Abstract
“Invasive giant prolactinoma” is a large prolactinoma (>4 cm in dimension) presenting with serum prolactin levels of >1000 ng/dL and mass related clinical symptoms. Here we report a patient with a giant prolactinoma presented with central hypogonadism, suppressed adrenal and thyroid function, supra sellar extension, visual field impairment and high prolactin level.
The patient was treated with cabergoline, levothyroxin and prednisolone. After 18 months, tumor size markedly reduced, associated with adrenal function and visual field improvement, but central hypogonadism and secondary hypothyroidism persisted.
Previous studies showed normalization of thyrotropin secretion after treatment but it remained low in our patient even after 18 months follow up.
Keywords: Giant prolactinoma, Cabergoline, Hypothyroidism
Background
Prolactinoma is the most common pituitary adenoma [1] which causes infertitity, menstrual irregularity and galactorrhea [2,3] in women and hypogonadism, decreased libido, infertility, erectile dysfunction and gynecomastia [4,5] in men.
In the present report we describe an unusuall giant prolactin – producing macroadenoma of pituitary and its response to cabergoline (a dopamine agonist).
Case presentation
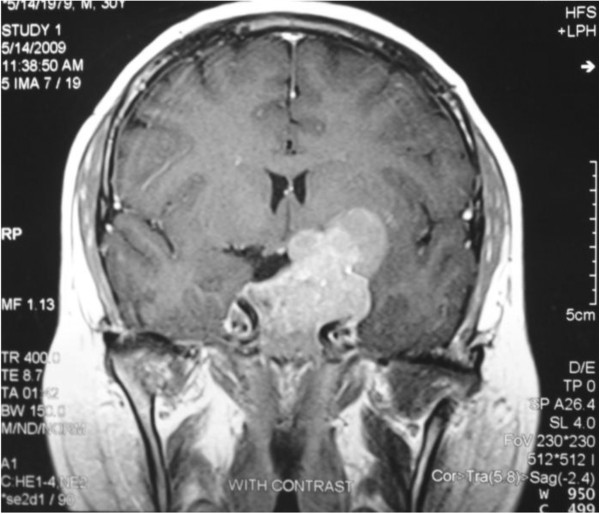
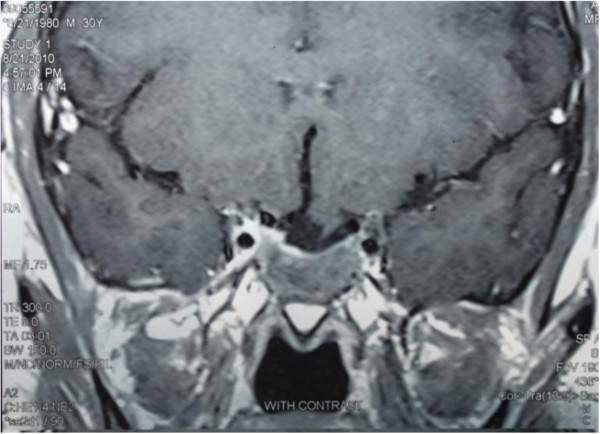
A 29 year – old married man was referred to us with headache, blurred vision, diplopia, decreased libido and weight gain from 12 months ago. He was married but did not have child. Laboratory evaluations showed prolactin levels as high as 12000 ng/mL (1.8–20) and further evaluations revealed central hypogonadism, secondary hypothyroidism, adrenal insufficiency and normal IGF1 level (Table 1). Pituitary MRI showed a large pituitary solid – cystic mass with suprasellar and left cranial fossa extension measuring 5.5 × 5.0 × 2.5 cm in dimension (Figure 1) and perimetry detected right side temporal hemianopia. Treatment with cabergoline (a dopamine agonist) 1 mg twice a week, levothyroxin 0.1 mg daily and prednisolone 7.5 mg resulted in visual improvement in one month. Prolactin level decreased to 222 ng/ml after 3 months but impotence and decreased libido didn’t show any improvement. Testosterone level was 1.32 ng/mL (2.8–8). He was started on testosterone (250 mg IM each 3 weeks) and cabergoline dose increased to 3 mg per week. One year after treatment, prolactin level reached to 165 ng/mL; ACTH stimulation test (Synacthen 0.25 mg IV injection and plasma cortisol measurement before, 30 and 60 min after administration) results were normal. So we discontinue prednisolone. Eighteen months later perimetry test showed normal results, prolactin level diminished to 71.5 ng/mL and tumor size markedly reduced on MRI to 2.2 × 2.3 × 1.2 cm in dimention (Figure 2) but central hypogonadism and secondary hypothyroidism persisted (Table 1).
Table 1.
Hormonal evaluation before and after treatment
| Normal range | Before treatment | After treatment | |
|---|---|---|---|
|
Prolactin |
1.8 – 20 ng/mL |
12000 |
71.5 |
|
IGF- I |
219 – 614.4 ng/mL |
120 |
230 |
| FSH |
1.4 – 15.4 mIU/mL |
0.6 |
3.1 |
|
LH |
1.2 – 7.8 mIU/mL |
0.8 |
2.7 |
|
Testosterone |
2.8 – 8 ng/mL |
<0.02 |
1 |
|
Cortisole |
6.2 – 14.4 micg/dL |
0.4 |
10 |
|
Cortisole 30 min after ACTH injection |
|
4.4 μg/dL |
22.2 μg/Dl |
|
Cortisole 60 min after ACTH injection |
|
5.2 μg/dL |
34.1 μg/Dl |
|
ACTH |
7.2 – 63 pg/dL |
8.8 |
|
|
T4 |
5.1 – 14 micg/dL |
5.5 |
8.2 |
| TSH | 0.5 – 5 mU/L | 2.05 | 0.2 |
Figure 1.
Huge macroprolactinoma with suprasellar invasion before treatment.
Figure 2.
14 months after treatment; significant tumor shrinkage.
Conclusion
Pituitary tumors larger than 4 cm in size are termed “giant adenomas” [6]. “Invasive giant prolactinoma” is defined as : 1) tumor diameter of >4 cm; 2) serum prolactin >1000 ng/mL; and 3) clinical symptoms induced by hyperprolactinemia or mass effect [7]. Most women lactotroph adenomas are microadenoma, however the men adenomas are usually larger [8]. Giant prolactinoma is rare and usually presents in men [9,10]. Complete surgical removal of giant tumor is difficult and biochemical cure is rare [11,12].
In prolactin – secreting macroadenemas, goals of treatment are to decrease tumor size, improve visual field defects and restore sexual function. Dopomine agonists are able to reach these goals with reducing tumor size [13,14]. In comparison with bromocriptine, cabergoline has fewer side effects and more positive effects at normalizing prolactin levels [15]. If visual field defect persists and chiasmal compression on MRI examination continues despite optimal medical treatment, surgery will be inevitable. But little is known about the role of dopamine agonist therapy in treatment of giant invasive prolactinomas. There were studies evaluating cabergoline (a dopamine agonist) in management of giant prolactinoma [14,16,17]. All of these studies showed that cabergoline is safe and well-tolerated and also suggested that cabergoline should be the first line of treatment for giant aggressive macroprolactionomas. In one study, cabergoline normalized prolactin levels in ten out of twelve patient and decreased significantly in the other two significantly. Visual field defect was present in nine patients at diagnosis which returned to normal in three of patients and improved in five after treatment. Tumor diameter responded to treatment with decrease of 47+/- 21% in size. Testosterone levels returned to normal in eight out of twelve patients. In this study only two of patients had secondary hypoadrenalism and hypothyroidism who improved after treatment [14]. Hypothyroidism and hypoadrenalism improve usually following normalization of prolactin level and tumor size in macroprolactinomas [14,15,18] but little is known about their recovery in giant prolactinoma. Hypogonadism persists in half of male patients with macroprolactinoma despite tumor shrinkage and normalization of prolactin levels [14,16,19,20]. Therefore testosterone replacement is required to maintain bone strength. Androgen can cause secondary rises in prolactin levels that postulated to central aromatization to estrogens [21].
In our case, tumor size markedly reduced and visual field and ACTH secretion recovered completely after 18 months of cabergline treatment but central hypogonadism and secondary hypothyroidism persisted. Somatotroph and gonadotroph cells are the most sensitive pituitary cells to injury secondary to sellar compression, but in this case thyrotroph cells also showed impaired function which did not recover after significant tumor shrinkage. With our best knowledge, there is not any report about this unusual response of giant prolactin-producing macroadenoma to cabergoline treatment in literature.
Consent
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interest.
Authors’ contribution
MR wrote the final version of manuscript, HAM read the case and comfirmed manuscript, BL supervise management of the case and approved manuscript, MRMT manage the patient and finalize the manuscript. All authors read and approved the final manuscript.
Contributor Information
Masoud Rahmanian, Email: rahmanian@razi.tums.ac.ir.
Hamidreza Aghaei Meybodi, Email: dr_aghai@yahoo.com.
Bagher Larijani, Email: EMRC@tums.ac.ir.
Mohammad-reza Mohajeri-Tehrani, Email: mrmohajeri@tums.ac.ir.
Acknowledgement
We appreciate patient and his family for their cooperation in this case report.
References
- Mindermann T, Wilson CB. Age – related occurrence of pituitary adenomas. Clin Endocrinol. 1999;41:359–364. doi: 10.1111/j.1365-2265.1994.tb02557.x. [DOI] [PubMed] [Google Scholar]
- Gomez F, Reyes FI, Faiman C. Nonpuerperal galactorrhea and hyperprolactinemia. Clinical Findings, endocrine features and therapeutic responses in 56 Cases. Am J Med. 1977;62:648–660. doi: 10.1016/0002-9343(77)90866-X. [DOI] [PubMed] [Google Scholar]
- Schelchte J, Sherman B, Halmi N. et al. Prolactin Secreting pituitary tumors in amenorrheic women: a comparative study. Endocrinol Rev. 1980;1:295. doi: 10.1210/edrv-1-3-295. [DOI] [PubMed] [Google Scholar]
- Carter JN, Faiman C, Tolis G. et al. Prolactin secreting tumors and hypogonadism in 22 men. N Engl J Med. 1978;299:847–852. doi: 10.1056/NEJM197810192991602. [DOI] [PubMed] [Google Scholar]
- Segal S, Yaffe H, Laufer N. Male hyperprolactinemia: effects on fertility. Fertil Steril. 1979;32:556–561. doi: 10.1016/s0015-0282(16)44359-1. [DOI] [PubMed] [Google Scholar]
- Murphy FY, Vesely DL, Jordan RM, Flamingan S, Kohler PO. Giant invasive prolactinomas. Am J Med. 1987;88:995–1002. doi: 10.1016/0002-9343(87)90668-1. [DOI] [PubMed] [Google Scholar]
- Siddiqui A, Chew N, Miszkiel K. Unusual orbital invasion by a giant prolactinoma. Br J Radiol. 2008;81:259–262. doi: 10.1259/bjr/98771490. [DOI] [PubMed] [Google Scholar]
- Delgrange E, Trouillas J, Maiter D. et al. sex – related difference in the growth of prolactinomas: a clinical and proliferation marker study. J Clin Endocrinol Metab. 1997;82:2102–2107. doi: 10.1210/jc.82.7.2102. [DOI] [PubMed] [Google Scholar]
- Shrivastava RK, Arginteanu MS, King WA, Post KD. Giant prolactinomas:clinical management and long-term follow up. J Neurosurg. 2002;97:299–306. doi: 10.3171/jns.2002.97.2.0299. [DOI] [PubMed] [Google Scholar]
- Corsello SM, Ubertini G, Altomare M, Lovicu RM, Migneco MG, Rota CA, Colosimo C. Giant prolactinomas in men: efficacy of cabergoline treatment. Clin Endocrinol. 2003;58:662–670. doi: 10.1046/j.1365-2265.2003.01770.x. [DOI] [PubMed] [Google Scholar]
- Davis JR, Sheppard MC, Health DA. Giant invasive prolactinoma: a case report and review of nine further cases. Q J Med. 1990;74:227–238. [PubMed] [Google Scholar]
- Ciric I, Mikhael M, Stafford T, Lawson L, Garces R. Transsphenoidal microsurgery of pituitary macroadenoma with long-term follow up results. J Neurosurg. 1983;59:395–401. doi: 10.3171/jns.1983.59.3.0395. [DOI] [PubMed] [Google Scholar]
- Verheist J, Abs R, Maiter D. et al. Cabergoline in the treatment of hyperprolactinemia: a study in 455 patients. J Clin Endocrinol Metab. 1999;84:2518–2522. doi: 10.1210/jc.84.7.2518. [DOI] [PubMed] [Google Scholar]
- Shiman I, Benbassat C, Hadani M. Effectiveness of long-term cabergoline treatment for giant prolactinoma: study of 12 men. Eur J Endocrinol. 2007;156:225–231. doi: 10.1530/EJE-06-0646. [DOI] [PubMed] [Google Scholar]
- Webster J, Piscitelli G, Polli A, Ferrari CI, Ismail I, Scanlon MF. A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. N Engl J Med. 1994;331:904–909. doi: 10.1056/NEJM199410063311403. [DOI] [PubMed] [Google Scholar]
- Cho EH, Lee SA, Chung JY, Koh EH, Cho YH, Kim JH, Kim CJ, Kim MS. Efficacy and safety of cabergoline as first line treatmentfor invasive giant prolactinoma. J Korean Med Sci. 2009;24:874–878. doi: 10.3346/jkms.2009.24.5.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acharya SV, Gopal RA, Menon PS, Bandgar TR, Shah NS. Giant prolactinoma and effectiveness of medical management. Endocrinol Pract. 2010;16:42–46. doi: 10.4158/EP09221.OR. [DOI] [PubMed] [Google Scholar]
- Colao A, Vitale G, Cappabianca P. et al. Outcome of cabergoline treatment in men with prolactinoma: effects of a 24- month treatmemt on prolactin level, tumor mass, recovery of pituitary fumction and semen analysis. J Clin Endocrinol Metab. 2004;89:1704–1711. doi: 10.1210/jc.2003-030979. [DOI] [PubMed] [Google Scholar]
- Pinzone JJ, Katznelson L, Danila DC, Pauler DK, Miller CS, Klibanski A. Primary medical therapy of micro- and macroprolactinomas in men. J Clin Endocrinol Metab. 2000;85:3053–3057. doi: 10.1210/jc.85.9.3053. [DOI] [PubMed] [Google Scholar]
- De Rosa M, Zarrilli S, Vitale G, Disomma C. et al. Six months of treatment with cabregeline restores sexual potency in hyper prolactinemic males: an open longitudinal study monitoring nocturnal penile tumescence. J Clin Endocrinol Metab. 2004;89:621–625. doi: 10.1210/jc.2003-030852. [DOI] [PubMed] [Google Scholar]
- Gillam MP, Middler S, Freed DJ, Molitch ME. The novel use of very high doses of cabergoline and a combination of testosterone and aromatase inhibitor in the treatment of giant prolactinoma. J Clin Endocrinol Metab. 2002;87:4447–4451. doi: 10.1210/jc.2002-020426. [DOI] [PubMed] [Google Scholar]