Abstract
Background. The UK population is ageing with the largest increase expected to occur in people aged more than 85 years (85+). We have examined the hypothesis that neck of femur (NOF) fractures in the 85+ group exhibit demonstrable key outcome measurement differences after surgery when compared to a standard NOF population. Patients and Methods. A prospective observational cohort study of the demographics, clinical features, and key clinical outcome measurements for 2 groups of patients (65-84 and 85+ years of age at presentation) was performed in a single trauma unit over a 3-year period. Results. A total of 699 patients with a median age of 78 in the 65 to 84 cohort were compared with 523 patients with a median age of 88 in the 85+ cohort. Despite a dedicated orthogeriatric service and no difference in time to surgery between the 2 groups, the 30-day and 1-year mortality rates were significantly higher in the 85+ cohort at 10% and 30%, respectively, compared with 5% and 19% in the younger patient group. In our 85+ group, 34% had evidence of significant measured cognitive impairment compared to only 19% in the 65 to 84 group (P < .001). The length of hospital inpatient stay was also longer in the 85+ cohort with a median of 20 days compared to 16 days in the younger cohort (P = .001). In the 85+ cohort, 60% of patients were discharged back to their usual (preinjury) place of residence compared to 72% in the 65 to 84 cohort (P = .001). Conclusions. Patients in 85+ group presenting with an NOF fracture represent a unique high-risk patient group. Despite adherence to published key principles of care, this group is at higher risk and as such merits focused clinical attention, with adequate patient and family member counseling with regard to prognosis and overall expectation.
Keywords: neck of femur fracture, elderly, outcome
Introduction
Over the past 25 years, the UK population aged over 65 has increased by approximately 1.7 million, with the largest change occurring in people aged over 85 years (85+). This population subgroup1 has doubled in number from 660 000 in 1984 to 1.4 million in 2009. The trend is expected to continue with population estimates of around 3.5 million in the 85+ cohort by 2034. This group will then represent approximately 5% of the population. Previous work has identified unique and challenging medical issues within this population.2 These include high levels of comorbidity, increased incidence of hospital admission, functional impairment, and social isolation. An increasing burden upon future medical services is expected.
Fractured neck of femur (NOF) remains the second leading cause of hospital admission in elderly patients.3 There remains a paucity of information on prognostic clinical factors influencing outcome in this at risk subset of patients. Previous work has examined the burden of comorbidity and general health of this age group in community studies.2 We have examined the hypothesis that NOF fractures in the patient subgroup aged 85+ will have both a different preinjury disease profile and have measurable differences in outcome after surgery, when compared to a standard NOF population. These differences may highlight areas for future improvement and focus in order to improve the delivery of care.
Patients and Methods
This study examined the demographics, inpatient characteristics, and outcome for all patients aged over 65 years presenting to a single trauma unit between June 2006 and June 2009. We have performed a detailed analysis of this prospectively collected data. Patients were arbitrarily divided into 2 groups, 65 to 84 years and over 85 (85+) on admission for the purposes of comparison. Data were collected to allow for analysis of patient demographics, preoperative clinical factors that may affect outcome (cognitive impairment and incidence of medical comorbidity), operative factors (eg, delay to surgery), and patient outcome after surgery (mortality rate, length of hospital stay, and discharge destination). Comorbidity was classified using the Charlson comorbidity index.4 This scoring system has previously been validated and used in several different population groups.5,6 The index predicts 1-year mortality for patients with a range of comorbidities. Evidence of cognitive impairment was coded between unspecified dementia, Alzheimer disease, vascular dementia, and dementia secondary to Parkinson disease. Specific data on comorbidity and cognitive impairment were obtained retrospectively from the medical notes. These data were validated by the Coding Service based at Newcastle upon Tyne Hospitals NHS Foundation Trust. Validation involved using the current approved coding guidelines to assign and sequence correct diagnosis and procedure codes for hospital inpatient services. All information was obtained directly from the patient’s medical records.
The data was then captured by the Information Service, Newcastle upon Tyne Hospitals NHS Foundation Trust and presented in an excel spread sheet. The study had Caldicott approval from the Research and Development department of Newcastle upon Tyne Hospitals NHS Foundation Trust.
Data was analyzed using direct numerical and percentage comparisons and with SPSS software package version 11.0 (SPSS Inc, Chicago, Illinois) and was expressed as a median with interquartile range (IQR). A nonparametric (Mann-Whitney) test was used to compare relevant continuous measurements between groups. Categorical data between our 2 cohorts were expressed as frequencies and compared using the chi-square test with the Fisher exact test. For all analyses, a P value of .05 or less was considered significant.
Results
Patient Demographics
The demographics of both patient cohorts are given in Table 1 . There were a higher relative proportion of female patients in the 85+ cohort. Socioeconomic class defined as a range from I (professional) to V (unskilled) was analyzed and both groups had similar numbers at presentation, for each category. A lower proportion of patients belonging to our highest social class (I) (professional) occurred in the 85+ group. The distribution is demonstrated in Figure 1 .
Table 1.
Patient Demographics
| 65-84 Years | 85+ | |
|---|---|---|
| Patient numbers | 699 | 523 |
| Age, median (interquatile range, IQR) | 78 (7) | 88 (6) |
| Male:female (%) | 30%:70% | 22%:78% |
| Fracture type (%); intracapsular:extracapsular | 52%:48% | 51%:49% |
Figure 1.
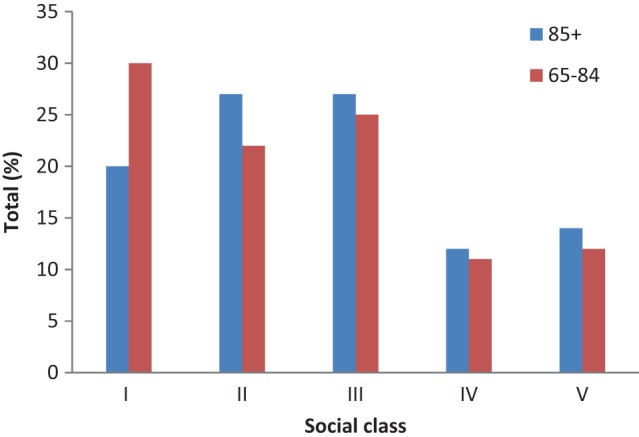
Social class of patients admitted with fractured neck of femur.
Comorbidity
The median (IQR) Charlson comorbidity score was significantly (P < .01) higher in the 85+ group compared to the 65 to 84 cohort with a median (IQR) score of 2 (2) versus 1 (3). The results showed an obvious skew with only 20 (4%) of 523 patients in our 85+ cohort scoring 0 in the Charlson comorbidity index compared to 185 (25%) of 699 patients in the younger 65 to 84 group.
Cognitive Function
Of 523 patients in our 85+ group, 180 (34%) had evidence of significant measured cognitive impairment compared to 129 (19%) of 699 patients, in the younger cohort (P < .001). The incidence of Alzheimer disease, vascular and Parkinsonian dementia appeared similar, however there was a higher incidence of “unspecified” dementia (19% vs 6%), in our older patient cohort. We also analyzed the relationship between documented cognitive impairment in our entire patient cohort and the length of hospital stay. The median length of hospital stay in the 309 patients who had cognitive impairment was 17 (IQR = 27) days. This was compared to 17 (IQR = 17) in the 912 patients who did not have cognitive impairment. These figures were not significantly different (P = .13). The 30-day and 1-year mortality rates were significantly higher in our cognitively impaired group. The results are demonstrated in Table 2 .
Table 2.
Cognitive Impairment and Mortality Rates
| Cognitive Impairment | No Cognitive Impairment | P Value | |
|---|---|---|---|
| 30-day mortality | 45/309 (14.6%) | 41/912 (4.5%) | P < .001 |
| 1-year mortality | 102/309 (33%) | 185/912 (20.3%) | P < .001 |
Time to Surgery
Of the 85+ cohort, 74% underwent surgery for their fractured NOF within 48 hours of admission. This compared to 78% in the younger cohort and was not significantly different (P = .12).
Length of Hospital Stay
The length of hospital inpatient stay was significantly longer in our 85+ age group with a median (IQR) of 20 (31) days compared to 16 (19) days in the younger cohort (P = .001). In addition, 87 patients (17%) required a hospital stay of longer than 50 days after surgery compared to only 61 patients (9%) in the 65- to 84-year group (P < .001).
Mortality Rate
A 30-day mortality rate in the 85+ group of 53 patients (10%) was demonstrated. This was significantly (P = .001) higher compared to only 36 patients (5%) in the 65- to 84-year cohort. Inpatient mortality rose to 80 (15%) of 523 in the 85+ group compared to 67 (9.6%) of 699 in the younger cohort (P = .003). One-year mortality in the 85+ cohort consisted of 157 patients (30%) compared to 130 (19%) patients in the 65- to 84-year group (P < .001).
Discharge Destination
In the 85+ cohort, 316 patients (60%) admitted with a fractured NOF were discharged back to their usual (preinjury) place of residence. This is compared to 508 patients (72%) in the 65- to 84-year cohort (P = .001). In addition, 127 patients (24%) of the 85+ group failed to return home and required discharge to a care facility (rehabilitation ward, local authority residence, or non-NHS residential/nursing care). This is compared to only 123 patients (17%) in the 65- to 84-year cohort (P = .001).
Discussion
The study has highlighted the unique challenges in the management of patients aged 85+ presenting with a fractured NOF. We found a higher 30-day and 1-year mortality rate, a higher incidence of comorbidity and cognitive impairment, and an increased inpatient hospital stay. In addition, our older patient cohort had less chance of being discharged back to their usual (preinjury) place of residence and a higher proportion required discharge to a care facility such as a rehabilitation ward, local authority residence, or non-NHS residential/nursing care. This was despite equivalent attempts to achieve early surgical intervention with no apparent prolonged delay to theater, as a direct result of being in the 85+ category.
Length of hospital stay after surgery is often seen as a key outcome measurement in the effective management of NOF fractures. Various studies have identified that increasing age in NOF patients is associated with prolonged hospital admission.7–9 This present study supports these findings with 17% of the 85+ population requiring a hospital admission of longer than 50 days. Lawrence et al10 analyzed 100 consecutive patients admitted to a single orthopedic trauma unit in 2003. The mean length of hospital stay was 23 days, at an average cost of £12 163 pounds per patient; 84% of the costs were attributed to the ward and length of inpatient stay. The economic impact of a prolonged hospital stay after NOF fracture was emphasized. There is a need to focus on effective methods to minimize this in future years. Hollingworth et al11 emphasized the economic benefits of an early supportive discharge scheme that reduced inpatient stay by an average of 9 days. The significant savings calculated were proportional to the reduction in the length of hospital stay; 40% of patients were judged suitable for this scheme, which reduced costs, despite a higher readmission rate. Length of hospital stay depends on the availability of early rehabilitation support services, continuing care beds, care services in the community, and patient family support. Our study has demonstrated the potential financial implications of an expanding 85+ subgroup and the need to focus on effective efforts to minimize hospital stay in order to optimize cost-efficiency.
Significant morbidity can often be expected following a fractured NOF injury, including a loss in mobility and independence. Approximately 50% of the elderly patients are unable to mobilize independently after a hip fracture.3 Resultantly, discharge destination is also often seen as a key outcome measurement in the effective management of NOF fractures. Deakin et al demonstrated that preinjury dependence, increasing age, male sex, and injury sustained while in hospital were all associated with discharge to an alternative location.12 Another study by Cree et al analyzed 304 patients with a fractured NOF who were residing at home before injury.13 The study identified that increasing age, dementia, and low levels of activities of daily living contributed to these patient’s failing to return to the community and thus requiring institutionalized care. In this present study, our 85+ group appear to experience a higher incidence of cognitive impairment, greater loss of independence, and require greater levels of care after this injury when compared to the younger cohort. This supports the findings of previously well-published clinical studies that conclude that increasing age in the NOF patients often represents a permanent loss of independent living and mobility.14–16 In addition, this present study demonstrates the link between cognitive impairment and failure to discharge back to usual preinjury place of residence in the 85+ population.
Recent British Orthopaedics Association (BOA) and British Geriatric Society (BGS) guidelines in collaboration with the National Hip Fracture Database (NHFD) recommend that all patients with hip fracture who are medically fit should have surgery within 48 hours of admission.17,18 Mortality rates appear to improve if surgery is performed within 48 hours of hospital admission.19 Parker et al identified that a delay in surgery of more than 48 hours significantly increased the patient’s length of hospital stay and increased the patient’s risk of morbidity after surgery.20 Barclay et al identified that early surgical intervention after fracture NOF is associated with reduced risk of mortality and morbidity in older patients. Moran et al found that a delay of more than 4 days in surgery resulted in a significant increase in mortality.21 However, mortality was not increased when surgery was delayed up to 4 days; 26% of our more than 85 years population and 22% of the younger cohort were not operated within 48 hours. This does not comply with national recommendations and may impact other key outcome measurements after injury, but there was no evidence that being in the 85+ group predisposed to a delay in surgery. It is possible that time to surgery may well be of limited value when predicting successful outcome following fracture NOF injury.
This present study demonstrated a 30-day mortality rate in our 85+ cohort, which was twice as high as the measured rate in our younger group (10% vs 5%). One-year mortality was also significantly higher (30% vs 19%). Documented risk factors for mortality after an NOF fracture include, advanced age, male gender, living in an institution, and cognitive impairment. Roche et al identified a 30-day mortality rate of 9% for fractured NOF patients.22 This study highlighted that postoperative complications such as chest infection and cardiac failure were associated with higher rates of mortality. Increasing age, male sex, and the presence of 3 or more comorbidities predicted an increased mortality risk. Our 85+ group had a higher incidence of comorbidity as demonstrated by the Charlson index of comorbidity scores and a higher incidence of cognitive impairment. Holt et al demonstrated that the extremely elderly patients had higher ASA scores and thus a poorer preinjury health status when studying a prospective group of patients from a large Scottish Registry.15 Moran et al demonstrated that patients with comorbidities and delayed fracture fixation surgery had 2.5 times the risk of death within 30 days after surgery when compared to those with no comorbidities.21 Optimizing elderly patients prior to surgery, preventing postoperative complications, and providing specialist medical and geriatric input are key factors in an effort to improve patient outcome.23
Strength of this study is the method of data collection, which was performed prospectively in an independent and neutral fashion, from a single trauma unit serving a well-defined and typical catchment population. The retrospective nature of our analysis could have introduced an observer bias and can be considered a study weakness. However, we feel that the outcome measurements that we used are relevant and consistent with much of the previously published literature. Some unique and relevant findings have been identified in the more than 85-year cohort.
In conclusion, this work strongly identifies that the 85+ fractured NOF population may represent a subset of patients who require focused consideration in the future to plan a tailored management program, thereby optimizing care and ultimately outcome.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research and/or authorship of this article.
References
- 1.Office for National Statistics, Population—Ageing, fastest increase in the ‘oldest old’, author. http://www.statistics.gov.uk/cci/nugget.asp?id=949 Accessed November 12, 2010.
- 2. Collerton J, Barrass K, Bond J, et al. The Newcastle 85+ study: biological, clinical and psychosocial factors associated with healthy ageing: study protocol. BMC Geriatr. 2007;7:14 doi:10.1186/1471-2318-7-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnell O. The socioeconomic burden of fractures: today and in the 21st centuary. Am J Med. 1997;103(2A):20S–25S [DOI] [PubMed] [Google Scholar]
- 4. Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383 [DOI] [PubMed] [Google Scholar]
- 5. Johnsen SP, Sorensen HT, Lucht U, Soballe K, Overgaard S, Pedersen AB. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. J Bone Joint Surg (Br). 2006;88(10):1303–1308 [DOI] [PubMed] [Google Scholar]
- 6. Rina Jain, Antoni Basinski, Hans J. Kreder Nonoperative treatment of hip fractures. Int Orthop. 2003;26(1):11–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jensen JS, Bagger J. Long term social prognosis after hip fractures. Acta Orthop Scand. 1982;53(1):97–101 [DOI] [PubMed] [Google Scholar]
- 8. Jette AM, Harris BA, Cleary PD, Campion EW. Functional recovery after hip fracture. Arch Phys Med and Rehab. 1987;68(10):735–740 [PubMed] [Google Scholar]
- 9. Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture; A prospective study. J Gerontol. 1990;45(3):M101–M107 [DOI] [PubMed] [Google Scholar]
- 10. Lawrence TM, White CT, Wenn R, Moran CG. The current hospital costs of treating hip fractures. Injury. 2005;36(1):88–91 [DOI] [PubMed] [Google Scholar]
- 11. Hollingworth W, Todd C, Parker M, Roberts JA, Williams R. Cost analysis of early discharge after hip fracture. BMJ. 1993;307(6909):903–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Deakin DE, Wenn RT, Moran CG. Factors influencing discharge location following hip fracture. Injury. 2008;39(2):213–218 [DOI] [PubMed] [Google Scholar]
- 13. Cree AK, Nade S. How to predict return to the community after fractured proximal femur in the elderly. Aust NZ J Surg. 1999;69(10):723–725 [DOI] [PubMed] [Google Scholar]
- 14. Borkan JM, Quirk M, Sullivan M. Finding Meaning after the Fall. Injury Narratives From Elderly patients. Soc Sci Med. 1991;33(8):947–957 [DOI] [PubMed] [Google Scholar]
- 15. Holt G, Smith R, Duncan K, Hutchison JD, Gregori A. Outcome after surgery for the treatment of hip fracture in the extremely elderly. J Bone Joint Surg Am. 2008;90(9):1899–1905 [DOI] [PubMed] [Google Scholar]
- 16. Lyons AR. Clinical outcomes and Treatment in Hip fractures. Am Js Med. 1997;103(2 suppl 1):s51–s64 [DOI] [PubMed] [Google Scholar]
- 17. BOA/BGS Blue Book The care of patients with fragility fractures, September 2007. Page 21 – Standard 2, NHFD Fields 1.04 and 4.01 Page 39 – Standard 4, NHFD field 4 www.fractures.com/pdf/BOA-BGS-Blue-Book.pdf Accessed October 14, 2010
- 18.National Hip Fracture Database, author. http://www.nhfd.co.uk/ Accessed October 15, 2010.
- 19. Bottle A, Aylin P. Mortality associated with delay in operation after hip fracture: observational study. BMJ. 2006;332(7547):947–951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Parker MJ, Pryor GA. The timing of surgery for proximal femoral fractures. J Bone Joint Surg Br. 1992;74(2):203–205 [DOI] [PubMed] [Google Scholar]
- 21. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important?. J Bone Joint Surg Am. 2005;87(3):483–489 [DOI] [PubMed] [Google Scholar]
- 22. Roche JJW, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Scottish Intercollegiate Guidelines Network 111–Management of hip fracture in older people A national clinical guideline Edinburgh: Scottish Intercollegiate Guidelines Network, 2009. www.sign.ac.uk/pdf/sign111.pdf Accessed October 14, 2010


