Abstract
Introduction: Nursing home residents represent a large proportion of patients hospitalized with hip fracture. Generally, residents do not achieve the same physical ability level as before their fracture and have an increased risk of death within few days after discharge. This study aims to compare 2 new approaches to geriatric intervention in residents with hip fracture. Materials and Methods: In nursing home residents aged 65 or older with hip fracture, 85 received a newly developed standardized rehabilitation intervention undertaken by the geriatric orthopedic team (GO team) from December 1, 2006 to November 30, 2007. This standardized method was compared with a further developed tailor-made intervention method performed by the GO team in 153 residents from February 1, 2008 to January 31, 2010. Both the interventions began at hospital admission and until 30 days after surgery. Outcomes were length of hospital stay (LOS), difference in physical ability, 90-day acute readmission, 30-day mortality, and 90-day mortality. Results: The tailor-made intervention method reduced the readmission rate (14% vs 26%) compared with the standardized intervention method (odds ratio [OR] = 0.47 [95% confidence interval [CI]: 0.23, 0.94]). Tailor-made intervention reduced 30-day mortality (8% vs 19%) compared with standardized intervention (OR = 0.42 [95% CI: 0.18, 0.97]). Improving 90-day survival could not be demonstrated (81% vs 73%; OR = 0.72 [95% CI: 0.37, 1.40]). Median LOS was 2 days in both the groups. A total of 7 follow-up visits were performed with tailor-made intervention versus 3 visits with standardized intervention. In both the groups, the physical ability decreased significantly within the first 30 postoperative days, with no difference between groups (β = 1.01 [95% CI: 0.82, 1.24]).Conclusion: A multidisciplinary and tailor-made geriatric intervention in nursing home residents has a positive effect on readmission rate and short-term mortality. Still, it is not obvious which part of the tailor-made intervention is most crucial.
Keywords: frail elderly, hip fractures, home care services, hospital-based, mortality, nursing homes
Introduction
In Denmark, approximately 25% of the elderly patients with hip fracture are residents admitted from nursing homes. The residents are characterized as frail elderly. Over the last decade, the average age of the Danish nursing home residents has increased, the physical functional level has decreased, and about 65% have a diagnosis of dementia. Nursing homes are defined as handicap-friendly accessible housings designed for older people with permanent and substantial physical and/or mental disability who are in need of care day and night and who cannot remain safely in their own homes.1,2
In patients with hip fracture, 30-day mortality is in excess of 10% and 1-year mortality is more than 25% despite improvements in surgical techniques and anesthesia. The risk of death in nursing home residents with hip fracture is higher than in elderly individuals with hip fracture admitted from own homes or senior housing, and the risk is highest within the first 2 weeks after discharge.2,3 The most frequent causes of death among residents with hip fractures are pneumonia, cancer, and cardiovascular diseases.2,4 A Danish study has previously shown that some deaths among nursing home residents with hip fracture could be avoided.4
Geriatric intervention programs have been developed for both acute care and the rehabilitation phase of elderly inpatients with hip fracture, but with varying results depending on the extent of the geriatric involvement. An early and intensive geriatric intervention by a multidisciplinary geriatric team has lead to further improvements.5–22 The results of meta-analysis of comprehensive geriatric assessment for inpatients, outpatients, and in-home treatments indicate that certain types of comprehensive geriatric assessments have a significant, positive effect on mortality, living location, patients' physical and cognitive functional status, and hospital admission/readmission risk during follow-up.23
Demented residents have a higher risk of delirium during hospitalization. Delirium occurs in 28% to 61% of older patients treated for hip fractures. Delirium is associated with the degree of dementia and increases mortality. A multidisciplinary geriatric intervention program reduces the duration of delirium and the mortality after hip fracture by early recognition and treatment.24 There is reasonable evidence that home treatment lowers the incidence of delirium compared with in-hospital treatment.9,25,26
“Early discharge—hospital-at-home” is a service that provides active treatment by health care professionals for a condition that otherwise would require acute hospital inpatient care.27 The concept has not yet been examined among older patients with hip fracture.
This study aims to compare 2 new geriatric approaches developed since 2006.
A multidisciplinary geriatric in-hospital intervention with early discharge followed by a standardized home-based rehabilitation program.
A multidisciplinary geriatric in-hospital intervention with early discharge followed by a tailor-made hospital-at-home treatment.
Materials and Methods
Design
The study was designed as a follow-up study and carried out prospectively in 2 cohorts. The first cohort followed the first model of a standardized rehabilitation program and served as reference, and the second cohort followed the tailor-made intervention.
Participants
All nursing home residents with hip fractures aged 65 or older admitted to the Orthopaedic Surgery Ward at Aarhus University Hospital were included consecutively during 2 observation periods. A total of 85 residents followed the standardized rehabilitation program from December 1, 2006 to November 30, 2007, and the results were compared with 153 residents admitted from February 1, 2008 to January 31, 2010, who were treated according to the tailor-made intervention. Completeness of the patient material was checked by comparing lists from the patient registration system of all hip fracture patients discharged from the Orthopaedic Surgery Ward with lists of nursing home addresses identified by Aarhus Municipal Registry of nursing homes.
In-Hospital Intervention
A geriatric intervention program based on in-hospital treatment before surgery and shortly afterward was established in an orthopedic ward in 2003 and used in the elderly patients with hip fracture. The geriatric and orthopedic collaboration implied that 1 or 2 days after surgery, the patients were either transferred to a geriatric rehabilitation unit or discharged directly to home-based rehabilitation. In-hospital geriatric intervention comprised medical and physical assessments, osteoporosis, and pain managements, fall diagnosing, and early discharge planning. Physical ability was assessed using the Modified Barthel Index (MBI) based on information from patient, their relatives, and nursing home staff. Early discharge and continuity of care were planned in cooperation with the staff of the orthopedic ward and the nursing homes. In-hospital intervention was performed by a geriatric orthopedic team (GO team). The team consisted of a physician, a nurse, and a physiotherapist working in daytime on weekdays.
Only patients admitted to hospital from nursing homes returned directly to the nursing homes from the orthopedic ward, without receiving geriatric follow-up, since these patients had regular access to medical care by general practitioners and as the 24-hour staff of the nursing homes was close to the residents. In 2003, the median length of hospital stay (LOS) for residents was 3 days, and the 3-month nonelective readmission rate was 21%.3 The residents had a 30-day mortality rate of 27% and increased the overall mortality for hip fracture at the hospital.3
To improve care and treatment after discharge of nursing home residents with hip fracture, a home-based follow-up was planned in 2 new approaches and carried out by the GO team together with the primary care team of the nursing home. The GO team served as coach for the staff. The efforts of the GO team were based on the recommendations of the Danish National Board of Health,28 Accelerated Recovery Program after Hip Fracture,29 and the geriatric specialist knowledge in the bridge building between the hospital and the municipalities.
Standardized Rehabilitation Method
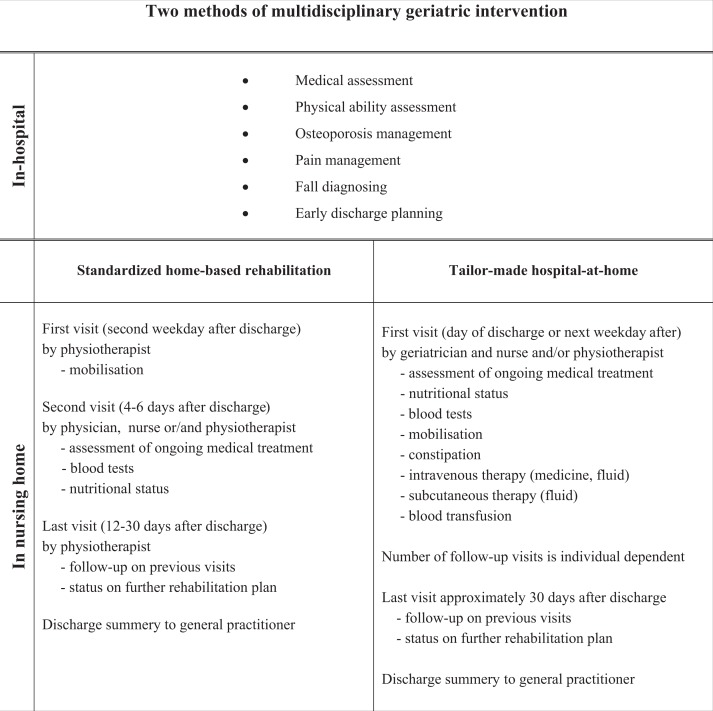
Two days after discharge, the physiotherapist of GO team visited the patient with a special view on mobilization and activities of daily living (ADLs). After 2 to 4 days, the patient was visited by the physician and the nurse, who monitored the nutritional status, assessed ongoing medical treatment including pain management, fall diagnosing, mobilization, and blood tests. If intravenous fluid therapy and blood transfusions were needed, the residents were transported to the hospital. The third and final visit took place between 12 and 30 days after discharge either by the physiotherapist or by the physician and the nurse to evaluate treatment and need for further rehabilitation (Figure 1 ).
Figure 1.
Two multidisciplinary geriatric intervention methods performed in residents with hip fracture in cooperation with staff in both the orthopedic ward and the nursing homes. In-hospital intervention was identical within the 2 methods. After discharge, a standardized home-based rehabilitation program was performed in 2007 and a tailor-made hospital-at-home intervention was performed in 2008 and 2009.
In nursing home residents, the standardized rehabilitation method reduced both 30-day mortality (20% vs 27%) and 3-month mortality (28% vs 40%) when compared with the care in 2003. Despite the promising results, preliminary survey from this 1-year period indicated a need for more individually designed actions. As a consequence, a regimen of tailor-made intervention was implemented from February 1, 2008.
Tailor-Made Intervention Method
The physician and physiotherapist or nurse of the GO team visited the patient on the day of discharge or the following weekday and a date for the next visit or telephone call was scheduled. From the first visit, the focus was on assessment of ongoing medical treatment, fall diagnosing, nutritional status, blood tests, and treatment of infections with oral or intravenous therapy. Anemia was corrected with blood transfusions, and water and electrolyte imbalance with subcutaneous or intravenous fluids therapy. All treatments were performed in the nursing homes. Depending on the issue, the visits were done by the physician, the nurse, and/or the physiotherapist. The number of visits varied individually; the residents had on the average 7 visits and a follow-up period of at least 30 days after surgery (Figure 1).
Data Collection and Main Outcome Measurement
All relevant data and observations were collected continuously for every patient during the follow-up period and retrospectively collected from patient records. Hip fractures were classified as femoral neck fractures or intertrochanteric fractures. Data on 30-day and 90-day mortalities and nonelective readmissions were obtained from The Danish Databank of Health. A preadmission (14 days) functional level estimated by MBI was calculated retrospectively by a physiotherapist from the GO team based on information from the nursing home staff or from relatives. Modified Barthel Index was measured 30 days after admission. The premeasurements and postmeasurements of MBI in a patient were performed by the same physiotherapist. Comorbidity at admission, expressed by Charlson Comorbidity Index (CCI), and dementia diagnosis were estimated from the electronic medical record database on concomitant diagnoses made by a physician. Hemoglobin values were collected from the electronic laboratory information system.
Statistical Analysis
Data were exported to Stata 11.0 for the statistical analysis. Significance level was set at 5%. Patient characteristics were calculated with proportions and percentages, and chi-square test and Student t test with equal variances were used to calculate the differences between the groups. Values of LOS were not normally distributed and were analyzed by the Wilcoxon rank sum test. Outcomes on 30-day and 90-day mortalities and readmissions were analyzed using the logistic regression model with indicator variables. In the postestimations of the regression model, the Hosmer–Lemeshow test for goodness-of-fit was performed. The missing values of MBI of the 30-day deaths were set to zero. The assumptions of the mean difference of the 2 MBI measurements were checked and compared in a multiple linear regression model, first by a crude estimate and then with adjustment of relevant prognostic effect variables. The model was controlled by a postestimated graphic line. All the regression models were tested for interaction and confounding.30
Results
Females constituted the majority of the residents and the average age of the population was 88 years. Both the groups were characterized by high comorbidity. More than two thirds had a known dementia diagnosis and most residents were physically dependent. Surgery methods were similar across groups. Mean value of hemoglobin at admission was 7.6 (standard deviation [SD] 0.87). At baseline, the groups were comparable except for significantly more females in the tailor-made intervention group than in the standardized rehabilitation group. A lower level of functional ability before the hip fracture was found in the standardized rehabilitation group (Table 1 ).
Table 1.
Baseline Characteristicsa
| Baseline characteristics | Multidisciplinary geriatric method |
|
|---|---|---|
| Standardized home-based rehabilitation, n = 85 | Tailor-made hospital-at-home, n = 153 | |
| Sex (%) | ||
| Female | 58 (68) | 127 (83) b |
| Age groups (%) | ||
| 65-79 years old | 36 (42) | 46 (30) |
| 80+ years old | 49 (58) | 107 (70) |
| Surgery methods (%) | ||
| Osteosynthesis | 72 (84) | 120 (79) |
| Hemialloplastic | 9 (11) | 29 (20) |
| Total alloplastic | 4 (5) | 2 (1) |
| Dementia diagnosis (%) | 57 (67) | 96 (63) |
| Charlson Comorbidity Index; mean (SD), (0 = none, 1-2 = moderate, >2 = severe) | 1.77 (1.17) | 1.54 (1.28) |
| Modified Barthel Index 14 days before hip fracture; mean (SD) (0 = minimum; 100 = maximum) | 56 (25.3) | 63 (21.7) b |
| Hemoglobin level at hospital admission (%) | ||
| >7 mmol/L | 63 (74) | 126 (82) |
| 6-7 mmol/L | 18 (21) | 20 (14) |
| 5-5.9 mmol/L | 4 (5) | 6 (3) |
| <5 mmol/L | 0 (0) | 1 (1) |
Abbreviation: SD, standard deviation.
a Nursing home residents with hip fracture admitted to surgery and exposed to standardized home-based rehabilitation program or tailor-made hospital-at-home intervention.
b P ≤ .05.
The 30-day mortality was 19% in the standardized rehabilitation group versus 8% in the tailor-made intervention group (odds ratio [OR]adj = 0.42 [95% confidence interval (CI): 0.18, 0.97]). Patients died 11 median days after surgery (interquartile range = 11). In the logistic regression model, the outcome was adjusted for age, sex, comorbidity, hemoglobin level at admission, and level of physical ability before admission. We found that comorbidity was associated with 30-day mortality (OR = 1.56 [95% CI: 1.14, 2.12]) and without interaction. Age, sex, hemoglobin level at admission, and physical ability before admission were not associated with 30-day mortality. The 90-day mortality was 27% in the standardized rehabilitation group versus 19% in the tailor-made intervention group (OR = 0.72 [95% CI: 0.37, 1.40]. Comorbidity was associated with the 90-day mortality (OR = 1.45 [95% CI: 1.12, 1.87]). No interaction was found. Age, sex, hemoglobin level at admission, and physical ability before admission were not associated with 90-day mortality (Table 2 ).
Table 2.
Nursing Home Residents With Hip Fracture Admitted to Surgery and Multidisciplinary Geriatric Intervention In-Hospital With Subsequent Standardized Home-Based Rehabilitation Program or Tailor-Made Hospital-At-Home Interventiona
| Standardized home-based rehabilitation, n = 85 | Tailor-made hospital-at-home intervention, n = 153 | Estimate with 95% confidence interval |
||
|---|---|---|---|---|
| Crude estimates | Adjusted estimates | |||
| Modified Barthel Index, mean difference (SD) | −22.3 (24.0) | −20.4 (20.0) | 1.03 (0.73, 1.45) | 1.01 (0.82, 1.24) b |
| 90-Day readmission (%) | 22 (26) | 21 (14) | 0.46 (0.23, 0.89) | 0.47 (0.23, 0.94) c |
| 30-Day mortality (%) | 16 (19) | 12 (8) | 0.37 (0.16, 0.82) | 0.43 (0.18, 0.97) c |
| 90-Day mortality (%) | 23 (27) | 29 (19) | 0.63 (0.34, 1.18) | 0.72 (0.37, 1.40) c |
Abbreviation: SD, standard deviation; MBI, Modified Barthel Index; CCI, Charlson Comorbidity Index.
a Outcomes are difference in MBI 14 days before fracture and 30 days after, 90-day nonelective readmission, 30-day mortality, and 90-day mortality. The outcomes in the 2 methods are compared and analyzed by multiple linear regression or logistic regression.
b Multiple linear regression model presented by β estimate (β). Adjustment of sex, age, CCI, MBI before admission, dementia diagnosis, and number of blood transfusions.
c Logistic regression model presented by odds ratio. Adjustment of sex, age, CCI, MBI before admission, and hemoglobin level at admission.
The overall physical functional ability among the residents was significantly reduced in both the groups after hip fracture surgery. The mean MBI score was 63 points before admission and 42 points after 30 days, in the tailor-made intervention group, versus 56 points before and 33 points after, in the standardized rehabilitation group. Mean difference in MBI before and after hospitalization between the groups did not differ from each other (P = .89). The adjusted mean difference in MBI showed an association with MBI before admission (P = .02) but was not associated with sex, age, comorbidity, dementia, or blood transfusion (Table 2). Data from medical records indicated that the incidence of delirium was same in both the groups (11% vs 12%).
Nonelective readmissions within 90 days after discharge occurred among 14% of the residents in the tailor-made intervention group and among 26% of the residents in the standardized rehabilitation group. The tailor-made intervention method reduced the readmission rate compared with the standardized intervention program (OR = 0.47 [95% CI: 0.23, 0.94]). Causes of the nonelective readmissions were hematemesis, melena, anemia, pneumonia, urosepsis, cold, hematuria, arteriosclerosis, cystitis, new fracture, and reoperation caused by displaced fracture. Postoperative hemoglobin values less than 6 mmol/L were associated with readmission (OR = 3.24 [95% CI: 1.15, 9.14]), as was age with readmissions within 90 days (OR = 2.98 [95% CI: 1.08, 8.21]). Neither a low hemoglobin value nor age modified the outcome. Readmissions were not associated with sex, comorbidity, hemoglobin level at admission, and physical ability (Table 2).
The median LOS was 2 days in both the groups (interquartile range = 1). The median period of geriatric follow-up in the tailor-made intervention group was 31 days (interquartile range = 9) versus 26 days in the standardized rehabilitation group days (interquartile range = 10; P < .01).
Discussion
We compared the effect of 2 geriatric methods in managing the frail elderly individuals with hip fracture from nursing homes. One method was a multidisciplinary geriatric in-hospital approach followed by a standardized home-based rehabilitation program. The other method was the same multidisciplinary geriatric in-hospital approach but followed by a tailor-made hospital-at-home treatment.
The tailor-made hospital-at-home intervention increased short-term survival, and some deaths may have been avoided in this frail patient group. According to a Danish mortality study in hip fracture patients, the 30-day mortality was 23% among nursing home residents. That study shows that 30-day mortality was potentially avoidable in 15% of the residents.4 In our study, it is not clear which parts of the tailor-made intervention were the most crucial. Subcutaneous fluid therapy and blood transfusion efforts may improve survival and that needs to be investigated in future randomized trials. A further possible explanation of the higher mortality in the standardized rehabilitation group may be that the proportion of males was higher and that more patients had a lower physical functional ability. Although it is well known that males have a shorter average life span, the short-term mortality was neither associated with sex nor associated with the lower preadmission physical ability as estimated at hospitalization, and it did not influence the outcome significantly.
A large proportion of the residents had a dementia diagnosis and many of them had severe cognitive impairments, which are associated with delirium and mortality.9,31 As a result of the home-based geriatric care, the demented residents were discharged after only 2 days of hospitalization. In both the groups, a potential risk of delirium and, we found that, short-term mortality had been reduced.20 The 5 days longer follow-up period in the tailor-made intervention group was probably not essential to the outcome, as the main part of the intervention was carried out within the first week after discharge.
A hospital-at-home intervention with an individually designed management seemed to reduce the nonelective readmission rate in the nursing home residents, compared with the standardized rehabilitation care and also compared with the usual care in 2003.3 Similar result was found in a study of comanagement in elderly patients with hip fracture, by geriatricians and orthopedic surgeons, where the patients had fewer complications with significantly lower risks of delirium and infections.18 In our study, provision of blood transfusions outside the hospital walls as well as subcutaneous and intravenous fluid therapy requires careful instructions and a close cooperation with the nursing homes staff. A study of blood transfusions given to patients with hip fractures demonstrated that a low hemoglobin level was associated with an increased number of readmissions within 60 days after discharge.32 We made similar findings. The staff had easy access to supervision from the GO team and nonelective readmissions may thus have been avoided.
The aims of rehabilitation after hip fracture in an elderly individual are to recover and maintain the patient’s previous physical ability and make it possible for the patient to return to his or her usual daily activities. In the literature, there is an association between early mobilization and a higher level of functional ability.28–30 It is possible to improve the short-term functional level even among demented patients with hip fracture.5 Early mobilization in the frail elderly individuals may be complicated by surgical complications and competing diseases.28 A difference in early functional recovery after hip fracture was not demonstrated between our 2 groups. That may be due to a similar early mobilization program by the GO team’s physiotherapist or due to the MBI data of the 2 groups being measured by 2 different physiotherapists and no inter-rater reliability was tested. The lower mortality may also lead to a higher number of patients with a low level of physical function in the tailor-made intervention group. A study found that a higher hemoglobin level was associated with early functional recovery after hip fracture.33 In our study, the postoperative hemoglobin levels were similar in both the groups.
Data are complete. All hospital-admitted residents were included and followed through the entire study period or until death. The data were collected prospectively so that few data were missing. Limitations of this study are the use of cohorts allocated in 2 periods rather than 2 concurrent groups. The groups are small and the results of the statistical comparisons can be misleading. However, the confidence intervals of the estimates are relatively narrow.
In conclusion, the concept “early discharge—hospital-at-home” would be applicable to the frail and elderly orthopedic patients as well.27 In-hospital intervention followed by a tailor-made hospital-at-home intervention in the acute phase is relevant in enhancing the quality of health care. Intervention performed immediately after discharge by a multidisciplinary GO team appeared to have a positive impact on short-term mortality and acute readmission. It should be further examined to make clear which parts of the comprehensive intervention are the most crucial. Prolongation of life is not necessarily the most relevant outcome in nursing home residents.34 Ethically, it would be relevant to study whether quality of life is improved in the frail elderly individuals along with improved survival.
Acknowledgment
The authors thank Anna Krogshede and Faranak Almasi (physiotherapists) and Inge Østergaard Holm-Petersen (nurse) of the geriatric orthopaedic team, who made this study possible.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Beck AM, Damkjær K, Schroll M. The care requirements of residents in Danish nursing homes [in Danish]. Ugeskr Laeger. 2008;170(9):749–752 [PubMed] [Google Scholar]
- 2. Gregersen M, Jensen NC, Mørch MM, Damsgaard EM. The effect of geriatric intervention in the rehabilitation of elderly patients with hip fracture [in Danish]. Ugeskr Laeger. 2009;171(46):3336–3340 [PubMed] [Google Scholar]
- 3. Gregersen M, Zintchouk D, Damsgaard EM, et al. Interdisciplinary geriatric intervention among nursing home residents with hip fracture reduces mortality [in Danish]. Ugeskr Laeger. 2010;172(25):1902–1907 [PubMed] [Google Scholar]
- 4. Foss NB, Kehlet H. Mortality analysis in hip fracture patients: implications for design of future outcome trials. Br J Anaesth. 2005;94(1):24–29 [DOI] [PubMed] [Google Scholar]
- 5. Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(9):1476–1482 [DOI] [PubMed] [Google Scholar]
- 6. Stott DJ, Buttery AK, Bowman A, et al. Comprehensive geriatric assessment and home-based rehabilitation for elderly people with a history of recurrent non-elective hospital admissions. Age Ageing. 2006;35(5):487–491 [DOI] [PubMed] [Google Scholar]
- 7. Elliot JR, Wilkinson TJ, Hanger HC, et al. The added effectiveness of early geriatrician involvement on acute orthopaedic wards to orthogeriatric rehabilitation. N Z Med J. 1996;109(1017):72–73 [PubMed] [Google Scholar]
- 8. Kennie DC, Reid J, Richardson IR, Kiamari AA, Kelt C. Effectiveness of geriatric rehabilitative care after fractures of the proximal femur in elderly women: a randomised clinical trial. BMJ. 1988;297(6656):1083–1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huusko TM, Karppi P, Avikainen V, Kautiainen H, Sulkava R. Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: subgroup analysis of patients with dementia. BMJ. 2000;321(7269):1107–1111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Handoll HHG, Cameron ID, Mak JCS, Finnegan TP. Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev. 2009;(4):CD007125. doi: 10.1002/14651858.CD007125.pub2 [DOI] [PubMed] [Google Scholar]
- 11. Gilchrist WJ, Newman RJ, Hamblen DL, Williams BO. Prospective randomised study of an orthopaedic geriatric inpatient service. BMJ. 1988;297(6656):1116–1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Adunsky A, Lusky A, Arad M, Heruti RJ. A comparative study of rehabilitation outcomes of elderly hip fracture patients: the advantage of a comprehensive orthogeriatric approach. J Gerontol A Biol Sci Med Sci. 2003;58(6):542–547 [DOI] [PubMed] [Google Scholar]
- 13. Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56(7):1349–1356 [DOI] [PubMed] [Google Scholar]
- 14. Thwaites JH, Mann F, Gilchrist N, Frampton C, Rothwell A, Sainsbury R. Shared care between geriatricians and orthopaedic surgeons as a model of care for older patients with hip fractures. N Z Med J. 2005;118(1214):U1438. [PubMed] [Google Scholar]
- 15. Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF., Sr. Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv. 2005;14(1):27–31 [PubMed] [Google Scholar]
- 16. González-Montalvo JI, Alarcón T, Mauleón JL, Gil-Garay E, Gotor P, Martín-Vega A. The orthogeriatric unit for acute patients: a new model of care that improves efficiency in the management of patients with hip fracture. Hip Int. 2010;20(2):229–235 [DOI] [PubMed] [Google Scholar]
- 17. Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20(3):172–178 [DOI] [PubMed] [Google Scholar]
- 18. Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged geriatric fracture center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717 [DOI] [PubMed] [Google Scholar]
- 19. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–522 [DOI] [PubMed] [Google Scholar]
- 20. Lundström M, Edlund A, Karlsson S, Brännström B, Bucht G, Gustafson Y. A multifactorial intervention program reduces the duration of delirium, length of hospitalization, and mortality in delirious patients. J Am Geriatr Soc. 2005;53(4):622–628 [DOI] [PubMed] [Google Scholar]
- 21. González-Montalvo JI, Alarcón T, Mauleón JL, Gil-Garay E, Gotor P, Martín-Vega A. The orthogeriatric unit for acute patients: a new model of care that improves efficiency in the management of patients with hip fracture. Hip Int. 2010;20(2):229–235 [DOI] [PubMed] [Google Scholar]
- 22. Adams AL, Schiff MA, Koepsell TD, et al. Physician consultation, multidisciplinary care, and 1-year mortality in medicare recipients hospitalized with hip an lower extremity injuries. J Am Geriatr Soc. 2010;58(10):1835–1842 [DOI] [PubMed] [Google Scholar]
- 23. Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993;342(8878):1032–1036 [DOI] [PubMed] [Google Scholar]
- 24. Milisen K, Foreman MD, Abraham IL, et al. A nurse-led interdisciplinary intervention program for delirium in elderly hip-fracture patients. J Am Geriatr Soc. 2001;49(5):523–532 [DOI] [PubMed] [Google Scholar]
- 25. Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department—the DEED II study. J Am Geriatr Soc. 2004;52(9):1417–1423 [DOI] [PubMed] [Google Scholar]
- 26. Siddiqi N, Holt R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev. 2007;(2): CD005563. doi: 10.1002/14651858.CD005563.pub2 [DOI] [PubMed] [Google Scholar]
- 27. Shepperd S, Doll H, Broad J, et al. Early discharge hospital at home. Cochrane Database Syst Rev. 2009;(1):CD000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. The Danish Orthopaedic Society Reference program for hip fracture. http://www.ortopaedi.dk/fileadmin/referennceprogram/Referenceprogram%2520for%2520patienter%2520med%2520hoftebrud%25202008.pdf Accessed April 2011
- 29. Rasmussen S, Kristensen BB, Foldager S, Myhrmann L, Kehlet H. Accelerated recovery program after hip fracture surgery [in Danish]. Ugeskr Laeger. 2002;165(1):29–33 [PubMed] [Google Scholar]
- 30. Kirkwood BR, Sterne JAC. Essential Medical Statistics. 2nd ed Malden, Mass: Blackwell Science; 2003 [Google Scholar]
- 31. Lauridsen UB, de la Cour BBD, Gottschalck L, Svensson BH. Intensive physical therapy after trochanteric femoral fracture. A randomized clinical trial [in Danish]. Ugeskr Laeger. 2002;164(8):1040–1044 [PubMed] [Google Scholar]
- 32. Halm EA, Wang JJ, Boockvar K, Penrod J, et al. Effects of blood transfusion on clinical and functional outcomes in patients with hip fracture. Transfusion. 2003;43(10):1358–1365 [DOI] [PubMed] [Google Scholar]
- 33. Lawrence VA, Silverstein JH, Cornell JE, Pederson T, Noveck H, Carson JL. Higher Hb level is associated with better early functional recovery after hip fracture repair. Transfusion. 2003;43(12):1717–1722 [DOI] [PubMed] [Google Scholar]
- 34. Kuo HK, Scandrett KG, Dave J, Mitchell SL. The influence of outpatient comprehensive geriatric assessment on survival: a meta-analysis. Arch Gerontol Geriatr. 2004;39(3):245–254 [DOI] [PubMed] [Google Scholar]