Abstract
Theory-based, efficacious, long-term, completely Internet-based interventions are needed to induce favorable shifts in health behaviors and prevent weight gain. To assess nutrition, physical activity and, secondarily, body weight outcomes in the tailored, social cognitive theory Guide to Health (web-based Guide to Health, WB-GTH) program with all recruitment, assessment, and intervention performed on the Internet. The focus of the efficacy study was engaged participants who completed three or more program modules plus baseline and 6-months post- and 16-months follow-up assessments (n = 247). To be eligible, participants needed to be between 18 and 63 years of age, with a BMI between 23 and 39, sedentary to low-active but otherwise healthy. Participants had a mean age of 45.5 years (10.3), 86.2% were female, with 8.5% from minority groups, with a mean 17.5 (3.0) years of education, and had a median annual household income of about $85,000. Nevertheless, about 83% were overweight or obese and about 75% were sedentary (i.e., <5,000 steps/day) or had low levels of activity (i.e., 5,000–7,499 steps/day). Participants were randomized to the WB-GTH-Basic intervention or WB-GTH-Enhanced intervention. Content, overall target behaviors, program goals, and strategies were the same in the two interventions with the difference that Basic included a generic feedback and planning approach and Enhanced included a highly tailored planning and feedback approach. Participants reported at assessments pedometer step counts to assess physical activity, bodyweight from a scale provided, and fruit and vegetable (F&V) servings were assessed from food frequency questionnaires completed online. Participants in both Basic and Enhanced at follow-up increased physical activity by about 1,400 steps/day, lost about 3% of bodyweight, and increased F&V by about 1.5 servings/day. There was evidence that the least physically active, those who were obese, and those with poorest nutrition made greater long-term improvements. Given similar outcomes for Basic and Enhanced, a relatively simple entirely Internet-based program can help people improve health behaviors and prevent weight gain.
Keywords: Health behaviors, Internet, Physical activity, Nutrition, Step counts, Weight gain prevention
INTRODUCTION
The large potential reach of Internet-based health behavior programs has been advocated as one way to address the increasing prevalence of overweight and obesity in the United States and other countries [1] that foreshadows increased risk for cancers, cardiovascular diseases, diabetes, and premature death, plus substantial healthcare expenditures [2, 3]. However, while there are programs showing the viability of Internet weight loss programs [4], from a population perspective, weight gain prevention may be a more attainable goal [5]. On a population basis, the secular trend for weight gain is about 0.5 to 1 kg per year [5]. As Hill has noted [5], relatively small though consistent changes in food consumption and physical activity should be sufficient to prevent weight gain. However, recently, the concept and utility of “small changes” has been questioned because of the degree of overweight and obesity and the excess energy consumption that it represents [6], plus the ready metabolic adaptations to small changes in energy consumption or expenditure [7]. Adding to questions about the viability of a public health initiative to prevent weight gain using the Internet as an intervention modality is that, to date, there have been few demonstrations of effective weight gain prevention particularly with an Internet delivery system that could then potentially reach large population segments [5].
Recent commentaries and reviews [8–10] have noted that the potential effectiveness, reach, and impacts on public health of Internet-based health behavior programs can be enhanced if programs are conceptually and methodologically grounded in science. In practice, this means that a program’s structure, operating principles, and health behavior change strategies are based on theory and constructs that mediate health behavior change; a high fidelity program can be repeatedly presented to diverse users, and, where possible, randomized controlled trials (RCTs) and standard measures are used to assess outcomes [4, 9]. An additional concern for any health behavior program is the demonstration of maintenance of a meaningful degree of behavior change after program contact is faded or eliminated. Programs that show minimal maintenance or regression to baseline levels at follow-up would likely have limited public health utility [9].
“Internet-based health behavior programs” also can entail multiple delivery systems [4, 9]. For example, parts of a program may be automated but may be used in conjunction with a face-to-face component. An Internet program may be housed within a healthcare delivery system and prescribed by medical staff. Or, an Internet-based program may have an individualized chat mode that may require considerable real-time human interactions. In fact, there are very few studies showing the efficacy of a completely Internet-based program where all recruitment and assessments are performed online and all program content is sufficiently automated so that real-time human interactions are not required [4, 9, 11]. Moreover, such studies also need to demonstrate maintenance of behavior change within the same automated program context. In addition, because attrition is reported to be notably high in Internet-based interventions (more than 50% in some studies; [9, 11]), untreated or education-only control conditions may be less viable in this context given that untreated controls may result in even higher and differential attrition rates [11]. Therefore, RCTs may need to compare two potentially efficacious treatments that can differ on one or more central, theoretically based components [11, 12].
Such designs in RCTs can make interpretations of results difficult if two interventions produce similar outcomes, suggesting that either intervention (or with motivated participants—time alone) could produce positive outcomes. However, the health behaviors that are the focus of this study—nutrition, physical activity (PA), and weight management—have been shown to be difficult to change and maintain over extended periods with self-help or commercial programs [13, 14]. Indeed, even some research-based programs with extensive and extended group and individual contacts have shown minimal changes (e.g., about 75 kcals/day in energy expenditure, the equivalent of walking little more than about 1 extra km/day; [15]). Thus, the health behaviors that were the focus of this study are unlikely to change substantially over an extended time period alone and/or with any given program.
There are other related issues that, while not entirely endemic to Internet-based programs, are of importance for future development and relative cost-effectiveness. Internet-based programs while able to negate most time and place specifications of more usual “face-to face” programs, also present the ability through algorithms and software to tailor program content based on an array of user characteristics and preferences, progress in behavior change, and preferred use and individual efficacy with key mediators of change such as self-regulation strategies [16]. Tailoring then combines these arrays and produces highly individualized renditions of a basic program. However, extensive tailoring adds appreciably to costs of program development [17]. While studies have shown that some tailoring can enhance behavior change [16], it is not clear how much tailoring will add to a program that includes theoretically based, “basic” elements of behavior change. Such basic programs could include strategies to increase self-efficacy and self-regulation tactics including goal setting and planning for change, problem solving, as well as tracking, reporting, and receiving feedback about targeted health behaviors. A “basic” health behavior change program may produce an adequate amount of change but with less development costs of a highly tailored, “enhanced” program. Such issues are critical for translating research into practice [18].
Additional concerns noted with Internet health behavior programs have focused on diversity. A “digital divide” along income and education levels, and to an extent, minority group status still exists for access to high speed Internet [19, 20]. However, reports indicate that at higher levels of income and education, Internet access is now nearly universal [19, 20]. An additional related issue and question, however, is which population segments benefit from using an Internet-based health behavior program? If program users, despite income and education advantages, were previous to program use sedentary, not eating nutritiously, and were obese, an effective program could have meaningful public health impacts. The diversity of users, therefore, also can be represented by users’ baseline health behaviors that are closely associated with disease risk [2, 21].
The present study focused on changes in nutrition and physical activity, and on prevention of weight gain, that are central to risk reduction for cancers and other diseases [1, 5]. In addition, the study addressed Internet intervention issues in a number of ways including: (1) electronically conducting all recruitment, assessment, and program activities; (2) using standard assessments for nutrition, physical activity, and weight; (3) including a long follow-up phase with minimal contact, (4) assessing the efficacy of a basic behavior change program based on social cognitive theory (SCT; [22]) compared to an enhanced program featuring tailored self-regulatory steps, with self-regulation presumably pivotal for health behavior changes; (5) assessing if the program was efficacious in changing the health behaviors of participants who initially were sedentary or inactive, overweight or obese, and lower in fruit and vegetable consumption; and (6) testing the viability of weight gain prevention. Given limited research on completely Internet-based, longer-term programs, the present study was designed and is presented as an efficacy study.
METHOD
Recruitment and procedures
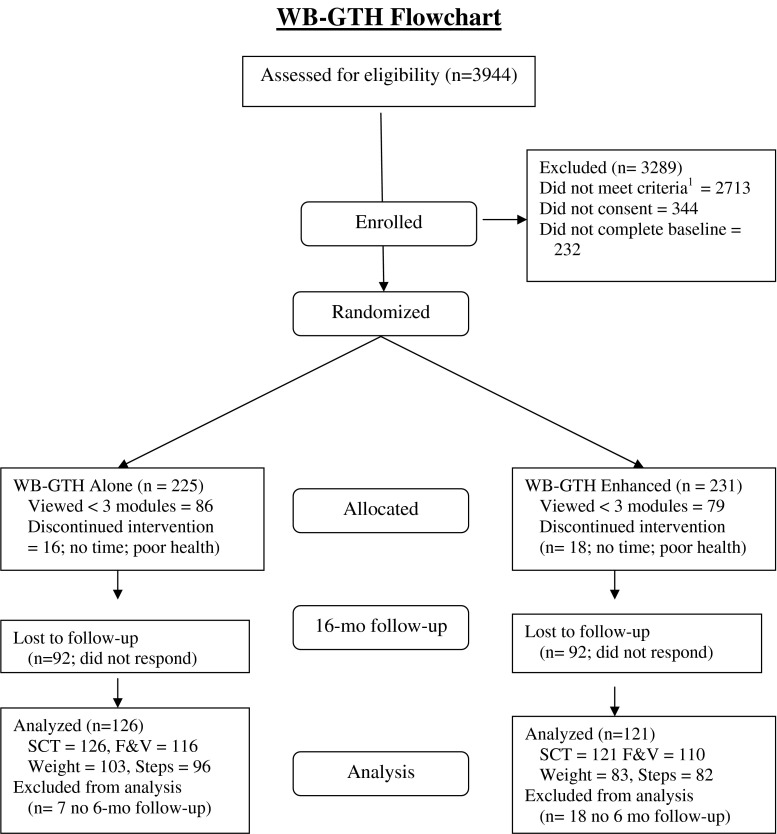
The project was reviewed by the full board of Virginia Tech’s Institutional Review Board and received approval on November 26, 2005. Recruitment and 16-month follow-up spanned the period September 2007 to February 2010. The web-based Guide to Health (WB-GTH) intervention study was conducted entirely online through the Guide-to-Health.com website. Participants were sedentary to low active, high normal weight to obese, but otherwise healthy adults (ages 18–63). Potential participants learned about the WB-GTH project from advertisements in print and online newspapers, and historically, African American newspapers, but primarily from print and online newsletters and listservs of existing organizations. All information described the program as focused on physical activity through walking, nutrition, and weight gain prevention (i.e., not weight management or weight loss). Almost 4,700 Internet users came to the WB-GTH information site that reiterated information provided in advertising and directed interested users to the main WB-GTH website. The first page of the main WB-GTH website provided a bit more detail about the eligibility requirements for the project, length of the program, and the research assessment requirements. To go beyond this “Welcome” page and determine eligibility, users were required to select a userid/password; 3,959 users (see Fig. 1; 85% of those coming to the site) completed this registration and 3,944 were assessed for eligibility. Potential participants were next screened via a series of webpages with questions about age (18–63-year-olds were eligible, with an age ceiling to reduce the risk of developing musculoskeletal problems from increased walking), body mass index (BMI; eligible range was 23 to 39), health status (healthy participants were eligible; those with existing diseases or musculoskeletal disorders were not eligible), and PA (eligibility criteria: less than 20 min of exercise three times a week and <10,000 steps a day assessed later). About 31% (1,231) of those registering at the website qualified for the WB-GTH study. Of ineligible participants, 45% were outside the BMI range (42% with BMI >39), 34% reported exclusory medical conditions (cardiovascular, pulmonary, liver, kidney disease, or thyroid disease, diabetes, cancer within the last 5 years, very limited fitness, currently pregnant or plan to be pregnant, and musculoskeletal problems limiting walking; [23]), and 20% were too active. Eligible participants received full information about the research project and completed informed consent online. About 74% of those found eligible consented to participate in the study (n = 963). Next, participants were asked to complete a series of online questionnaires, requiring about 2 h and assessing PA levels, food intake, and health beliefs. Participants then received a pedometer, digital bathroom scale, and walking-and-weight log in the mail. After 7 days of keeping the log (see below), participants returned to the WB-GTH website to report their daily steps and minutes in planned walking, height, and weight. About 75% (n = 731) of participants consenting to the WB-GTH study completed baseline assessments. Participants whose reported steps (<10,000/day) and BMI (23 to 39) were within the eligible range (about 90% of those completing these assessments; n = 655) qualified for the study. Participants were then automatically randomly assigned to one of the two interventions WB-GTH-Basic (n = 327) or WB-GTH-Enhanced (n = 328). Differences between the intervention conditions were not explained to participants. Post-assessment occurred 6 months after baseline and follow-up occurred 16 months after baseline. Participants were paid $20 for completing post-assessments and $30 for completing follow-up assessments. Participants were sent an email at the start of each assessment phase and were taken to post- and follow-up assessments when they logged into the WB-GTH website. Participant who did not begin assessments within 7 days were sent an automatic reminder email. If after 3 weeks an assessment was not completed, final emails were sent by research staff from the research office.
Fig 1.
Flow of participants from enrollment to 16-month analysis point in the web-based Guide to Health (WB-GTH) trial. 1 Included participants were 18–63 years old, body mass index of 23 to 39, with less than 20 min of exercise three times a week and <10,000 steps/day, and otherwise healthy. F&V fruits and vegetables
Figure 1 shows the flow diagram for the study.
Participants
Of the 655 automatically randomly assigned participants, 165 participants did not complete three or more programs (WB-GTH-Basic, n = 86; WB-GTH-Enhanced, n = 79) and 34 participants withdrew from the program (WB-GTH-Basic, n = 16; WB-GTH-Enhanced, n = 18) and, for purposes of assessing efficacy, were considered as essentially not using the program. In each group, 92 engaged participants did not provide follow-up data, and a small number of engaged participants who did provide follow-up data had not provided post-data (WB-GTH-Basic, n = 7; WB-GTH-Enhanced, n = 18). As shown in Fig. 1, the present report focuses on eligible, “engaged” participants who completed at least three modules and who also provided data for baseline and post- and follow-up assessments (n = 247). This represents 37.7% of randomly assigned participants and 54.2% of engaged participants. Thus, the analyses presented include data from participants who completed at least three program modules and all assessments.
Engaged participants completing baseline and 6-month post- and 16-month follow-up assessments and at least three program modules (n = 247) had a mean age of 43.9 years (10.52), range 19–63 years; 87.5% were female and 91.5% were Caucasian. The sample was well educated with a mean of 17.5 (3.0) years of education, range of 3–20 years, and had a median annual household income of about $85,000. Nevertheless, about 83% were overweight or obese and about 75% were sedentary (i.e., <5,000 steps/day) or had lower levels of activity (i.e., <7,500 steps/day).
Compared to engaged participants (n = 456), non-engaged participants (n = 199) reported taking fewer steps per day at baseline (M = 6,215, SD = 1,897; M = 5,749, SD = 2030; F[1, 653] = 7.99, p = 0.005). There were no other differences between engaged and non-engaged participants across other variables. Of those engaged participants who did not return for follow-up assessments (n = 184; see Fig. 1), the only difference across variables was that those participants not returning had a higher BMI (M = 30.4, SD = 4.2) than those participants returning (M = 29.2, SD = 3.8; F[1, 454] = 9.70, p = 0.002). In addition, 25 engaged participants (see Fig. 1), who did not provide post-assessment data (but who did complete follow-up assessments), were not included in the analyses.
The WB-GTH intervention
The WB-GTH program consisted of 52 weekly SCT-based modules of 15–20 screens (taking 5–10 min per module). It was based on a much briefer, more generic, 12-module program, also called Guide to Health, used within a church-based intervention [24] with the prior and present program based on social cognitive theory [22]. All modules were available prior to the 16-month assessment. Randomly assigned participants logged-in as often as once a week with the username/password they created during enrollment. Following SCT, modules 1–5 targeted self-efficacy (i.e., guided, gradual behavior change, e.g., increasing steps 400 steps per/day, and increasing intake of fruit and vegetable (F&V) by one serving per day) and introduced self-regulatory strategies (i.e., tracking food intake, daily steps). In addition to self-efficacy and self-regulation (i.e., providing feasible and acceptable strategies, e.g., building steps into one’s normal routine and switching to acceptable fat modified foods), modules 6–16 focused on outcome expectations, on garnering social support for walking and nutrition changes, and on increasing PA enjoyment. Modules 17–52 involved continued self-regulation to enhance and maintain nutrition and PA behavior change.
The WB-GTH-Basic program provided in one study condition included the content noted above within a rich audio-visual format (using text-to-speech software) that was presented and guided by on-screen male and female (avatar) “coaches” with different ethnic characteristics. In addition, after completion of a module, monitoring forms for tracking each day’s steps and planning walks, servings of fruits and vegetables, low-fat dairy, whole-grain products, and caution foods (regular soft drinks, candy, higher calorie snacks), and noting body weight were emailed as attachments to participants. Participants reported these values on the site at the beginning of each module. Consistent with SCT, feedback and goal setting pertinent to the overall program goal in each area reported was provided, as well as content urging participants to plan for meeting goals in the upcoming week. Participants viewed behavior change strategies for increasing PA (e.g., scheduling walks at a specific time on selected days) and improving nutrition (e.g., switching to whole-grain bread). WB-GTH-Basic users received program goals for adding steps and walking minutes to their daily routines (add 400 steps/day each week up to 3,000 steps and 5 min up to 30 min 5 days/week). Program goals for adding F&V (one per day each week to reach five to nine for female and five to ten for male users), whole-grain foods and low-fat dairy foods (one per day each week for up to three servings a day), and decreasing high fat and high sugar caution foods (no more than 28 servings each week) were also provided. Thus, the WB-GTH-Basic condition included detailed tracking and reporting of PA and nutrition goal attainment, feedback (e.g., comparison of current levels and overall goals), restatement of program goals, information about strategies, and prompts for users to plan for the next week. In addition, participants received a reminder email 10 days and then again 15 days after their last module if they had not returned to the site to complete the next module.
WB-GTH-Enhanced included all the features of the Basic program plus provided an enhanced and a comprehensive [25] approach to self-regulation including tailored planning, feedback, and goal setting, given the primacy within SCT of self-regulation for health behavior changes [22]. Participants in this condition were emailed monitoring forms as attachments with their forms providing individuals with their specific goals for each target behavior plus individualized walking plans specified by each participant in the completed module. Tailored feedback and goal setting were based on meeting the previously designated walking plan plus algorithms combining step counts, weight gain, and nutrition variables, progress in each area, and specific module. In addition, participants selected specific behavior change strategies for increasing PA (e.g., scheduling walks at a specific time on selected days) and improving nutrition (e.g., switching to whole-grain bread) and set individualized goals for steps and for adding fruits and vegetable, whole-grain, and low-fat dairy foods and decreasing caution foods. The Enhanced condition also included reporting on the use of selected strategies which led to tailored feedback (e.g., “Nice work, you met your goal of adding 300 steps a day!”) and refinement of goals and plans for the next week. The same email reminders used in the Basic condition were used in the Enhanced condition. Thus, the major difference between the Basic and Enhanced conditions was the more general compared to the highly tailored goal setting, planning, and feedback self-regulation components. It was hypothesized that the WB-GTH-Enhanced would produce greater change in physical activity (pedometer step counts), servings of fruits and vegetables, and body weight than WB-GTH-Basic. Based on the previous church-based trial noted above [24], it was estimated that at follow-up assessment, with n = 112 per group, an effect size of d = 0.39 could be detected for group differences in steps counts and for servings of fruits and vegetables.
Measures
Nutrition
The Block 2005 Food Frequency Questionnaire [26] was completed online at baseline, 6-months, and 16-months and provided the estimates of participants’ intake of daily servings of F&V examined in the current study.
PA and body weight
Participants were provided with a pedometer (Yamax Digi-walker SW-200; Antonio, TX), a digital bathroom scale (Health-O-Meter HDL150-01, Sunbeam Products, Inc., Maitland, FL, or Tanita 313, Arlington Heights, IL), and a 7-Day Walking Log at baseline, 6-months, and 16-months follow-up. PA was measured by mean daily steps taken over 1 week. Participants wore their pedometers for 7 days and recorded the number of steps registered at the end of each day [27] and returned to the WB-GTH website to report their step counts. Participants were asked to use the bathroom scale provided to weigh themselves without clothing just after waking in the morning or before going to bed in the evening. Participants were instructed to record their weight in pounds on the space provided on the walking log and to report their weight online along with their walking log data.
Social cognitive variables
The Health Beliefs Survey, shown to be reliable and valid as detailed in previous research [28, 29], was administered online and measured nutrition- and PA-related social support, self-efficacy, outcome expectations, and self-regulation at baseline, 6-months, and 16-months.
Fruit and vegetable consumption and steps per day were considered primary outcome measures while bodyweight and SCT measures were considered secondary outcome measures.
Statistical analysis
Repeated measures, analysis of variance conducted on baseline and 6-month and 16-month data tested the effects of the two WB-GTH treatments (WB-GTH-Basic and WB-GTH-Enhanced) and level of baseline behavior separately for daily steps taken, servings of fruits and vegetables consumed, and bodyweight. Two additional repeated measures MANOVAs tested the effects of treatment on participants’ PA-related and nutrition-related social cognitive characteristics.
RESULTS
WB-GTH outcomes
There was no difference in the mean module completion between groups (WB-GTH-Basic = 23.2 (17.5); WB-GTH-Enhanced = 22.2 (17.1), F[1, 245] = 0.18, p = 0.67). The changes observed across the two WB-GTH treatments were similar for steps (time × condition: F[2, 156] = 1.74, ηp2 = 0.26, p = 0.18), fruits and vegetable servings (time × condition: F[2, 220] = 0.61, ηp2 = 0.005, p = 0.55), and body weight (time × condition: F[1, 164] = 0.13, ηp2 = 0.002, p = 0.87).
Across both conditions, however, participants made and maintained improvements in each area: steps (baseline, M = 6,179, SE = 61; 6 months, M = 7,787, SE = 193; 16-months, M = 7,602, SE = 257; time: F[2, 156] = 43.67, ηp2 = 0.358, p = < 0.001), fruits and vegetable servings (baseline, M = 5.0, SE = 0.1; 6 months, M = 6.4, SE = 0.2, 16-months, M = 6.1, SE = 0.2; time: F[2, 220] = 29.37, ηp2 = 0.211, p < 0.001), and body weight (baseline, M = 171.9, SE = 1.6; 6 months, M = 167.0, SE = 1.7, 16 months, M = 168.0, SE = 1.8; time: F[2, 164] = 12.05, ηp2 = 0.128, p < 0.001).
As shown in Table 1, changes observed across the two WB-GTH treatments were similar for PA-related SCT variables (time × condition: F[18, 224] = 1.03, ηp2 = 0.076, p = 0.43). However, self-efficacy for overcoming barriers to PA decreased over time (baseline, M = 63.6, SE = 1.2; 6 months M = 61.2, SE = 0.1.5, 16 months M = 55.8, SE = 1.6; time: F[2, 241] = 512.54, ηp2 = .549, p < 0.001).
Table 1.
Baseline, 6-month, and 16-month nutrition and physical activity behaviors and social cognitive characteristics and body weight by baseline behavior level of participants in web-based Guide to Health
| Baseline level | Baseline | 6 months | 16 months | ||||
|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | ||
| Physical activity | |||||||
| Daily steps | Sedentarya | 3,763 | 118 | 6,232 | 372 | 5,943 | 495 |
| Inactiveb | 6,232 | 88 | 7,873 | 278 | 7,947 | 370 | |
| Low-activec | 8,540 | 110 | 9,255 | 346 | 8,915 | 461 | |
| Family support | Sedentary | 2.4 | 0.1 | 2.7 | 0.1 | 2.7 | 0.1 |
| Inactive | 2.4 | 0.1 | 2.7 | 0.1 | 2.7 | 0.1 | |
| Low-active | 2.6 | 0.1 | 2.9 | 0.1 | 2.9 | 0.1 | |
| Self-efficacy | Sedentary | 57.0 | 2.3 | 55.3 | 2.7 | 49.8 | 2.9 |
| Inactive | 66.1 | 1.7 | 62.4 | 2.0 | 57.5 | 2.2 | |
| Low-active | 67.8 | 2.4 | 65.8 | 2.8 | 60.0 | 3.1 | |
| Set goals and plan | Sedentary | 1.9 | .01 | 3.2 | 0.1 | 2.0 | 0.1 |
| Inactive | 2.00 | 0.1 | 3.6 | 0.1 | 3.1 | 0.1 | |
| Low-active | 2.1 | 0.1 | 3.6 | 0.1 | 3.2 | 0.1 | |
| Self-monitoring | Sedentary | 1.5 | 0.1 | 3.5 | 0.2 | 2.7 | 0.2 |
| Inactive | 1.5 | 0.1 | 3.7 | 0.1 | 2.8 | 0.1 | |
| Low-active | 1.6 | 0.1 | 3.7 | 0.2 | 2.9 | 0.2 | |
| Nutrition | |||||||
| F&V per day | <5 F&V/day | 2.8 | 0.1 | 5.0 | 0.2 | 4.7 | 0.2 |
| 5+ F&V/day | 7.2 | 0.2 | 7.8 | 0.3 | 7.5 | 0.3 | |
| Family support | <5 F&V/day | 2.6 | 0.1 | 3.0 | 0.1 | 3.0 | 0.1 |
| 5+ F&V/day | 2.9 | 0.1 | 3.2 | 0.1 | 3.2 | 0.1 | |
| Friends support | <5 F&V/day | 2.8 | 0.1 | 3.1 | 0.1 | 3.1 | 0.1 |
| 5+ F&V/day | 3.1 | 0.1 | 3.3 | 0.1 | 3.3 | 0.1 | |
| SE: avoid fat and sugar | <5 F&V/day | 75.1 | 1.3 | 76.9 | 1.3 | 76.3 | 1.4 |
| 5+ F&V/day | 78.4 | 2.1 | 79.2 | 2.0 | 77.4 | 2.3 | |
| SE: healthy eating | <5 F&V/day | 71.4 | 1.2 | 73.8 | 1.3 | 72.0 | 1.4 |
| 5+ F&V/day | 78.5 | 2.0 | 79.9 | 2.1 | 78.3 | 2.3 | |
| SE: plan and track | <5 F&V/day | 81.1 | 1.4 | 79.6 | 1.6 | 75.9 | 2.0 |
| 5+ F&V/day | 85.1 | 2.2 | 81.5 | 2.5 | 75.6 | 3.2 | |
| Negative OE | <5 F&V/day | 3.0 | 0.1 | 2.8 | 0.1 | 2.7 | 0.1 |
| 5+ F&V/day | 2.6 | 0.1 | 2.6 | 0.1 | 2.5 | 0.1 | |
| Plan and track nutrition | <5 F&V/day | 2.3 | 0.1 | 3.5 | 0.1 | 3.2 | 0.1 |
| 5+ F&V/day | 2.6 | 0.1 | 3.7 | 0.1 | 3.4 | 0.1 | |
| Regulate fat and sugar | <5 F&V/day | 2.9 | 0.1 | 3.8 | 0.1 | 3.8 | 0.1 |
| 5+ F&V/day | 3.3 | 0.1 | 4.0 | 0.1 | 3.9 | 0.1 | |
| Regulate healthy food choices | <5 F&V/day | 3.0 | 0.1 | 4.0 | 0.1 | 3.9 | 0.1 |
| 5+ F&V/day | 3.5 | 0.1 | 4.2 | 0.1 | 4.1 | 0.1 | |
| Weight (lb) | Normal weightd | 145.7 | 3.5 | 144.3 | 3.7 | 145.9 | 3.9 |
| Overweighte | 168.2 | 2.2 | 163.6 | 2.3 | 164.1 | 2.5 | |
| Obesef | 201.7 | 2.4 | 193.3 | 2.6 | 193.8 | 2.8 | |
F&V fruits and vegetables servings, SE self-efficacy, OE outcome expectations
aLess than 5,000 steps/day
b5,000–7,499 steps/day
c7,500–9,999 steps/day
dBMI <25
eBMI 25–29
fBMI 30+
As also shown in Table 1, changes in nutrition-related social cognitive characteristics observed across 16 months favored the WB-GTH-Enhanced condition (time × condition: F[22, 222] = 1.62, ηp2 = 0.139, p = 0.04). WB-GTH-Enhanced participants increased self-efficacy for reducing fat and calories (baseline, M = 76.0, SE = 1.7; 6 months, M = 78.9, SE = 1.7; 16 months, M = 79.0, SE = 1.9) while WB-GTH-Basic participants decreased (baseline, M = 77.5, SE = 1.8; 6 months, M = 77.3, SE = 1.7; 16 months, M = 74.7, SE = 1.9; time × condition: F[2, 243] = 3.43, ηp2 = 0.036, p = 0.01).
As shown in Table 2, across both conditions, WB-GTH users made improvements from baseline to 16 months in PA-related SCT variables (time: F[18, 224] = 41.10, ηp2 = 0.767, p < 0.001) and nutrition-related SCT variables (time: F[22, 222] = 16.40, ηp2 = 0.62, p < 0.001).
Table 2.
Influence of baseline social cognitive characteristics on change in social cognitive variables at 16-months among users of the web-based Guide to Health intervention
| Change at 16 months variable | Baseline level coefficient | |
|---|---|---|
| Β | t value | |
| Family support for physical activity | −0.43 | −7.44* |
| Self-efficacy for physical activity | −0.41 | −7.08* |
| Physical activity goal setting and planning | −0.45 | −7.80* |
| Physical activity self-monitoring | −0.37 | −6.18* |
| Family support for healthy nutrition | −0.40 | −6.92* |
| Friend support for healthy nutrition | −0.52 | −9.39* |
| Self-efficacy for avoiding high fat and high sugar foods | −0.42 | −7.31* |
| Self-efficacy for eating healthy foods | −0.38 | −6.46* |
| Self-efficacy for planning and tracking intake | −0.43 | −7.56* |
| Negative nutrition outcome expectations | −0.33 | −5.39* |
| Regulate healthy food choices | −0.64 | −13.18* |
| Plan and track nutrition | −0.49 | −8.79* |
| Regulate high fat and high sugar foods | −0.59 | −11.59* |
F&V fruit and vegetable servings
*p < 0.001
Effects by baseline levels
Baseline activity level
The number of steps participants took at baseline provided the basis [27] for dividing participants into three categories of physical activity: sedentary (less than 5,000 steps/day, n = 44), inactive (5,000–7,499 steps/day, n = 86), and lower active (7,500–9,999 steps/day, n = 48). The number of daily steps added over time by participants who were sedentary, inactive, or lower active at baseline differed (see Table 1; time × baseline step level: F[2, 157] = 4.119, ηp2 = .05, p = 0.018). The extent to which change in steps from baseline to the 16-month follow-up (i.e., 16-month daily steps minus baseline daily steps) differed by baseline step level was investigated directly (ANOVA). Sedentary participants increased steps (M = 2,314 steps; SD = 3,168) more than lower-active participants (M = 388, SD = 3,670, p = 0.009), but not more than participants in the inactive group (M = 1,680 steps, SD = 2,601) resulting in an overall effect for baseline step level (F[2, 175] = 4.87, ηp2 = 0.053, p = 0.009).
Baseline fruit and vegetable consumption
WB-GTH users who at baseline did not meet nutritional guidelines of consuming at least five F&V a day (n = 165) made greater increases in fruit and vegetable consumption at 16 months than users who consumed at least five F&V at baseline (n = 63; see Table 1; time × F&V level: F[1, 221] = 17.278, ηp2 = 0.073, p < 0.001).
Baseline BMI
Participants’ baseline BMI was used to create three weight categories normal weight (BMI <25; n = 34), overweight (BMI 25–29; n = 85), and obese (BMI ≥30; n = 67). The weight lost by participants over the course of the WB-GTH intervention depended on their baseline BMI levels (see Table 1; time × BMI level: F[2, 165] = 4.90, ηp2 = 0.056, p = 0.009). Change in weight from baseline to the 16-month follow-up differed by baseline BMI level (F[2, 183] = 5.95, ηp2 = 0.081, p < 0.003; ANOVA) and was greatest for obese participants (M = −7.8, SD = 14.2) who lost more pounds than normal weight participants (M = 0.6, SD = 7.9, p = 0.003). Neither of these groups differed from the amount lost by participants in the overweight group (M = −4.4, SD = 10.7, p > 0.15).
Baseline SCT levels
Although baseline behavior (i.e., steps taken or F&V consumed) did not influence how much participant’s social cognitive characteristics changed over the course of WB-GTH (nutrition: time × base F&V level; F[2, 222] = 1.11, ηp2 = 0.009, p = 0.337. PA: time × base step level; F[36, 450] = 0.96, ηp2 = 0.07, p = 0.52), secondary regression analyses, controlling for WB-GTH condition, indicated, without exception, baseline SCT levels were negatively related to change in SCT variables at the 16-month follow-up (see Table 2). Across the board, participants with lower social support, self-efficacy, and self-regulation levels at baseline made greater changes in these areas at follow-up.
DISCUSSION
The present study reports an early efficacy trial of a long-term, completely web-based intervention—WB-GTH—that electronically conducted all recruitment, assessment, and activities for a nutrition, physical activity, and weight-gain prevention program using standard assessment approaches over 16 months. There are several caveats and study limitations that temper the relatively positive findings. Analyses focused on participants who were more than merely tentative users of the program [30] and who participated in all assessment points. Including in analyses every participant who was randomized but did not complete all assessments and using procedures for missing values likely would have shown more minimal outcomes. However, it should be again noted that the analyses that were presented focused on assessment completers and not treatment completers, with some participants in the analyses only completing the bare minimum of three modules. Nevertheless, the outcomes should be viewed conservatively.
Similar to other reports of web-based interventions [9], attrition in WB-GTH was high (>50%). Web-based interventions often are accessible, removing time and place barriers to participation, but also easy to abandon as they can lack other features that may increase commitment and efficacy such as personal contact or, in this case, supportive, electronic social networking [9]. Additionally, participants self-reported their step counts, weight, and nutrition information and such reporting could be influenced by social desirability and other factors.
Short-term and stable users [30] of the WB-GTH participating in all assessments only represented 37.7% of the participants who consented and completed baseline assessments but did represent 54.2% of engaged participants. While less stringent initial exclusion criteria would have enabled more people to be eligible to participate, there is no reason to expect expanding inclusion criteria would have resulted in a greater percent of engaged participants. As noted, entirely web-based programs may be easy for users to abandon and the percent of tentative users of WB-GTH (about 25% or 165 of 655 viewing fewer than three weekly modules) is consistent with other web-based programs [9]. The length of the commitment may also been a barrier to program completion. Almost 70% (447 of 655) of WB-GTH users overall and 40% of users in the current report (94 of 247) stopped viewing content modules prior to the 6-month assessment. A third barrier to participants’ continuation was, perhaps, the extensive assessments entailed in a research trial—in WB-GTH, 299 participants completed the 6-month assessment, or 58% of 512 who began the assessment, or 46% of 655 participants eligible for the assessment.
WB-GTH primarily attracted middle-aged, well-educated, upper middle-class, Caucasian women. Despite these limitations, WB-GTH attracted and retained participants with a wide range of BMI, physical activity, and nutrition characteristics, and clearly, segments of the participants were at higher risk given baseline values [2, 3]. Nevertheless, a major challenge to meeting public health goals will be to attract diverse participants to WB-GTH and similar programs
With high attrition rates for viable Internet-based programs, RCTs evaluating interventions may not be able to provide untreated control or education-only conditions [9, 11]. It is likely that participation in such typical comparison conditions would present additional, differential, barriers to program completion. The danger, as demonstrated here, is that comparison groups based on essential and theoretically sound program components hypothesized to enhance outcomes may also influence behavior. Lack of differential effects renders conclusions about WB-GTH tentative given an alternative possibility that any program or simply the passage of time would have resulted in changes in a highly educated, confident sample similar to those recruited for WB-GTH. This seems unlikely, however. The effects of WB-GTH appear to be sustained over time, while for health behavior interventions, self-help and commercial programs [13, 14] typically produce minimal long-term effects, and even some more intensive, face-to-face long-term programs have shown minimal impacts on physical activity [15]. Moreover, in our prior church-based GTH project [24], face-to-face contacts allowed a waiting list control condition. At three assessment points using virtually the same measures as in this study, over the course of 16 months, the participants in the waiting list control showed no significant changes in fruits and vegetable consumption, steps per day, and bodyweight or SCT measures.
In addition to promoting improvements in some SCT variables, consumption of fruits and vegetable, steps per day, and a small weight loss, WB-GTH led to decreases in self-efficacy for barriers to physical activity and for planning and tracking nutrition consistent with the role of self-efficacy for changing unfamiliar behaviors [22]. Further, while self-efficacy decreased, participants reported increasing self-regulation behaviors. Individuals who make systematic, long-term attempts at changing behavior may be viewed as developing more realistic views of how difficult such changes can be [22]. Program developers need to be aware that high, perhaps, unrealistic self-efficacy may characterize people who access health behavior programs. Some content, in fact, can be framed in anticipation of some decline in self-efficacy, such as: “You may be finding this is harder than you thought, but don’t worry you are doing fine!”
There is some evidence that WB-GTH could be most efficacious for those individuals at higher initial levels of risk (either low step counts, or low consumption of fruits and vegetables, or high BMI at baseline). At follow-up, initially sedentary participants appear to have increased steps by about 2,200 steps/day compared to about 375 steps/day added by participants who were more active at baseline. Participants with low consumption of F&V at baseline appear to have added about two F&V servings per day at 16 months compared with about 0.3 F&V servings reported among participants initially consuming recommended levels. And obese participants appear to have lost about 3.5% of their bodyweight at 16 months while normal weight participants remained unchanged. A caveat is that the correlation between these baseline measures was low (all r < 0.14) such that different participants were represented in these different groups at baseline. For example, a participant could have very low step counts but be in the high F&V group. Nevertheless, lower physical activity, lower consumption of fruits and vegetables, and obesity is each associated with disease risk and change in any one of these is associated with decreased risk [2, 3].
Most encouraging was that changes in nutrition and physical activity were apparently maintained through a minimal contact (and in many cases, no contact) 16-month follow-up. In addition, while the caveats about the comparison group and diversity of participants pertain, the outcomes provide some evidence of weight gain prevention as a viable treatment goal. Across 16 months, participants in all BMI groups did not gain weight, and there was some evidence for a small weight loss. This is encouraging given that people with higher BMI levels are prone to weight gain [5, 6]. While WB-GTH was a weight gain prevention program and not a weight loss program, the reported weight loss is plausible. The program focused on small changes in energy consumption and expenditure that over time can result in a small weight loss [5]. For example, a consistent caloric deficit as small as 75 kcal/day could result in a year in a weight loss similar to the weight loss reported by obese participants in the current study.
The study’s results indicated that WB-GTH-Basic and WB-GTH-Enhanced produced about the same outcomes across measures. Both interventions included what can be considered essential behavior change components: relevant content about health and self-regulation strategies and consistent monitoring and reporting with feedback and goals plus minimal planning. And, both interventions used on-screen “coaches” and the same audio-visual characteristics. The elaborately tailored goal setting, planning, and feedback self-regulation component of WB-GTH-Enhanced did not further increase program efficacy. It also is of note that the mean number of modules that participants accessed was about 22 of 52 available. Many participants viewed the entire program content and behavior change components. Modules 17–52 focused on continued self-regulation of behavior providing minimal new content and “checking-in” (reporting behavior, receiving feedback). Perhaps other tactics such as electronic social networking or tailoring on preferred means of presentation and communication [10] would have produced longer program use and greater behavioral change. Key translation research points would thus include better access and appeal to diverse groups of people, simple, less time-consuming assessments, briefer intervention programming, and perhaps, commercial tie-ins where program participants can obtain pedometers and scales at substantial discounts. Regardless, the outcomes from the present study indicate that brief weekly interactions over several months with an entirely web-based program containing essential health behavior information and behavior change components, especially self-monitoring, may be sufficient for helping about 50% of people who engage with it to both initiate and maintain nutrition and physical activity behavior change and avoid weight gain.
Acknowledgments
We thank Ashley Dorough, Ph.D., of Virginia Tech, for her involvement in piloting and refining the physical activity component of the intervention and Todd Bowden, Ph.D., of PCR for helping to develop the software for the project. This project was supported by a grant from the National Cancer Institute (1R01CA106250-01A) to Virginia Tech., clinical trials identifier NCT00128570.
Conflicts of interest
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Footnotes
Implications
Practice: A relatively brief, entirely web-based program containing essential health behavior information and behavior change components, especially self-monitoring, can be sufficient for both initiating and maintaining nutrition and physical activity behavior changes and preventing weight gain in about 50% of people who actively are engaged in using a web-based program.
Policy: Resources should be directed toward the further development, evaluation, and dissemination of entirely web-based, health behavior programs.
Research: Research needs to be directed towards approaches to increase the diversity and long-term engagement of users of web-based, health behavior programs.
References
- 1.Winett RA, Tate DF, Anderson ES, Wojcik JR, Winett SG. Long-term weight gain prevention: a theoretically-based internet approach. Preventive Medicine. 2005;41:629–641. doi: 10.1016/j.ypmed.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 2.Goodarz D, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, Ezzati M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic factors. PLoS Medicine. 2009;6(4):e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford ES, Bergmann MM, Kroger J, Schienkiewitz A, Weikert C, Boeing H. Healthy living is the best revenge: findings from the European prospective study into cancer and nutrition—Potsdam study. Archives of Internal Medicine. 2009;169:1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- 4.Ritterband LM, Thorndike FP, Cox DJ, Kovatchev BP, Gonder-Frederick LA. A behavior change model for internet interventions. Annals of Behavioral Medicine. 2009;38:18–27. doi: 10.1007/s12160-009-9133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill JO. Can a small changes approach address the obesity epidemic? Journal of Clinical Nutrition. 2008;89:1–8. doi: 10.3945/ajcn.2008.26792. [DOI] [PubMed] [Google Scholar]
- 6.Bouchard C. The magnitude of the energy imbalance in obesity is generally underestimated. International Journal of Obesity. 2008;32:879–880. doi: 10.1038/sj.ijo.0803796. [DOI] [PubMed] [Google Scholar]
- 7.Katan MB, Ludwig DS. Extra calories cause weight gain but how much? JAMA. 2010;303:65–66. doi: 10.1001/jama.2009.1912. [DOI] [PubMed] [Google Scholar]
- 8.Ritterband LM, Tate DF. The science of internet interventions. Annals of Behavioral Medicine. 2009;38:1–3. doi: 10.1007/s12160-009-9132-5. [DOI] [PubMed] [Google Scholar]
- 9.Bennett GG, Glasgow RE. The delivery of public health interventions via the internet: actualizing their potential. Annual Review of Public Health. 2009;30:273–292. doi: 10.1146/annurev.publhealth.031308.100235. [DOI] [PubMed] [Google Scholar]
- 10.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;12(1):e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danaher BG, Seeley JR. Methodological issues on Web-based behavioral interventions. Annals of Behavioral Medicine. 2009;38:28–39. doi: 10.1007/s12160-009-9129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glasgow RE, Strycker LA, Kurz D, Faber A, Hillary Bell H, Dickman JM, Halterman E, Estabrooks PA, Diego O. Recruitment for an internet-based diabetes self-management program: scientific and ethical implications. Annals of Behavioral Medicine. 2010;40:40–48. doi: 10.1007/s12160-010-9189-1. [DOI] [PubMed] [Google Scholar]
- 13.Heshka S, Anderson JW, Atkinson RL, Greenway FL, Hill JO, Phinney SD, Kolotkin RL, Miller-Kovach K, Pi-Sunyer FX. Weight loss with self-help compared with a structured commercial program: a randomized trial. The Journal of the American Medical Association. 2003;289:1792–1798. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 14.Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Archives of Internal Medicine. 2005;142:56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 15.Elmer AJ, Vollmer WM, Simons-Morton D, et al. Effects of a comprehensive life style modification on diet, weight, physical activity, and blood pressure control: 18 months results of a randomized trial. Annals of Internal Medicine. 2006;144:485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 16.Strecher V. Internet methods for delivering behavioral and health-related interventions (eHealth) Annual Review of Clinical Psychology. 2007;3:53–76. doi: 10.1146/annurev.clinpsy.3.022806.091428. [DOI] [PubMed] [Google Scholar]
- 17.Tate DF, Finkelstein EA, Khavjou O. Cost effectiveness of internet interventions: review and recommendations. Annals of Behavioral Medicine. 2009;38:40–45. doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 19.Pew Internet & American Life Project (2009). Online activities: daily internet activities. http://www.pewinternet.org/Trend-Data/Online-Activities-Daily.aspx. Accessed April 20, 2010.
- 20.Pew Internet & American Life Project (2009b). Who’s online: demographics of Internet-users. http://www.pewinternet.org/Trend-Data/Whos-Online.aspx. Accessed April 20, 2010.
- 21.Roberts CK, Bernard RJ. Effects of exercise and diet on chronic diseases. Journal of Applied Physiology. 2005;98:3–30. doi: 10.1152/japplphysiol.00852.2004. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. The primacy of self-regulation in health promotion. Applied Psychology. 2005;54:245–254. doi: 10.1111/j.1464-0597.2005.00208.x. [DOI] [Google Scholar]
- 23.American College of Sports Medicine (2009). ACSM’s guidelines for exercise testing and prescription, 8th ed. Baltimore, MD: Williams Wilkins. [DOI] [PubMed]
- 24.Winett RA, Anderson ES, Wojcik JR, Winett SG, Bowden T. Guide to health: nutrition and physical activity outcomes of a group-randomized trial of an Internet-based intervention in churches. Annals of Behavioral Medicine. 2007;33:245–255. doi: 10.1007/BF02879907. [DOI] [PubMed] [Google Scholar]
- 25.Maes S, Karoly P. Self-regulation assessment and intervention in physical health and illness: a review. Applied Psychology. 2005;54:267–299. doi: 10.1111/j.1464-0597.2005.00210.x. [DOI] [Google Scholar]
- 26.Nutrition Quest (2005). Block 2005 Food Frequency Questionnaire. Berkle Nutrition Quest. Block 2005 Food Frequency Questionnaire. Berkley, CA; 2005.y, CA.
- 27.Tudor-Locke C, Bassett DR. How many steps/day are enough? Preliminary pedometer indices for public health. Sports Medicine. 2004;34:1–8. doi: 10.2165/00007256-200434010-00001. [DOI] [PubMed] [Google Scholar]
- 28.Anderson ES, Wojcik JR, Winett RA, Williams DM. Social cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome-expectations, and self-regulation. Health Psychology. 2006;25:510–520. doi: 10.1037/0278-6133.25.4.510. [DOI] [PubMed] [Google Scholar]
- 29.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Annals of Behavioral Medicine. 2007;34:304–312. doi: 10.1007/BF02874555. [DOI] [PubMed] [Google Scholar]
- 30.Eysenbach G. The law of attrition. Journal of Medical Internet Research. 2005;7:e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]