Abstract
Background
Plaque psoriasis is a chronic disease characterized by scaly plaques on the skin that can itch and bleed. Psoriasis covering over 10% of the body is classified as moderate to severe, and can impact patient quality of life.
Objectives
To assess the relationship between plaque psoriasis self-reported severity symptoms and health-related quality of life, work productivity, and activity impairment among patients with moderate-to-severe psoriasis.
Methods
The study sample included 199 patients recruited from internet panels, of which 179 respondents had plaque psoriasis and 20 had plaque and inverse psoriasis. Itching, pain, and scaling symptoms were studied. A structural equation modeling framework was used to estimate the effect of these symptoms on patient outcomes. First, each severity variable was regressed on a set of covariates to generate a predicted severity score. These predicted values were placed in a second-stage model with patient mental and physical scores (Short-Form 12 questionnaire), work productivity, and activity impairment indicators as dependent variables.
Results
Itching severity had a marginal negative effect (P < 0.06) on patients’ Short-Form 12 physical and mental component scores. Pain severity also negatively affected physical and mental health scores (P < 0.02). Patients were more likely to miss work because of itching (odds ratio [OR]: 2.31, 95% confidence interval [CI]: 1.30, 4.10), pain (OR: 1.78, 95% CI: 1.25, 2.52), and scaling (OR: 2.15, 95% CI: 1.31, 3.52) symptoms. These symptoms also lowered self-reported productivity. As itching (OR: 1.74, 95% CI: 1.03, 2.95), scaling (OR: 1.84, 95% CI: 1.16, 2.90), and pain symptoms (OR: 1.53, 95% CI: 1.12, 2.09) increased, so did the odds that a patient would be less productive at work.
Conclusion
Plaque psoriasis significantly affects patient quality of life. In addition to greater mental and physical pain, patients are more likely to miss work and have diminished productivity as symptom severity increases.
Keywords: psoriasis, severity, activity impairment, work productivity loss, structural equation modeling
Introduction
Psoriasis is a chronic, systemic, inflammatory disease characterized by erythematous, scaly plaques on the skin that can itch and bleed. It is the most prevalent autoimmune disease in the United States, affecting approximately 7.5 million, or 2.2%, of the US population.1 There are five different types of psoriasis, with the most common type being plaque psoriasis. Symptoms of plaque psoriasis include red and white scaly patches that can appear on any part of the body. In most cases, these symptoms are mild and cover less than 3% of the body. However, for a small subset of individuals (8% of psoriasis patients), psoriasis can cover over 10% of the skin and is classified as severe.2 Severe psoriasis can have a major impact on patient quality of life.
Individuals with severe psoriasis may experience extreme discomfort (eg, burning, stinging, itching, pain, cracking of the skin). In 2008, the National Psoriasis Foundation surveyed 426 individuals suffering from psoriasis, of which 71% reported that psoriasis had a significant effect on their everyday quality of life.2 Other studies have compared the impact of extreme psoriasis to diseases such as cancer, arthritis, hypertension, heart disease, diabetes, and depression.3
A variety of treatments are available to control the symptoms of psoriasis. However, psoriasis is a lifelong condition with symptoms appearing and disappearing intermittently throughout a patient’s life. Currently, most clinical trials do not collect data on common psoriasis symptoms such as itching, stinging, and burning, which, though subjective, can have a major effect on patients’ personal and professional lives. Further study of the relationship between psoriasis symptom severity and health-related quality of life is an important step to clarify patient-centered end points to optimize treatment.
Methods
A retrospective analysis was performed using cross-sectional survey data collected from 199 patients. Participants were recruited from internet panels maintained by Lightspeed Research and partners. Potential respondents were identified through the 2009 US National Health and Wellness Survey. Respondents were included if they reported having plaque psoriasis, or both plaque and inverse psoriasis, affecting at least 10% of their bodies, using the area of one palm to represent 1% of body surface area.
Patients’ demographic characteristics, including sex, age, employment type (full time or not), and work environment (business office or not), were captured in the survey. Clinical characteristics collected include comorbidities, body mass index, psoriasis symptoms, total number of body locations affected by psoriasis, frequency and trigger of flare-ups, season with most flare-ups, skin color, and current psoriasis treatment.
Short-Form 12 health status instrument total, mental, and physical components
The Short-Form 12 (SF-12) instrument was derived from the longer SF-36 to measure self-reported health-related quality of life and contains two summary components: the physical component score (PCS) and the mental component score (MCS). The PCS4 and the MCS are composite scores generated based on answers to a variety of physical and mental health questions, respectively, and have a scale from 0 to 100, with higher scores indicating better physical or mental health. Scores in this dataset range from 30 to 70. In the US general population, the average PCS is 49.63, and the average MCS is 49.37.
Work productivity and activity impairment
In the survey, there were four items related to work activity and performance: absenteeism, work missed for other reasons, overall work impairment, and activity impairment. All questions were coded as binary variables.
During the past 7 days, how many hours did you miss from work because of problems associated with your psoriasis? (>0 hours = yes; 0 hours = no)
During the past 7 days, how many hours did you miss from work because of any other reason, such as vacation, holidays, time off to participate in this study? (>0 hours = yes; 0 hours = no)
During the past 7 days, how much did your psoriasis affect your productivity while you were working? (none = 1; some = 0)
During the past 7 days, how much did your psoriasis affect your ability to do your regular daily activities, other than work at a job? (none = 1; some = 0)
Statistical analysis
All study variables, including outcome measures, were analyzed descriptively. Descriptive tables were prepared for the entire sample (n = 199). Numbers and percentages were provided for dichotomous and polychotomous variables. Means and standard deviations (SDs) were provided for continuous variables.
Clinical covariates were divided into two types: covariates for adjustment and psoriasis severity predictor variables. The following clinical covariates were created: comorbidities (no comorbidities, one to two comorbidities, more than two comorbidities), body mass index (underweight, normal, overweight, and obese), total number of body locations (includes scalp, face, neck, shoulders, chest, upper arms, lower arms, elbows, back of hands, palms, nails, genitals, buttocks, back, upper legs, lower legs, knees, soles of feet, top of feet, other) affected by psoriasis (over ten body locations versus under ten body locations), psoriasis symptoms (blisters, cracked skin, dry skin, fatigue, itching, inflammation, lesions, pain, redness, scaling, shedding of skin, skin bleeding, swollen/stiff joints, tenderness/soreness, thickened/pitted or rigid nails, other), frequency of flare-ups (patients with and without continuous flare-ups), triggers of flare-ups (cold or dry weather, stress, other [humidity, food, alcohol], none), season with the most flare-ups (winter, other), skin color (pink, light red/brown, bright red/purple, deep dark red/purple/brown, grey/white/silver), and current treatment (topical steroids, other topical medications, oral medications, phototherapy, biologics, over-the-counter medications).
Three symptom severity predictor variables were calculated, including itching (0 = no itching to 10 = itching as bad as you can imagine), pain (0 = no pain to 10 = pain as bad as you can imagine), and scaling (0 = no scaling/flaking to 10 = scaling/flaking as bad as you can imagine). In addition, two categories of outcome variables were created: SF-12 health status instrument total, including mental and physical components, and work productivity and activity impairment.
Structural equation modeling (SEM) provides a framework for statistical analysis that includes multivariate procedures, and has been used in other research to assess latent constructs such as mental and physical health status using SF-12 score measurements.5,6 In this study, SEM was used to estimate the effect of psoriasis symptom severity on patient outcomes. In the first stage, each symptom severity variable was regressed on all clinical covariates to generate a predicted symptom severity score. These predicted values were then placed in a second-stage model (ordinary least squares and logistic models) with patient mental and physical scores (SF-12) as continuous dependent variables, and work productivity and activity impairment as binary dependent variables (1 = none; 0 = some activity impairment). Sex, age, overweight, obese, having one to two comorbidities, over two comorbidities, full-time worker, work in business environment, more than ten body locations, and continuous flare-up factors were also controlled in the second-stage model. A path diagram helps illustrate the hypothesized causal relationships between the variables (Figure 1). The independent variables (X1, X2) are related to both response variables: severity and outcome. In addition, severity itself is a predictor in explaining outcome. The two circles represent the unobservable error terms in each model. Error terms are assumed to be independent, because the relationship between outcome and severity is nonreciprocal.
Figure 1.
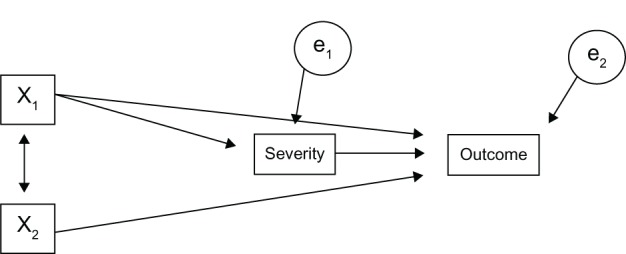
Path diagram of hypothesized causal relationships.
The bootstrap method was used to estimate the effect of severity predictor variables on the outcome in a distribution-independent manner. Through the process of sampling with replacement, bootstrapping has been recommended to provide estimations for small population sizes.7,8 The statistical procedure was performed using STATA v11 software (Stata-Corp LP, College Station, TX, USA) with 100 replications.
Results
Demographic characteristics
After applying the inclusion and exclusion criteria, 179 respondents reported having plaque psoriasis only, and 20 reported having both plaque and inverse psoriasis. The majority of patients were female (58.79%). The mean age was 48 years, and 60.80% of patients were not employed full time. The majority of patients did not miss any work as a result of psoriasis (75.45%). They did, however, have some work (64.95%) and activity (72.36%) impairment due to the disease. The severity measure with the highest score was scaling at 5.61 (SD = 2.70). Pain had the lowest level of severity at 3.92 (SD = 2.94) (Table 1).
Table 1.
Demographic, SF-12, and WPAI Characteristics
| Total sample size (n = 199)
|
||
|---|---|---|
| n/mean | %/SD | |
| Sex | ||
| Male | 82 | 41.21% |
| Female | 117 | 58.79% |
| Age (years) | 48.48 | 13.26 |
| Comorbidities | ||
| None | 23 | 11.56% |
| 1 to 2 | 127 | 63.82% |
| Over 2 | 49 | 24.62% |
| Employment type | ||
| Full time | 78 | 39.20% |
| Not full time | 121 | 60.80% |
| BMI | ||
| Underweight | 6 | 3.09% |
| Normal weight | 45 | 23.20% |
| Overweight | 55 | 28.35% |
| Obese | 88 | 45.36% |
| Work environment | ||
| Business office | 40 | 20.10% |
| Not business office | 159 | 79.90% |
| SF-12 total | ||
| Physical component score (range: 30–70) | 43.58 | 11.99 |
| Mental component score (range: 30–70) | 42.15 | 12.54 |
| Severity measures | ||
| Severity of itching (range: 0–10) | 5.13 | 2.56 |
| Severity of pain (range: 0–10) | 3.92 | 2.94 |
| Severity of scaling (range: 0–10) | 5.61 | 2.7 |
| WPAI | ||
| Absenteeism | ||
| No hours missed | 83 | 75.45% |
| Some hours missed | 27 | 24.55% |
| Missed work for other reasons | ||
| No hours missed | 65 | 59.09% |
| Some hours missed | 45 | 40.91% |
| Overall work impairment | ||
| None | 34 | 35.05% |
| Some | 63 | 64.95% |
| Activity impairment | ||
| None | 55 | 27.64% |
| Some | 144 | 72.36% |
Abbreviations: BMI, body mass index; SD, standard deviation; SF-12, Short-Form 12 health survey; WPAI, work productivity and activity impairment.
Clinical characteristics and current treatment
Nearly one-third of patients (32.16%) had at least ten affected body locations (Table 2). The most common psoriasis symptom was scaling (88.94%), followed by itching (87.44%), dry skin (85.43%), and redness of skin (79.40%). Lesions (31.66%), blisters (12.56%), and other symptoms (1.51%) were less common in the study population. Roughly half of the respondents experienced continuous flare-ups (50.25%), and the majority (77.89%) had specific triggers for these flare-ups, including cold, dry weather (61.81%) and stress (60.80%).
Table 2.
Clinical characteristics and current treatment
| Total sample size (n = 199)
|
||
|---|---|---|
| n | % | |
| Total number of body locations with psoriasis | ||
| Less than 10 | 135 | 67.84% |
| Over 10 | 64 | 32.16% |
| Psoriasis symptoms | ||
| Blisters | 25 | 12.56% |
| Cracked skin | 130 | 65.33% |
| Dry skin | 170 | 85.43% |
| Fatigue | 72 | 36.18% |
| Itching | 174 | 87.44% |
| Inflammation | 122 | 61.31% |
| Lesions | 63 | 31.66% |
| Pain | 92 | 46.23% |
| Redness | 158 | 79.40% |
| Scaling | 177 | 88.94% |
| Shedding of skin | 137 | 68.84% |
| Skin bleeding | 96 | 48.24% |
| Swollen/stiff joints | 72 | 36.18% |
| Tenderness/soreness | 73 | 36.68% |
| Thickened/pitted/ridged nails | 87 | 43.72% |
| Other | 3 | 1.51% |
| Frequency of flare-ups | ||
| Continuous flare-ups | 100 | 50.25% |
| No continuous flare-ups | 99 | 49.75% |
| Triggers of flare-ups | ||
| Cold, dry weather | 123 | 61.81% |
| Stress | 121 | 60.80% |
| Other (humid, food, alcohol) | 76 | 38.19% |
| None | 44 | 22.11% |
| Season with most flare-ups | ||
| Winter | 156 | 78.39% |
| Not winter | 43 | 21.61% |
| Skin color | ||
| Pink | 54 | 27.14% |
| Light red or brown | 31 | 15.58% |
| Bright red or purple | 41 | 20.60% |
| Deep dark red, purple, or brown | 10 | 5.03% |
| Grey, white, or silver | 63 | 31.66% |
| Current treatment | ||
| Prescription topical steroids | ||
| Use topical steroids | 91 | 45.73% |
| Do not use topical steroids | 108 | 54.27% |
| Other prescription topical treatments | ||
| Use topical treatments | 25 | 12.56% |
| Do not use topical treatments | 174 | 87.44% |
| Prescription oral medications | ||
| Use oral medications | 23 | 11.56% |
| Do not use oral medications | 176 | 88.44% |
| Prescription injection/infusion medications (biologics) | ||
| Use biologics | 24 | 12.06% |
| Do not use biologics | 175 | 87.94% |
| Any OTC, nonprescription products (topical creams, shampoos, foams, moisturizers, coal tar, bath solutions [oatmeal, Epsom salts]) | ||
| Use OTC medications | 60 | 30.15% |
| Do not use OTC medications | 139 | 69.85% |
Abbreviations: OTC, over-the-counter medications; SD, standard deviation.
Although the majority of respondents were not prescribed the treatments listed in Table 2, a high proportion used topical steroids (45.73%) and over-the-counter medications (30.15%), compared with topical treatments (12.56%), biologics (12.06%), or oral medications (11.56%).
Outcome models
Bootstrapped results of the second-stage models are summarized in Table 3. Itching severity had a significant negative effect on patients’ SF-12 PCS (coefficient: −1.46, 95% confidence interval [CI]: −2.93, 0.01, P-value = 0.052). To correct for the small sample size (N = 179), the bootstrapping method was used to estimate the coefficients of all severity variables on the outcome. The bootstrapped P-values and CIs for the effect of itching severity on PCS were significant (coefficient: −1.49, 95% CI: −2.88, −0.11, P-value = 0.035). However, itching severity did not have a significant effect on patients’ SF-12 MCS (coefficient: −1.67, 95% CI: −3.40, 0.06, P-value = 0.058), even after bootstrapping. Pain severity had a significant negative effect on PCS (coefficient: −1.97, 95% CI: −2.89, −1.04, P-value < 0.001) and MCS (coefficient: −1.38, 95% CI: −2.46, −0.31, P-value = 0.012).
Table 3.
Second-stage ordinary least squares regression for Short-Form 12 component scores
| Variable | Coefficient | Standard error | Z | P > z | 95% confidence interval |
|---|---|---|---|---|---|
| Mental component score | |||||
| Severity of itching | −1.67 | 0.88 | −1.91 | 0.0580 | −3.40, −0.06 |
| Severity of pain | −1.38 | 0.55 | −2.53 | 0.0120 | −2.46, −0.31 |
| Severity of scaling | −0.04 | 0.78 | −0.05 | 0.9570 | −1.58, −1.49 |
| Physical component score | |||||
| Severity of itching | −1.46 | 0.75 | −1.95 | 0.0520 | −2.93, −0.01 |
| Severity of pain | −1.97 | 0.47 | −4.19 | <0.0001 | −2.89, −1.04 |
| Severity of scaling | −1.00 | 0.68 | −1.48 | 0.1410 | −2.34, −0.33 |
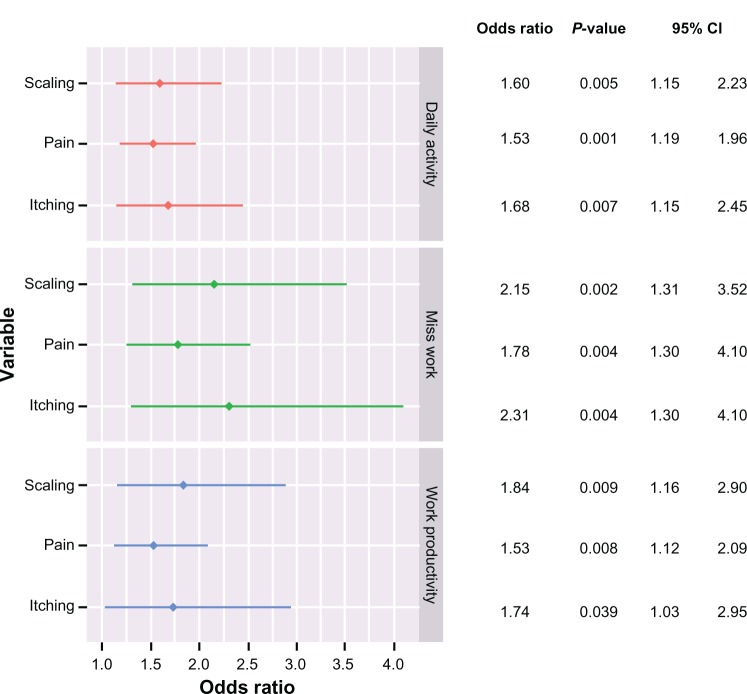
A second set of logistic models examined the binary work-related variables (Figure 2). Patients were significantly more likely to miss work with increasing severity of itching (odds ratio [OR]: 2.31, 95% CI: 1.30, 4.10, P-value = 0.004), pain (OR: 1.78, 95% CI: 1.25, 2.52, P-value = 0.001), and scaling (OR: 2.15, 95% CI: 1.31, 3.52, P-value = 0.002) symptoms. These symptoms also affected work productivity. More severe itching (OR: 1.74, 95% CI: 1.03, 2.95, P-value = 0.039), scaling (OR: 1.84, 95% CI: 1.16, 2.90, P-value = 0.009), and pain symptoms (OR: 1.53, 95% CI: 1.12, 2.09, P-value = 0.008) increased the odds that a patient would be less productive at work. Coefficients were of similar magnitude for symptoms affecting the performance of daily activities (Figure 2).
Figure 2.
Logistic regression for dependent variables: missing work, reduced work productivity, and difficulty performing daily activities due to psoriasis.
Note: All variables are statistically significant.
Abbreviation: CI, confidence interval.
Discussion
This study examined the effect of psoriasis symptoms on patients’ health-related quality of life and work productivity loss. Nearly all symptoms studied had a negative impact on patients’ well-being. For mental health variables, severity of pain and itching had statistically significant effects. The same outcomes were found for the physical health score. Other outcomes studied were work productivity, absenteeism, and the ability to perform daily activities. Scaling, pain, and itching severity measures were also negatively related to these three outcome variables. The largest effect sizes were associated with itching and scaling severity. As these severity levels increased, patients were more likely to miss work or be less productive performing work and daily activities. A recent study by Horn et al9 using patient-reported survey data found a similar correlation between absence from work and lower work productivity for people with moderate-to-severe psoriasis. However, that study assessed body surface area involvement rather than symptom severity. Another patient survey study assessed the relationship between health-related quality of life and work productivity.10 However, that study also did not assess specific symptom severity. Although the quality of life instrument used contained a single item assessing overall symptom severity, only the overall score was used for the analysis.
This is the first study to examine the relationship between the severity of specific psoriasis symptoms and a variety of personal and work-related health outcomes. In addition to determining that symptoms such as itching and pain have an effect on patients’ physical and mental well-being, the study results showed a positive correlation between the severity of those symptoms and reduced productivity and attendance at work. Our results supplement and extend the results from previous surveys on psoriasis patients and demonstrate a direct effect of symptom severity on health-related quality of life as well as work productivity. Regarding limitations to this analysis, it should be noted that there may be omitted variables implicated in the causal process of the model. These omitted variables could have an effect on parameter estimates, standard errors, and the overall structure of the model. Additionally, the cross-sectional method of data collection lacks the ability to assess a temporal relationship between covariates and outcomes. Lastly, data used in this study were derived from a self-report survey without clinician confirmation for diagnosis and severity.
Conclusion
Patient-reported symptom severity in plaque psoriasis, particularly itching, pain, and scaling, negatively affects health outcomes and work productivity. Effective management of debilitating psoriasis symptoms will reduce functional impairment and improve quality of life.
Footnotes
Disclosures
This study was sponsored by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. Colin Lewis-Beck was an employee of STATinMED Research at the time of the study. Onur Baser and Lin Xie are employees of STATinMED Research, which was retained by Novartis Pharmaceuticals for this study. Edward Kim is an employee of Novartis Pharmaceuticals Corporation. Safiya Abouzaid was an employee of Novartis at the time of the study. Editorial support was provided by Elizabeth M Moran of STATinMED Research and was funded by Novartis Pharmaceuticals Corporation. The authors report no other conflicts of interest in this work.
References
- 1.Stern RS, Nijsten T, Feldman SR, et al. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. J Investig Dermatol Symp Proc. 2004;9(2):136–139. doi: 10.1046/j.1087-0024.2003.09102.x. [DOI] [PubMed] [Google Scholar]
- 2.The National Psoriasis Foundation http://www.psoriasis.org/Accessed December 18, 2012
- 3.de Korte J, Sprangers MA, Mombers FM, Bos JD. Quality of life in patients with psoriasis: a systematic literature review. J Investig Dermatol Symp Proc. 2004;9(2):140–147. doi: 10.1046/j.1087-0024.2003.09110.x. [DOI] [PubMed] [Google Scholar]
- 4.Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the SF-12 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2002. [Google Scholar]
- 5.Hox JJ, Bechger TM. An introduction to structural equation modeling. Family Science Review. 1998;11:354–373. [Google Scholar]
- 6.McAuley E, Konopack JF, Ed M, et al. Physical activity and quality of life in older adults: influence of health status and self-efficacy. The Society of Behavioral Medicine. 2006;31(1):99–103. doi: 10.1207/s15324796abm3101_14. [DOI] [PubMed] [Google Scholar]
- 7.Mooney CZ, Duval RD. Bootstrapping: A Nonparametric Approach to Statistical Inference. Newbury Park, CA: Sage; 1993. [Google Scholar]
- 8.Linnet K. Nonparametric estimation of reference intervals by simple and bootstrap-based procedures. Clin Chem. 2000;46(6):867–869. [PubMed] [Google Scholar]
- 9.Horn EJ, Fox KM, Patel V, et al. Association of patient-reported psoriasis severity with income and employment. J Am Acad Dermatol. 2007;57(6):963–971. doi: 10.1016/j.jaad.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 10.Schmitt JM, Ford DE. Work limitations and productivity loss are associated with health-related quality of life but not with clinical severity in patients with psoriasis. Dermatology. 2006;213(2):102–110. doi: 10.1159/000093848. [DOI] [PubMed] [Google Scholar]