Abstract
This study examined the interaction of depressive symptoms and drug use on HIV/STI risk among sexual minority young adults. Analyses tested the interactive effect of depressive symptoms and drug use on unprotected sex. Among drug users, more depressive symptoms were associated with higher rates of unprotected sex with a male partner (for both male and female participants) but this was non-significant for non-users. Interventions with these groups should incorporate content on depression and drug use to reduce HIV/STI risk. Prevention efforts also should not neglect the vulnerability of young women that have sex with women and/or identify as non-heterosexual.
Keywords: HIV prevention, depression, drug use, sexual minorities, young adults
Introduction
In the United States, HIV/AIDS and sexually transmitted infections (STIs) continue to be a public health concern among young adults, particularly among young sexual minority men (CDC, 2011b). Regardless of sexuality, young adults who use illicit drugs are at heightened risk of infection through an increased number of sexual partners (Howard & Wing, 2004), unprotected sex (Howard & Wing, 2004), and sex while under the influence of alcohol or drugs. Psychological distress also increases this risk (Brown et al., 2006). However, few studies have examined the co-occurrence of psychological distress with substance use in the context of sexual risk Ramrakha, Caspi, Dickson, Moffit, & Paul, 2000; Teplin et al., 2005). Further, only recently have these relationships been examined with young sexual minority men (YSMM; Mustanski, Garofalo, Herrick, & Donenberg, 2007), and no such studies have included young sexual minority women (YSMW), despite their vulnerability (Reisner et al., 2007; Herrick, Matthews, & Garofalo, 2010).
The current study examines these associations in cross-sectional samples of YSMM/YSMW to further inform HIV/STI prevention. We hypothesized that greater depressive symptoms would be associated with unprotected sex with a male partner in both YSMM and YSMW groups. Additionally, we hypothesized that illicit drug use would moderate this association such that the interaction of depression and drug use would heighten HIV/STI risk.
Methods
Participants and Procedures
Adult males (n=838) and females (n=583) were recruited in 2001 in a large, urban Midwestern city from diverse LGBT-friendly venues. Venues ranged from large “pride” and festival events to small poetry readings (e.g., occurring in community-based organization settings). The paper-and-pencil survey was completed at the particular venues and took approximately 10–15 minutes to complete. Participants were reimbursed $5.00 at time of survey completion. The study was approved by cooperating sites’ Institutional Review Boards. Current secondary analyses focused on the subsample of 81 female and 159 male young adults, aged 18–24 years (M age = 22), who reported sexual identity as either gay, lesbian or bisexual and/or reported lifetime same-sex sexual behavior. Samples were predominantly African American (YSMM = 58%; YSMW = 64%).
Measures
Demographics included age, race and ethnicity, annual income, education and sexual identity. Sexual identity was measured differently for male and female samples. Males were asked to check “all terms you use to identify yourself” out of the following options: Gay/homosexual, bisexual, straight/heterosexual, “down low”, “homo thug”, same gender-loving, just “mess around”, no label or term or other. Females were asked “How do you identify or think about yourself sexually?” and responded to the following options: Straight/heterosexual, mostly straight, bisexual, mostly lesbian/gay and lesbian. Given that the majority of sexual identity responses were in the gay/homosexual and lesbian categories (e.g., 61% of all YMSM and 63% of all YWSW), male and female participants were grouped into “Gay/Homosexual versus Other” or “Lesbian/Homosexual versus Other” categories.
Depressive symptoms were measured using a 9-item version of Center for Epidemiological Studies for Depression (CES-D) scale (Santor & Coyne, 1997; YSMM sample, α= .79, YSMW sample, α = .72). Higher scores indicate more depressive symptoms.
Illicit drug use included past 6 month frequency of marijuana, cocaine (including crack), speed, ecstasy, heroin and any other illicit drug use over the past 6 months. Respondents were asked “how often have you used” each particular drug with responses ranging from 0 (never) to 6 (nearly every day). Item responses were dichotomized into “any” versus “no use” for each item and then summed to create a total score for illicit drug use (ranging from 0–7). Non-use was coded as a total score of “0”; any use (i.e., score of 1–7) was coded as “1”.
Recent HIV/STI risk behavior for the YSMM sample was assessed by asking: In the past 6 months, how often have you had any unprotected insertive or receptive anal sex? For the YSMW sample, we combined responses from two yes/no items (have you had vaginal or anal sex with any men without a condom in the past 6 months? have you had oral sex with any men without a condom in the past 6 months?) to assess unprotected oral, vaginal or anal sex with any male partner. Both sample responses were dichotomized to 0 (never) versus 1 (at least once) to represent any recent unprotected sex. Our study was limited to the available data on any unprotected sexual risk behaviors, which were measured differently for YSMM than for YSMW in that YSMM were not asked about oral sexual activity.
Data Analysis
Bivariate analyses were conducted to examine the associations between demographics, depressive symptoms, illicit drug use and HIV/STI risk. Controlling for relevant demographics, we tested separate logistic regression models by sex examining the interaction effect of depression and drug use on HIV/STI risk for YSMM and YSMSW. Significance of conditional effects were deconstructed using procedures outlined by Hayes and Matthes (2009).
Results
Bivariate findings
Recent unprotected sex was reported at 35% (n = 56) and 25% (n = 20) for YSMM and YSMW, respectively. Any illicit drug use was high (49% of YSMM; 58% of YSMW) with marijuana primarily used among YSMW (54%) and YSMM (44%). Mean depressive symptoms score were 7.80 (SD = 5.52) and 9.04 (SD = 5.32) for YSMM and YSMW, respectively.
YSMM reporting an educational level of college BA or higher had lower rates of illicit drug use than those with less education, χ2 (1,139) = 4.69, p < .05. There were no demographic differences among YSMM on depressive symptoms or rates of unprotected sex. Among YSMW, lesbians reported lower rates of unprotected oral, anal, or vaginal sex with a male partner compared to YSMW that identified as other, χ2 (1,139) = 4.69, p < .05.
Model Testing
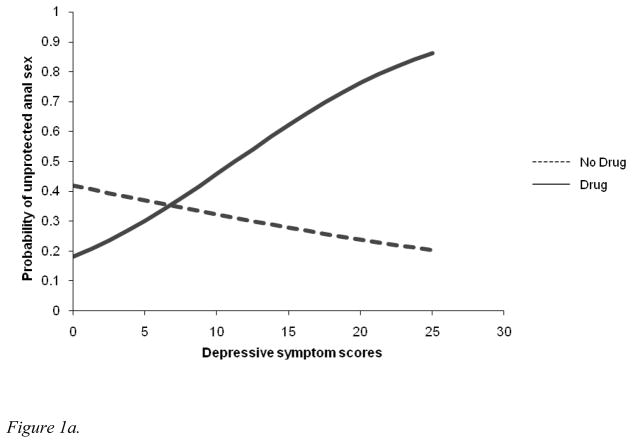
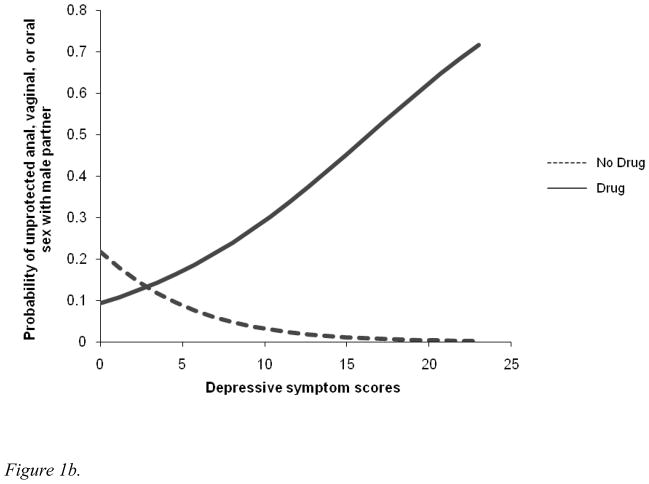
For YSMM, the depressive symptoms x drug use interaction term was found to be significant (b = .18, SE = .07, Wald = 6.27, p = .012), controlling for education. Figure 1a displays graphically the probability of a participant reporting unprotected anal sex at various levels of depressive symptoms for drug users and non-users (conditional effects). For YSMW the depressive symptoms x illicit drug use interaction was also significant (b = .35, SE = .16, Wald = 4.71, p = .03); probabilities of unprotected sex displayed in Figure 1b. For both groups, the probability of reporting unprotected sex increased for drug users but not for non-users.
Figure 1.
Figure 1a. Interaction of illicit drug use and depressive symptoms on probability of unprotected anal sex with male partner among YSMM
Figure 1b. Interaction of drug use and depressive symptoms on probability of unprotected sex with male partner among YSMW
Discussion
This is the first study, to our knowledge, to examine parallel HIV/STI risk factors in both YSMM and YSMW populations. Our findings suggest that drug use and depression interact to heighten HIV/STI risk across sexes and within a sample heavily comprised of African American sexual minorities; a population typically underrepresented in sexual minority research. Additionally, unlike YSMM, YSMW are typically not queried (e.g., by health care providers) about their sexual risk behavior with men. Our findings suggest that inquiry (from both a research and clinical perspective) into all sexual risk and substance use behaviors is critical to understanding HIV risk among YSMW. During this stage of development, sexual identity may be more fluid and shift more rapidly and readily than for older adults. Therefore, relying on sexual identity as a means of assessing HIV/STI risk may lead to inaccuracies in understanding actual behavioral risk. In addition to explicating sexual risk behaviors, our data suggest a need to target both mood and drug use in HIV/STI prevention interventions. Young adults who engage in same-sex behaviors may be using illicit drugs as a way of self-medicating depressive symptoms that may be triggered by a variety of psychosocial factors (e.g. family and/or community stigma).\
Findings should be considered in light of several study limitations, such as the use of a convenience sample. Self-selection biases (inherent in convenience samples), for example, with respect to who attended such events and who volunteered to complete the survey limits our ability to generalize findings to other YSMM and YSMW. The generalizability of our findings should be considered in this context and future a priori studies should aim to incorporate more representative sampling approaches. Additionally, despite that our data were originally collected in 2001, young sexual (and racial/ethnic) minority men continue to face alarming rates of new HIV infection. For example, rates of new infections attributed to male-to-male sexual contact increased from 67% of all new infections in 2007 to 75% in 2010 (CDC, 2011a). Moreover, 60% of infections occurred among African American/Black youth (CDC, 2011a) and between 2006 and 2009, this age and racial/ethnic group had the largest increase in new infections (CDC, 2011b). Likewise, for HIV-positive female adolescent/young adults, an overwhelming 63% identify as African American/Black (CDC, 2011a). More recent evidence also indicates mental health difficulties and substance abuse are substantial problems for many sexual minorities (Salomon et al., 2009), and major contributors to their HIV risk (Mustanski et al., 2007). Despite substantial prevention efforts (see Johnson et al., 2008 for a review), it is clear that HIV continues to be a concern among many sexual minority communities. Moreover, the nascent stage of the health promotion and HIV prevention literature with sexual minority youth (particularly YWSW) allows these study findings to still make a significant contribution to the field and serve as a springboard for future research with more representative populations. Ultimately, given the lack of studies focusing on the health and mental health needs of the young sexual minority population, dissemination of our findings despite aforementioned study limitations is germane to advancing the field.
In sum, HIV primary and secondary prevention interventions uniquely tailored to the needs of both young sexual minority men and women appear urgently needed. Further research is required to replicate these findings and elucidate other salient factors to include in the development of HIV prevention interventions for these high-risk young adults.
Acknowledgments
Research supported by NIDA grant K23DA021532, NIMH grant T32MH 078788-04 and the Lifespan/Tufts/Brown Center for AIDS Research for the data analysis and manuscript preparation. Howard Brown Health Center and The City of Chicago Department of Public Health provided financial support for data collection and management. This research was made possible by generous contributions of time and energy from Howard Brown Health Center staff and volunteers and the collaboration of gay, lesbian and bisexual community members in community health research. Recruitment of participants was conducted in collaboration with community-based gay/lesbian/bisexual/transgendered and HIV/AIDS organizations in Chicago.
References
- Brown LK, Tolou-Shams M, Lescano C, Houck C, Zeidman J, Pugatch D Project Shield Study Group. Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. Journal of Adolescent Health. 2006;39(3):444. e1–8. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV surveillance in adolescents and young adults. 2011a Retrieved from www.cdc.gov/hiv/topics/surveillance/resources/slides/adolescents/index.htm.
- CDC. HIV surveillance in men who have sex with men. 2011b Retrieved from www.cdc.gov/hiv/topics/surveillance/resources/slides/msm/slides/msm.pdf.
- Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavioral Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Herrick AL, Matthews AK, Garofalo R. Health risk behaviors in an urban sample of young women who have sex with women. Journal of Lesbian Studies. 2010;14(1):80–92. doi: 10.1080/10894160903060440. [DOI] [PubMed] [Google Scholar]
- Howard DE, Wing MQ. The relationship between substance use and STD/HIV-related sexual risk behaviors among US adolescents. Journal of HIV/AIDS Prevention in Children & Youth. 2004;6(2):65–82. [Google Scholar]
- Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, Malow R, McClellan WM. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Systematic Reviews. 2008;16(3):CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Annals of Behavioral Medicine. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramrakha S, Caspi A, Dickson N, Moffit TE, Paul C. Psychiatric disorders and risky sexual behaviour in young adulthood: Cross sectional study in birth cohort. BMJ. 2000;321(7256):263–266. doi: 10.1136/bmj.321.7256.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Mimiaga MJ, Case P, Grasso C, O’Brien CT, Harigopal P, Mayer KH. Sexually transmitted disease (STD) diagnoses and mental health disparities among women who have sex with women screened at an urban community health center, Boston, MA. Sexually Transmitted Diseases. 2007;37(1):5–12. doi: 10.1097/OLQ.0b013e3181b41314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santor DA, Coyne JC. Shortening the CES–D to improve its ability to detect cases of depression. Psychological Assessment. 1997;9(3):233–243. [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, et al. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: Implications for age-specific interventions. AIDS & Behavior. 2009;13(4):811–21. doi: 10.1007/s10461-008-9439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services. 2005;56(7):823–828. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]