched controls in the 3 months following the fracture, but excess mortality persists even after 10 years.12 Twenty percent of patients die in the year following a hip fracture.13
Multimorbidity, or the development of multiple concomitant chronic illnesses, increases with age. Fifty-four percent of individuals aged 65 to 69 years have 2 or more chronic conditions, whereas 73% aged 85 years and more have multiple chronic conditions.14 A chronic condition may be seen more commonly in the presence of another condition for several reasons, including (1) common causal pathways for 2 conditions leading to increased frequency of co-occurrence (ie, shared risk factors); (2) one condition increasing the risk of another, often via intermediate risk factors; and (3) treatment for one condition worsening another.15 This paper will address these 3 pathways as they pertain to dementia and hip fractures.
Individuals who suffer from dementia or cognitive impairment are at substantially higher risk of sustaining a hip fracture than those who are cognitively intact.16–23 In the 10 years following a diagnosis of Alzheimer disease, the risk is 2.7-fold higher than in age- and sex-matched controls.24 Hip fractures occur as a result of an interaction between cognitive, environmental, physical, behavioral, and socioeconomic factors.9 As outlined in the accompanying paper by Menzies et al, much of this increased risk may be due to missed practice opportunities. As we will address further, there are several pathogenic changes that are seen in patients with dementia that may in turn put them at higher risk for hip fracture. On the basis of a thorough literature review and consultation with experts in both fields, we propose a model to explain the relationship between dementia and hip fractures.
Dementia as a Spectrum
Dementia is a progressive syndrome, with a median life expectancy of 4.5 years following diagnosis.25 Dementia most commonly results from Alzheimer disease (60%-89%), vascular disease (15%-37%), Lewy body dementia (5%-24%), and Parkinson disease (3%-4%).26–29 Clinical presentations differ based on etiology. For example, Lewy body dementia is characterized by parkinsonism, fluctuations in cognition, visual hallucinations, disturbances in consciousness, sensitivity to neuroleptic medications, and frequent falls.27 Many of these features may increase hip fracture risk. It is likely that hip fracture incidence differs based on etiology of dementia. For example, in a study of 192 African Americans with dementia, 8.1% of those with Alzheimer disease had a history of hip fracture versus 1.3% of those with vascular dementia.30 This paper will review literature addressing cognitive impairment, dementia, and specific etiologies of dementia. Where etiologies are identified (eg, Alzheimer disease), we specify the cause of dementia.
The risk of hip fracture remains fairly constant in mild, moderate, and severe Alzheimer disease. In Melton’s study evaluating hip fracture risk over the 10 years following diagnosis of Alzheimer disease, the slope of the incidence did not change substantially over time.24 A longitudinal study by Guo supports this finding, showing that patients with Mini-Mental State Exam31 (MMSE) scores of 18 to 23 (mild impairment) had a relative risk of hip fracture of 2.04, versus 2.09 for patients with an MMSE score <18 (moderate–severe impairment).32 However, it is likely that the mechanism of hip fractures change over time. For example, immobility increases as Alzheimer disease progresses. In a study by Buchner and Larson evaluating falls and fractures in predominantly community-dwelling older adults with Alzheimer disease, one third of those who were ambulatory at baseline were nonambulatory after a follow-up of 3 years.33 However, in this study as well, dementia severity was not significantly predictive of fractures.
Shared Risk Factors for Dementia and Hip Fractures
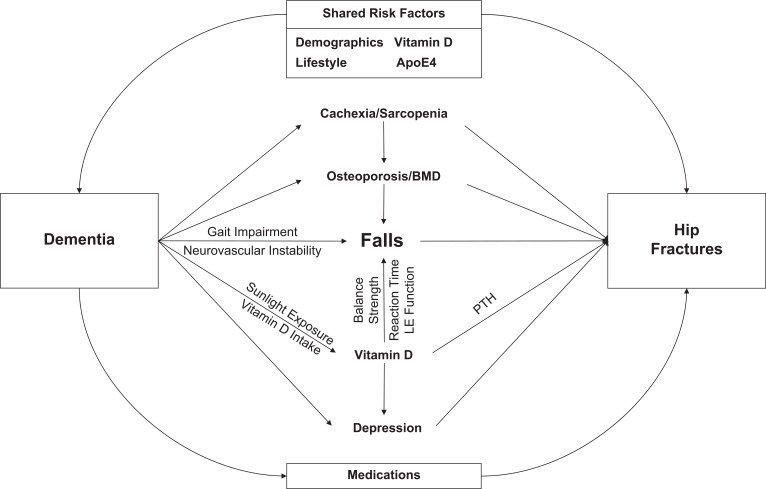
Figure 1 presents a theoretical framework of the relationship of dementia and hip fracture. It demonstrates 3 pathways, including characteristics that increase the risk of both outcomes (Table 1), multiple interacting intermediate mechanisms that increase fracture risk (Table 2), and the increase in risk of hip fracture due to dementia treatment. Several risk factors are common to both outcomes.
Figure 1.
Pathogenic framework for dementia and hip fractures. Several intermediate risk factors are interrelated, and this is described in the text. These connections are not depicted in the Figure for ease of reading. This framework depicts 3 mechanisms by which dementia increases hip fracture risk: (1) shared risk factors increase co-occurrence; (2) dementia increases the risk of multiple intermediate risk factors, which in turn, increase hip fracture risk; (3) treatment of dementia increases hip fracture risk.
Table 1.
Shared Risk Factors for Dementia and Hip Fracture
| Age |
|---|
| Decreased activity |
| Smoking |
| Alcohol |
| Vitamin D deficiency |
| Apolipoprotein E4 |
Table 2.
Intermediate Risk Factors for Dementia and Hip Fracture
| Gait |
|---|
| Neurovascular instability |
| Falls |
| Vitamin D |
| Osteoporosis/bone mineral density |
| Cachexia/sarcopenia |
| Depression |
| bone mineral density |
Demographics
Age is a shared risk factor for both dementia34 and hip fractures.35 As discussed above, both dementia and hip fractures are more prevalent with advancing age, particularly in the “old old,” or those over the age of 75 years. Women, who have a longer life expectancy than men, have a higher prevalence of vitamin D deficiency,36 osteoporosis,20 Alzheimer disease,20 and hip fractures.6,17,37
Vitamin D
The role of vitamin D as an intermediate risk factor between dementia and hip fractures is described below. Recent data also shows an association of vitamin D with cognitive decline and dementia.28 Vitamin D receptors have been localized in the brain38 and may provide neuroprotection as a result of detoxification and neurotrophin synthesis, a process necessary for neuronal survival. Messenger RNA levels for vitamin D receptors are reduced in the hippocampus of patients with Alzheimer disease but not in the temporal cortex or cerebellum.39 Cross sectionally, serum 25(OH)D concentrations have been positively correlated with MMSE scores31,40 and with Sum of Boxes and Short Blessed tests of cognition.41,42 The direction of association has yet to be fully established, but the biological plausibility of a role for vitamin D in cognition is well supported.
Lifestyle
Recreational exercise is protective against hip fracture, with a relative risk of 1.9 for those who report little or no exercise versus those who report much or moderate exercise.35 In patients with dementia, there is evidence that physical activity reduces the risk of falls.43 However, wandering has been shown to substantially increase risk of hip fractures in patients with Alzheimer disease, with an odds ratio (OR) of 6.9.33 There is growing evidence that physical activity may have a protective effect on cognition.44–46
Smoking is a risk factor for both cognitive decline and dementia, with a relative risk of 1.79 for Alzheimer disease and 1.78 for vascular dementia.47 Some elements of cognition may be particularly impacted by tobacco use. In one study of healthy older adults, heavy smoking was associated with worse executive function and problem solving, but there were no differences in visual-spatial capabilities, attention, or memory.48 Smoking is associated cross-sectionally with decreased appendicular bone mass in older women.49 It has been shown to increase the risk of hip fracture in both women and men, with 19% of the risk of hip fracture attributable to smoking.50 As a result, the FRAX tool incorporates smoking as a predictor of osteoporotic fracture, including hip fracture.51 The FRAX tool is a Web-based algorithm, available online, that was developed by the World Health Organization to assess 10-year risk of hip fracture as well as any major osteoporotic fracture.
The impact of alcohol on risk of dementia appears to depend on level of intake, with low intake being somewhat protective and large doses increasing risk.52 Studies evaluating the relationship between alcohol and hip fractures have been inconsistent, with several showing an increased risk with higher intake and others showing no relationship.37 Individuals with alcoholism often have low bone mass, which may be nutritionally mediated. The FRAX tool for assessment of fracture risk incorporates a value of 3 or more units of alcohol per day to determine risk.51
Apolipoprotein E4
Presence of the apolipoprotein E4 (apoE4) gene increases risk for both Alzheimer disease and hip fracture. The risk ratio for developing Alzheimer disease is 30.1 and 3.7 for E4/E4 homozygotes and E4/E3 heterozygotes versus E3/E3 homozygotes, respectively.53 In a community-based case-control study, participants with 1 or 2 E4 alleles had an age-adjusted OR of 2.1 for reporting a hip fracture.54 This relationship persisted after adjusting for dementia and history of falls. However, this study included only 25 patients with hip fracture and did not reach statistical significance. A study of patients with hemodialysis showed that 44% of those with E3/4 and E4/4 genotypes had a history of fractures versus 16% of those with E2/3 or E2/2 genotypes (P < .005).55 It is theorized that the increased risk of hip fracture may be mediated through vitamin K metabolism. Individuals with the apoE4 allele clear vitamin K more quickly than those with other variants.56 Patients with hip fracture have been demonstrated to have lower levels of vitamin K,57 and supplementation increases osteocalcin and bone alkaline phosphatase, which are markers of bone formation.58 The population prevalence of the apoE4 allele is 11.8%.53
Intermediate Risk Factors for Dementia and Hip Fracture
Gait
Studies of patients with moderate Alzheimer disease have demonstrated shorter stride length, lower gait speed, lower stepping frequency, greater step-to-step variability, greater double support ratio (ie, more time spent in stance phase), and greater sway path than those without Alzheimer disease.59,60 Participants with vascular dementia have slower velocity and shorter stride length than those with Alzheimer disease.60 Stride length and walking speed have been shown to be related to falls risk.61 In a study of community-dwelling Alzheimer patients, poor tandem gait was a predictor of both falls and fractures 3 years later.33 In a study of nursing home residents with moderate-stage Alzheimer disease, stride length variability predicted falls.62
In addition to changes in the specific components of gait, a high proportion of patients with Alzheimer disease have a gait apraxia. This has been defined as “the loss of ability to properly use the lower limbs in the act of walking,” not due to other causes, such as muscle wasting or orthopedic abnormalities. In one study that evaluated gait apraxia comprehensively, 40% of patients exhibited an apraxia.63 Impairment of central integration of information for maintaining balance and gait is a major underlying issue in patients with dementia.64
Impairments in gait may become more marked in stress situations for patients with dementia. Patients with Alzheimer disease have been noted to slow their gait while simultaneously performing a verbal fluency task, which may also contribute to falls.65
Neurovascular Instability
Patients with Alzheimer disease have a high prevalence of autonomic dysfunction,66 leading to an increased prevalence of orthostatic hypotension. The literature regarding orthostasis as a risk factor for falls is mixed,67 but it is plausible that this could increase falls risk. Patients with dementia have a higher prevalence of carotid sinus hypersensitivity, with a rate up to 50% in patients with Lewy body dementia versus 4% healthy older adults.64 A study of patients with Lewy body dementia and Alzheimer disease showed a prevalence of carotid sinus hypersensitivity of 41% and 28%, respectively.68 In a case-controlled study of hip fracture patients, 36% of patients admitted with a femoral neck fracture versus 13% admitted with acute medical illness had carotid sinus sensitivity.69
Falls
Most patients who sustain a hip fracture do so as the result of a fall.22 Patients with dementia have up to an 8-fold higher risk of falling,32,43,70–77 and a particularly high risk of sustaining multiple falls,78 compared with those without dementia. Annual incidence of falls ranges from 67% to 85% in prospectively collected data.64 They are also at higher risk of sustaining injurious falls.16,79–81 In one study in which participants were followed for 4 years, 36% of patients with Alzheimer disease versus 11% of controls experienced a serious fall that required immediate medical attention or resulted in death.16 However, a study of institutionalized older adults showed that the odds ratio for the relationship between Alzheimer disease and hip fractures remained relatively unchanged after adjusting for falls and osteoporosis, suggesting that there are other factors involved that increase fracture risk in patients with Alzheimer disease.20
The cause of dementia appears to be significantly related to falls risk. In one study, the incidence-density ratio, or the ratio of the number of falls per 1000 patient years for each group, adjusted for age and sex, was 20.5 for Parkinson disease, 6.1 for dementia with Lewy bodies, 2.0 for Alzheimer disease, and 1.8 for vascular dementia, respectively, when compared with cognitively intact participants.43 Another small study showed that patients with Lewy body dementia were twice as likely to sustain 2 or more falls as patients with Alzheimer disease over a 3-month period (57% versus 26%, respectively).27
It is unclear whether progression of dementia is associated with higher risk of falls. In a study of 97 nursing home residents with Alzheimer disease, those with a Clinical Dementia Rating score of 1 (mild) had a 20% incidence of falls, versus 38% among those with a score of 2 (moderate).62 A study of falls in community-dwelling older adults showed an OR of 1.7 per 10-point drop in MMSE score.82 Other studies have failed to show an association of falls with time or duration of dementia.16,43 It may be that mobility and dementia interact in nonlinear ways over time; a study of nursing home patients that used a scale incorporating physical and psychological impairment as well as dementia severity showed a parabolic association with falls rate.83 More study is needed to further understand this relationship.
Cognitive tests that have been shown to be predictive of falls include the Trail Making Test part B,80 MMSE score,73,80 Standardized Mini-Mental State Exam,74 short portable mental status questionnaire,70 verbal reasoning,73 and tests of immediate recall.84 Even mild decrements in cognition lead to increased risk of falls, with a relative risk of 1.2 for each point drop of MMSE score31 between 30 (maximum) and 22.85 In another analysis of individuals with MMSE scores of >24, MMSE score was inversely associated with fall risk.73
In Melton’s study of fracture incidence following a diagnosis of dementia, hip fractures were increased, but wrist and vertebral fractures were not, suggesting that the mechanics of the falls may be different in patients with and without dementia.24 A study of nursing home patients who fell showed that those who fell onto their hip or the side of the leg were almost 22 times more likely to fracture their hip than those whose point of impact was elsewhere, such as the buttock.22 Cognitively impaired residents who fell to the side were 7 times more likely to sustain a hip fracture than those who fell in different directions. Similarly, in a study of 100 nursing home residents who were fallers, falling to the side was associated with an OR of 5.7 for sustaining a hip fracture,86 and in a case-control study of men with hip fractures, falling on the hip or thigh led to a markedly elevated risk of hip fracture, with an OR of 98.87 It is not clear whether fall direction or point of impact differs by cognitive status.
There is a paucity of information on falls risk factors specific to patients with dementia. In a study evaluating risk of falls and fractures in patients with Alzheimer dementia (mean MMSE score 17.6 ± 7.5), rigidity, poor tandem gait, wandering, and agitation—all characteristics that could potentially increase falls risk—were associated with lower MMSE scores.33 In this population, risk factors for falls in the subsequent year were peripheral neuropathy, a musculoskeletal problem limiting function, cataract, and poor tandem gait. A recent prospective study found that type of dementia, history of previous falls, use of cardioactive medication, abnormal gait or balance, Cornell Scale for Depression in Dementia score ≥10, autonomic symptoms, autonomic neuropathy, and symptomatic orthostasis were associated with subsequent falls.43 Older age and physical activity were protective. Depression, autonomic symptoms, and orthostasis were independently predictive. In a population of patients with more advanced Alzheimer disease (mean MMSE 15), Unified Parkinson’s Disease Rating Scale and fewer steps per minute predicted falls.78 Extrapyramidal motor impairment is more common in advanced Alzheimer disease. Trajectory of decline appears to be important; in a study of institutionalized women with Alzheimer disease, those who were the most vigorous and had shown significant declines in the previous year were more likely to fall than those who had been the least vigorous but were stable.88
Vitamin D Deficiency
There is a high prevalence of vitamin D deficiency in patients with dementia, which has been seen in both community89 and nursing home90 populations. Vitamin D deficiency is particularly prominent in frail nursing home patients with Alzheimer disease, where in one study, 54% had serum levels at a severe deficiency level of <5 ng/mL.90 Even in individuals with better cognition, as assessed by an abbreviated mental test score of 7 or more, there is a correlation between vitamin D level and cognition.91
Vitamin D deficiency is a risk factor for falls,92 and the incidence of falls is particularly high in vitamin D-deficient patients with elevated parathyroid hormone (PTH) levels.19 The impact of vitamin D on falls may be mediated through its effect on muscle strength,36,93–96 balance,70,91,95,96 gait,97 lower extremity function,98–100 and reaction time,91 although studies of these pathways have been mixed.101
Vitamin D deficiency is a risk factor for hip fracture. Serum PTH is negatively correlated with vitamin D levels in Alzheimer disease patients with hip fractures, but not in Alzheimer disease patients without, suggesting that compensatory hyperparathyroidism increases risk further.19 Supplementation of vitamin D increases bone mineral density (BMD)97,102 and reduces falls,103,104 which in turn reduces hip fracture risk.102
There are several causes of vitamin D deficiency in older adults with dementia. Alzheimer disease patients with hip fractures have lower dietary intake of calcium and vitamin D than Alzheimer disease patients without fractures, who in turn have lower intake than cognitively intact controls.19 Similarly, sunlight exposure is lowest in Alzheimer disease fracture patients, intermediate in nonfracture patients with Alzheimer disease, and highest in controls. A study of nursing home residents with dementia showed that their sunlight exposure was particularly low, with none of the 46 residents receiving 15 minutes or more of sunlight per week. Their vitamin D intake was also low, with 83% receiving less than the recommended daily allowance.90 Finally, older adults have reduced ability to synthesize vitamin D3 in the skin. Even in the presence of normal vitamin D and PTH levels, gastrointestinal calcium absorption may be low, in both Alzheimer disease and vascular dementia.105
Osteoporosis/Bone Mineral Density
Bone mineral density is an independent predictor of fractures.86,106 After adjusting for age, each decrease in femoral neck bone density by 1 standard deviation increases risk of hip fracture 2.6 times, and women in the lowest quartile of bone density have an 8.5-fold risk of hip fracture versus those in the highest quartile.107
There is evidence that patients with Alzheimer disease have lower BMD and are more likely to have osteoporosis,20 although the findings are mixed.17,89,108 In a study of 71 patients with early Alzheimer disease and 69 who were cognitively intact, mean BMD was lower in the early AD group (1.11 ± 0.13) compared with those without dementia (1.16 ± 0.12, P = .02), after adjusting for age, sex, habitual physical activity, smoking, depression, estrogen replacement, and apoE4 carrier status.109 In a study of Alzheimer disease and hip fracture, BMD was 1.42 mm Al ± 0.19 in the dementia with hip fracture group, 2.24 mm Al ± 0.44 in the dementia without hip fracture group, and 2.55 mm Al ± 0.36 in the cognitively intact group.19 Bone mineral density was correlated negatively with duration of dementia.
Cachexia/Sarcopenia
Patients with dementia have lower body mass index (BMI) than their cognitively intact counterparts.19,110 Weight loss is a common finding in Alzheimer disease, particularly in the late stages.111 The etiology may be multifactorial, including inability to prepare and eat food, sensory impairment, concomitant depression, increased energy requirements, social factors, and comorbidity.110 Causes may vary based on type of dementia and stage of disease.
Low BMI, in turn, increases hip fracture risk in many22,35 but not all86 studies and is correlated with other findings that may increase hip fracture risk. In patients with Alzheimer disease, BMD is positively correlated with BMI in patients with and without hip fractures.19 This may mediate much of the impact of BMI on fracture risk; in one large study of ambulatory, non-black older women, adjustment for BMD reduced the relative risk of hip fracture in thin women from 2.51 to 0.98.112 In addition, older adults with a BMI <20 are more likely to have low vitamin D levels than their normal weight and overweight counterparts.98 Weight loss is typically associated with a reduction in muscle mass,111 or sarcopenia, which can in turn reduce strength. Arm muscle area is correlated with BMI, and low muscle area increases the relative risk of hip fracture by 1.8.35 It is theorized that reduced fat thickness leads to diminished absorption of energy of the greater trochanter in the event of a fall,22 and low skin-fold thickness increases the risk of hip fractures 2-fold.35 All of these outcomes increase the risk of sustaining hip fractures. Studies of community-dwelling older men21 and women113 showed that a weight loss of 10% or greater was associated with an adjusted relative risk of hip fracture of 1.8 and 2.9 for men and women, respectively, whereas weight gain of 10% or more was associated with a reduction of risk, with a relative risk of 0.4 and 0.7, respectively.
Depression
Patients with dementia commonly suffer from depression. The best estimates of the prevalence of depression in people with probable or possible Alzheimer disease are 20% and 13%, respectively, in community-dwelling individuals with dementia.114 Approximately 41% have depressive symptoms. Apathy is very common in Alzheimer disease, occurring in 61% to 92% of patients, and is sometimes difficult to distinguish from depression.
A recent meta-analysis of 14 prospective studies showed that depression increases fracture risk.115 Depression was associated with a hazard ratio of 1.17 for sustaining a fracture and an overall risk ratio of 1.52.
Depression is associated with several risk factors that increase hip fracture risk. For example, depression is associated with increased falls risk,75,77 lower BMI,110 higher rate of bone loss,116 higher prevalence of smoking,116 lower activity level,116 and lower use of calcium supplementation.116 In a cross-sectional study of older adults with an average age of 75, participants with vitamin D deficiency were almost 12 times as likely to suffer from a mood disorder as those who had adequate vitamin D levels.41
People with depression are also at higher risk of developing dementia. A recent longitudinal study showed that those with depression at baseline had a hazard ratio of 1.72 for developing dementia and 1.76 for developing Alzheimer disease.117
The medications that patients with depression take can affect risk as well. Antidepressants increase the risk of fracture,17,18,32,118 contribute to bone loss,115 and increase falls risk.119 A large prospective study demonstrated that individuals who took selective serotonin reuptake inhibitors (SSRIs), but not tricyclic antidepressants (TCAs), had a greater rate of bone loss than those who were not on antidepressants.120 Both SSRIs and TCAs increase the risk of falls.119 Patients with depression and patients on antidepressants are more likely to be prescribed benzodiazepines,121 which in turn increases risk of fracture.
Impact of Treatment of Dementia on Hip Fractures
In addition to the risks associated with antidepressants as above, patients with dementia are more likely to take medications that have been shown to increase risk for falls and fractures.122 Antipsychotics122 and anxiolytics17,18 increase the risk of hip fracture. The risk of typical versus atypical antipsychotic agents appears similar, although the evidence is still inconclusive.123 In one study, the use of hypnotics-anxiolytics with an elimination half-life of 24 hours or less did not lead to increased risk, but those with a longer half-life had an OR of 1.8 for sustaining a hip fracture.122
Cholinesterase inhibitors, which are often prescribed for Alzheimer disease, increase the risk of syncope and bradycardia and had a hazard ratio of 1.18 for the risk of hip fractures in a population-based cohort study of over 80 000 patients.124 In another large, case-control study, patients with hip fractures were twice as likely to be taking cholinesterase inhibitors as their age- and sex-matched counterparts who were admitted for pneumonia or myocardial infarction.118
Certain medications may also impact intermediate risk factors. Psychotropic medications increase the risk of falls in patients with dementia, and account for 36% of attributable risk.125 Patients with dementia of the Lewy body type are at high risk of sensitivity to antipsychotics, resulting in postural instability and falls. Treatment with neuroleptics increases the risk of extrapyramidal symptoms, which can lead to reduced gait speed.
Hip Fracture as a Predictor of Cognitive Decline
The above discussion has focused on the trajectory from dementia to hip fracture, but there is some evidence that a hip fracture can in turn lead to cognitive decline.24 In a study by Melton et al, 25 of 26 Alzheimer disease patients with hip fracture had the onset of Alzheimer disease after the hip fracture. The authors postulate that either the hip fracture brought the dementia to clinical attention or that patients who were marginally compensated prior to the event had further cognitive deterioration.
Delirium is certainly a major risk following hip fracture surgery, occurring in 35% to 65% of patients with hip fracture.126 Delirium can persist for months; in one study, 32% had delirium at 1 month and 6% had it at 6 months.127 There is also a growing appreciation of an overlap of delirium and dementia; that is, delirium may “unmask” a dementia that did not come to attention prior to the onset of the delirium.
In one study, patients with dementia were 4 times more likely to have depression immediately after a hip fracture than patients without dementia (OR calculated from data in text).128 In another study, 38% of patients with cognitive impairment had depression.129 This could, in turn, lead to worsening cognition.
Summary and Conclusions
Dementia and hip fractures are increasingly common problems in older adults and are associated with substantial morbidity and mortality. The incidence of hip fractures in patients with dementia is higher than in older adults without dementia, and there are several pathways that are implicated in this increase in risk. The relationship between dementia and hip fracture is complex, and we are unaware of any previous articles that have explored the pathway from one endpoint to another in a comprehensive manner.
Given the serious outcomes to patients with dementia and hip fractures, the goal of prevention is an important one. The expected demographic shift over the coming decades adds urgency to this issue. There are multiple physiologic/pathologic intermediate risk factors that have the potential for intervention and treatment in order to reduce risk. However, the individual risk factors for each pathway and the relative reduction in risk with treatment need to be explored further, in order to reduce the consequences of hip fracture in a vulnerable group of patients. Research evaluating the multiple intermediate risk factors in a comprehensive way is needed as a step toward developing an optimal evidence-based approach to reducing hip fractures in patients with dementia.
Acknowledgment
The authors would like to thank Dr. William Hall for his thoughtful feedback on this manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: NIA grant T32 020493-05, the AO Research Foundation, and Highland Hospital in the preparation of this article. None of these sources of support had any role in the development of this paper.
References
- 1. Evans DA, Funkenstein HH, Albert MS, et al. Prevalence of Alzheimer's disease in a community population of older persons. Higher than previously reported. JAMA. 1989;262(18):2551–2556 [PubMed] [Google Scholar]
- 2. Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366(9503):2112–2117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diagnostic and Statistical Manual of Mental Disorders DSM-IV. Fourth ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 4. Guo Z, Viitanen M, Winblad B. Low blood pressure and five-year mortality in a Stockholm cohort of the very old: possible confounding by cognitive impairment and other factors. Am J Public Health. 1997;87(4):623–628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370 [DOI] [PubMed] [Google Scholar]
- 6. Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149(11):2445–2448 [PubMed] [Google Scholar]
- 7. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leslie WD, O'Donnell S, Jean S, et al. Trends in hip fracture rates in Canada. JAMA. 2009;302(8):883–889 [DOI] [PubMed] [Google Scholar]
- 9. Marks R. Hip fracture epidemiological trends, outcomes, and risk factors, 1970-2009. Int J Gen Med. 2010;3:1–17 [PMC free article] [PubMed] [Google Scholar]
- 10. Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498–M507 [DOI] [PubMed] [Google Scholar]
- 11. Morris AH, Zuckerman JD. National Consensus Conference on Improving the Continuum of Care for Patients with Hip Fracture. J Bone Joint Surg Am. 2002;84-A(4):670–674 [DOI] [PubMed] [Google Scholar]
- 12. Haentjens P, Magaziner J, Colon-Emeric CS, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50(10):1644–1650 [DOI] [PubMed] [Google Scholar]
- 14. Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–2276 [DOI] [PubMed] [Google Scholar]
- 15. Yancik R, Ershler W, Satariano W, Hazzard W, Cohen HJ, Ferrucci L. Report of the national institute on aging task force on comorbidity. J Gerontol A Biol Sci Med Sci. 2007;62(3):275–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Morris JC, Rubin EH, Morris EJ, Mandel SA. Senile dementia of the Alzheimer's type: an important risk factor for serious falls. J Gerontol. 1987;42(4):412–417 [DOI] [PubMed] [Google Scholar]
- 17. Johansson C, Skoog I. A population-based study on the association between dementia and hip fractures in 85-year olds. Aging (Milano). 1996;8(3):189–196 [DOI] [PubMed] [Google Scholar]
- 18. van Staa TP, Leufkens HG, Cooper C. Utility of medical and drug history in fracture risk prediction among men and women. Bone. 2002;31(4):508–514 [DOI] [PubMed] [Google Scholar]
- 19. Sato Y, Kanoko T, Satoh K, Iwamoto J. Risk factors for hip fracture among elderly patients with Alzheimer's disease. J Neurol Sci. 2004;223(2):107–112 [DOI] [PubMed] [Google Scholar]
- 20. Weller I, Schatzker J. Hip fractures and Alzheimer's disease in elderly institutionalized Canadians. Ann Epidemiol. 2004;14(5):319–324 [DOI] [PubMed] [Google Scholar]
- 21. Langlois JA, Visser M, Davidovic LS, Maggi S, Li G, Harris TB. Hip fracture risk in older white men is associated with change in body weight from age 50 years to old age. Arch Intern Med. 1998;158(9):990–996 [DOI] [PubMed] [Google Scholar]
- 22. Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA. Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int. 1993;52(3):192–198 [DOI] [PubMed] [Google Scholar]
- 23. Porter RW, Miller CG, Grainger D, Palmer SB. Prediction of hip fracture in elderly women: a prospective study. BMJ. 1990;301(6753):638–641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Melton LJ 3rd, Beard CM, Kokmen E, Atkinson EJ, O'Fallon WM. Fracture risk in patients with Alzheimer's disease. J Am Geriatr Soc. 1994;42(6):614–619 [DOI] [PubMed] [Google Scholar]
- 25. Xie J, Brayne C, Matthews FE. Survival times in people with dementia: analysis from population based cohort study with 14 year follow-up. BMJ. 2008;336(7638):258–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Holmes C, Cairns N, Lantos P, Mann A. Validity of current clinical criteria for Alzheimer's disease, vascular dementia and dementia with Lewy bodies. Br J Psychiatry. 1999;174:45–50 [DOI] [PubMed] [Google Scholar]
- 27. Ballard CG, Shaw F, Lowery K, McKeith I, Kenny R. The prevalence, assessment and associations of falls in dementia with Lewy bodies and Alzheimer's disease. Dement Geriatr Cogn Disord. 1999;10(2):97–103 [DOI] [PubMed] [Google Scholar]
- 28. Buell JS, Dawson-Hughes B. Vitamin D and neurocognitive dysfunction: preventing “D"ecline?. Mol Aspects Med. 2008;29(6):415–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Aarsland D, Zaccai J, Brayne C. A systematic review of prevalence studies of dementia in Parkinson's disease. Mov Disord. 2005;20(10):1255–1263 [DOI] [PubMed] [Google Scholar]
- 30. Gorelick PB, Freels S, Harris Y, Dollear T, Billingsley M, Brown N. Epidemiology of vascular and Alzheimer's dementia among African Americans in Chicago, IL: baseline frequency and comparison of risk factors. Neurology. 1994;44(8):1391–1396 [DOI] [PubMed] [Google Scholar]
- 31. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198 [DOI] [PubMed] [Google Scholar]
- 32. Guo Z, Wills P, Viitanen M, Fastbom J, Winblad B. Cognitive impairment, drug use, and the risk of hip fracture in persons over 75 years old: a community-based prospective study. Am J Epidemiol. 1998;148(9):887–892 [DOI] [PubMed] [Google Scholar]
- 33. Buchner DM, Larson EB. Falls and fractures in patients with Alzheimer-type dementia. JAMA. 1987;257(11):1492–1495 [PubMed] [Google Scholar]
- 34. Hebert LE, Scherr PA, Beckett LA, et al. Age-specific incidence of Alzheimer's disease in a community population. JAMA. 1995;273(17):1354–1359 [PubMed] [Google Scholar]
- 35. Farmer ME, Harris T, Madans JH, Wallace RB, Cornoni-Huntley J, White LR. Anthropometric indicators and hip fracture. The NHANES I epidemiologic follow-up study. J Am Geriatr Soc. 1989;37(1):9–16 [DOI] [PubMed] [Google Scholar]
- 36. Zamboni M, Zoico E, Tosoni P, et al. Relation between vitamin D, physical performance, and disability in elderly persons. J Gerontol A Biol Sci Med Sci. 2002;57(1):M7–M11 [DOI] [PubMed] [Google Scholar]
- 37. Cumming RG, Nevitt MC, Cummings SR. Epidemiology of hip fractures. Epidemiol Rev. 1997;19(2):244–257 [DOI] [PubMed] [Google Scholar]
- 38. Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ. Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat. 2005;29(1):21–30 [DOI] [PubMed] [Google Scholar]
- 39. Sutherland MK, Somerville MJ, Yoong LK, Bergeron C, Haussler MR, McLachlan DR. Reduction of vitamin D hormone receptor mRNA levels in Alzheimer as compared to Huntington hippocampus: correlation with calbindin-28k mRNA levels. Brain Res Mol Brain Res. 1992;13(3):239–250 [DOI] [PubMed] [Google Scholar]
- 40. Przybelski RJ, Binkley NC. Is vitamin D important for preserving cognition? A positive correlation of serum 25-hydroxyvitamin D concentration with cognitive function. Arch Biochem Biophys. 2007;460(2):202–205 [DOI] [PubMed] [Google Scholar]
- 41. Wilkins CH, Sheline YI, Roe CM, Birge SJ, Morris JC. Vitamin D deficiency is associated with low mood and worse cognitive performance in older adults. Am J Geriatr Psychiatry. 2006;14(12):1032–1040 [DOI] [PubMed] [Google Scholar]
- 42. Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–739 [DOI] [PubMed] [Google Scholar]
- 43. Allan LM, Ballard CG, Rowan EN, Kenny RA. Incidence and prediction of falls in dementia: a prospective study in older people. PLoS One. 2009;4(5):e5521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fritsch T, Smyth KA, McClendon MJ, et al. Associations between dementia/mild cognitive impairment and cognitive performance and activity levels in youth. J Am Geriatr Soc. 2005;53(7):1191–1196 [DOI] [PubMed] [Google Scholar]
- 45. Podewils LJ, Guallar E, Kuller LH, et al. Physical activity, APOE genotype, and dementia risk: findings from the Cardiovascular Health Cognition Study. Am J Epidemiol. 2005;161(7):639–651 [DOI] [PubMed] [Google Scholar]
- 46. Baker LD, Frank LL, Foster-Schubert K, et al. Effects of aerobic exercise on mild cognitive impairment: a controlled trial. Arch Neurol. 2010;67(1):71–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Anstey KJ, von Sanden C, Salim A, O'Kearney R. Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol. 2007;166(4):367–378 [DOI] [PubMed] [Google Scholar]
- 48. Razani J, Boone K, Lesser I, Weiss D. Effects of cigarette smoking history on cognitive functioning in healthy older adults. Am J Geriatr Psychiatry. 2004;12(4):404–411 [DOI] [PubMed] [Google Scholar]
- 49. Bauer DC, Browner WS, Cauley JA, et al. Factors associated with appendicular bone mass in older women. The Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1993;118(9):657–665 [DOI] [PubMed] [Google Scholar]
- 50. Hoidrup S, Prescott E, Sorensen TI, et al. Tobacco smoking and risk of hip fracture in men and women. Int J Epidemiol. 2000;29(2):253–259 [DOI] [PubMed] [Google Scholar]
- 51. Kanis JFRAX: WHO Fracture Risk Assessment Tool Web version 3.1. World Health Organization on Collaborating Centre for Metabolic Bone Diseases. http://www.shef.ac.uk/FRAX/ Accessed November 8, 2010
- 52. Kumar V, Kinsella LJ. Healthy brain aging: effect of head injury, alcohol and environmental toxins. Clin Geriatr Med. 2010;26(1):29–44 [DOI] [PubMed] [Google Scholar]
- 53. Myers RH, Schaefer EJ, Wilson PW, et al. Apolipoprotein E epsilon4 association with dementia in a population-based study: The Framingham study. Neurology. 1996;46(3):673–677 [DOI] [PubMed] [Google Scholar]
- 54. Johnston JM, Cauley JA, Ganguli M. APOE 4 and hip fracture risk in a community-based study of older adults. J Am Geriatr Soc. 1999;47(11):1342–1345 [DOI] [PubMed] [Google Scholar]
- 55. Kohlmeier M, Saupe J, Schaefer K, Asmus G. Bone fracture history and prospective bone fracture risk of hemodialysis patients are related to apolipoprotein E genotype. Calcif Tissue Int. 1998;62(3):278–281 [DOI] [PubMed] [Google Scholar]
- 56. Kohlmeier M, Salomon A, Saupe J, Shearer MJ. Transport of vitamin K to bone in humans. J Nutr. 1996;126(4 suppl):1192S–1196S [DOI] [PubMed] [Google Scholar]
- 57. Hart JP, Catterall A, Dodds RA, et al. Circulating vitamin K1 levels in fractured neck of femur. Lancet. 1984;2(8397):283. [DOI] [PubMed] [Google Scholar]
- 58. Vermeer C, Gijsbers BL, Craciun AM, Groenen-van Dooren MM, Knapen MH. Effects of vitamin K on bone mass and bone metabolism. J Nutr. 1996;126(4 suppl):1187S–1191S [DOI] [PubMed] [Google Scholar]
- 59. Visser H. Gait and balance in senile dementia of Alzheimer's type. Age Ageing. 1983;12(4):296–301 [DOI] [PubMed] [Google Scholar]
- 60. Tanaka A, Okuzumi H, Kobayashi I, Murai N, Meguro K, Nakamura T. Gait disturbance of patients with vascular and Alzheimer-type dementias. Percept Mot Skills. 1995;80(3 pt 1):735–738 [DOI] [PubMed] [Google Scholar]
- 61. Wolfson L, Whipple R, Amerman P, Tobin JN. Gait assessment in the elderly: a gait abnormality rating scale and its relation to falls. J Gerontol. 1990;45(1):M12–M19 [DOI] [PubMed] [Google Scholar]
- 62. Nakamura T, Meguro K, Sasaki H. Relationship between falls and stride length variability in senile dementia of the Alzheimer type. Gerontology. 1996;42(2):108–113 [DOI] [PubMed] [Google Scholar]
- 63. Della Sala S, Spinnler H, Venneri A. Walking difficulties in patients with Alzheimer's disease might originate from gait apraxia. J Neurol Neurosurg Psychiatry. 2004;75(2):196–201 [PMC free article] [PubMed] [Google Scholar]
- 64. Shaw FE. Falls in cognitive impairment and dementia. Clin Geriatr Med. 2002;18(2):159–173 [DOI] [PubMed] [Google Scholar]
- 65. Camicioli R, Howieson D, Lehman S, Kaye J. Talking while walking: the effect of a dual task in aging and Alzheimer's disease. Neurology. 1997;48(4):955–958 [DOI] [PubMed] [Google Scholar]
- 66. Algotsson A, Viitanen M, Winblad B, Solders G. Autonomic dysfunction in Alzheimer's disease. Acta Neurol Scand. 1995;91(1):14–18 [DOI] [PubMed] [Google Scholar]
- 67. Robbins AS, Rubenstein LZ, Josephson KR, Schulman BL, Osterweil D, Fine G. Predictors of falls among elderly people. Results of two population-based studies. Arch Intern Med. 1989;149(7):1628–1633 [PubMed] [Google Scholar]
- 68. Ballard C, Shaw F, McKeith I, Kenny R. High prevalence of neurovascular instability in neurodegenerative dementias. Neurology. 1998;51(6):1760–1762 [DOI] [PubMed] [Google Scholar]
- 69. Ward CR, McIntosh S, Kenny RA. Carotid sinus hypersensitivity--a modifiable risk factor for fractured neck of femur. Age Ageing. 1999;28(2):127–133 [DOI] [PubMed] [Google Scholar]
- 70. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707 [DOI] [PubMed] [Google Scholar]
- 71. Horikawa E, Matsui T, Arai H, Seki T, Iwasaki K, Sasaki H. Risk of falls in Alzheimer's disease: a prospective study. Intern Med. 2005;44(7):717–721 [DOI] [PubMed] [Google Scholar]
- 72. Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143(11):1129–1136 [DOI] [PubMed] [Google Scholar]
- 73. Anstey KJ, von Sanden C, Luszcz MA. An 8-year prospective study of the relationship between cognitive performance and falling in very old adults. J Am Geriatr Soc. 2006;54(8):1169–1176 [DOI] [PubMed] [Google Scholar]
- 74. Chen JS, March LM, Schwarz J, et al. A multivariate regression model predicted falls in residents living in intermediate hostel care. J Clin Epidemiol. 2005;58(5):503–508 [DOI] [PubMed] [Google Scholar]
- 75. Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age Ageing. 1981;10(4):264–270 [DOI] [PubMed] [Google Scholar]
- 76. Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med. 1994;121(6):442–451 [DOI] [PubMed] [Google Scholar]
- 77. van Doorn C, Gruber-Baldini AL, Zimmerman S, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. J Am Geriatr Soc. 2003;51(9):1213–1218 [DOI] [PubMed] [Google Scholar]
- 78. Camicioli R, Licis L. Motor impairment predicts falls in specialized Alzheimer care units. Alzheimer Dis Assoc Disord. 2004;18(4):214–218 [PubMed] [Google Scholar]
- 79. Asada T, Kariya T, Kinoshita T, et al. Predictors of fall-related injuries among community-dwelling elderly people with dementia. Age Ageing. 1996;25(1):22–28 [DOI] [PubMed] [Google Scholar]
- 80. Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46(5):M164–M170 [DOI] [PubMed] [Google Scholar]
- 81. Myers AH, Baker SP, Van Natta ML, Abbey H, Robinson EG. Risk factors associated with falls and injuries among elderly institutionalized persons. Am J Epidemiol. 1991;133(11):1179–1190 [DOI] [PubMed] [Google Scholar]
- 82. Buchner DM, Larson EB. Transfer bias and the association of cognitive impairment with falls. J Gen Intern Med. 1988;3(3):254–259 [DOI] [PubMed] [Google Scholar]
- 83. van Dijk PT, Meulenberg OG, van de Sande HJ, Habbema JD. Falls in dementia patients. Gerontologist. 1993;33(2):200–204 [DOI] [PubMed] [Google Scholar]
- 84. van Schoor NM, Smit JH, Pluijm SM, Jonker C, Lips P. Different cognitive functions in relation to falls among older persons. Immediate memory as an independent risk factor for falls. J Clin Epidemiol. 2002;55(9):855–862 [DOI] [PubMed] [Google Scholar]
- 85. Gleason CE, Gangnon RE, Fischer BL, Mahoney JE. Increased risk for falling associated with subtle cognitive impairment: secondary analysis of a randomized clinical trial. Dement Geriatr Cogn Disord. 2009;27(6):557–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Greenspan SL, Myers ER, Kiel DP, Parker RA, Hayes WC, Resnick NM. Fall direction, bone mineral density, and function: risk factors for hip fracture in frail nursing home elderly. Am J Med. 1998;104(6):539–545 [DOI] [PubMed] [Google Scholar]
- 87. Schwartz AV, Kelsey JL, Sidney S, Grisso JA. Characteristics of falls and risk of hip fracture in elderly men. Osteoporos Int. 1998;8(3):240–246 [DOI] [PubMed] [Google Scholar]
- 88. Brody EM, Kleban MH, Moss MS, Kleban F. Predictors of falls among institutionalized women with Alzheimer's disease. J Am Geriatr Soc. 1984;32(12):877–882 [DOI] [PubMed] [Google Scholar]
- 89. Kipen E, Helme RD, Wark JD, Flicker L. Bone density, vitamin D nutrition, and parathyroid hormone levels in women with dementia. J Am Geriatr Soc. 1995;43(10):1088–1091 [DOI] [PubMed] [Google Scholar]
- 90. Sato Y, Asoh T, Oizumi K. High prevalence of vitamin D deficiency and reduced bone mass in elderly women with Alzheimer's disease. Bone. 1998;23(6):555–557 [DOI] [PubMed] [Google Scholar]
- 91. Dhesi JK, Bearne LM, Moniz C, et al. Neuromuscular and psychomotor function in elderly subjects who fall and the relationship with vitamin D status. J Bone Miner Res. 2002;17(5):891–897 [DOI] [PubMed] [Google Scholar]
- 92. Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of Vitamin D on falls: a meta-analysis. JAMA. 2004;291(16):1999–2006 [DOI] [PubMed] [Google Scholar]
- 93. Glerup H, Mikkelsen K, Poulsen L, et al. Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int. 2000;66(6):419–424 [DOI] [PubMed] [Google Scholar]
- 94. Schott GD, Wills MR. Muscle weakness in osteomalacia. Lancet. 1976;1(7960):626–629 [DOI] [PubMed] [Google Scholar]
- 95. Gerdhem P, Ringsberg KA, Obrant KJ, Akesson K. Association between 25-hydroxy vitamin D levels, physical activity, muscle strength and fractures in the prospective population-based OPRA Study of Elderly Women. Osteoporos Int. 2005;16(11):1425–1431 [DOI] [PubMed] [Google Scholar]
- 96. Pfeifer M, Begerow B, Minne HW, Suppan K, Fahrleitner-Pammer A, Dobnig H. Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int. 2009;20(2):315–322 [DOI] [PubMed] [Google Scholar]
- 97. Bunout D, Barrera G, Leiva L, et al. Effects of vitamin D supplementation and exercise training on physical performance in Chilean vitamin D deficient elderly subjects. Exp Gerontol. 2006;41(8):746–752 [DOI] [PubMed] [Google Scholar]
- 98. Wicherts IS, van Schoor NM, Boeke AJ, et al. Vitamin D status predicts physical performance and its decline in older persons. J Clin Endocrinol Metab. 2007;92(6):2058–2065 [DOI] [PubMed] [Google Scholar]
- 99. Bischoff-Ferrari HA, Dietrich T, Orav EJ, et al. Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged > or =60 y. Am J Clin Nutr. 2004;80(3):752–758 [DOI] [PubMed] [Google Scholar]
- 100. Stel VS, Smit JH, Pluijm SM, Lips P. Balance and mobility performance as treatable risk factors for recurrent falling in older persons. J Clin Epidemiol. 2003;56(7):659–668 [DOI] [PubMed] [Google Scholar]
- 101. Annweiler C, Schott AM, Berrut G, Fantino B, Beauchet O. Vitamin D-related changes in physical performance: a systematic review. J Nutr Health Aging. 2009;13(10):893–898 [DOI] [PubMed] [Google Scholar]
- 102. Chapuy MC, Arlot ME, Duboeuf F, et al. Vitamin D3 and calcium to prevent hip fractures in the elderly women. N Engl J Med. 1992;327(23):1637–1642 [DOI] [PubMed] [Google Scholar]
- 103. Jackson C, Gaugris S, Sen SS, Hosking D. The effect of cholecalciferol (vitamin D3) on the risk of fall and fracture: a meta-analysis. QJM. 2007;100(4):185–192 [DOI] [PubMed] [Google Scholar]
- 104. Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res. 2000;15(6):1113–1118 [DOI] [PubMed] [Google Scholar]
- 105. Ferrier IN, Leake A, Taylor GA, et al. Reduced gastrointestinal absorption of calcium in dementia. Age Ageing. 1990;19(6):368–375 [DOI] [PubMed] [Google Scholar]
- 106. Nguyen T, Sambrook P, Kelly P, et al. Prediction of osteoporotic fractures by postural instability and bone density. BMJ. 1993;307(6912):1111–1115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Cummings SR, Black DM, Nevitt MC, et al. Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet. 1993;341(8837):72–75 [DOI] [PubMed] [Google Scholar]
- 108. Foldes J, Menczel J. Cognitive function, hip fractures, and spinal osteoporosis in the elderly. J Am Geriatr Soc. 1988;36(8):756. [DOI] [PubMed] [Google Scholar]
- 109. Loskutova N, Honea RA, Vidoni ED, Brooks WM, Burns JM. Bone density and brain atrophy in early Alzheimer's disease. J Alzheimers Dis. 2009;18(4):777–785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Berlinger WG, Potter JF. Low Body Mass Index in demented outpatients. J Am Geriatr Soc. 1991;39(10):973–978 [DOI] [PubMed] [Google Scholar]
- 111. Poehlman ET, Dvorak RV. Energy expenditure, energy intake, and weight loss in Alzheimer disease. Am J Clin Nutr. 2000;71(2):650S–655S [DOI] [PubMed] [Google Scholar]
- 112. Ensrud KE, Lipschutz RC, Cauley JA, et al. Body size and hip fracture risk in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Am J Med. 1997;103(4):274–280 [DOI] [PubMed] [Google Scholar]
- 113. Langlois JA, Harris T, Looker AC, Madans J. Weight change between age 50 years and old age is associated with risk of hip fracture in white women aged 67 years and older. Arch Intern Med. 1996;156(9):989–994 [PubMed] [Google Scholar]
- 114. Landes AM, Sperry SD, Strauss ME. Prevalence of apathy, dysphoria, and depression in relation to dementia severity in Alzheimer's disease. J Neuropsychiatry Clin Neurosci. 2005;17(3):342–349 [DOI] [PubMed] [Google Scholar]
- 115. Wu Q, Liu J, Gallegos-Orozco JF, Hentz JG. Depression, fracture risk, and bone loss: a meta-analysis of cohort studies. Osteoporos Int. 2010;21(10):1627–1635 [DOI] [PubMed] [Google Scholar]
- 116. Diem SJ, Blackwell TL, Stone KL, et al. Depressive symptoms and rates of bone loss at the hip in older women. J Am Geriatr Soc. 2007;55(6):824–831 [DOI] [PubMed] [Google Scholar]
- 117. Saczynski JS, Beiser A, Seshadri S, Auerbach S, Wolf PA, Au R. Depressive symptoms and risk of dementia: The Framingham Heart Study. Neurology. 2010;75(1):35–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. French DD, Campbell R, Spehar A, Cunningham F, Foulis P. Outpatient medications and hip fractures in the US: a national veterans study. Drugs Aging. 2005;22(10):877–885 [DOI] [PubMed] [Google Scholar]
- 119. Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30–39 [DOI] [PubMed] [Google Scholar]
- 120. Diem SJ, Blackwell TL, Stone KL, et al. Use of antidepressants and rates of hip bone loss in older women: the study of osteoporotic fractures. Arch Intern Med. 2007;167(12):1240–1245 [DOI] [PubMed] [Google Scholar]
- 121. Bartlett G, Abrahamowicz M, Grad R, Sylvestre MP, Tamblyn R. Association between risk factors for injurious falls and new benzodiazepine prescribing in elderly persons. BMC Fam Pract. 2009;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Ray WA, Griffin MR, Schaffner W, Baugh DK, Melton LJ., 3rd Psychotropic drug use and the risk of hip fracture. N Engl J Med. 1987;316(7):363–369 [DOI] [PubMed] [Google Scholar]
- 123. Trifiro G, Spina E, Gambassi G. Use of antipsychotics in elderly patients with dementia: do atypical and conventional agents have a similar safety profile?. Pharmacol Res. 2009;59(1):1–12 [DOI] [PubMed] [Google Scholar]
- 124. Gill SS, Anderson GM, Fischer HD, et al. Syncope and its consequences in patients with dementia receiving cholinesterase inhibitors: a population-based cohort study. Arch Intern Med. 2009;169(9):867–873 [DOI] [PubMed] [Google Scholar]
- 125. Thapa PB, Gideon P, Fought RL, Ray WA. Psychotropic drugs and risk of recurrent falls in ambulatory nursing home residents. Am J Epidemiol. 1995;142(2):202–211 [DOI] [PubMed] [Google Scholar]
- 126. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–522 [DOI] [PubMed] [Google Scholar]
- 127. Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48(6):618–624 [DOI] [PubMed] [Google Scholar]
- 128. Billig N, Ahmed SW, Kenmore P, Amaral D, Shakhashiri MZ. Assessment of depression and cognitive impairment after hip fracture. J Am Geriatr Soc. 1986;34(7):499–503 [DOI] [PubMed] [Google Scholar]
- 129. Givens JL, Sanft TB, Marcantonio ER. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc. 2008;56(6):1075–1079 [DOI] [PubMed] [Google Scholar]