Abstract
Background.
There is no consensus regarding the definition of frailty for clinical uses.
Methods.
A modified Delphi process was used to attempt to achieve consensus definition. Experts were selected from different fields and organized into five Focus Groups. A questionnaire was developed and sent to experts in the area of frailty. Responses and comments were analyzed using a pre-established strategy. Statements with an agreement more than or equal to 80% were accepted.
Results.
Overall, 44% of the statements regarding the concept of frailty and 18% of the statements regarding diagnostic criteria were accepted. There was consensus on the value of screening for frailty and about the identification of six domains of frailty for inclusion in a clinical definition, but no agreement was reached concerning a specific set of clinical/laboratory biomarkers useful for diagnosis.
Conclusions.
There is agreement on the usefulness of defining frailty in clinical settings as well as on its main dimensions. However, additional research is needed before an operative definition of frailty can be established.
Keywords: Frailty, Consensus definition, Older people, Biomarkers
The concept of frailty has grown in importance because of a need for a better understanding of the health and functional status of older persons and a need to prevent or at least delay the onset of late-life disability and its adverse consequences (1). There is to date no clear consensus regarding the definition of frailty (2,3). The most frequently used definition (4) is focused on the evaluation of five domains (nutritional status, energy, physical activity, mobility, and strength) and has established five criteria (one per each domain: weight loss, exhaustion, leisure time activity, gait speed, and grip strength, respectively) for defining the frail phenotype and for identifying older persons at elevated risk for numerous adverse outcomes.
However, other definitions have been proposed, each with their own strengths and weaknesses (5). In addition to assessing physical functioning, many researchers believe that frailty definitions should also include domains, such as cognition, mood, and other aspects of mental health (6,7). Frailty definitions should be validated in a wide variety of cultural, economic, ethnic, and clinical settings (8) and demonstrate the predictive validity of frailty for adverse outcomes (9,10).
The diagnosis of frailty relies currently on the assessment of a relatively small subset of easily measurable clinical markers (eg, Fried Criteria). While recognizing the multifactorial nature of frailty, it is important to develop an “operational definition” of frailty that is simple enough to be used clinically and to guide prevention and care. A working group of experts from a variety of fields related to frailty were invited to participate in a collaborative project, with the aim of developing the most complete and concrete definition of frailty possible.
METHODS
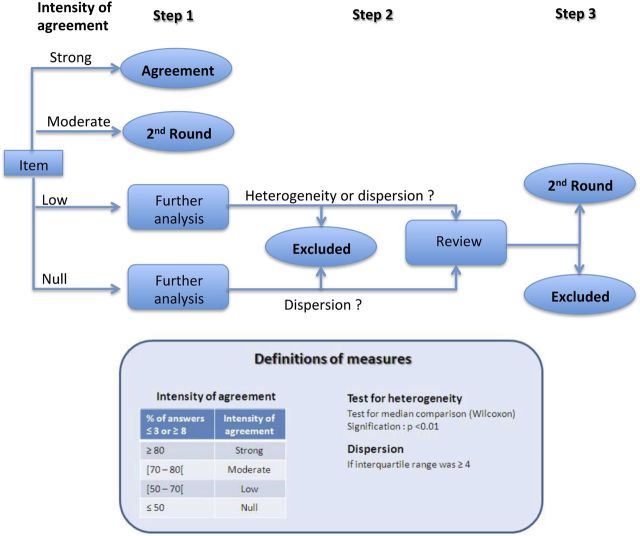
To reach consensus between experts, we used a traditional Delphi process (Figure 1; (11)) with some minor modifications that increased the role of panel members in questionnaire development. The Delphi technique is well suited for consensus building because of its proven ability to expose underlying assumptions and to seek out new perspectives that can help lead to consensus among multiple respondents (12).
Figure 1.
Flow chart of the Delphi process.
Selection of the Panel of Experts
Five Focus Groups (FG) of experts (geriatricians, nongeriatrician physicians, other health professionals, basic scientists, and social and nongovernmental workers) were selected to represent various fields with an interest in frailty. Each FG was composed of 5–7 experts and a chairman. FG experts were selected based on their background and experience and their willingness to work toward the achievement of consensus following Delphi procedures (13). Participants were provided the main objectives and tasks and a compilation of peer-reviewed publications on frailty. Overall, 848 articles were chosen for initial review, and 113 were selected for final distribution. All FG members received 27 articles that were common to all groups and another 20 specific articles specific to their specialty.
Development and Administration of the Questionnaires
Preliminary questionnaire.
All FG members received an Open-ended Preliminary Questionnaire. Responses were collated and discussed during the first face-to-face meeting.
First meeting (February 2011).
Discussions among FG members led to the development of a set of statements for the First Round Questionnaire (1RQ). The 1RQ consisted of 107 statements. All experts were asked to score each statement on a 10-point numerical scale ranging from 1 (no agreement) to 10 (full agreement).
Second meeting (May 2011).
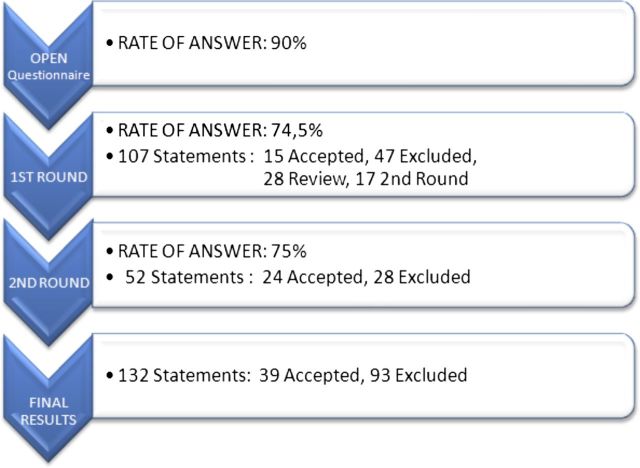
During a second face-to-face meeting, participants established criteria to determine strength of agreement and analyzed the 1RQ data (Figure 2). To improve the response rate for the questionnaire (81 of 130: 62%), nonrespondents were recontacted, and additional experts were selected for those FGs that had the lowest rate of response in the initial analysis.
Figure 2.
Methods and cutoff points to classify the statements according to the reached agreement.
Second round questionnaire.
The Second Round Questionnaire (2RQ) consisted of 52 statements and was sent to all the experts who evaluated the 1RQ. To facilitate agreement among experts, respondents were asked to try to either accept (score 8, 9, and 10) or reject (score 1, 2, and 3) the proposed statements.
Final meeting (October 2011).
The statements accepted into the definition were presented, discussed, and submitted for approval in the final meeting.
Statistical Analysis
Statistical analyses were performed in accordance with previously established procedures (14). We used a stepwise procedure to select the final statements (Figure 3). Every statement was classified into one of four groups: Strong agreement (>80% of answers rated ≥8 or ≤3), moderate agreement (70%–80%), low agreement (50%–70%), and no agreement (<50%). Statements with moderate agreement were selected to enter the 2RQ, and statements with low or no agreement were further analyzed to determine if it was due to heterogeneity (assessed using tests for median comparison, ie, Wilcoxon scores rank test) or due to dispersion (assessed by the presence of an Inter Quartile Range ≥4). All items meeting criteria for heterogeneity or dispersion were re-reviewed and included in the 2RQ if members believed a consensus could be reached or if appropriate modifications could improve the clarity of the statement.
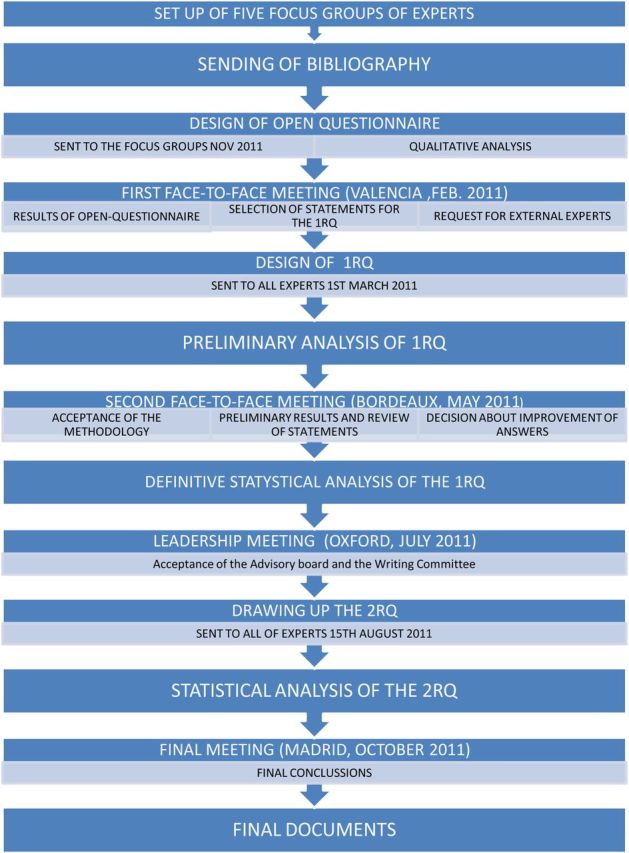
Figure 3.
Rate of answer and status of the statements in the different stages of our Delphi process.
RESULTS
Thirty-one experts participated in the FGs. An additional 121 experts responded the questionnaires.
The response rate in both rounds was similar (74.5% and 75%). A total of 29.1% of statements were finally accepted (39 of 134; Table 1). Statements pertaining to diagnosis or biomarkers of frailty had the lowest agreement rates. Statements regarding the framework or structure of frailty reached a consensus in 38% of cases, whereas only 16% of the biomarker statements were accepted (Table 2). The multi-dimensional nature of frailty was broadly accepted, as was the necessity to include multiple domains in its assessment. However, experts could not reach agreement about any single clinical definition. Consensus was not reached about the usefulness of specific laboratory biomarkers. Nor was there consensus about procedures to reach a diagnosis of frailty. Forty-four percent of the statements regarding the underlying concept of frailty were accepted, whereas only 18% of the statements about diagnosis were accepted.
Table 1.
List of Accepted Statements (in Light Gray, Statements Accepted After the First Round; in Dark Gray, Statements Accepted After the Second Round)
| Statements | Answers ≤3 | Answers ≥8 | Classification | Second Classification | ||
| n | % | n | % | |||
| 4. Frailty may be a clinical syndrome. | 7 | 8.4 | 69 | 83.1 | Framework | Concept |
| 6. Frailty is characterized by decreased reserve and diminished resistance to stressors | 2 | 1.8 | 95 | 85.6 | Framework | Concept |
| 7. The same definition of frailty should be valid across different clinical settings | 2 | 2.4 | 70 | 84.3 | Framework | Concept |
| 9. The definition must show reproducibility across time. | 2 | 2.4 | 72 | 86.8 | Framework | Concept |
| 12. The concept of frailty and its operational definition can help in identifying and stratifying older persons at high risk of disability and/or other adverse outcomes | 2 | 1.8 | 98 | 88.3 | Framework | Prognosis |
| 13. Frailty is multidimensional and may involve psychological, social, emotional and spiritual aspects in addition to physical components | 4 | 3.6 | 90 | 81.8 | Framework | Diagnostic |
| 21. Frailty is a condition of older people with increased vulnerability in which minimal stress may cause functional impairment | 1 | 1.2 | 73 | 88 | Framework | Prevention and/or treatment |
| 22. Frailty might be reversible or attenuated by interventions | 2 | 2.4 | 71 | 85.5 | Framework | Prevention and/or treatment |
| 23. Frailty is a condition where prevention may still be possible and it is mandatory for clinicians and health workers to detect it as early as possible | 2 | 2.4 | 72 | 86.8 | Framework | Concept |
| 24. Frailty is a dynamic nonlinear process | 3 | 2.7 | 93 | 83.8 | Framework | Concept |
| 26. Frailty is a dynamic process, nonlinear, different from vulnerability and disability | 2 | 2.4 | 79 | 95.2 | Framework | Concept |
| 27. Frailty increases vulnerability to impairments and the ensuing consequences | 1 | 0.9 | 97 | 89 | Framework | Prognosis |
| 28. Frailty involves alterations in multiple, not individual, body systems | 6 | 5.5 | 89 | 81.7 | Framework | Concept |
| 29. Frailty involves alteration in several domains of function | 3 | 2.7 | 88 | 80 | Framework | Concept |
| 32. Frailty cannot be defined in terms of a single molecular mechanism | 5 | 4.6 | 96 | 88.9 | Framework | Concept |
| 39. Frailty is different from disability | 4 | 4.8 | 74 | 89.2 | Framework | Concept |
| 40. Frailty typically involves alteration in multiple systems | 3 | 3.6 | 75 | 90.4 | Framework | Diagnostic |
| 43. Definitions must be tested in clinical and non-clinical settings | 8 | 7.3 | 92 | 83.6 | Framework | Concept |
| 45. The purpose of diagnosing frailty is to identify the nonrobust, nondisabled older patient, which is at risk of adverse health outcomes in the near future | 4 | 4.8 | 73 | 88 | Framework | Diagnostic |
| 46. Frailty diagnosis is useful in primary care and community care | 0 | 0 | 74 | 89.2 | Framework | Diagnostic |
| 47. A Frailty diagnosis is useful in managing older people with chronic diseases | 3 | 3.6 | 67 | 80.7 | Biomarkers | Diagnostic |
| 48. A diagnosis of frailty is only necessary in settings specialized in geriatric medicine | 67 | 80.7 | 6 | 7.2 | Framework | Diagnostic |
| 59. It is important to know the predictive value of biomarkers | 1 | 0.9 | 91 | 83.5 | Biomarkers | Diagnostic |
| 60. There is no single biomarker that is adequate to predict or diagnose frailty | 3 | 2.8 | 95 | 88 | Biomarkers | Diagnostic |
| 64. Mental health assessment and cognitive status evaluation are highly recommended as part of the assessment of frailty. | 4 | 4.8 | 70 | 84.3 | Frailty versus disability | Prognosis |
| 96. Frailty is not disability | 2 | 1.8 | 94 | 84.7 | Frailty versus disability | Concept |
| 97. Frailty and disability may coexist but they do not require each other to be present | 4 | 3.6 | 94 | 85.5 | Frailty versus disability | Concept |
| 99. Frailty is a risk factor for disability, although disability can exist without previous frailty | 2 | 1.8 | 102 | 91.9 | Frailty versus disability | Concept |
| 100. Frailty has different predictive values for different health outcomes (including disability, falls, hospitalization, permanent institutionalization and death) | 3 | 2.8 | 88 | 81.5 | Frailty versus disability | Prognosis |
| 101. The predictive value of Frailty depends of its severity | 5 | 6 | 69 | 83.1 | Framework | Concept |
| 102. The frailty process is modulated by disease | 3 | 3.6 | 72 | 86.8 | Frailty versus Disability | Diagnostic |
| 104. Frailty modifies the negative effects of comorbidities leading to adverse outcomes | 1 | 1.2 | 71 | 85.5 | Frailty versus disability | Prognosis |
| N6. Physical activity should be considered an intervention for the management of frailty | 3 | 3.6 | 72 | 86.8 | Biomarkers | Prevention and/or treatment |
| N7. Healthy lifestyles are important for the prevention and recovery of frailty | 3 | 3.6 | 73 | 88 | Biomarkers | Prevention and/or treatment |
| N8. Determining nutritional status can be important in the diagnosis of frailty | 2 | 2.4 | 68 | 81.9 | Biomarkers | Diagnostic |
| N9. Determining cognitive status can be important in the diagnosis of frailty | 2 | 2.4 | 71 | 85.5 | Biomarkers | Diagnostic |
| N14. Physical performance tests can be important in the diagnosis of frailty | 1 | 1.2 | 78 | 94 | Biomarkers | Diagnostic |
| N16. Assessing gait speed can be important in the diagnosis of frailty | 3 | 3.6 | 69 | 83.1 | Biomarkers | Diagnostic |
| N17. Mobility assessment can be important in the diagnosis of frailty | 2 | 2.4 | 72 | 86.8 | Biomarkers | Diagnostic |
Table 2.
Percent Acceptance of Statements by Category
| Final | ||
| Total, n | Accepted, n (%) | |
| Framework | 57 | 22 (38.6) |
| Biomarkers | 63 | 10 (15.9) |
| Frailty versus disability | 9 | 6 (66.6) |
| Frailty versus comorbidity | 4 | 1 (25.0) |
| Animal models | 1 | 0 (0.0) |
| Total | 134 | 39 (29.1) |
| Concept | 36 | 16 (44.4) |
| Diagnosis | 78 | 14 (17.9) |
| Prognosis | 15 | 5 (33.3) |
| Prevention/treatment | 5 | 4 (80.0) |
| Total | 134 | 39 (29.1) |
Experts agreed that frailty and disability are distinct entities, but an agreement on the relationships between frailty and comorbidities was not established (Table 2). However, 80% of the statements regarding prevention and treatment of frailty were accepted (Table 2).
DISCUSSION
The aim of the Frailty Operative Definition-Consensus Conference Project was to reach a consensus definition of frailty that is useful in daily practice using, for the first time in frailty research by implementing a Delphi consensus building process.
In our study, experts agreed on the importance of a more comprehensive definition of frailty that should include assessment of physical performance, including gait speed and mobility, nutritional status, mental health, and cognition. Although a consensus was reached on these six domains, the proposed diagnostic paths and procedures needed to achieve an operational definition were not agreed upon, with only one of six of the statements related to diagnosis achieving consensus.
Experts agreed that no single biomarker by itself was adequate for the assessment of frailty, suggesting a need for a combination of multiple biomarkers. However, none of the proposed combinations of biomarkers was able to reach the 80% threshold of agreement required by the Delphi process. Importantly, among all the laboratory biomarkers suggested for the assessment of frailty, none was accepted.
The low level of consensus regarding the constituent elements to be included in an operational definition of frailty is balanced by the high degree of agreement regarding the underlying conceptual framework of frailty. The experts clearly agreed that frailty is a multidimensional syndrome characterized by decreased reserve and diminished resistance to stressors. The experts established a clear-cut difference between disability and frailty as shown by the percentage of agreement (85%–95%) in the related statements. This notion is somewhat different from the World Health Organization conceptualization of disability, in which disability is considered to be contextual and every human being can experience some degree of disability (15). Frailty was also differentiated from vulnerability. While everybody is potentially vulnerable, frailty represents a state of extreme vulnerability where minimal stress may cause functional impairment.
Although frailty has a clear conceptual framework, there is no single operational definition of frailty that can satisfy all experts. A possible explanation may be a paucity of data from primary research sources, which make efforts to reach a consensus premature. Supporting this perspective, we found agreement regarding the necessity to combine biomarkers but no agreement regarding which combination of biomarkers to include in the definition; agreement regarding the necessity to assess the severity of frailty but no agreement on identifying specific severity markers; agreement on the relation between age and frailty but little agreement on establishing an age threshold to assess frailty. Finally, there was substantial disagreement about the timeline for assessing clinical and laboratory biomarkers in the diagnostic process. These areas of agreement and disagreement provide a valuable road map for future research on frailty.
CONCLUSION S
Additional experimental work is needed to identify the specific combination of clinical and laboratory biomarkers that can be used for the diagnosis of frailty. Such studies may well enable us to move beyond a theoretical definition of frailty to a robust consensual operational definition that can be employed in a variety of settings.
FUNDING
Supported by EU HEALTH.2010.2.2.2-5 (Grant agreement no.: 261270) program, Red Temática de Investigación Cooperativa en Envejecimiento y Fragilidad (RD06/0013), Instituto de Salud Carlos III, Ministry of Science and Innovation, Spain and by the Intramural Research Program of the National Institute on Aging, National Institutes of Health , USA.
Acknowledgments
The views expressed in this article are those of the author(s) and do not necessarily represent the views or policies of the World Health Organization. Note: Results from the Frailty Operative Definition-Consensus Conference project.
References
- 1.Seeman TE, Merkin SS, Crimmins EM, Karlamangla AS. Disability trends among older Americans: National Health And Nutrition Examination Surveys, 1988-1994 and 1999-2004. Am J Public Health. 2010;100:100–107. doi: 10.2105/AJPH.2008.157388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abellan van Kan G, Rolland Y, Bergman H, Morley JE, Kritchevsky SB, Vellas B. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12:29–37. doi: 10.1007/BF02982161. [DOI] [PubMed] [Google Scholar]
- 3.Rockwood K, Hogan DB, MacKnight C. Conceptualisation and measurement of frailty in elderly people. Drugs Aging. 2000;17:295–302. doi: 10.2165/00002512-200017040-00005. [DOI] [PubMed] [Google Scholar]
- 4.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 5.de Vries NM, Staal JB, van Ravensberg CD, Hobbelen JS, Olde Rikkert MG, Nijhuis-van der Sanden MW. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev. 2010;10:104–114. doi: 10.1016/j.arr.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Bergman H, Ferrucci L, Guralnik J, et al. Frailty: an emerging research and clinical paradigm–issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62:731–737. doi: 10.1093/gerona/62.7.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Avila-Funes JA, Amieva H, Barberger-Gateau P, et al. Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: the three-city study. J Am Geriatr Soc. 2009;57:453–461. doi: 10.1111/j.1532-5415.2008.02136.x. [DOI] [PubMed] [Google Scholar]
- 8.Avila-Funes JA, Aguilar-Navarro S, Melano-Carranza E. [Frailty, an enigmatic and controversial concept in geriatrics. The biological perspective] Gac Med Mex. 2008;144:255–262. [PubMed] [Google Scholar]
- 9.Robinson TN, Eiseman B, Wallace JI, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250:449–455. doi: 10.1097/SLA.0b013e3181b45598. [DOI] [PubMed] [Google Scholar]
- 10.Sundermann S, Dademasch A, Rastan A, et al. One-year follow-up of patients undergoing elective cardiac surgery assessed with the Comprehensive Assessment of Frailty test and its simplified form. Interact Cardiovasc Thorac Surg. 2010;13:119–123. doi: 10.1510/icvts.2010.251884. ; discussion 123. [DOI] [PubMed] [Google Scholar]
- 11.Turoff M, Linstone H. The Delphi Method: Techniques and Applications. Reading, MA: Addison-Wesley Publishing Company; 1975. [Google Scholar]
- 12.Delbecq AL, Van de Hen AH, Gustafson DH. Group Techniques for Program Planning. Glenview, IL: Scott, Foresman, and Co; 1975. [Google Scholar]
- 13.Pill J. The Delphi method: substance, context, a critique and an annotated bibliography. Socio-Econ Plan Sci. 1975;5:57–71. [Google Scholar]
- 14.Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Practical Assess Res Eval. 2007;12:1–8. [Google Scholar]
- 15.World Health Organization. International Classification of Functioning, Disability and Health (ICF) Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]