Abstract
We narrate the case of a term baby who presented at 30 h of age in congestive cardiac failure due to vein of Galen aneurysmal malformation. A successful interventional radiology embolisation of the feeding vessels to the aneurysm was performed on day 5. Twenty hours following the procedure, the baby developed significant intraventricular haemorrhage with extension into the brain parenchyma; care was reoriented on day 7 of life after discussion with the parents. Vein of Galen aneurysmal malformation is a rare congenital vascular malformation. It usually manifests in the newborn period with high-output cardiac failure. The death rate is higher in those who present early in the neonatal period. The management of this condition requires a multidisciplinary approach.
Background
The vein of Galen aneurysmal malformation (VGAM) is a rare condition (figure 1). The main clinical presentation here was congestive cardiac failure, although rare, it is important to highlight the fact that all cases of cardiac failure may not be due to a primary cardiac cause. A thorough clinical examination (cranial bruit elicited retrospectively) with bedside investigation-echocardiography, (retrograde diastolic flow in descending aorta with continuous forward flow in arch arteries) leads to colour Doppler ultrasound scan, which helped in making the diagnosis. An early diagnosis with prompt referral is crucial in the management of this life-threatening condition.
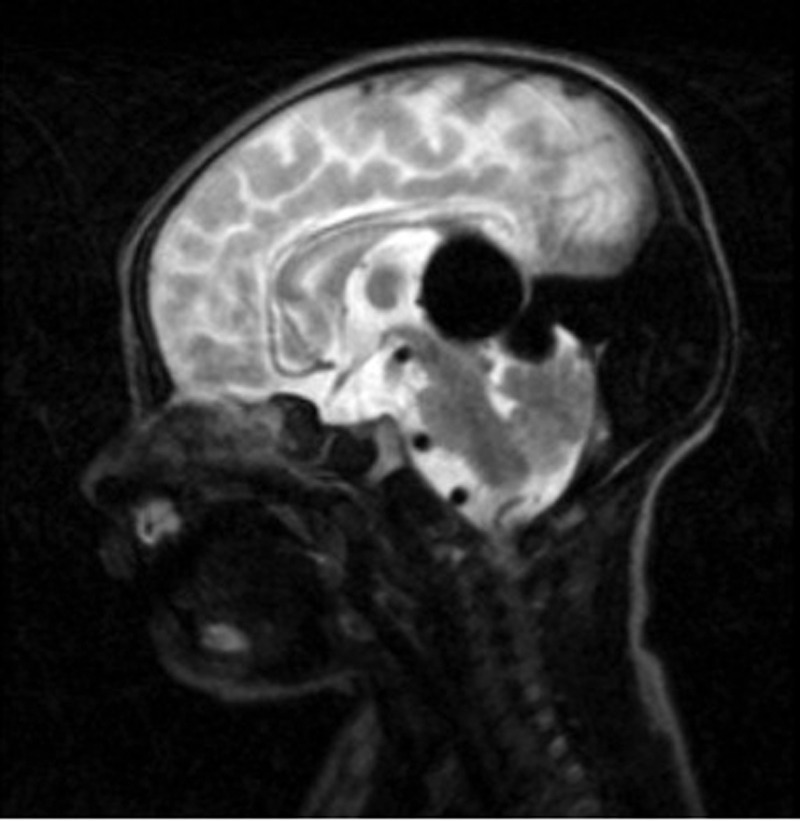
Figure 1.
Sagittal T2-weighted image. Enlarged vein of Galen draining into prominent straight sinus and torcula herophili (venous confluence) seen as a flow void.
Case presentation
A term baby who weighed 3400 g was born by spontaneous vaginal delivery in good condition. The pregnancy was uneventful and the mother did not have any significant medical history. At 30 h of age, he presented with features suggestive of cardiac failure—poor feeding, cyanosis, tachypnoea, a grade 3/6 systolic murmur heard all over the praecordium with a left parasternal heave and hepatomegaly. The blood pressure and femoral pulses were normal. There were no dysmorphic features and the other systemic examination was unremarkable. Retrospective clinical examination elicited a significant cranial bruit.
Investigations
Chest x-ray confirmed cardiomegaly. Bedside echocardiography showed normal cardiac anatomy with dilated right atrium. Telemedicine review by paediatric cardiologist confirmed dilated right heart chambers with high cardiac output in ascending aorta, retrograde diastolic flow in descending aorta and continuous forward flow in arch arteries. This indicated low resistance to flow in the cerebral circulation.
A bedside cranial ultrasound examination showed a midline cystic mass posterior to the third ventricle, and Doppler examination showed pulsatile cystic mass, suggestive of arterio-venous malformation of the vein of Galen.
MRI of brain confirmed the diagnosis.
Full blood count and C reactive protein were normal and blood culture had no growth.
Treatment
The baby required ventilatory support, inotopes, diuretics, fresh frozen plasma and cryoprecipitate. He developed deranged renal and hepatic function. Following transfer to a cardiology centre and a difficult period of stabilisation, successful embolisation of the feeding vessels were carried out by the neuroradiologist on day 5.
Outcome and follow-up
There was significant improvement in the general condition, his heart failure partially subsided and there was improvement in the renal and hepatic function. Twenty hours following embolisation, he had a sudden drop in haemoglobin secondary to a massive intraventricular haemorrhage. Subsequent CT of brain demonstrated extension of the haemorrhage into the cerebral parenchyma. The baby's general condition deteriorated with cerebral oedema and seizures; care was withdrawn on day 7, with the consent of the parents.
Discussion
VGAMs are rare congenital vascular malformations resulting from the development of arteriovenous connection between primitive choroidal vessels and the median prosencephalic vein of Markowski (figure 2).1 The malformation develops between 6th and 11th week of fetal development2 and constitutes about 1% of all intracranial vascular malformations.3 In the newborn period, the usual presentation is high output cardiac failure which can be associated with multiorgan dysfunction. VGAM can also cause mass effect leading to progressive neurological impairment, can present with cerebral ischaemic changes and can result in hydrocephalus from the obstruction of cerebrospinal fluid flow. In utero, the low systemic resistance can decrease the flow through the fistula and minimise the cardiac decompensation. Evidence of progressive cardiac dysfunction in utero indicates a high-flow lesion.1 Studies show that a poor outcome is associated with presentation early in the neonatal period. Reported neonatal mortality following treatment ranges from 8% to 63% compared with around 10% in children presenting later.4 The management of this complex condition involves a multidisciplinary approach with involvement of neuroradiologists neurosurgeons, cardiologists and neonatologists.
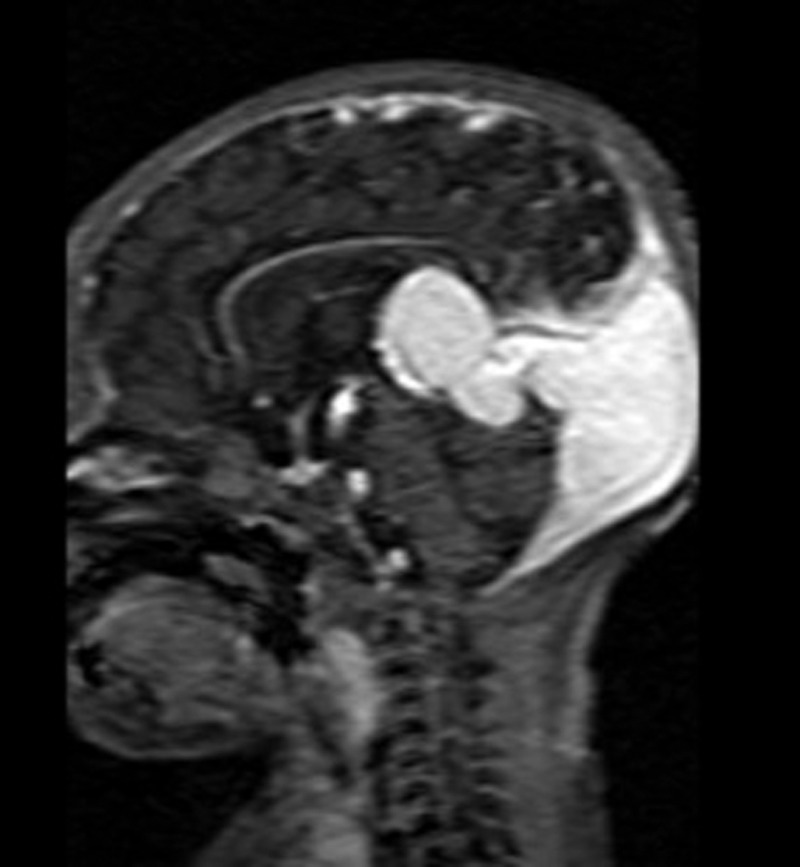
Figure 2.
Sagittal T1-weighted postcontrast (gadolinium) showing enhanced vessel signal.
Learning points.
Cases of cardiac failure need not be due to a primary cardiac condition.
Highlights the importance of thorough clinical examination (here, eliciting cranial bruit can give a clue to the possible diagnosis).
Early diagnosis and prompt referral is crucial in the management of these life-threatening conditions.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jones BV, Ball WS, Tomsick TA, et al. Vein of Galen aneurysmal malformation: diagnosis and treatment of 13 children with extended clinical follow-up. Am J Neuroradiol 2002;23:1717–24 [PMC free article] [PubMed] [Google Scholar]
- 2.Raybaud CA, Strother CM, Hald JK. Aneurysm of the vein of Galen: embryonic considerations and anatomical features relating to the pathogenesis of the malformation. Neuroradiology 1989;31:109–28 [DOI] [PubMed] [Google Scholar]
- 3.Kothari SS, Naik N, Juneja R, et al. Aneurysm of the vein of Galen in neonates: report of four cases. Indian Heart J 2001;53:499–502 [PubMed] [Google Scholar]
- 4.McSweeney N, Brew S, Bhate S, et al. Management and outcome of vein of Galen malformation. Arch Dis Child 2010;95:903–9. [DOI] [PubMed] [Google Scholar]