Abstract
Background
Researchers theorize that interventions increase physical activity by influencing key theory-based mediators (e.g., behavioral processes). However, few studies have been adequately powered to examine the importance of mediators.
Purpose
This study examined both physical activity behavior and psychosocial mediators in a randomized trial specifically powered to detect mediation.
Methods
Healthy, sedentary adults (n=448; 70% Caucasian, 87% women, mean age was 43) were randomly assigned to either a six-month print-based theory tailored physical activity intervention (n=224) or a six-month health/wellness contact control arm (n=224).
Results
The print intervention arm exhibited greater increases in physical activity than the control arm at six and 12 months (p<.05). Additionally, behavioral processes were found to be an important mediator of physical activity behavior.
Conclusions
It is important for researchers and practitioners to focus on increasing behavioral strategies for physical activity adoption. Future studies should examine other potential mediators of physical activity.
Keywords: Exercise, Physical Activity, Mediators, Intervention Studies
Physical activity interventions based on theories such as Social Cognitive theory and the Transtheoretical Model are effective in promoting physical activity [1]. Therefore, researchers recommend that physical activity interventions be theory-based [2–4]. The advantage of theory driven interventions is that they leverage an accumulated body of knowledge in the selection of techniques for behavior change. It also provides researchers with the opportunity to examine why an intervention is effective or ineffective [5]. Therefore, as noted by Cerin and MacKinnon [6], mediator analyses allows for an “action theory test” (i.e., did the intervention successfully change the mediators) and a “conceptual theory test” (which of those constructs predict change in the targeted behavior).
Previous Research on Mediators in Physical Activity Interventions
The most common theory used in physical activity intervention research examining mediators is the Transtheoretical Model [4]. The Transtheoretical Model postulates that individuals move through a series of stages as they adopt and maintain physical activity [7, 8]. Behavioral strategies (e.g., rewarding yourself), cognitive strategies (e.g., increasing knowledge), and decisional balance (i.e., weighing the pros and cons of becoming physically active) are constructs hypothesized to be important as individuals move through the theorized stages. Social Cognitive Theory is also a common theory used in physical activity intervention research. The central focus of Social Cognitive Theory is self-efficacy, which refers to one’s confidence to become physically active [9].
A comprehensive review of psychosocial mediators indicates that self-regulation (i.e., planning, behavioral processes) has the most consistent support as a mediator [4]. However, the authors classified only one study in their review as having high quality and this study was still limited by low power to detect mediation [3]. The conclusion of this review is in contrast to a previous review suggesting that both behavioral processes and self-efficacy were important mediators [10]. Since the Rhodes and Pfaeffli [4] review, additional physical activity mediator studies have been published. For example, Crain and colleagues [2] found that their intervention increased self-efficacy, which was related to enjoyment of physical activity, integration into self-concept, and physical activity maintenance. Another study found that of the 14 variables tested, the intervention was related to an increase in only two of the variables (e.g., change in pros and initial change in experiential/cognitive processes) and none of the variables were significant mediators [11].
Baruth and colleagues [12] examined mediators of a church-based physical activity intervention. Groups of churches were randomly assigned to either receive the intervention immediately or in one year. Several potential mediators were tested (i.e., church support, instrumental church support, emotional church support, self-efficacy, and enjoyment) and none were significant mediators. In another study by Baruth and colleagues [13], psychosocial mediators were examined among participants who received one of three interventions: physician advice, assistance, or counseling. There were no differences on total physical activity minutes between the groups; however, the assistance and counseling groups exhibited higher cardiovascular fitness than the advice group for women. Regarding mediators, changes in behavioral processes from baseline to 24 months significantly mediated the effect of the intervention on physical activity and cardiorespiratory fitness. Self-efficacy, cognitive processes, and decisional balance were not significant mediators.
One major limitation of the previous studies is that many were not specifically powered to detect mediation. Therefore, the purpose of the present study was to improve upon previous studies by specifically powering our trial to examine mediation in addition to powering on the overall outcome of the trial (i.e., physical activity behavior). Our trial also improved upon many of the previous trials by implementing the following: (1) Specifically tailoring the intervention to target the potential mediators; (2) including a no-exercise control group controlling for contact time (i.e., health and wellness with no focus on physical activity); (3) utilizing a prospective design; and (4) examining mediators both at the end of the six month intervention and six months after the intervention ended (i.e., 12 months).
In the present study, we randomized 448 sedentary participants to either a tailored print-based intervention or a health/wellness contract control. We hypothesized that the print arm would report greater minutes of physical activity per week than the control arm. Additionally, we hypothesized that behavioral processes (e.g., enlisting social support, rewarding yourself) and self-efficacy would mediate the relationship between the intervention and physical activity behavior. Cognitive processes (e.g., comprehending benefits, increasing healthy opportunities) and decisional balance were also explored.
Method
Participants
Participants were recruited primarily through newspaper advertisements, email advertisements at worksites, and letters sent directly to potential participants (identified through their electronic medical record). Participants completed a telephone screening interview based on the 10-item Physical Activity Readiness Questionnaire [14, 15]. Participants were healthy low-active women and men (n=448) ages 18 and older. Low-active was defined as self-reporting 90 minutes per week or less of moderate or vigorous intensity physical activity for the last six months. Physical activity was assessed on the telephone screening interview by asking if the participant engaged in any physical activity that was at least of moderate intensity during the previous month (which was thoroughly defined for the participant). If the participants answered yes, number of days per week and number of minutes per session were assessed. We also obtained healthcare provider consent for each participant in the trial.
We excluded participants who had medical conditions that may have impaired their ability to engage in physical activity including a history of coronary heart disease (history of myocardial infarction, symptoms of angina), orthopedic problems that would limit physical activity participation, or any other medical condition that may make physical activity unsafe. Other exclusion criteria included current or planned pregnancy, consumption of three or more alcoholic drinks per day, and psychosis or current suicidal ideation. Participants also had to be willing to be assigned to either study arm. This study was approved by and in compliance with both the HealthPartners and the Miriam Hospital Institutional Review boards. Participants read and signed a consent form approved by our institutional review board prior to participation. This study was conducted from August, 2005 to July, 2008.
Measures
Primary Dependent Variable: Seven-Day Physical Activity Recall Interview
We utilized the Physical Activity Recall Interview to assess physical activity, our primary dependent variable in the study. Several studies have demonstrated the Physical Activity Recall Interview’s reliability and validity. One study found the test re-test reliability between two interviewers administering the Physical Activity Recall Interview to be 0.86 [16]. Validity has been established by a significant correlation between the Physical Activity Recall Interview and an objective measure of physical activity using the accelerometer based Caltrac [0.33; 17]. The Physical Activity Recall Interview also correlated with four-week physical activity diaries [0.36; 17]. We administered the Physical Activity Recall Interview at baseline, six months (i.e., end of the intervention), and 12 months (i.e., six months following the end of the intervention) over the telephone. The telephone-administered Physical Activity Recall Interview is correlated with the face-to-face Physical Activity Recall Interview [r = 0.96;18]. The assessment research assistant was blinded to the participant’s study arm at all Physical Activity Recall Interview assessments.
Demographic Variables.
We administered a questionnaire at baseline assessing several demographic variables including age, gender, race, ethnicity, marital status, occupation, education, and income level.
Behavioral and Cognitive Processes
We assessed behavioral and cognitive processes using the 40-item Processes of Change for physical activity measure. Behavioral processes included 20 items from the following five subscales: (1) Substituting alternatives; (2) enlisting social support; (3) rewarding yourself; (4) committing yourself; and (5) reminding yourself [19]. Cognitive processes included 20 items from the following five subscales: (1) Increasing knowledge; (2) being aware of risks; (3) caring about consequences to others; (4) comprehending benefits; and (5) increasing healthy opportunities [19]. The internal consistency for the subscales averaged 0.83 in a previous study [19] and the internal consistency for the current study was .74. Validity has been established in that scores on the cognitive and behavioral processes are significantly related to stage of change [19] and behavioral processes correlates with physical activity participation [20].
Self-Efficacy
We measured self-efficacy using a five-item measure that examines self-efficacy for physical activity in five different situations [i.e., vacation, feeling tired, bad mood, not having enough time, and weather; 21]. The internal consistency for this measure was 0.76 in a previous study [21] and 0.80 in the current study. The test-retest reliability over 2 weeks is 0.90 [21] and self-efficacy correlates with physical activity participation [20]
Decisional Balance
We administered the 16-item Decisional Balance measure [22] to assess participants’ beliefs about the pros (i.e., benefits) and cons (i.e., costs) of physical activity. The internal consistency for the Pros subscale is 0.79 and for the Cons subscale it is 0.95 [22]. In the current study, the internal consistency for the entire scale was 0.86. A decisional balance index score can be computed by subtracting the mean con score from the mean pro score. Regarding validity, this decisional balance index score significantly correlates with stage of change [22] and physical activity participation [20].
Procedure
Interested participants called a study line and completed a telephone screening interview. Eligible participants provided their healthcare provider name and fax number as well as their verbal consent to contact their healthcare provider. Next we faxed their healthcare provider a consent form and upon receipt of their signed consent form stating that it was safe for their patient to engage in physical activity, we sent the participant a consent form and baseline questionnaires. Upon receipt of the signed participant consent form and baseline questionnaires (demographic questionnaire, behavioral processes, cognitive processes, self-efficacy, and decisional balance), we contacted the potential participant to schedule a time to conduct the 7-Day Physical Activity Recall Interview.
Upon completion of the Physical Activity Recall Interview, a computer program implemented by the data programmer and unobservable to the study coordinator and intervention staff, randomly selected participants for the tailored print or contact control arm. The randomization allocation 1:1 was generated using SAS and was stratified on stage of change and gender. Both groups received a letter from the intervention staff (who were not involved in the assessments or data analysis) stating which group they were randomly assigned to, their first set of monthly mediator questionnaires, and physical activity logs (i.e., logs that resemble a calendar in which participants documented the frequency, type, and duration of physical activity each day). The intervention and contact control arm lasted six months with a 12 month follow-up (i.e., six months following the end of the intervention). In addition to baseline, physical activity was assessed at six and 12 months. Participants completed the mediator questionnaires monthly for the first six months and at 12 months. Participants were given $10 for completing each questionnaire (during the first six months) and physical activity log (for a total of $120 for both questionnaires and logs), $15 for completing their six-month assessment, $15 for completing the 12-month assessment, and $15 for completing both assessments for a total of $165.
Tailored Print-Based Intervention
The goal of the tailored print-based intervention was to increase participants’ physical activity level to meet or exceed the Surgeon General, Centers for Disease Control, and American College of Sports Medicine’s current recommendations at the time of the study. The recommendations stated that American adults should participate in 30 minutes or more of moderate-intensity physical activity on five days per week [23]. Participants received intervention materials weekly during the first month, bi-weekly during months two and three, and monthly during months four through six for a total of 11 contacts, consistent with the delivery schedule in other studies [1, 24]. All intervention materials were delivered through the mail.
Participants received a three-page physical activity feedback report based on their responses to the monthly mediator questionnaires. These feedback reports were generated by a computerized expert system and were based on the Transtheoretical Model and Social Cognitive Theory. The reports consisted of pre-planned counseling messages created by Ph.D. level psychologists who had experience in health behavior change. Participants received motivational, educational, and normative feedback. Motivational feedback included information based on the participant’s current stage of change and status on the mediator variable (i.e., low self-efficacy). Educational feedback included information on the Centers for Disease Control/American College of Sports MedicineCSM recommendations of moderate intensity physical activity (e.g., three 10-minute bouts of physical activity can be accumulated each day). Normative feedback included information on how participants compared to individuals who have successfully adopted physical activity. Participants received feedback on the mediator variables (i.e., self-efficacy, behavioral processes, cognitive processes, and decisional balance).
Participants also received manuals matched to the participant’s stage of motivational readiness to change. The manuals were on average 14 pages in length and the content varied depending on the person’s stage of change. For example, participants in the preparation stage received information on the benefits of physical activity, how to fit physical activity into their day, ways to increase enjoyment of physical activity, and strategies for overcoming barriers. Participants were given a manual at the start of the intervention and additional manuals throughout the study when they endorsed a different stage of change. In addition to the manuals, 14 tips sheets were sent to the participants throughout the study. The tip sheets addressed various topics related to physical activity (e.g., rewarding yourself, exercising despite bad weather, how to fit physical activity into your day, maintaining activity). Participants received the tip sheets bi-weekly during the first two months and monthly during months three through six. Participants also logged the frequency, duration, and type of physical activity on a log that resembled a monthly calendar.
Contact Control Arm
Participants randomized to the contact control arm received health and wellness educational materials. Topics included stress management, nutrition, sleep, time management, preventive health, common health questions, headache management, healthy home tips, and mental/emotional health. Contact time was controlled in that the contact control group received the health and wellness mailings on the same schedule as the intervention group described above. Participants did not receive physical activity information for 12 months. To control for the effect of logging, participants in the control group also completed the monthly physical activity logs. Upon completion of the 12 months as controls, participants received American Heart Association standard care print materials on physical activity and the same tip sheets distributed to the tailored print arm.
Data Analysis
Between-group differences in baseline demographic and outcomes data was assessed using Analysis of Variance (ANOVA) for continuous variables and chi-squared tests for categorical variables.
First Study Aim: Effects of Intervention on Physical Activity at Six and 12 Months
Using longitudinal mixed effects models, we assessed the overall effect of the intervention. Models included a random intercept term, which is used to account for the within-subject correlation in the outcome variable over time. In addition, we controlled for baseline values of the outcome. Models were run on the intent to treat sample, such that all participants randomized at baseline were included in the analysis. Mixed effects models used a likelihood based approach to estimation and thus make use of all available data without any formal imputation (e.g., no baseline value carried forward).
Second Study Aim: Identify Mediators of the Treatment Effect on Physical Activity Outcomes at Six and 12 Months
The second aim of the study was to identify the mechanisms through which the treatment impacts physical activity at follow-up. As discussed in more detail below, this study was powered for mediation as well as for the primary aim outlined above. Using the product of coefficients method with bootstrapped standard errors [25, 26], we tested the simultaneous effects of the potential mediators (multiple mediation) and present both a path coefficients (effect of treatment on the mediators) and b path coefficients (effect of mediators on the outcome), as well as the total direct and indirect effects of the treatment. The a path coefficients can be thought of as tests of Action theory and the b paths can be considered tests of Conceptual theory. As noted in Preacher and Hayes [26], the test of mediation is actually the test of the indirect effect of treatment, and as such, will be considered our criteria for determining whether a construct is in fact a mediator of the treatment effect.
As the outcome of interest was physical activity at both six and 12 months (adoption and maintenance phase respectively), data on the potential mediators were analyzed at baseline, three, and six months. In order to meet the temporal precedence assumption of mediator models, we examined whether changes in behavioral and cognitive processes, self-efficacy, and decisional balance from baseline to three months would mediate the effect of treatment on six month physical activity outcomes. Similarly, we examined if changes in these constructs from baseline to six months would mediate the effect of treatment on 12 month outcomes. In both sets of analyses, the potential mediators were coded as changes from baseline and outcomes were absolute scores (Physical Activity Recall Interview at six and 12 months respectively). Models were adjusted for baseline values of the potential mediators and baseline levels of physical activity. All analyses were conducted using SAS 9.3.
Sample Size Estimates
Primary Dependent Variable
Sample size was calculated to detect between group differences on physical activity using procedures described by Cohen [27]. We based our estimates on a previous study using the same intervention comparing a tailored print intervention to a control condition [28]. Based on this previous study, we anticipated that the intervention group would report 151 minutes of physical activity per week at the end of treatment and the control group would report 98 minutes. We assumed an 80% follow-up rate, which indicated that we would need 260 participants for the entire study to detect a significant difference between the groups at a .05 significance level (two-tailed).
Mediator Variables.
We based the mediator estimates for the mediators analysis on the study referenced above [28]. We assumed a two-tailed test (alpha = .05) and power of .80. Assuming a low effect size (.13) of the treatment on the mediators and a low effect size of the mediators on the outcome (.18), we estimated needing a total sample size of 336 at 12 months. Therefore, our goal was to recruit 420 participants assuming a 20% dropout rate (420 X 80%=336).
Results
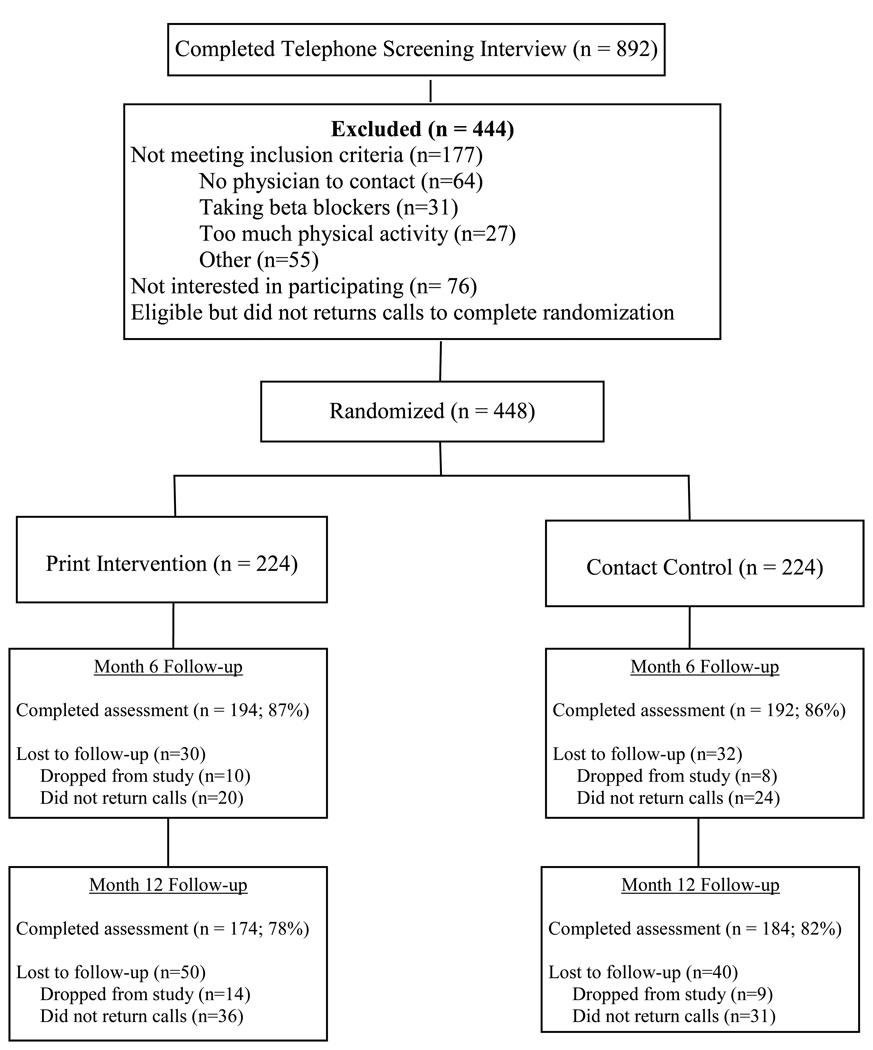
The overall flow of recruitment and randomization is summarized in Figure 1. The final sample consisted of 448 women and men. Baseline descriptive data summarized by treatment arm are presented in Table 1. There were no significant between-group differences on the baseline variables. The retention rate was 86% at six months (87% for the print arm and 86% for the control arm) and 80% at 12 months (78% for the print arm and 82% for the control arm), with no differential drop-out between groups. The retention rates were based on completion of the primary dependent variable (i.e., 7-Day Physical Activity Interview). Eighty percent of the sample completed the mediator questionnaires at three months (81% in the intervention group and 79% in the control group) and 69% at six months (70% in the intervention group and 68% in the control group).
Figure 1.
Participant Flow Chart
Table 1.
Baseline Descriptive Statistics by Group
| Variable | Control | |
|---|---|---|
| (n= 224) | (n=224) | |
| Age (years) | 43.1 | 42.2 |
| Gender (% Female) | 87.1 | 87.1 |
| Race (%) | ||
| Caucasian | 67.0 | 72.8 |
| African-American | 27.2 | 23.7 |
| Other | 5.8 | 3.5 |
| Marital Status (% Married) | 51.3 | 51.8 |
| Employment (% Employed) | 87.5 | 88.4 |
| Income (% over $50,000) | 50.9 | 57.1 |
| Education (% College Graduate) | 55.4 | 60.2 |
| Cigarette Use (% Smokers) | 15.2 | 12.1 |
| Physical Activity (Minutes/Week)* | 24.49(27.67) | 22.72(27.03) |
Means for each group are reported. Standard deviations are in parentheses.
First Study Aim: Effect of Intervention on Physical Activity at Six and 12 Months
Longitudinal regression models suggested a significant treatment effect on physical activity outcomes at both six and 12 months. Specifically, relative to baseline, participants in the print arm reported participating in 31.26 (Standard Error (SE) =11.51, p=0.007) more minutes of physical activity per week than the control participants at six months and 39.06 (SE=11.93, p=0.001) more minutes per week than the control participants at 12 months.
Second Study Aim: Identify Mediators of the Treatment Effect on Physical Activity Outcomes at Six and 12 Months
The means and standard deviations for the mediator variables are presented in Table 2. A multiple mediation model for six month outcomes suggested a significant effect of treatment on changes in the potential mediators from baseline to three months (a path coefficients), when controlling for baseline values of the outcomes and mediators. These results are presented in Table 3. In each case, the print participants showed greater changes in each of the constructs from baseline to three months. In addition, changes in behavioral processes from baseline to three months were significantly associated with physical activity level at six months (b path coefficient), such that a greater change was associated with more activity reported at six months . These results are presented in the lower half of Table 3. The total indirect effect of treatment through the mediators was 29.40 at six months (SE=6.83, 95% Confidence Interval (CI): 17.61–44.62). Results indicated that the indirect effect of the treatment through behavioral processes was considered significant at six months (ab=27.29, SE=7.96, 95% CI: 13.32–45.92). Table 4 summarizes the indirect effect of each of the potential mediators on physical activity outcomes at six months.
Table 2.
Baseline, Three, and Six Month Scores for the Mediators Variables
| Variable | Baseline |
3-Month |
6-Month |
|||
|---|---|---|---|---|---|---|
| Control | Control | Control | ||||
| (n=224) | (n=224) | (n=181) | (n=177) | (n=156) | (n=152) | |
| Behavioral Processes | 2.57(.58) | 2.49(.51) | 3.07(.60) | 2.66(.59) | 3.20(.71) | 2.67(.69) |
| Cognitive Processes | 3.08(.64) | 3.00(.68) | 3.27(.63) | 2.95(.68) | 3.33(.73) | 2.90(.73) |
| Self-Efficacy | 2.66(.82) | 2.59(.86) | 2.83(.74) | 2.51(.74) | 3.00(.87) | 2.56(.84) |
| Decisional Balance Index* | −.001(.13) | −.01(.13) | .01(.14) | −.03(.13) | .02(.14) | −.03(.13) |
Mean pros minus mean cons. Standard deviations are in parentheses.
Table 3.
The Effect of Treatment on the Mediators (a paths) and the Effect of the Mediators on 6 and 12 Month Outcomes (b paths)
|
a path coefficients (Treatment to Mediator) | ||
|---|---|---|
| Variable | Beta*(SE) | P-value |
| Behavioral Processes | ||
| Change in Mediator Baseline to 3m | .37(.05) | <.001 |
| Change in Mediator Baseline to 6m | .48(.07) | <.001 |
| Cognitive Processes | ||
| Change in Mediator Baseline to 3m | .24(.05) | <.001 |
| Change in Mediator Baseline to 6m | .38(.07) | <.001 |
| Self-Efficacy | ||
| Change in Mediator Baseline to 3m | .31(.07) | <.001 |
| Change in Mediator Baseline to 6m | .44(.09) | <.001 |
| Decisional Balance Index | ||
| Change in Mediator Baseline to 3m | .03(.01) | <.01 |
| Change in Mediator Baseline to 6m | .05(.01) | <.001 |
|
b path coefficients (Mediator to Outcome) | |||
|---|---|---|---|
| Variable | Beta*(SE) | P-value | |
| Behavioral Processes | |||
| 6 Month Outcomes | 74.56 (20.54) | <.01 | |
| 12 Month Outcomes | 72.28(24.17) | <.01 | |
| Cognitive Processes | |||
| 6 Month Outcomes | −17.57 (18.58) | 0.35 | |
| 12 Month Outcomes | −40.02(18.93) | 0.04 | |
| Self-Efficacy | |||
| 6 Month Outcomes | 18.53 (14.14) | 0.19 | |
| 12 Month Outcomes | 10.43(14.77) | 0.48 | |
| Decisional Balance Index | |||
| 6 Month Outcomes | 21.15 (70.81) | 0.77 | |
| 12 Month Outcomes | 31.20(80.03) | 0.70 | |
Betas are regression coefficients. Mediators for models of 6m outcomes are change scores from baseline to 3 months. Mediators for models of 12 month outcomes are change scores from baseline to 6 months. Physical activity is an absolute score. SE denotes standard error. Models are adjusted for baseline physical activity and baseline values of the mediators.
Table 4.
The Indirect Effect of Each Potential Mediator on Six and 12 Month Physical Activity Outcomes
| Indirect Effect of Intervention on Physical Activity at Follow-Up (ab) | |||
|---|---|---|---|
| Variable | Indirect Effect | 95% CI | |
| Behavioral Processes | |||
| 6 Month Outcome | 27.29 (7.96) | 13.32–45.92 | |
| 12 Month Outcome | 34.89(14.59) | 9.49–68.12 | |
| Cognitive Processes | |||
| 6 Month Outcome | −4.28 (5.05) | −15.74–5.61 | |
| 12 Month Outcome | −15.10(7.81) | −30.78– −0.56 | |
| Self-Efficacy | |||
| 6 Month Outcome | 5.67(4.89) | −2.89–17.18 | |
| 12 Month Outcome | 4.54(6.64) | −7.29–20.51 | |
| Decisional Balance Index | |||
| 6 Month Outcome | 0.71 (2.12) | −3.50–5.45 | |
| 12 Month Outcome | 1.47(1.57) | −6.80–10.30 | |
CI denotes confidence interval.
A subsequent model for 12 month outcomes suggested a significant effect of treatment on changes in the potential mediators from baseline to six months (a path coefficients), when controlling for baseline values of the outcomes and mediators. These results are presented in Table 3. In each case, the print participants showed greater changes in each of the constructs from baseline to six months. In addition, changes in both behavioral and cognitive processes from baseline to six months were significantly associated with physical activity level at 12 months (b path coefficients). Specifically, greater changes in behavioral processes and lower changes in cognitive processes over the adoption period were associated with more activity reported at 12 months. These results are presented in the lower half of Table 3. The total indirect effect of treatment through the mediators was 25.81 at 12 months (SE=9.96, 95% CI: 8.43–49.46). Results indicated that the indirect effect of treatment through behavioral and cognitive processes were significant for behavioral (ab=34.89, SE=14.59, 95% CI: 9.49–68.12) and cognitive processes at 12 months (ab=−15.10, SE=7.81, 95% CI: −30.78, −0.56). Table 4 summarizes the indirect effect of each of the potential mediators on physical activity outcomes at 12 months.
Discussion
This study examined the efficacy of a motivationally tailored print-based physical activity intervention and examined which psychosocial variables mediated the effects of the intervention on physical activity. Consistent with previous research, the tailored print intervention resulted in greater increases in physical activity than the health/wellness contact control condition [1]. This finding alone is not particularly novel; however, our goal was to better understand which variables facilitate the change in physical activity found in previous studies. Consistent with our hypothesis, behavioral processes (rewarding yourself, reminding yourself, substituting alternatives, enlisting social support, and committing yourself) was a significant mediator. This is consistent with previous studies [4].
According to the Transtheoretical Model, individuals increase their use of cognitive processes (i.e., increasing knowledge, being aware of risks, caring about consequences to others, comprehending benefits, increasing healthy opportunities) as they progress through the stages of change and increase their physical activity. However, a majority of previous studies indicate that cognitive processes are not an important mediator of physical activity behavior change [e.g., 3, 13]. In our study, cognitive processes were a significant mediator; however, the effect was in the opposite direction than what would be expected based on theory. Consistent with another study [29], participants in the intervention arm increased their cognitive processes relative to the control arm but this increase was related to a decrease in physical activity. It is important to note that this finding occurred for physical activity change at 12 months but not for physical activity at six months.
Despite our findings, it is possible that changes in cognitive processes are still important for physical activity behavior change. For example, it is possible that cognitive processes play an important role for intention to engage in physical activity. Perhaps potential participants already increased their cognitive processes prior to enrolling in the study. It is also possible that as physical activity behavior becomes more habitual over time, cognitions about physical activity become more fully integrated into the sense of self. Therefore, the importance of cognitive processes may become less important over time. Our study did not examine cognitive processes prior to enrollment and therefore, it was not possible to examine the importance of cognitive processes on intention and the comments above should only be considered hypotheses. Future studies should examine the influence of cognitive processes changes on intention to become physically active.
Self-efficacy was not a significant mediator in our study. Previous studies suggest some evidence for the importance of self-efficacy as a mediator, although studies have been mixed. According to Rhodes and Pfaeffli [4], seven of the ten studies in their review indicated that the intervention successfully increased self-efficacy but fewer studies indicated a significant relationship between self-efficacy and physical activity and only one study found that selfefficacy was a mediator [30]. Similar to self-efficacy, decisional balance was not a significant mediator in our study. This is consistent with previous studies indicating that decisional balance is not an important mediator [3, 29]. Similar to self-efficacy, our intervention led to increases in decisional balance relative to the control arm; however, decisional balance did not mediate the relationship between the intervention and physical activity.
According to the Transtheoretical Model, individuals view more cons of being physically active than pros in the earlier stages of change when there is no physical activity participation [7]. As individuals move through the stages, the Transtheoretical Model postulates that individuals report more pros of being physically active than cons. In our study, participants in the intervention arm reported more cons than pros at baseline but the pros exceeded the cons at three and six months. However, the cons exceeded the pros at baseline, three, and six months for the control group. Therefore, the intervention successfully changed the pros/cons index for the intervention as postulated by the Transtheoretical Model. However, decisional balance did not mediate the relationship between the intervention and physical activity behavior change indicating that even though the intervention successfully improved the pros/cons index, this did not account for the intervention’s effectiveness on physical activity.
Our study improved upon previous studies by having an adequate sample size to detect mediation, including an appropriate control group, utilizing a prospective design, and examining physical activity both at the end of the intervention and six months following the end of the intervention. We also improved upon some of the previous literature by using a multiple mediation model rather than a single mediation approach. An important advantage of using a multiple mediation model is it allows researchers to simultaneously test the effect of a set of mediators, while controlling for the effects of the other mediators. It allows for a comparison of the effects of the mediators to determine the relative influence of each mediator. It also mimics theory in that theory postulates that the mediators work together to influence the outcome and do not work in isolation (as is suggested by single mediation models). Multiple mediation models also somewhat account for the potential collinearity among mediators. Finally, the use of a multiple mediation model is consistent with trends in the literature [26].
Despite these strengths, there were some limitations of the study. First, our sample consisted of mostly women (87%) and highly educated individuals. A second limitation is that we had large physical activity increases in the contact control group. This could potentially be attributed to the fact that participants responding to our recruitment advertisements were highly motivated individuals and completed physical activity logs. However, inclusion of a comparison condition that was matched on motivation and physical activity self-monitoring gave us more confidence that our findings were due to intervention-specific effects [31]. A third limitation is that it is possible that the incentives and potential practice or sensitization effects of completing the mediator questionnaires each month influenced the findings. However, this limitation is potentially offset by the fact that both groups received the same incentives and completed the same questionnaires. A final limitation is that social desirability could have played a role in the findings. The participants in the print arm could have reported higher levels of behavioral processes because they believed that this is what was expected.
Mediators not typically tailored on in previous studies such as enjoyment, social support, and outcome expectancies should be tested in future studies to determine if these variables are important mediators. Even though theory-based tailored interventions have led to significant increases in physical activity relative to controls [1], there are a number of participants who do not achieve the physical activity participation guidelines. Therefore, researchers need to start “thinking outside the box” to reach individuals by utilizing new theoretical constructs that are potentially important for successfully increasing physical activity. For example, recent research indicates that increased availability of home and facility-based resources for physical activity was important for physical activity behavior change in a randomized trial [32].
In summary, behavioral processes appears to be an important mediator for physical activity behavior change in intervention trials. Consistent with previous studies [4], cognitive processes, self-efficacy, and decisional balance were not important mediators of physical activity. Future studies including new and innovative designs will enhance our understanding of which mediators are important for behavior change at different points in the behavior change process as well as lead to improvements in the efficacy of physical activity interventions. Abraham and Michie [33] have identified 26 behavioral change techniques used in interventions. Future research should identify which of these specific behavioral change strategies are most useful for increasing physical activity. Based on our findings, interventions should continue to target behavioral processes in order to make a significant public health impact on our sedentary society.
Acknowledgements
This research was supported through a grant from the National Heart, Lung, and Blood Institute (R01 HL72947). The authors would like to acknowledge the incredible work by the research assistants including Kris Nozal and Jane Wheeler and the data programmer Alexander Kravchik. We would also like to thank the study participants without whom this study would not have been possible.
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest to disclose.
Contributor Information
Beth A. Lewis, University of Minnesota, 1900 University Ave SE, Cooke Hall, Minneapolis, MN 55455, Phone 612-625-0756; Fax: 612-626-7700; blewis@umn.edu.
David M. Williams, Brown University, Box G-S121-8, Providence, RI 02912, Phone: 401-863-6248; Fax: 401-863-6551; david_m_williams@brown.edu.
Brian C. Martinson, HealthPartners Research Foundation, Mail Stop: 21111R, P.O. Box 1524, 8170 33rd Avenue South, Minneapolis, MN 55440-1524, Phone: 952-967-5021; Fax: 952-967-5022; brian.c.martinson@healthpartners.com.
Shira Dunsiger, The Miriam Hospital & Brown Medical School, Centers for Behavioral and Preventive Medicine, Coro Building East, 167 Pine St, Suite 1B, Providence RI 02903, Phone: 401-793-8151; Fax: 401-793-8059; shira@stat.brown.edu.
Bess H. Marcus, University of California, San Diego, UCSD School of Medicine, 9500 Gilman Drive, La Jolla, CA 92093, Phone: 858-534-8363; bmarcus@ucsd.edu.
References
- 1.Marcus BH, Napolitano MA, King AC, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychol. 2007;26(4):401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- 2.Crain AL, Martinson BC, Sherwood NE, O’Connor P. The long and winding road to physical activity maintenance. Am J Health Behav. 2010;34(6):764–775. doi: 10.5993/ajhb.34.6.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis BA, Forsyth LH, Pinto BM, Bock BC, Roberts M, Marcus BH. Psychosocial mediators of physical activity in a randomized controlled intervention Trial. J Sport Exerc Psychol. 2006;28:193–204. [Google Scholar]
- 4.Rhodes RE, Pfaeffli LA. Mediators of physical activity behaviour change among adult non-clinical populations. A review update. Int J Behav Nutr Phys Act. 2010;7:37. doi: 10.1186/1479-5868-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Biddle SJH, Nigg CR. Theories of exercise behavior. Int J Sport Psychol. 2000;31:290–304. [Google Scholar]
- 6.Cerin E, MacKinnon DP. A commentary on current practice in mediating variable analyses in behavioural nutrition and physical activity. Public Health Nutr. 2009;12(8):1182–1188. doi: 10.1017/S1368980008003649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcus BH, Forsyth LH. Motivating people to be physically active. Champaign, Ill: Human Kinetics; 2009. [Google Scholar]
- 8.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 9.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentiss-Hall; 1986. [Google Scholar]
- 10.Lewis BA, Marcus BH, Pate RR, Dunn AL. Psychosocial mediators of physical activity behavior among adults and children. Am J Prev Med. 2002;23:26–35. doi: 10.1016/s0749-3797(02)00471-3. [DOI] [PubMed] [Google Scholar]
- 11.Plotnikoff RC, Pickering MA, Rhodes RE, Courneya KS, Spence JC. A test of cognitive mediation in a 12-month physical activity workplace intervention: Does it explain behaviour change in women? Int J Behav Nutr Phys Act. 2010;7:32. doi: 10.1186/1479-5868-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baruth MS, Wilcox S, Blair S, Hooker S, Hussey J, Saunders R. Psychosocial mediators of a faith-based physical activity intervention: implications and lessons learned from null findings. Health Educ Res. 2010;25:645–55. doi: 10.1093/her/cyq007. [DOI] [PubMed] [Google Scholar]
- 13.Baruth M, Wilcox S, Dunn AL, et al. Psychosocial mediators of physical activity and fitness changes in the activity counseling trial. Ann Behav Med. 2010;39:274–289. doi: 10.1007/s12160-010-9178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cardinal BJ, Esters J, Cardinal MK. Evaluation of the revised physical activity readiness questionnaire in older adults. Med Sci Sports Exerc. 1996;28:468–472. doi: 10.1097/00005768-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q) Can J Sport Sci. 1992;17:338–345. [PubMed] [Google Scholar]
- 16.Gross LD, Sallis JF, Buono MJ, Roby JJ, Nelson JA. Reliably of interviewers using the seven-day physical activity recall. Res Q Exerc Sport. 1990;61:321–325. doi: 10.1080/02701367.1990.10607494. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs DR, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25:81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Hayden-Wade HA, Coleman KJ, Sallis JF, Armstrong C. Validation of the telephone and in-person interview versions of the 7-day PAR. Med Sci Sports Exerc. 2003;35:801–809. doi: 10.1249/01.MSS.0000064941.43869.4E. [DOI] [PubMed] [Google Scholar]
- 19.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychol. 1992;11:386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 20.Williams DM, Lewis BA, Dunsiger S, et al. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008;36:186–194. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63:60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 22.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision-making for exercise. Health Psychol. 1992;11:257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 23.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 24.Marcus BH, Lewis BA, Williams DM, et al. A comparison of Internet and print-based physical activity interventions. Arch Intern Med. 2007;167:944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 25.MacKinnon DP. Introduction to statistical mediation analysis. Mahwah, NJ: Erlbaum; 2008. [Google Scholar]
- 26.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 27.Cohen J. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. The Claremont Symposium on applied social psychology. Thousand Oaks, CA: Sage Publications, Inc.; 1988. pp. 31–67. [Google Scholar]
- 28.Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally-tailored physical activity intervention. Ann Behav Med. 1998;20:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 29.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: A multivariate approach. Health Psychol. 2008;27:409–418. doi: 10.1037/0278-6133.27.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Blanchard CM, Fortier M, Sweet S, et al. Explaining physical activity levels from a self-efficacy perceptive: The physical activity counseling trial. Ann Behav Med. 2007;34:323–328. doi: 10.1007/BF02874557. [DOI] [PubMed] [Google Scholar]
- 31.Williams DM. Importance of the nature of comparison condition for testing theory-based interventions: Comment on Michie and Prestwich, 2010. Health Psychol. 2010;29:467. doi: 10.1037/a0019597. [DOI] [PubMed] [Google Scholar]
- 32.Ries AV, Dunsiger S, Marcus BH. Physical activity interventions and changes in perceived home and facility environments. Prev Med. 2009;49:515–517. doi: 10.1016/j.ypmed.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27:379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]